Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study
et al., Diabetologia, doi:10.1007/s00125-020-05180-x, CORONADO, NCT04324736, May 2020
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 1,317 hospitalized COVID-19 patients with diabetes showing lower mortality with metformin use, without statistical significance.
|
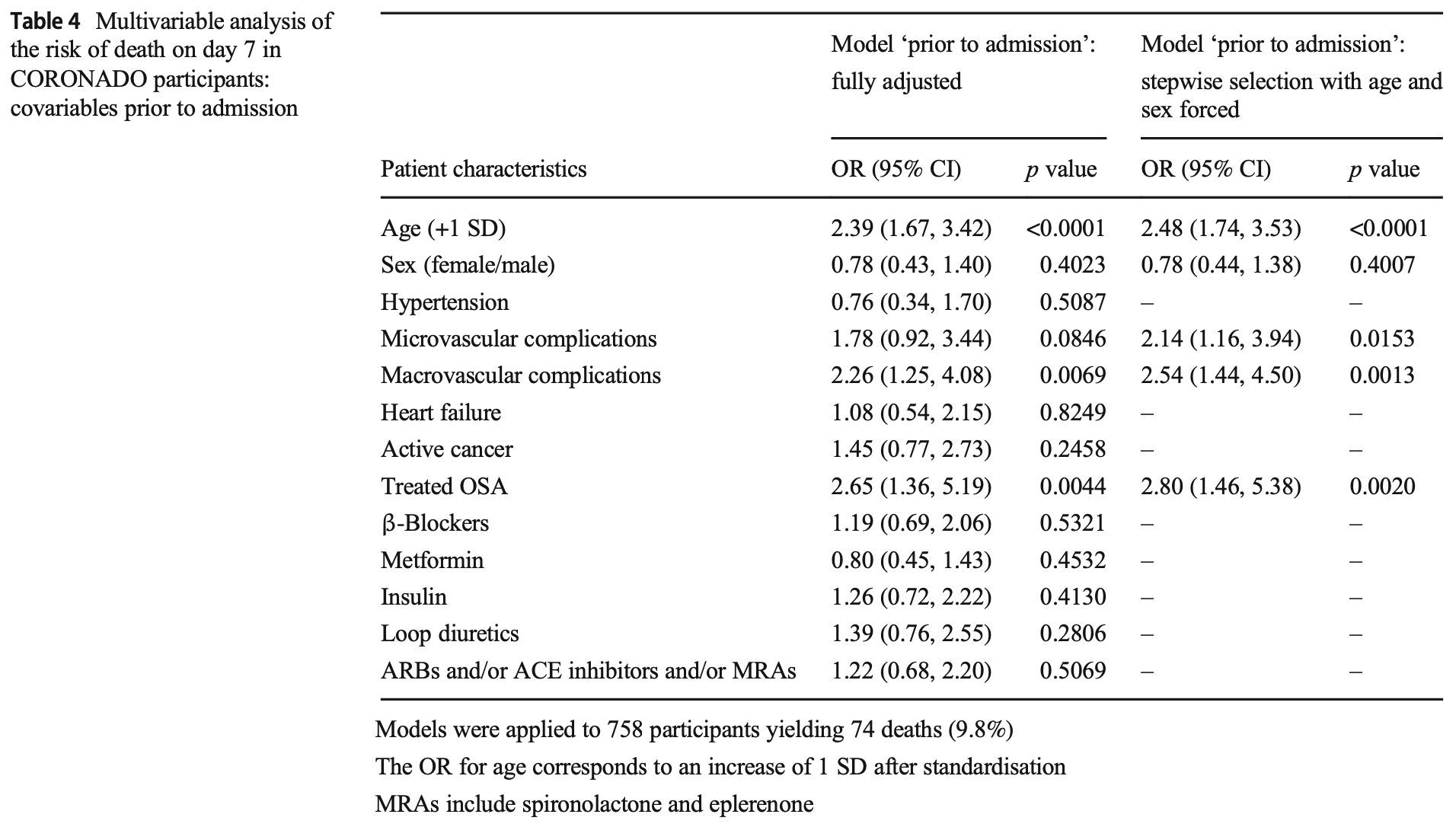
risk of death, 20.0% lower, OR 0.80, p = 0.46, treatment 746, control 571, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Cariou et al., 29 May 2020, retrospective, France, peer-reviewed, mean age 69.8, 41 authors, study period 10 March, 2020 - 10 April, 2020, trial NCT04324736 (history) (CORONADO).
Contact: bertrand.cariou@univ-nantes.fr, samy.hadjadj@univ-nantes.fr.
Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study
doi:10.1007/s00125-020-05180
Aims/hypothesis Coronavirus disease-2019 (COVID-19) is a life-threatening infection caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) virus. Diabetes has rapidly emerged as a major comorbidity for COVID-19 severity. However, the phenotypic characteristics of diabetes in COVID-19 patients are unknown. Methods We conducted a nationwide multicentre observational study in people with diabetes hospitalised for COVID-19 in 53 French centres in the period 10-31 March 2020. The primary outcome combined tracheal intubation for mechanical ventilation and/or death within 7 days of admission. Age-and sex-adjusted multivariable logistic regressions were performed to assess the prognostic value of clinical and biological features with the endpoint. ORs are reported for a 1 SD increase after standardisation. Results The current analysis focused on 1317 participants: 64.9% men, mean age 69.8 ± 13.0 years, median BMI 28.4 (25th-75th percentile: 25.0-32.7) kg/m 2 ; with a predominance of type 2 diabetes (88.5%). Microvascular and macrovascular diabetic complications were found in 46.8% and 40.8% of cases, respectively. The primary outcome was encountered in 29.0% (95% CI 26.6, 31.5) of participants, while 10.6% (9.0, 12.4) died and 18.0% (16.0, 20.2) were discharged on day 7. In univariate analysis, characteristics prior to admission significantly associated with the primary outcome were sex, BMI and previous treatment with renin-angiotensin-aldosterone system (RAAS) blockers, but not age, type of diabetes, HbA 1c , diabetic complications or glucoselowering therapies. In multivariable analyses with covariates prior to admission, only BMI remained positively associated with the primary outcome (OR 1.28 [1.10, 1.47]). On admission, dyspnoea (OR 2.10 [1.31, 3.35]), as well as lymphocyte count (OR A complete list of the CORONADO trial investigators is provided in the Electronic supplementary material (ESM).
Authors' relationships and activities BC reports grants and personal fees from Amgen, personal fees from AstraZeneca, personal fees from Akcea, personal fees from Genfit, personal fees from Gilead, personal fees from Eli Lilly, personal fees from Novo Nordisk, personal fees from MSD, grants and personal fees from Sanofi, and grants and personal fees from Regeneron. SH reports personal fees and non-financial support from AstraZeneca, grants and personal fees from Bayer, personal fees from Boehringer Ingelheim, grants from Dinno Santé, personal fees from Eli Lilly, non-financial support from LVL, personal fees and non-financial support from MSD, personal fees from Novartis, grants from Pierre Fabre Santé, personal fees and non-financial support from Sanofi, personal fees and non-financial support from Servier, and personal fees from Valbiotis. MP reports personal fees and non-financial support from Novo Nordisk, non-financial support from Sanofi, and non-financial support from Amgen. SB reports personal fees from Novo Nordisk, personal fees from Sanofi, personal fees from Eli Lilly, personal fees from Medtronic, and personal fees from Abbott. PD reports personal fees from Novo Nordisk, personal fees from Sanofi, personal fees from Eli Lilly, personal fees from MSD, personal fees from Novartis, personal fees from Abbott, personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, and personal fees from Mundipharma. BG reports personal fees from Eli Lilly, personal..
References
Alqahtani, Aleanizy, Hadi, Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: a retrospective study, Epidemiol Infect, doi:10.1017/S0950268818002923
Bhatraju, Ghassemieh, Nichols, Covid-19 in critically ill patients in the Seattle region -case series, N Engl J Med, doi:10.1056/NEJMoa2004500
Centre, St, Joseph -St, Luc, Lyon, Rennes, France 26 Département d'Endocrinologie et de Diabétologie
Drucker, Coronavirus infection and type 2 diabetes shared-pathways with therapeutic implications, Endocr Rev, doi:10.1056/NEJMsr2005760
Fosse-Edorh, Mandereau-Bruno, Piffaretti, Le poids du diabète en France en 2016 Synthèse épidémiologique. Santé p u b l i q u e F, doi:10.1056/NEJMoa011300
Garg, Kim, Whitaker, Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 -COVID-NET, 14 States, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6915e3
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcome of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy, JAMA, doi:10.1001/jama.2020.5394
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Huang, Anthonius, Pranata, Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia -a systematic review, meta-analysis, and metaregression, Diabetes Metab Syndr, doi:10.15585/mmwr.mm6913
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, Lancet, doi:10.1016/S0140-6736(20)30183-5
Kulcsar, Coleman, Beck, Frieman, Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection, JCI Insight, doi:10.1016/j.dsx.2020.04.018
Muller, Gorter, Hak, Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus, Clin Infect Dis, doi:10.1086/431587
Onder, Rezza, Brusaferro, Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy, JAMA, doi:10.1001/jama.2020.4683
Pornet, Bourdel-Marchasson, Lecomte, Trends in the quality of care for elderly people with type 2 diabetes: the need for improvements in safety and quality (the 2001 and 2007 ENTRED Surveys), Diabetes Metab, doi:10.1016/j.csda.2005.07.015
Roncon, Zuin, Rigatelli, Zuliani, Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome, J Clin Virol, doi:10.1016/j.jcv.2020.104354
Sauerbrei, Meier-Hirmer, Benner, Royston, Multivariable regression model building by using fractional polynomials: description of SAS, STATA and R programs, Comput Stat Data Anal, doi:10.1016/j.csda.2005.07.015
Schetz, Jong, Deane, Obesity in the critically ill: a narrative review, Intensive Care Med, doi:10.1002/oby.22831
Shah, Hux, Quantifying the risk of infectious diseases for people with diabetes, Diabetes Care, doi:10.2337/diacare.26.2.510
Simonnet, Chetboun, Poissy, High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity, doi:10.1172/jci.insight.13177
Vaduganathan, Vardeny, Michel, Mcmurray, Pfeffer et al., Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19, N Engl J Med, doi:10.1007/s00134-019-05594-1
Van Den Berghe, Wouters, Weekers, Intensive insulin therapy in critically ill patients, N Engl J Med, doi:10.1210/endrev/bnaa011
Wu, Chen, Cai, Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China, JAMA Intern Med, doi:10.1001/jamainternmed.2020.0994
Yang, Feng, Yuan, Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS, Diabet Med, doi:10.1111/j.1464-5491.2006.01861.x
Yang, Yu, Xu, Clinical course and outcomes of critically ill patients with SARS-CoV2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med, doi:10.1016/j.diabet.2011.02.001
Yang, Zheng, Gou, Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.03.01
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)305
DOI record:
{
"DOI": "10.1007/s00125-020-05180-x",
"ISSN": [
"0012-186X",
"1432-0428"
],
"URL": "http://dx.doi.org/10.1007/s00125-020-05180-x",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Aims/hypothesis</jats:title>\n <jats:p>Coronavirus disease-2019 (COVID-19) is a life-threatening infection caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) virus. Diabetes has rapidly emerged as a major comorbidity for COVID-19 severity. However, the phenotypic characteristics of diabetes in COVID-19 patients are unknown.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>We conducted a nationwide multicentre observational study in people with diabetes hospitalised for COVID-19 in 53 French centres in the period 10–31 March 2020. The primary outcome combined tracheal intubation for mechanical ventilation and/or death within 7 days of admission. Age- and sex-adjusted multivariable logistic regressions were performed to assess the prognostic value of clinical and biological features with the endpoint. ORs are reported for a 1 SD increase after standardisation.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>The current analysis focused on 1317 participants: 64.9% men, mean age 69.8 ± 13.0 years, median BMI 28.4 (25th–75th percentile: 25.0–32.7) kg/m<jats:sup>2</jats:sup>; with a predominance of type 2 diabetes (88.5%). Microvascular and macrovascular diabetic complications were found in 46.8% and 40.8% of cases, respectively. The primary outcome was encountered in 29.0% (95% CI 26.6, 31.5) of participants, while 10.6% (9.0, 12.4) died and 18.0% (16.0, 20.2) were discharged on day 7. In univariate analysis, characteristics prior to admission significantly associated with the primary outcome were sex, BMI and previous treatment with renin–angiotensin–aldosterone system (RAAS) blockers, but not age, type of diabetes, HbA<jats:sub>1c</jats:sub>, diabetic complications or glucose-lowering therapies. In multivariable analyses with covariates prior to admission, only BMI remained positively associated with the primary outcome (OR 1.28 [1.10, 1.47]). On admission, dyspnoea (OR 2.10 [1.31, 3.35]), as well as lymphocyte count (OR 0.67 [0.50, 0.88]), C-reactive protein (OR 1.93 [1.43, 2.59]) and AST (OR 2.23 [1.70, 2.93]) levels were independent predictors of the primary outcome. Finally, age (OR 2.48 [1.74, 3.53]), treated obstructive sleep apnoea (OR 2.80 [1.46, 5.38]), and microvascular (OR 2.14 [1.16, 3.94]) and macrovascular complications (OR 2.54 [1.44, 4.50]) were independently associated with the risk of death on day 7.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusions/interpretations</jats:title>\n <jats:p>In people with diabetes hospitalised for COVID-19, BMI, but not long-term glucose control, was positively and independently associated with tracheal intubation and/or death within 7 days.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Trial registration</jats:title>\n <jats:p><jats:ext-link xmlns:xlink=\"http://www.w3.org/1999/xlink\" ext-link-type=\"uri\" xlink:href=\"http://clinicaltrials.gov\">clinicaltrials.gov</jats:ext-link> NCT04324736.</jats:p>\n </jats:sec>",
"alternative-id": [
"5180"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "23 April 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "7 May 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "29 May 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Date",
"name": "change_date",
"order": 4,
"value": "22 November 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Type",
"name": "change_type",
"order": 5,
"value": "Update"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Details",
"name": "change_details",
"order": 6,
"value": "The link in reference 15 has been corrected."
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Date",
"name": "change_date",
"order": 7,
"value": "2 July 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Type",
"name": "change_type",
"order": 8,
"value": "Correction"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Details",
"name": "change_details",
"order": 9,
"value": "A Correction to this paper has been published:"
},
{
"URL": "https://doi.org/10.1007/s00125-020-05207-3",
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Details",
"name": "change_details",
"order": 10,
"value": "https://doi.org/10.1007/s00125-020-05207-3"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-1580-8040",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cariou",
"given": "Bertrand",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-7110-6994",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hadjadj",
"given": "Samy",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6027-9486",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wargny",
"given": "Matthieu",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6822-6132",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pichelin",
"given": "Matthieu",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7951-9926",
"affiliation": [],
"authenticated-orcid": false,
"family": "Al-Salameh",
"given": "Abdallah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Allix",
"given": "Ingrid",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0581-7592",
"affiliation": [],
"authenticated-orcid": false,
"family": "Amadou",
"given": "Coralie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Arnault",
"given": "Gwénaëlle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baudoux",
"given": "Florence",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bauduceau",
"given": "Bernard",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6240-8253",
"affiliation": [],
"authenticated-orcid": false,
"family": "Borot",
"given": "Sophie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bourgeon-Ghittori",
"given": "Muriel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7348-7161",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bourron",
"given": "Olivier",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9722-2029",
"affiliation": [],
"authenticated-orcid": false,
"family": "Boutoille",
"given": "David",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4325-023X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cazenave-Roblot",
"given": "France",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chaumeil",
"given": "Claude",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8785-3385",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cosson",
"given": "Emmanuel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Coudol",
"given": "Sandrine",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1726-2296",
"affiliation": [],
"authenticated-orcid": false,
"family": "Darmon",
"given": "Patrice",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4045-0503",
"affiliation": [],
"authenticated-orcid": false,
"family": "Disse",
"given": "Emmanuel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ducet-Boiffard",
"given": "Amélie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4180-158X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gaborit",
"given": "Bénédicte",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8731-7355",
"affiliation": [],
"authenticated-orcid": false,
"family": "Joubert",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kerlan",
"given": "Véronique",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9541-6708",
"affiliation": [],
"authenticated-orcid": false,
"family": "Laviolle",
"given": "Bruno",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9101-5002",
"affiliation": [],
"authenticated-orcid": false,
"family": "Marchand",
"given": "Lucien",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3687-5522",
"affiliation": [],
"authenticated-orcid": false,
"family": "Meyer",
"given": "Laurent",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6268-7360",
"affiliation": [],
"authenticated-orcid": false,
"family": "Potier",
"given": "Louis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prevost",
"given": "Gaëtan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7991-0741",
"affiliation": [],
"authenticated-orcid": false,
"family": "Riveline",
"given": "Jean-Pierre",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5989-5409",
"affiliation": [],
"authenticated-orcid": false,
"family": "Robert",
"given": "René",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1862-4252",
"affiliation": [],
"authenticated-orcid": false,
"family": "Saulnier",
"given": "Pierre-Jean",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9540-8222",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sultan",
"given": "Ariane",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4926-9943",
"affiliation": [],
"authenticated-orcid": false,
"family": "Thébaut",
"given": "Jean-François",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0696-974X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Thivolet",
"given": "Charles",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tramunt",
"given": "Blandine",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8342-1596",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vatier",
"given": "Camille",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2292-8363",
"affiliation": [],
"authenticated-orcid": false,
"family": "Roussel",
"given": "Ronan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6458-2001",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gautier",
"given": "Jean-François",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5362-3813",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gourdy",
"given": "Pierre",
"sequence": "additional"
},
{
"affiliation": [],
"name": "for the CORONADO investigators",
"sequence": "additional"
}
],
"container-title": "Diabetologia",
"container-title-short": "Diabetologia",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2020,
5,
29
]
],
"date-time": "2020-05-29T06:02:31Z",
"timestamp": 1590732151000
},
"deposited": {
"date-parts": [
[
2021,
11,
30
]
],
"date-time": "2021-11-30T18:47:08Z",
"timestamp": 1638298028000
},
"funder": [
{
"DOI": "10.13039/100019009",
"award": [
"CORONADO Initiative Emergency Grant"
],
"doi-asserted-by": "crossref",
"name": "Fondation Francophone pour la Recherche sur le Diabète"
},
{
"DOI": "10.13039/100007542",
"award": [
"CORONADO Initiative Emergency grant"
],
"doi-asserted-by": "publisher",
"name": "Air Liquide"
},
{
"award": [
"CORONADO Initiative Emergency Grant"
],
"name": "Sociéte Francophone du Diabète"
}
],
"indexed": {
"date-parts": [
[
2023,
9,
8
]
],
"date-time": "2023-09-08T05:02:56Z",
"timestamp": 1694149376375
},
"is-referenced-by-count": 546,
"issue": "8",
"issued": {
"date-parts": [
[
2020,
5,
29
]
]
},
"journal-issue": {
"issue": "8",
"published-print": {
"date-parts": [
[
2020,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
5,
29
]
],
"date-time": "2020-05-29T00:00:00Z",
"timestamp": 1590710400000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
5,
29
]
],
"date-time": "2020-05-29T00:00:00Z",
"timestamp": 1590710400000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00125-020-05180-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s00125-020-05180-x/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00125-020-05180-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "1500-1515",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2020,
5,
29
]
]
},
"published-online": {
"date-parts": [
[
2020,
5,
29
]
]
},
"published-print": {
"date-parts": [
[
2020,
8
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"author": "C Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"issue": "10223",
"journal-title": "Lancet",
"key": "5180_CR1",
"unstructured": "Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223):497–506. https://doi.org/10.1016/S0140-6736(20)30183-5",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"author": "WJ Guan",
"doi-asserted-by": "publisher",
"first-page": "1708",
"issue": "18",
"journal-title": "N Engl J Med",
"key": "5180_CR2",
"unstructured": "Guan WJ, Ni ZY, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18):1708–1720. https://doi.org/10.1056/NEJMoa2002032",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.2337/diacare.26.2.510",
"author": "BR Shah",
"doi-asserted-by": "publisher",
"first-page": "510",
"issue": "2",
"journal-title": "Diabetes Care",
"key": "5180_CR3",
"unstructured": "Shah BR, Hux JE (2003) Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care 26(2):510–513. https://doi.org/10.2337/diacare.26.2.510",
"volume": "26",
"year": "2003"
},
{
"DOI": "10.1086/431587",
"author": "LM Muller",
"doi-asserted-by": "publisher",
"first-page": "281",
"issue": "3",
"journal-title": "Clin Infect Dis",
"key": "5180_CR4",
"unstructured": "Muller LM, Gorter KJ, Hak E et al (2005) Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus. Clin Infect Dis 41(3):281–288. https://doi.org/10.1086/431587",
"volume": "41",
"year": "2005"
},
{
"DOI": "10.1111/j.1464-5491.2006.01861.x",
"author": "JK Yang",
"doi-asserted-by": "publisher",
"first-page": "623",
"issue": "6",
"journal-title": "Diabet Med",
"key": "5180_CR5",
"unstructured": "Yang JK, Feng Y, Yuan MY (2006) Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med 23(6):623–628. https://doi.org/10.1111/j.1464-5491.2006.01861.x",
"volume": "23",
"year": "2006"
},
{
"DOI": "10.1017/S0950268818002923",
"author": "FY Alqahtani",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Epidemiol Infect",
"key": "5180_CR6",
"unstructured": "Alqahtani FY, Aleanizy FS, Ali El Hadi Mohamed R et al (2018) Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: a retrospective study. Epidemiol Infect 147:1–5. https://doi.org/10.1017/S0950268818002923",
"volume": "147",
"year": "2018"
},
{
"DOI": "10.1016/j.ijid.2020.03.01",
"author": "J Yang",
"doi-asserted-by": "publisher",
"first-page": "91",
"journal-title": "Int J Infect Dis",
"key": "5180_CR7",
"unstructured": "Yang J, Zheng Y, Gou X et al (2020) Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis 94:91–95. https://doi.org/10.1016/j.ijid.2020.03.01",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.5394",
"author": "G Grasselli",
"doi-asserted-by": "publisher",
"first-page": "1674",
"issue": "16",
"journal-title": "JAMA",
"key": "5180_CR8",
"unstructured": "Grasselli G, Zangrillo A, Zanella A et al (2020) Baseline characteristics and outcome of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 323(16):1674–1581. https://doi.org/10.1001/jama.2020.5394",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6915e3",
"author": "S Garg",
"doi-asserted-by": "publisher",
"first-page": "458",
"issue": "15",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "5180_CR9",
"unstructured": "Garg S, Kim L, Whitaker M et al (2020) Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 – COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 69(15):458–464. https://doi.org/10.15585/mmwr.mm6915e3",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.4683",
"doi-asserted-by": "publisher",
"key": "5180_CR10",
"unstructured": "Onder G, Rezza G, Brusaferro S (2020) Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. https://doi.org/10.1001/jama.2020.4683"
},
{
"DOI": "10.1056/NEJMoa2004500",
"doi-asserted-by": "publisher",
"key": "5180_CR11",
"unstructured": "Bhatraju PK, Ghassemieh BJ, Nichols M et al (2020) Covid-19 in critically ill patients in the Seattle region – case series. N Engl J Med. https://doi.org/10.1056/NEJMoa2004500"
},
{
"DOI": "10.1016/S0140-6736(20)305",
"author": "F Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet",
"key": "5180_CR12",
"unstructured": "Zhou F, Yu T, Du R et al (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054–1062. https://doi.org/10.1016/S0140-6736(20)305",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"doi-asserted-by": "publisher",
"key": "5180_CR13",
"unstructured": "Wu C, Chen X, Cai Y et al (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2020.0994"
},
{
"DOI": "10.1016/j.jcv.2020.104354",
"author": "L Roncon",
"doi-asserted-by": "publisher",
"first-page": "104354",
"journal-title": "J Clin Virol",
"key": "5180_CR14",
"unstructured": "Roncon L, Zuin M, Rigatelli G, Zuliani G (2020) Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol 127:104354. https://doi.org/10.1016/j.jcv.2020.104354",
"volume": "127",
"year": "2020"
},
{
"key": "5180_CR15",
"unstructured": "Centers for Disease Control and Prevention (2020) Coronavirus Disease 2019 (COVID-19): groups at higher risk for severe illness. Available from https://aimvein.com/blogs/news/covid-19-measure-for-high-risk-groups. Accessed 21 April 2020"
},
{
"DOI": "10.1016/j.csda.2005.07.015",
"author": "W Sauerbrei",
"doi-asserted-by": "publisher",
"first-page": "3464",
"issue": "12",
"journal-title": "Comput Stat Data Anal",
"key": "5180_CR16",
"unstructured": "Sauerbrei W, Meier-Hirmer C, Benner A, Royston P (2006) Multivariable regression model building by using fractional polynomials: description of SAS, STATA and R programs. Comput Stat Data Anal 50(12):3464–3485. https://doi.org/10.1016/j.csda.2005.07.015",
"volume": "50",
"year": "2006"
},
{
"DOI": "10.1016/j.diabet.2011.02.001",
"author": "C Pornet",
"doi-asserted-by": "publisher",
"first-page": "152",
"issue": "2",
"journal-title": "Diabetes Metab",
"key": "5180_CR17",
"unstructured": "Pornet C, Bourdel-Marchasson I, Lecomte P et al (2011) Trends in the quality of care for elderly people with type 2 diabetes: the need for improvements in safety and quality (the 2001 and 2007 ENTRED Surveys). Diabetes Metab 37(2):152–161. https://doi.org/10.1016/j.diabet.2011.02.001",
"volume": "37",
"year": "2011"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"author": "X Yang",
"doi-asserted-by": "publisher",
"first-page": "475",
"issue": "5",
"journal-title": "Lancet Respir Med",
"key": "5180_CR18",
"unstructured": "Yang X, Yu Y, Xu J et al (2020) Clinical course and outcomes of critically ill patients with SARS-CoV2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8(5):475–481. https://doi.org/10.1016/S2213-2600(20)30079-5",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6913",
"author": "CDC COVID-19 response team",
"doi-asserted-by": "publisher",
"first-page": "382",
"issue": "13",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "5180_CR19",
"unstructured": "CDC COVID-19 response team (2020) Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 – United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep 69(13):382–386. https://doi.org/10.15585/mmwr.mm6913",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.018",
"author": "I Huang",
"doi-asserted-by": "publisher",
"first-page": "395",
"issue": "4",
"journal-title": "Diabetes Metab Syndr",
"key": "5180_CR20",
"unstructured": "Huang I, Anthonius M, Pranata R (2020) Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia – a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr 14(4):395–403. https://doi.org/10.1016/j.dsx.2020.04.018",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1172/jci.insight.13177",
"author": "J Kulcsar",
"doi-asserted-by": "publisher",
"first-page": "e131774",
"issue": "20",
"journal-title": "JCI Insight",
"key": "5180_CR21",
"unstructured": "Kulcsar J, Coleman CM, Beck SE, Frieman MD (2019) Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection. JCI Insight 4(20):e131774. https://doi.org/10.1172/jci.insight.13177",
"volume": "4",
"year": "2019"
},
{
"DOI": "10.1002/oby.22831",
"doi-asserted-by": "publisher",
"key": "5180_CR22",
"unstructured": "Simonnet A, Chetboun M, Poissy J et al (2020) High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). https://doi.org/10.1002/oby.22831"
},
{
"DOI": "10.1007/s00134-019-05594-1",
"author": "M Schetz",
"doi-asserted-by": "publisher",
"first-page": "757",
"issue": "6",
"journal-title": "Intensive Care Med",
"key": "5180_CR23",
"unstructured": "Schetz M, De Jong A, Deane AM et al (2019) Obesity in the critically ill: a narrative review. Intensive Care Med 45(6):757–769. https://doi.org/10.1007/s00134-019-05594-1",
"volume": "45",
"year": "2019"
},
{
"DOI": "10.1056/NEJMsr2005760",
"author": "M Vaduganathan",
"doi-asserted-by": "publisher",
"first-page": "1653",
"issue": "17",
"journal-title": "N Engl J Med",
"key": "5180_CR24",
"unstructured": "Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD (2020) Renin–angiotensin–aldosterone system inhibitors in patients with COVID-19. N Engl J Med 382(17):1653–1659. https://doi.org/10.1056/NEJMsr2005760",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1210/endrev/bnaa011",
"author": "DJ Drucker",
"doi-asserted-by": "publisher",
"first-page": "bnaa011",
"issue": "3",
"journal-title": "Endocr Rev",
"key": "5180_CR25",
"unstructured": "Drucker DJ (2020) Coronavirus infection and type 2 diabetes shared-pathways with therapeutic implications. Endocr Rev 41(3):bnaa011. https://doi.org/10.1210/endrev/bnaa011",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa011300",
"author": "G Van den Berghe",
"doi-asserted-by": "publisher",
"first-page": "1359",
"issue": "19",
"journal-title": "N Engl J Med",
"key": "5180_CR26",
"unstructured": "Van den Berghe G, Wouters P, Weekers F et al (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345(19):1359–1367. https://doi.org/10.1056/NEJMoa011300",
"volume": "345",
"year": "2001"
},
{
"key": "5180_CR27",
"unstructured": "Fosse-Edorh S, Mandereau-Bruno L, Piffaretti C (2018). Le poids du diabète en France en 2016 Synthèse épidémiologique. Santé publique France:8p; available from https://www.santepubliquefrance.fr/maladies-et-traumatismes/diabete/documents/rapport-synthese/le-poids-du-diabete-en-france-en-2016.-synthese-epidemiologique. Accessed 21 April 2020 [Article in French]"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s00125-020-05180-x"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "63"
}
