Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney
et al., Redox Biology, doi:10.1016/j.redox.2023.102957, Nov 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Mouse models showing reduced lung and kidney injury with metformin. Metformin minimized lung damage and fibrosis in a mouse model of LPS-induced ARDS, and reduced UUO and FAN-induced kidney fibrosis. In vitro study showing that metformin increased mitochondrial function and decreased TGF-β-induced fibrosis, apoptosis, and inflammation markers in lung epithelial cells.
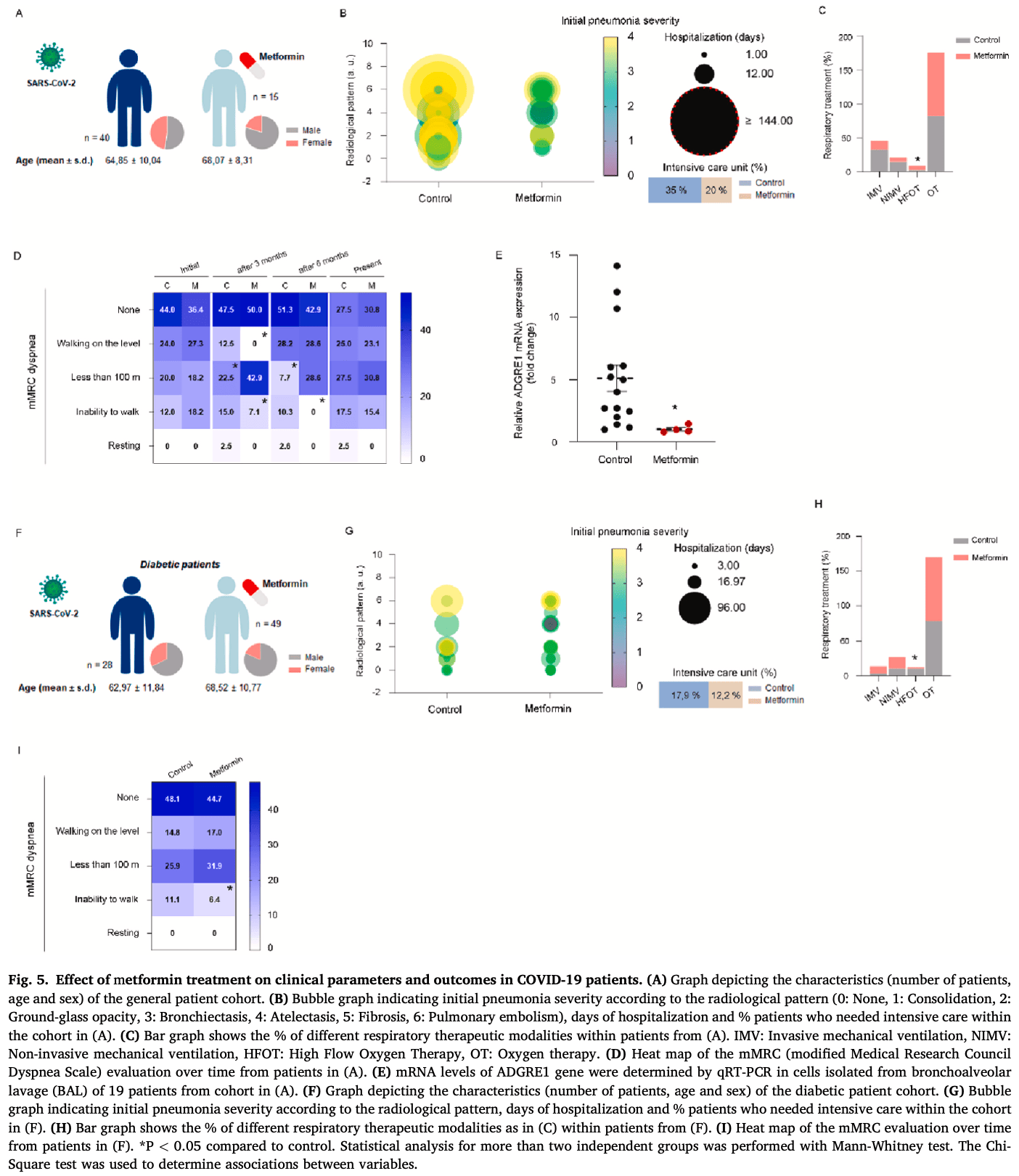
Authors also include a retrospective study showing lower ICU admission with metformin without statistical significance.
18 preclinical studies support the efficacy of metformin for COVID-19:
A systematic review and meta-analysis of 15 non-COVID-19 preclinical studies showed that metformin inhibits pulmonary inflammation and oxidative stress, minimizes lung injury, and improves survival in animal models of acute respiratory distress syndrome (ARDS) or acute lung injury (ALI)15.
Metformin inhibits SARS-CoV-2 in vitro11,12, minimizes LPS-induced cytokine storm in a mouse model14, minimizes lung damage and fibrosis in a mouse model of LPS-induced ARDS10, may protect against SARS-CoV-2-induced neurological disorders9, may be beneficial via inhibitory effects on ORF3a-mediated inflammasome activation16, reduces UUO and FAN-induced kidney fibrosis10, increases mitochondrial function and decreases TGF-β-induced fibrosis, apoptosis, and inflammation markers in lung epithelial cells10, may reduce inflammation, oxidative stress, and thrombosis via regulating glucose metabolism2, attenuates spike protein S1-induced inflammatory response and α-synuclein aggregation8, may protect against COVID-19 cognitive impairment by suppressing HIF-1α stabilization and reducing neurodegenerative protein aggregation13, may reduce COVID-19 severity and long COVID by inhibiting NETosis via suppression of protein kinase C activation17, enhances interferon responses and reduces SARS-CoV-2 infection and inflammation in diabetic models by suppressing HIF-1α signaling7, may improve COVID-19 outcomes by preventing VDAC1 mistargeting to the plasma membrane, reducing ATP loss, and preserving immune cell function during cytokine storm18, reduces hyperglycemia-induced hepatic ACE2/TMPRSS2 up-regulation and SARS-CoV-2 entry6, may reduce COVID-19 severity by suppressing monocyte inflammatory responses and glycolytic activation via AMPK pathway modulation5, and may improve outcomes via modulation of immune responses with increased anti-inflammatory T lymphocyte gene expression and via enhanced gut microbiota diversity19.
|
risk of ICU admission, 37.4% lower, RR 0.63, p = 0.24, treatment 64, control 68, both cohorts combined.
|
|
risk of ICU admission, 42.9% lower, RR 0.57, p = 0.34, treatment 3 of 15 (20.0%), control 14 of 40 (35.0%), NNT 6.7.
|
|
risk of ICU admission, 31.4% lower, RR 0.69, p = 0.52, treatment 6 of 49 (12.2%), control 5 of 28 (17.9%), NNT 18.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Tavares et al., Investigation of Interactions Between the Protein MPro and the Vanadium Complex VO(metf)2∙H2O: A Computational Approach for COVID-19 Treatment, Biophysica, doi:10.3390/biophysica5010004.
2.
Hou et al., Metformin is a potential therapeutic for COVID-19/LUAD by regulating glucose metabolism, Scientific Reports, doi:10.1038/s41598-024-63081-0.
3.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
4.
Lockwood, T., Coordination chemistry suggests that independently observed benefits of metformin and Zn2+ against COVID-19 are not independent, BioMetals, doi:10.1007/s10534-024-00590-5.
5.
Maurmann et al., Immunoregulatory effect of metformin in monocytes exposed to SARS-CoV-2 spike protein subunit 1, bioRxiv, doi:10.1101/2025.09.12.675877.
6.
Rao et al., Pathological Glucose Levels Enhance Entry Factor Expression and Hepatic SARS‐CoV‐2 Infection, Journal of Cellular and Molecular Medicine, doi:10.1111/jcmm.70581.
7.
Joshi et al., Severe SARS‐CoV‐2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α‐IFN axis, Clinical and Translational Medicine, doi:10.1002/ctm2.70275.
8.
Chang et al., SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin, Biomedicines, doi:10.3390/biomedicines12061223.
9.
Yang et al., SARS-CoV-2 infection causes dopaminergic neuron senescence, Cell Stem Cell, doi:10.1016/j.stem.2023.12.012.
10.
Miguel et al., Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney, Redox Biology, doi:10.1016/j.redox.2023.102957.
11.
Ventura-López et al., Treatment with metformin glycinate reduces SARS-CoV-2 viral load: An in vitro model and randomized, double-blind, Phase IIb clinical trial, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113223.
12.
Parthasarathy et al., Metformin Suppresses SARS-CoV-2 in Cell Culture, bioRxiv, doi:10.1101/2021.11.18.469078.
13.
Lee et al., SARS-CoV-2 spike protein causes synaptic dysfunction and p-tau and α-synuclein aggregation leading cognitive impairment: The protective role of metformin, PLOS One, doi:10.1371/journal.pone.0336015.
14.
Taher et al., Anti‑inflammatory effect of metformin against an experimental model of LPS‑induced cytokine storm, Experimental and Therapeutic Medicine, doi:10.3892/etm.2023.12114.
15.
Wang et al., Effects of metformin on acute respiratory distress syndrome in preclinical studies: a systematic review and meta-analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1215307.
16.
Zhang et al., SARS-CoV-2 ORF3a Protein as a Therapeutic Target against COVID-19 and Long-Term Post-Infection Effects, Pathogens, doi:10.3390/pathogens13010075.
17.
Monsalve et al., NETosis: A key player in autoimmunity, COVID-19, and long COVID, Journal of Translational Autoimmunity, doi:10.1016/j.jtauto.2025.100280.
Miguel et al., 17 Nov 2023, retrospective, Spain, peer-reviewed, 19 authors, study period March 2020 - June 2020.
Contact: veronica.miguel@cnic.es, slamas@cbm.csic.es.
Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney
Redox Biology, doi:10.1016/j.redox.2023.102957
Progressive respiratory failure is the primary cause of death in the coronavirus disease 2019 (COVID-19) pandemic. It is the final outcome of the acute respiratory distress syndrome (ARDS), characterized by an initial exacerbated inflammatory response, metabolic derangement and ultimate tissue scarring. A positive balance of cellular energy may result crucial for the recovery of clinical COVID-19. Hence, we asked if two key pathways involved in cellular energy generation, AMP-activated protein kinase (AMPK)/acetyl-CoA carboxylase (ACC) signaling and fatty acid oxidation (FAO) could be beneficial. We tested the drugs metformin (AMPK activator) and baicalin (CPT1A activator) in different experimental models mimicking COVID-19 associated inflammation in lung and kidney. We also studied two different cohorts of COVID-19 patients that had been previously treated with metformin. These drugs ameliorated lung damage in an ARDS animal model, while activation of AMPK/ ACC signaling increased mitochondrial function and decreased TGF-β-induced fibrosis, apoptosis and inflammation markers in lung epithelial cells. Similar results were observed with two indole derivatives, IND6 and IND8 with AMPK activating capacity. Consistently, a reduced time of hospitalization and need of intensive care was observed in COVID-19 patients previously exposed to metformin. Baicalin also mitigated the activation of pro-inflammatory bone marrow-derived macrophages (BMDMs) and reduced kidney fibrosis in two animal models of kidney injury, another key target of COVID-19. In human epithelial lung and kidney cells, both drugs improved mitochondrial function and prevented TGF-β-induced renal epithelial cell dedifferentiation. Our results support that favoring cellular energy production through enhanced FAO may prove useful in the prevention of COVID-19-induced lung and renal damage.
Author contributions SL conceived and directed research. VM designed, performed and analyzed the majority of experiments. CRS, JT, BS, EA, IR and LF performed experiments. JIH provided technical assistance for mouse experiments. CC performed histological evaluation. KCR, JJ, RK and DS provided intellectual insight and resources. LS and JMRGM collected information about COVID-19 patient cohorts. JN and IC performed bioinformatic studies. AC provided indol-based compounds. All authors helped with the discussion of the results and SL and VM wrote the manuscript.
Declaration of competing interest The authors have no conflicts of interest.
Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi. org/10.1016/j.redox.2023.102957.
References
Ayres, A metabolic handbook for the COVID-19 pandemic, Nat. Metab
Berber, Sumbria, Kokkaya, A metabolic blueprint of COVID-19 and longterm vaccine efficacy, Drug Metab Pers Ther
Berlin, Gulick, Martinez, Severe covid-19, N. Engl. J. Med
Bramante, Buse, Liebovitz, Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial, Lancet Infect. Dis
Carling, AMPK signalling in health and disease, Curr. Opin. Cell Biol
Chevalier, Forbes, Thornhill, Ureteral obstruction as a model of renal interstitial fibrosis and obstructive nephropathy, Kidney Int
Console, Scalise, Giangregorio, The link between the mitochondrial fatty acid oxidation derangement and kidney injury, Front. Physiol
Cui, Xie, Banerjee, Impairment of fatty acid oxidation in alveolar epithelial cells mediates acute lung injury, Am. J. Respir. Cell Mol. Biol
Dai, Liang, Zhao, Chemoproteomics reveals baicalin activates hepatic CPT1 to ameliorate diet-induced obesity and hepatic steatosis, Proc. Natl. Acad. Sci. U. S. A
De Boer, Petrache, Goldstein, Decreased fatty acid oxidation and altered lactate production during exercise in patients with post-acute COVID-19 syndrome, Am. J. Respir. Crit. Care Med
Erickson, Fenno, Barzilai, Metformin for treatment of acute COVID-19: systematic review of clinical trial data against SARS-CoV-2, Diabetes Care
Fajgenbaum, June, Cytokine storm, N. Engl. J. Med
Fink, Henry, Tange, Experimental folic acid nephropathy, Pathology
Foretz, Guigas, Bertrand, Metformin: from mechanisms of action to therapies, Cell Metabol
Grant, Morales-Nebreda, Markov, Circuits between infected macrophages and T cells in SARS-CoV-2 pneumonia, Nature
He, Wondisford, Metformin action: concentrations matter, Cell Metabol
Huynh, Green, Koves, Measurement of fatty acid oxidation rates in animal tissues and cell lines, Methods Enzymol
Jackson, Farzan, Chen, Mechanisms of SARS-CoV-2 entry into cells, Nat. Rev. Mol. Cell Biol
Jansen, Reimer, Nagai, SARS-CoV-2 infects the human kidney and drives fibrosis in kidney organoids, Cell Stem Cell
Jung, Park, Huh, The effect of human adipose-derived stem cells on lipopolysaccharide-induced acute respiratory distress syndrome in mice, Ann. Transl. Med
Kang, Ahn, Choi, Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development, Nat. Med
Kheirollahi, Wasnick, Biasin, Metformin induces lipogenic differentiation in myofibroblasts to reverse lung fibrosis, Nat. Commun
Kulkarni, Gubbi, Barzilai, Benefits of metformin in attenuating the hallmarks of aging, Cell Metabol
Lee, Su, Baloni, Integrated analysis of plasma and single immune cells uncovers metabolic changes in individuals with COVID-19, Nat. Biotechnol
Li, Yang, Yan, Metformin in patients with COVID-19: a systematic review and meta-analysis, Front. Med
Lin, Tsai, Hsu, Study of baicalin toward COVID-19 treatment: in silico target analysis and in vitro inhibitory effects on SARS-CoV-2 proteases, Biomed. Hub
Livak, Schmittgen, Analysis of relative gene expression data using realtime quantitative PCR and the 2(-Delta Delta C(T)) Method, Methods
Ma, Tian, Zhang, Low-dose metformin targets the lysosomal AMPK pathway through PEN2, Nature
Matheson, Lehner, How does SARS-CoV-2 cause COVID-19?, Science
Merad, Blish, Sallusto, The immunology and immunopathology of COVID-19, Science
Miguel, Tituana, Herrero, Renal tubule Cpt1a overexpression protects from kidney fibrosis by restoring mitochondrial homeostasis, J. Clin. Invest
Moolamalla, Balasubramanian, Chauhan, Host metabolic reprogramming in response to SARS-CoV-2 infection: a systems biology approach, Microb. Pathog
Mora, Bueno, Rojas, Mitochondria in the spotlight of aging and idiopathic pulmonary fibrosis, J. Clin. Invest
Pernicova, Korbonits, Metformin-mode of action and clinical implications for diabetes and cancer, Nat. Rev. Endocrinol
Prasun, COVID-19: a mitochondrial perspective, DNA Cell Biol
Price, Miguel, Ding, Genetic deficiency or pharmacological inhibition of miR-33 protects from kidney fibrosis, JCI Insight
Rangarajan, Bone, Zmijewska, Metformin reverses established lung fibrosis in a bleomycin model, Nat. Med
Ravi, Chacko, Kramer, Defining the effects of storage on platelet bioenergetics: the role of increased proton leak, Biochim. Biophys. Acta
Reddel, Ke, Gerwin, Transformation of human bronchial epithelial cells by infection with SV40 or adenovirus-12 SV40 hybrid virus, or transfection via strontium phosphate coprecipitation with a plasmid containing SV40 early region genes, Cancer Res
Rena, Hardie, Pearson, The mechanisms of action of metformin, Diabetologia
Roberts, Muelas, Taylor, Untargeted metabolomics of COVID-19 patient serum reveals potential prognostic markers of both severity and outcome, Metabolomics
Sanchez-Cerrillo, Landete, Aldave, COVID-19 severity associates with pulmonary redistribution of CD1c+ DCs and inflammatory transitional and nonclassical monocytes, J. Clin. Invest
Sanz-Gomez, Aledavood, Beroiz-Salaverri, Novel indolic AMPK modulators induce vasodilatation through activation of the AMPK-eNOS-NO pathway, Sci. Rep
Saz-Leal, Del Fresno, Brandi, Targeting SHIP-1 in myeloid cells enhances trained immunity and boosts response to infection, Cell Rep
Tanner, Alfieri, The fatty acid lipid metabolism nexus in COVID-19, Viruses
Thomas, Stefanoni, Reisz, COVID-19 infection alters kynurenine and fatty acid metabolism, correlating with IL-6 levels and renal status, JCI Insight
Thompson, Chambers, Liu, Acute respiratory distress syndrome, N. Engl. J. Med
Tian, Xiong, Liu, Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies, Mod. Pathol
Valdes, Moreno, Rello, Metabolomics study of COVID-19 patients in four different clinical stages, Sci. Rep
Van Der Windt, Chang, Pearce, Measuring bioenergetics in T cells using a Seahorse extracellular Flux analyzer, Curr. Protoc. Im
Varga, Brenner, Phan, Fibrosis Research: Methods and Protocols
Vernooy, Dentener, Van Suylen, Long-term intratracheal lipopolysaccharide exposure in mice results in chronic lung inflammation and persistent pathology, Am. J. Respir. Cell Mol. Biol
Wang, An, Liu, Metformin improves mitochondrial respiratory activity through activation of AMPK, Cell Rep
Wang, Jiang, Zhang, Baicalin protects against renal interstitial fibrosis in mice by inhibiting the TGF-beta/Smad signalling pathway, Pharm. Biol
Wang, Tang, Liu, The role of IL-6 in coronavirus, especially in COVID-19, Front. Pharmacol
Wiernsperger, Al-Salameh, Cariou, Protection by metformin against severe Covid-19: an in-depth mechanistic analysis, Diabetes Metab
Zhou, Myers, Li, Role of AMP-activated protein kinase in mechanism of metformin action, J. Clin. Invest
DOI record:
{
"DOI": "10.1016/j.redox.2023.102957",
"ISSN": [
"2213-2317"
],
"URL": "http://dx.doi.org/10.1016/j.redox.2023.102957",
"alternative-id": [
"S2213231723003580"
],
"article-number": "102957",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Redox Biology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.redox.2023.102957"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Authors. Published by Elsevier B.V."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-9863-0710",
"affiliation": [],
"authenticated-orcid": false,
"family": "Miguel",
"given": "Verónica",
"sequence": "first"
},
{
"affiliation": [],
"family": "Rey-Serra",
"given": "Carlos",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tituaña",
"given": "Jessica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sirera",
"given": "Belén",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alcalde-Estévez",
"given": "Elena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Herrero",
"given": "J. Ignacio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ranz",
"given": "Irene",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fernández",
"given": "Laura",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Castillo",
"given": "Carolina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sevilla",
"given": "Lucía",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nagai",
"given": "James",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reimer",
"given": "Katharina C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jansen",
"given": "Jitske",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kramann",
"given": "Rafael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Costa",
"given": "Ivan G.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Castro",
"given": "Ana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sancho",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rodríguez González-Moro",
"given": "José Miguel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5166-4155",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lamas",
"given": "Santiago",
"sequence": "additional"
}
],
"container-title": "Redox Biology",
"container-title-short": "Redox Biology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
11,
3
]
],
"date-time": "2023-11-03T13:44:50Z",
"timestamp": 1699019090000
},
"deposited": {
"date-parts": [
[
2023,
12,
13
]
],
"date-time": "2023-12-13T15:22:17Z",
"timestamp": 1702480937000
},
"indexed": {
"date-parts": [
[
2023,
12,
14
]
],
"date-time": "2023-12-14T00:46:58Z",
"timestamp": 1702514818593
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
12
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
12,
1
]
],
"date-time": "2023-12-01T00:00:00Z",
"timestamp": 1701388800000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
11,
2
]
],
"date-time": "2023-11-02T00:00:00Z",
"timestamp": 1698883200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2213231723003580?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2213231723003580?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "102957",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
12
]
]
},
"published-print": {
"date-parts": [
[
2023,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1038/s41580-021-00418-x",
"article-title": "Mechanisms of SARS-CoV-2 entry into cells",
"author": "Jackson",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Nat. Rev. Mol. Cell Biol.",
"key": "10.1016/j.redox.2023.102957_bib1",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1056/NEJMcp2009575",
"article-title": "Severe covid-19",
"author": "Berlin",
"doi-asserted-by": "crossref",
"first-page": "2451",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.redox.2023.102957_bib2",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1126/science.abc6156",
"article-title": "How does SARS-CoV-2 cause COVID-19?",
"author": "Matheson",
"doi-asserted-by": "crossref",
"first-page": "510",
"journal-title": "Science",
"key": "10.1016/j.redox.2023.102957_bib3",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1056/NEJMra2026131",
"article-title": "Cytokine storm",
"author": "Fajgenbaum",
"doi-asserted-by": "crossref",
"first-page": "2255",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.redox.2023.102957_bib4",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1038/s42255-020-0237-2",
"article-title": "A metabolic handbook for the COVID-19 pandemic",
"author": "Ayres",
"doi-asserted-by": "crossref",
"first-page": "572",
"journal-title": "Nat. Metab.",
"key": "10.1016/j.redox.2023.102957_bib5",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1038/nrendo.2013.256",
"article-title": "Metformin--mode of action and clinical implications for diabetes and cancer",
"author": "Pernicova",
"doi-asserted-by": "crossref",
"first-page": "143",
"journal-title": "Nat. Rev. Endocrinol.",
"key": "10.1016/j.redox.2023.102957_bib6",
"volume": "10",
"year": "2014"
},
{
"DOI": "10.1073/pnas.1801745115",
"article-title": "Chemoproteomics reveals baicalin activates hepatic CPT1 to ameliorate diet-induced obesity and hepatic steatosis",
"author": "Dai",
"doi-asserted-by": "crossref",
"first-page": "E5896",
"journal-title": "Proc. Natl. Acad. Sci. U. S. A.",
"key": "10.1016/j.redox.2023.102957_bib7",
"volume": "115",
"year": "2018"
},
{
"article-title": "Transformation of human bronchial epithelial cells by infection with SV40 or adenovirus-12 SV40 hybrid virus, or transfection via strontium phosphate coprecipitation with a plasmid containing SV40 early region genes",
"author": "Reddel",
"first-page": "1904",
"journal-title": "Cancer Res.",
"key": "10.1016/j.redox.2023.102957_bib8",
"volume": "48",
"year": "1988"
},
{
"DOI": "10.1172/JCI13505",
"article-title": "Role of AMP-activated protein kinase in mechanism of metformin action",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1167",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.redox.2023.102957_bib9",
"volume": "108",
"year": "2001"
},
{
"DOI": "10.1038/s41598-022-07077-8",
"article-title": "Novel indolic AMPK modulators induce vasodilatation through activation of the AMPK-eNOS-NO pathway",
"author": "Sanz-Gomez",
"doi-asserted-by": "crossref",
"first-page": "4225",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.redox.2023.102957_bib10",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1056/NEJMra1608077",
"article-title": "Acute respiratory distress syndrome",
"author": "Thompson",
"doi-asserted-by": "crossref",
"first-page": "562",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.redox.2023.102957_bib11",
"volume": "377",
"year": "2017"
},
{
"DOI": "10.1038/s41586-020-03148-w",
"article-title": "Circuits between infected macrophages and T cells in SARS-CoV-2 pneumonia",
"author": "Grant",
"doi-asserted-by": "crossref",
"first-page": "635",
"journal-title": "Nature",
"key": "10.1016/j.redox.2023.102957_bib12",
"volume": "590",
"year": "2021"
},
{
"DOI": "10.1016/j.stem.2021.12.010",
"article-title": "SARS-CoV-2 infects the human kidney and drives fibrosis in kidney organoids",
"author": "Jansen",
"doi-asserted-by": "crossref",
"first-page": "217",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.redox.2023.102957_bib13",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1172/JCI140695",
"article-title": "Renal tubule Cpt1a overexpression protects from kidney fibrosis by restoring mitochondrial homeostasis",
"author": "Miguel",
"doi-asserted-by": "crossref",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.redox.2023.102957_bib14",
"volume": "131",
"year": "2021"
},
{
"DOI": "10.1172/jci.insight.131102",
"article-title": "Genetic deficiency or pharmacological inhibition of miR-33 protects from kidney fibrosis",
"author": "Price",
"doi-asserted-by": "crossref",
"journal-title": "JCI Insight",
"key": "10.1016/j.redox.2023.102957_bib15",
"volume": "4",
"year": "2019"
},
{
"DOI": "10.1126/science.abm8108",
"article-title": "The immunology and immunopathology of COVID-19",
"author": "Merad",
"doi-asserted-by": "crossref",
"first-page": "1122",
"journal-title": "Science",
"key": "10.1016/j.redox.2023.102957_bib16",
"volume": "375",
"year": "2022"
},
{
"DOI": "10.1038/s41587-021-01020-4",
"article-title": "Integrated analysis of plasma and single immune cells uncovers metabolic changes in individuals with COVID-19",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "110",
"journal-title": "Nat. Biotechnol.",
"key": "10.1016/j.redox.2023.102957_bib17",
"volume": "40",
"year": "2022"
},
{
"DOI": "10.1515/dmpt-2022-0148",
"article-title": "A metabolic blueprint of COVID-19 and long-term vaccine efficacy",
"author": "Berber",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Drug Metab Pers Ther",
"key": "10.1016/j.redox.2023.102957_bib18",
"volume": "38",
"year": "2023"
},
{
"DOI": "10.1089/dna.2020.6453",
"article-title": "COVID-19: a mitochondrial perspective",
"author": "Prasun",
"doi-asserted-by": "crossref",
"first-page": "713",
"journal-title": "DNA Cell Biol.",
"key": "10.1016/j.redox.2023.102957_bib19",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1172/JCI87440",
"article-title": "Mitochondria in the spotlight of aging and idiopathic pulmonary fibrosis",
"author": "Mora",
"doi-asserted-by": "crossref",
"first-page": "405",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.redox.2023.102957_bib20",
"volume": "127",
"year": "2017"
},
{
"DOI": "10.1016/j.cmet.2020.04.001",
"article-title": "Benefits of metformin in attenuating the hallmarks of aging",
"author": "Kulkarni",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Cell Metabol.",
"key": "10.1016/j.redox.2023.102957_bib21",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1007/s00125-017-4342-z",
"article-title": "The mechanisms of action of metformin",
"author": "Rena",
"doi-asserted-by": "crossref",
"first-page": "1577",
"journal-title": "Diabetologia",
"key": "10.1016/j.redox.2023.102957_bib22",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.1016/j.cmet.2014.09.018",
"article-title": "Metformin: from mechanisms of action to therapies",
"author": "Foretz",
"doi-asserted-by": "crossref",
"first-page": "953",
"journal-title": "Cell Metabol.",
"key": "10.1016/j.redox.2023.102957_bib23",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1038/s41586-022-04431-8",
"article-title": "Low-dose metformin targets the lysosomal AMPK pathway through PEN2",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "159",
"journal-title": "Nature",
"key": "10.1016/j.redox.2023.102957_bib24",
"volume": "603",
"year": "2022"
},
{
"DOI": "10.1016/j.ceb.2017.01.005",
"article-title": "AMPK signalling in health and disease",
"author": "Carling",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Curr. Opin. Cell Biol.",
"key": "10.1016/j.redox.2023.102957_bib25",
"volume": "45",
"year": "2017"
},
{
"article-title": "Metformin in patients with COVID-19: a systematic review and meta-analysis",
"author": "Li",
"journal-title": "Front. Med.",
"key": "10.1016/j.redox.2023.102957_bib26",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(23)00299-2",
"article-title": "Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "1119",
"journal-title": "Lancet Infect. Dis.",
"key": "10.1016/j.redox.2023.102957_bib27",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.2337/dc22-2539",
"article-title": "Metformin for treatment of acute COVID-19: systematic review of clinical trial data against SARS-CoV-2",
"author": "Erickson",
"doi-asserted-by": "crossref",
"first-page": "1432",
"journal-title": "Diabetes Care",
"key": "10.1016/j.redox.2023.102957_bib28",
"volume": "46",
"year": "2023"
},
{
"DOI": "10.1172/JCI140335",
"article-title": "COVID-19 severity associates with pulmonary redistribution of CD1c+ DCs and inflammatory transitional and nonclassical monocytes",
"author": "Sanchez-Cerrillo",
"doi-asserted-by": "crossref",
"first-page": "6290",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.redox.2023.102957_bib29",
"volume": "130",
"year": "2020"
},
{
"article-title": "The role of IL-6 in coronavirus, especially in COVID-19",
"author": "Wang",
"journal-title": "Front. Pharmacol.",
"key": "10.1016/j.redox.2023.102957_bib30",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1172/jci.insight.140327",
"article-title": "COVID-19 infection alters kynurenine and fatty acid metabolism, correlating with IL-6 levels and renal status",
"author": "Thomas",
"doi-asserted-by": "crossref",
"journal-title": "JCI Insight",
"key": "10.1016/j.redox.2023.102957_bib31",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2022.101359",
"article-title": "Protection by metformin against severe Covid-19: an in-depth mechanistic analysis",
"author": "Wiernsperger",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes Metab.",
"key": "10.1016/j.redox.2023.102957_bib32",
"volume": "48",
"year": "2022"
},
{
"DOI": "10.1038/s41591-018-0087-6",
"article-title": "Metformin reverses established lung fibrosis in a bleomycin model",
"author": "Rangarajan",
"doi-asserted-by": "crossref",
"first-page": "1121",
"journal-title": "Nat. Med.",
"key": "10.1016/j.redox.2023.102957_bib33",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.1038/s41467-019-10839-0",
"article-title": "Metformin induces lipogenic differentiation in myofibroblasts to reverse lung fibrosis",
"author": "Kheirollahi",
"doi-asserted-by": "crossref",
"first-page": "2987",
"journal-title": "Nat. Commun.",
"key": "10.1016/j.redox.2023.102957_bib34",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1016/j.celrep.2019.09.070",
"article-title": "Metformin improves mitochondrial respiratory activity through activation of AMPK",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1511",
"journal-title": "Cell Rep.",
"key": "10.1016/j.redox.2023.102957_bib35",
"volume": "29",
"year": "2019"
},
{
"DOI": "10.1016/j.cmet.2015.01.003",
"article-title": "Metformin action: concentrations matter",
"author": "He",
"doi-asserted-by": "crossref",
"first-page": "159",
"journal-title": "Cell Metabol.",
"key": "10.1016/j.redox.2023.102957_bib36",
"volume": "21",
"year": "2015"
},
{
"DOI": "10.3389/fphys.2020.00794",
"article-title": "The link between the mitochondrial fatty acid oxidation derangement and kidney injury",
"author": "Console",
"doi-asserted-by": "crossref",
"first-page": "794",
"journal-title": "Front. Physiol.",
"key": "10.1016/j.redox.2023.102957_bib37",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1165/rcmb.2018-0152OC",
"article-title": "Impairment of fatty acid oxidation in alveolar epithelial cells mediates acute lung injury",
"author": "Cui",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "Am. J. Respir. Cell Mol. Biol.",
"key": "10.1016/j.redox.2023.102957_bib38",
"volume": "60",
"year": "2019"
},
{
"DOI": "10.1038/nm.3762",
"article-title": "Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development",
"author": "Kang",
"doi-asserted-by": "crossref",
"first-page": "37",
"journal-title": "Nat. Med.",
"key": "10.1016/j.redox.2023.102957_bib39",
"volume": "21",
"year": "2015"
},
{
"DOI": "10.1080/13880209.2022.2097700",
"article-title": "Baicalin protects against renal interstitial fibrosis in mice by inhibiting the TGF-beta/Smad signalling pathway",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1407",
"journal-title": "Pharm. Biol.",
"key": "10.1016/j.redox.2023.102957_bib40",
"volume": "60",
"year": "2022"
},
{
"DOI": "10.1164/rccm.202108-1903LE",
"article-title": "Decreased fatty acid oxidation and altered lactate production during exercise in patients with post-acute COVID-19 syndrome",
"author": "de Boer",
"doi-asserted-by": "crossref",
"first-page": "126",
"journal-title": "Am. J. Respir. Crit. Care Med.",
"key": "10.1016/j.redox.2023.102957_bib41",
"volume": "205",
"year": "2022"
},
{
"DOI": "10.1016/j.micpath.2021.105114",
"article-title": "Host metabolic reprogramming in response to SARS-CoV-2 infection: a systems biology approach",
"author": "Moolamalla",
"doi-asserted-by": "crossref",
"journal-title": "Microb. Pathog.",
"key": "10.1016/j.redox.2023.102957_bib42",
"volume": "158",
"year": "2021"
},
{
"DOI": "10.1038/s41598-022-05667-0",
"article-title": "Metabolomics study of COVID-19 patients in four different clinical stages",
"author": "Valdes",
"doi-asserted-by": "crossref",
"first-page": "1650",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.redox.2023.102957_bib43",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1007/s11306-021-01859-3",
"article-title": "Untargeted metabolomics of COVID-19 patient serum reveals potential prognostic markers of both severity and outcome",
"author": "Roberts",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Metabolomics",
"key": "10.1016/j.redox.2023.102957_bib44",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.3390/v13010090",
"article-title": "The fatty acid lipid metabolism nexus in COVID-19",
"author": "Tanner",
"doi-asserted-by": "crossref",
"journal-title": "Viruses",
"key": "10.1016/j.redox.2023.102957_bib45",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1159/000519564",
"article-title": "Study of baicalin toward COVID-19 treatment: in silico target analysis and in vitro inhibitory effects on SARS-CoV-2 proteases",
"author": "Lin",
"doi-asserted-by": "crossref",
"first-page": "122",
"journal-title": "Biomed. Hub",
"key": "10.1016/j.redox.2023.102957_bib46",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1165/ajrcmb.26.1.4652",
"article-title": "Long-term intratracheal lipopolysaccharide exposure in mice results in chronic lung inflammation and persistent pathology",
"author": "Vernooy",
"doi-asserted-by": "crossref",
"first-page": "152",
"journal-title": "Am. J. Respir. Cell Mol. Biol.",
"key": "10.1016/j.redox.2023.102957_bib47",
"volume": "26",
"year": "2002"
},
{
"DOI": "10.21037/atm.2019.10.48",
"article-title": "The effect of human adipose-derived stem cells on lipopolysaccharide-induced acute respiratory distress syndrome in mice",
"author": "Jung",
"doi-asserted-by": "crossref",
"first-page": "674",
"journal-title": "Ann. Transl. Med.",
"key": "10.1016/j.redox.2023.102957_bib48",
"volume": "7",
"year": "2019"
},
{
"DOI": "10.1038/ki.2009.86",
"article-title": "Ureteral obstruction as a model of renal interstitial fibrosis and obstructive nephropathy",
"author": "Chevalier",
"doi-asserted-by": "crossref",
"first-page": "1145",
"journal-title": "Kidney Int.",
"key": "10.1016/j.redox.2023.102957_bib49",
"volume": "75",
"year": "2009"
},
{
"DOI": "10.3109/00313028709077125",
"article-title": "Experimental folic acid nephropathy",
"author": "Fink",
"doi-asserted-by": "crossref",
"first-page": "143",
"journal-title": "Pathology",
"key": "10.1016/j.redox.2023.102957_bib50",
"volume": "19",
"year": "1987"
},
{
"DOI": "10.1016/j.celrep.2018.09.092",
"article-title": "Targeting SHIP-1 in myeloid cells enhances trained immunity and boosts response to infection",
"author": "Saz-Leal",
"doi-asserted-by": "crossref",
"first-page": "1118",
"journal-title": "Cell Rep.",
"key": "10.1016/j.redox.2023.102957_bib51",
"volume": "25",
"year": "2018"
},
{
"DOI": "10.1006/meth.2001.1262",
"article-title": "Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method",
"author": "Livak",
"doi-asserted-by": "crossref",
"first-page": "402",
"journal-title": "Methods",
"key": "10.1016/j.redox.2023.102957_bib52",
"volume": "25",
"year": "2001"
},
{
"DOI": "10.1016/B978-0-12-416618-9.00020-0",
"article-title": "Measurement of fatty acid oxidation rates in animal tissues and cell lines",
"author": "Huynh",
"doi-asserted-by": "crossref",
"first-page": "391",
"journal-title": "Methods Enzymol.",
"key": "10.1016/j.redox.2023.102957_bib53",
"volume": "542",
"year": "2014"
},
{
"article-title": "Measuring bioenergetics in T cells using a Seahorse extracellular Flux analyzer",
"author": "van der Windt",
"first-page": "3 16B 1",
"journal-title": "Curr. Protoc. Im.",
"key": "10.1016/j.redox.2023.102957_bib54",
"volume": "113",
"year": "2016"
},
{
"DOI": "10.1016/j.bbadis.2015.08.026",
"article-title": "Defining the effects of storage on platelet bioenergetics: the role of increased proton leak",
"author": "Ravi",
"doi-asserted-by": "crossref",
"first-page": "2525",
"journal-title": "Biochim. Biophys. Acta",
"key": "10.1016/j.redox.2023.102957_bib55",
"volume": "1852",
"year": "2015"
},
{
"author": "Varga",
"key": "10.1016/j.redox.2023.102957_bib56",
"series-title": "Fibrosis Research: Methods and Protocols",
"year": "2008"
},
{
"DOI": "10.1038/s41379-020-0536-x",
"article-title": "Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies",
"author": "Tian",
"doi-asserted-by": "crossref",
"first-page": "1007",
"journal-title": "Mod. Pathol.",
"key": "10.1016/j.redox.2023.102957_bib57",
"volume": "33",
"year": "2020"
}
],
"reference-count": 57,
"references-count": 57,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2213231723003580"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Organic Chemistry",
"Biochemistry",
"Clinical Biochemistry"
],
"subtitle": [],
"title": "Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "68"
}
