Metformin Suppresses SARS-CoV-2 in Cell Culture
et al., bioRxiv, doi:10.1101/2021.11.18.469078, Nov 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
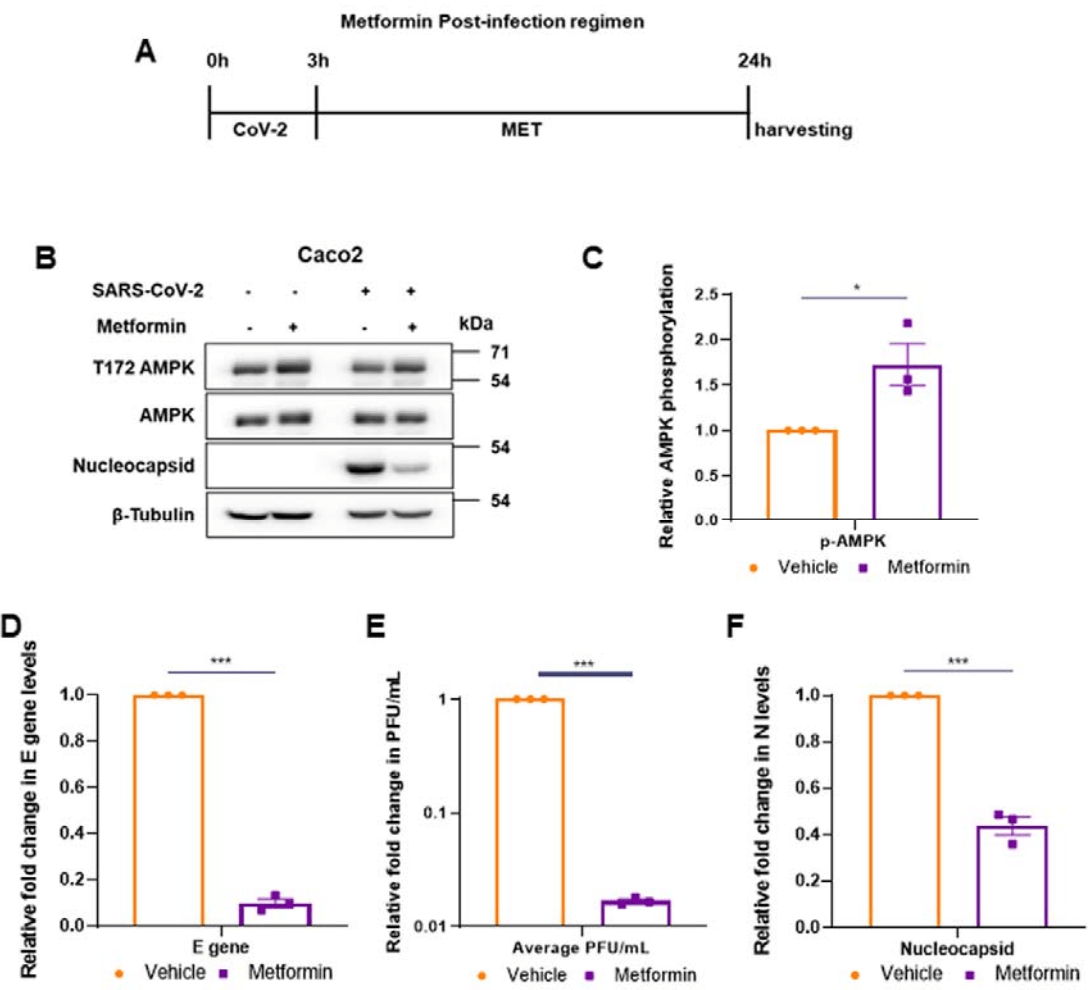
In vitro study showing metformin inhibits SARS-CoV-2 in Caco2 cells. Metformin reduced viral titers by nearly 99%, and by about 90% when cells were treated prior to infection.
18 preclinical studies support the efficacy of metformin for COVID-19:
A systematic review and meta-analysis of 15 non-COVID-19 preclinical studies showed that metformin inhibits pulmonary inflammation and oxidative stress, minimizes lung injury, and improves survival in animal models of acute respiratory distress syndrome (ARDS) or acute lung injury (ALI)15.
Metformin inhibits SARS-CoV-2 in vitro11,12, minimizes LPS-induced cytokine storm in a mouse model14, minimizes lung damage and fibrosis in a mouse model of LPS-induced ARDS10, may protect against SARS-CoV-2-induced neurological disorders9, may be beneficial via inhibitory effects on ORF3a-mediated inflammasome activation16, reduces UUO and FAN-induced kidney fibrosis10, increases mitochondrial function and decreases TGF-β-induced fibrosis, apoptosis, and inflammation markers in lung epithelial cells10, may reduce inflammation, oxidative stress, and thrombosis via regulating glucose metabolism2, attenuates spike protein S1-induced inflammatory response and α-synuclein aggregation8, may protect against COVID-19 cognitive impairment by suppressing HIF-1α stabilization and reducing neurodegenerative protein aggregation13, may reduce COVID-19 severity and long COVID by inhibiting NETosis via suppression of protein kinase C activation17, enhances interferon responses and reduces SARS-CoV-2 infection and inflammation in diabetic models by suppressing HIF-1α signaling7, may improve COVID-19 outcomes by preventing VDAC1 mistargeting to the plasma membrane, reducing ATP loss, and preserving immune cell function during cytokine storm18, reduces hyperglycemia-induced hepatic ACE2/TMPRSS2 up-regulation and SARS-CoV-2 entry6, may reduce COVID-19 severity by suppressing monocyte inflammatory responses and glycolytic activation via AMPK pathway modulation5, and may improve outcomes via modulation of immune responses with increased anti-inflammatory T lymphocyte gene expression and via enhanced gut microbiota diversity19.
1.
Tavares et al., Investigation of Interactions Between the Protein MPro and the Vanadium Complex VO(metf)2∙H2O: A Computational Approach for COVID-19 Treatment, Biophysica, doi:10.3390/biophysica5010004.
2.
Hou et al., Metformin is a potential therapeutic for COVID-19/LUAD by regulating glucose metabolism, Scientific Reports, doi:10.1038/s41598-024-63081-0.
3.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
4.
Lockwood, T., Coordination chemistry suggests that independently observed benefits of metformin and Zn2+ against COVID-19 are not independent, BioMetals, doi:10.1007/s10534-024-00590-5.
5.
Maurmann et al., Immunoregulatory effect of metformin in monocytes exposed to SARS-CoV-2 spike protein subunit 1, bioRxiv, doi:10.1101/2025.09.12.675877.
6.
Rao et al., Pathological Glucose Levels Enhance Entry Factor Expression and Hepatic SARS‐CoV‐2 Infection, Journal of Cellular and Molecular Medicine, doi:10.1111/jcmm.70581.
7.
Joshi et al., Severe SARS‐CoV‐2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α‐IFN axis, Clinical and Translational Medicine, doi:10.1002/ctm2.70275.
8.
Chang et al., SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin, Biomedicines, doi:10.3390/biomedicines12061223.
9.
Yang et al., SARS-CoV-2 infection causes dopaminergic neuron senescence, Cell Stem Cell, doi:10.1016/j.stem.2023.12.012.
10.
Miguel et al., Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney, Redox Biology, doi:10.1016/j.redox.2023.102957.
11.
Ventura-López et al., Treatment with metformin glycinate reduces SARS-CoV-2 viral load: An in vitro model and randomized, double-blind, Phase IIb clinical trial, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113223.
12.
Parthasarathy et al., Metformin Suppresses SARS-CoV-2 in Cell Culture, bioRxiv, doi:10.1101/2021.11.18.469078.
13.
Lee et al., SARS-CoV-2 spike protein causes synaptic dysfunction and p-tau and α-synuclein aggregation leading cognitive impairment: The protective role of metformin, PLOS One, doi:10.1371/journal.pone.0336015.
14.
Taher et al., Anti‑inflammatory effect of metformin against an experimental model of LPS‑induced cytokine storm, Experimental and Therapeutic Medicine, doi:10.3892/etm.2023.12114.
15.
Wang et al., Effects of metformin on acute respiratory distress syndrome in preclinical studies: a systematic review and meta-analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1215307.
16.
Zhang et al., SARS-CoV-2 ORF3a Protein as a Therapeutic Target against COVID-19 and Long-Term Post-Infection Effects, Pathogens, doi:10.3390/pathogens13010075.
17.
Monsalve et al., NETosis: A key player in autoimmunity, COVID-19, and long COVID, Journal of Translational Autoimmunity, doi:10.1016/j.jtauto.2025.100280.
Parthasarathy et al., 19 Nov 2021, preprint, 3 authors.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Metformin Suppresses SARS-CoV-2 in Cell Culture
doi:10.1101/2021.11.18.469078
People with diabetes are reported to have a higher risk of experiencing severe COVID-19 complications. Metformin, a first-line medication for type 2 diabetes, has antiviral properties. Some studies have indicated its prognostic potential in COVID-19. Here, we report that metformin significantly inhibits SARS-CoV-2 growth in cell culture models. SARS-CoV-2 infection of gut epithelial cell line, Caco2, resulted in higher phosphorylation of AMPK. Metformin reduced viral titers in the infected cells by nearly 99%, and by about 90% when cells were treated prior to infection. Metformin pre-treatment resulted in further phosphorylation of AMPK and caused a ten-fold reduction of viral titers indicating its potential in preventing naïve infections. Confirming the positive impact of AMPK activation, another AMPK activator AICAR substantially inhibited of viral titers and, AMPK inhibitor Compound C, augmented it considerably. Metformin treatment post-SARS-CoV-2 infection resulted in nearly hundred-fold reduction of viral titers, indicating that the antiviral potency of the drug is far higher in infected cells, while still being able to reduce fresh infection. Metformin displayed SARS-CoV-2 TCID50 and TCID90 at 3.5 and 8.9 mM, respectively. In conclusion, our study demonstrates that metformin is very effective in limiting the replication of SARS-CoV-2 in cell culture and thus possibly could offer double benefits to diabetic COVID-19 patients by lowering both blood glucose levels and viral load.
AMPK is activated. In this context, it is interesting to note that N protein was detected at modestly higher abundance during pharmacological activation of AMPK unlike the viral RNA and infectious titer, indicating that viral protein translation is not inhibited during the treatments. However, a significant drop in N levels during the postinfection treatment suggested an overall inhibition of viral life-stages concurrent with an overall drop of cellular activities indicated by MTT results. Inhibition of metabolic activities particularly in the infected cells upon post-infection metformin treatment indicated that metformin treatment specifically targeted the infected cells for destruction. This could be viewed as beneficial to the system fighting to clear the virus from it. Although multiple reports show AMPK as the major effector of metformin action, it is now well established that metformin exerts its affects through other pathways such as PKA and FBPase-1 mediated regulation as well (Pernicova & Korbonits, 2014) . Further study into the mechanism SARS-CoV-2 inhibition by metformin could pave the way for it to be a possible therapeutic target for COVID-patients. From a clinical perspective, our study provides some answers to the favorable prognosis of metformin-treated diabetic patients who contracted COVID-19.
Institutional biosafety Institutional biosafety clearance was obtained for the experiments pertaining to SARS-CoV-2.
References
Abu-Farha, Thanaraj, Qaddoumi, Hashem, Abubaker et al., The Role of Lipid Metabolism in COVID-19 Virus Infection and as a Drug Target, International Journal of Molecular Sciences, doi:10.3390/IJMS21103544
Bernal, Andrews, Gower, Gallagher, Simmons et al., Effectiveness of Covid-19 Vaccines against the B, doi:10.1056/NEJMoa2108891
Bhutta, Gallo, Borenstein, Multifaceted Role of AMPK in Viral Infections, Cells, doi:10.3390/CELLS10051118
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, The Lancet Healthy Longevity, doi:10.1016/S2666-7568(20)30033-7
Chen, Guo, Qiu, Zhang, Deng et al., Immunomodulatory and Antiviral Activity of Metformin and Its Potential Implications in Treating Coronavirus Disease 2019 and Lung Injury, Frontiers in Immunology, doi:10.3389/FIMMU.2020.02056
Chen, Yang, Cheng, Chen, Peng et al., Clinical Characteristics and Outcomes of Patients with Diabetes and COVID-19 in Association with Glucose-Lowering Medication, Diabetes Care, doi:10.2337/dc20-0660
Cn, Cd, Jf, Ie, La et al., The antiviral effect of metformin on zika and dengue virus infection, Scientific Reports, doi:10.1038/S41598-021-87707-9
Crouse, Grimes, Li, Might, Ovalle et al., POPULATION WITH COVID-19 AND DIABETES, doi:10.1101/2020.07.29.20164020
Dardano, Del Prato, Metformin: an inexpensive and effective treatment in people with diabetes and COVID-19?, The Lancet Healthy Longevity, doi:10.1016/S2666-7568(20)30047-7
Davidson, Peters, An overview of metformin in the treatment of type 2 diabetes mellitus, American Journal of Medicine, doi:10.1016/S0002-9343(96)00353-1
Dias, Soares, Ferreira, Sacramento, Fintelman-Rodrigues et al., Lipid droplets fuel SARS-CoV-2 replication and production of inflammatory mediators, PLOS Pathogens, doi:10.1371/JOURNAL.PPAT.1009127
Gupta, Parthasarathy, Sah, Tandel, Vedagiri et al., Inactivation of SARS-CoV-2 by β-propiolactone causes aggregation of viral particles and loss of antigenic potential, Virus Research, doi:10.1016/J.VIRUSRES.2021.198555
Herker, Ott, Emerging Role of Lipid Droplets in Host/Pathogen Interactions, Journal of Biological Chemistry, doi:10.1074/JBC.R111.300202
Ibrahim, Lowe, Bramante, Shah, Klatt et al., Metformin and Covid-19: Focused Review of Mechanisms and Current Literature Suggesting Benefit, Frontiers in Endocrinology, doi:10.3389/FENDO.2021.587801
Lui, Tan, Is metformin a miracle or a menace in COVID-19 patients with type 2 diabetes?, Journal of Diabetes Investigation, doi:10.1111/JDI.13484
Marmor, Bramante, Ingraham, Murray, Marmor et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Articles Lancet Healthy Longev, doi:10.1016/S2666-7568(20)30033-7
Pereira-Dutra, Teixeira, Costa, De, Bozza, Fat, fight, and beyond: The multiple roles of lipid droplets in infections and inflammation, Journal of Leukocyte Biology, doi:10.1002/JLB.4MR0119-035R
Pernicova, Korbonits, Metformin-mode of action and clinical implications for diabetes and cancer, Nature Reviews Endocrinology, doi:10.1038/nrendo.2013.256
Rena, Hardie, Pearson, The mechanisms of action of metformin, Diabetologia, doi:10.1007/s00125-017-4342-z
Sanyaolu, Okorie, Marinkovic, Patidar, Younis et al., Comorbidity and its Impact on Patients with COVID-19, Sn Comprehensive Clinical Medicine, doi:10.1007/S42399-020-00363-4
Schneider, Rasband, Eliceiri, NIH Image to ImageJ: 25 years of image analysis, Nature Methods, doi:10.1038/nmeth.2089
Xl, Jl, Hy, Wh, Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis, The American Journal of Tropical Medicine and Hygiene, doi:10.4269/AJTMH.20-0375
Zangiabadian, Nejadghaderi, Zahmatkesh, Hajikhani, Mirsaeidi et al., The Efficacy and Potential Mechanisms of Metformin in the Treatment of COVID-19 in the Diabetics: A Systematic Review, Frontiers in Endocrinology, doi:10.3389/fendo.2021.645194
Zg, Jj, Xj, Mm, Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes, Cell Metabolism, doi:10.1016/J.CMET.2020.04.021
Zhou, Myers, Li, Chen, Shen et al., Role of AMPactivated protein kinase in mechanism of metformin action, The Journal of Clinical Investigation, doi:10.1172/JCI13505
DOI record:
{
"DOI": "10.1101/2021.11.18.469078",
"URL": "http://dx.doi.org/10.1101/2021.11.18.469078",
"abstract": "<jats:p>People with diabetes are reported to have a higher risk of experiencing severe COVID-19 complications. Metformin, a first-line medication for type 2 diabetes, has antiviral properties. Some studies have indicated its prognostic potential in COVID-19. Here, we report that metformin significantly inhibits SARS-CoV-2 growth in cell culture models. SARS-CoV-2 infection of gut epithelial cell line, Caco2, resulted in higher phosphorylation of AMPK. Metformin reduced viral titers in the infected cells by nearly 99%, and by about 90% when cells were treated prior to infection. Metformin pre-treatment resulted in further phosphorylation of AMPK and caused a ten-fold reduction of viral titers indicating its potential in preventing naive infections. Confirming the positive impact of AMPK activation, another AMPK activator AICAR substantially inhibited of viral titers and, AMPK inhibitor Compound C, augmented it considerably. Metformin treatment post-SARS-CoV-2 infection resulted in nearly hundred-fold reduction of viral titers, indicating that the antiviral potency of the drug is far higher in infected cells, while still being able to reduce fresh infection. Metformin displayed SARS-CoV-2 TCID50 and TCID90 at 3.5 and 8.9 mM, respectively. In conclusion, our study demonstrates that metformin is very effective in limiting the replication of SARS-CoV-2 in cell culture and thus possibly could offer double benefits to diabetic COVID-19 patients by lowering both blood glucose levels and viral load.</jats:p>",
"accepted": {
"date-parts": [
[
2021,
11,
19
]
]
},
"author": [
{
"affiliation": [],
"family": "Tandel",
"given": "Dixit",
"sequence": "first"
},
{
"affiliation": [],
"family": "Parthasarathy",
"given": "Haripriya",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6079-7101",
"affiliation": [],
"authenticated-orcid": false,
"family": "Harshan",
"given": "Krishnan Harinivas",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
11,
20
]
],
"date-time": "2021-11-20T04:40:32Z",
"timestamp": 1637383232000
},
"deposited": {
"date-parts": [
[
2021,
11,
20
]
],
"date-time": "2021-11-20T04:40:32Z",
"timestamp": 1637383232000
},
"group-title": "Microbiology",
"indexed": {
"date-parts": [
[
2021,
11,
20
]
],
"date-time": "2021-11-20T05:33:10Z",
"timestamp": 1637386390540
},
"institution": [
{
"name": "bioRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2021,
11,
19
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2021.11.18.469078",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2021,
11,
19
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2021,
11,
19
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [],
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": [
"Metformin Suppresses SARS-CoV-2 in Cell Culture"
],
"type": "posted-content"
}
