Severe SARS‐CoV‐2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α‐IFN axis
et al., Clinical and Translational Medicine, doi:10.1002/ctm2.70275, Apr 2025
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
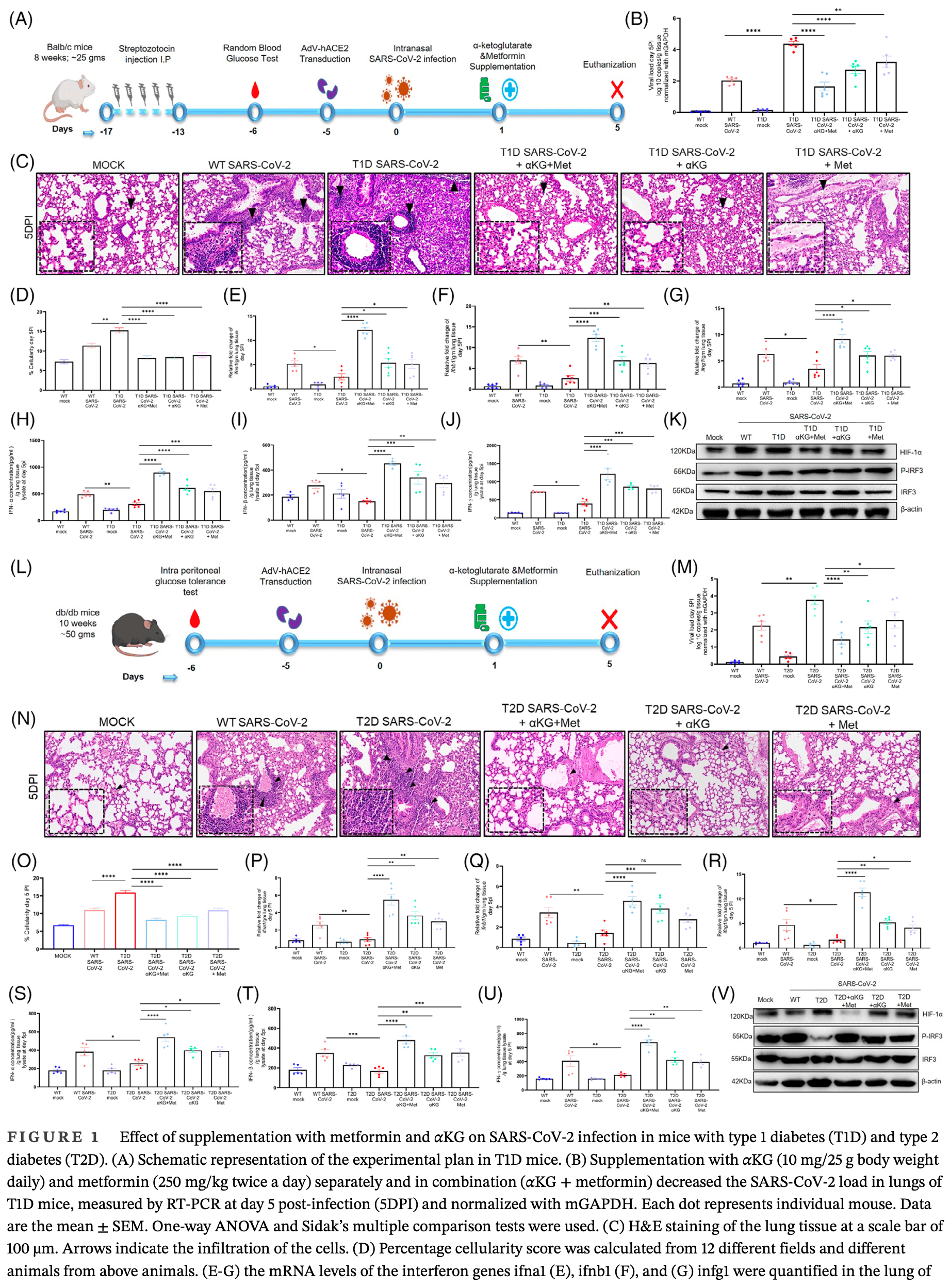
In vitro and mouse study showing that metformin and/or alpha-ketoglutarate (αKG) supplementation reduces SARS-CoV-2 infection severity in diabetic mice by modulating the HIF1α-interferon axis. Diabetic mice exhibited elevated viral loads, inflammation, and reduced IFN production. Treatment with metformin and/or αKG suppressed HIF-1α, restored IFN expression, and reduced lung viral load and inflammation. In vitro experiments confirmed this mechanism in insulin-resistant and HIF1A-knockdown cell lines. Human data from diabetic COVID-19 patients on metformin showed upregulation of IFN-related genes and higher neutralizing antibody titers, especially at 1000 mg/day versus 500 mg/day doses, suggesting dose-dependent immune benefits.
18 preclinical studies support the efficacy of metformin for COVID-19:
A systematic review and meta-analysis of 15 non-COVID-19 preclinical studies showed that metformin inhibits pulmonary inflammation and oxidative stress, minimizes lung injury, and improves survival in animal models of acute respiratory distress syndrome (ARDS) or acute lung injury (ALI)15.
Metformin inhibits SARS-CoV-2 in vitro11,12, minimizes LPS-induced cytokine storm in a mouse model14, minimizes lung damage and fibrosis in a mouse model of LPS-induced ARDS10, may protect against SARS-CoV-2-induced neurological disorders9, may be beneficial via inhibitory effects on ORF3a-mediated inflammasome activation16, reduces UUO and FAN-induced kidney fibrosis10, increases mitochondrial function and decreases TGF-β-induced fibrosis, apoptosis, and inflammation markers in lung epithelial cells10, may reduce inflammation, oxidative stress, and thrombosis via regulating glucose metabolism2, attenuates spike protein S1-induced inflammatory response and α-synuclein aggregation8, may protect against COVID-19 cognitive impairment by suppressing HIF-1α stabilization and reducing neurodegenerative protein aggregation13, may reduce COVID-19 severity and long COVID by inhibiting NETosis via suppression of protein kinase C activation17, enhances interferon responses and reduces SARS-CoV-2 infection and inflammation in diabetic models by suppressing HIF-1α signaling7, may improve COVID-19 outcomes by preventing VDAC1 mistargeting to the plasma membrane, reducing ATP loss, and preserving immune cell function during cytokine storm18, reduces hyperglycemia-induced hepatic ACE2/TMPRSS2 up-regulation and SARS-CoV-2 entry6, may reduce COVID-19 severity by suppressing monocyte inflammatory responses and glycolytic activation via AMPK pathway modulation5, and may improve outcomes via modulation of immune responses with increased anti-inflammatory T lymphocyte gene expression and via enhanced gut microbiota diversity19.
1.
Tavares et al., Investigation of Interactions Between the Protein MPro and the Vanadium Complex VO(metf)2∙H2O: A Computational Approach for COVID-19 Treatment, Biophysica, doi:10.3390/biophysica5010004.
2.
Hou et al., Metformin is a potential therapeutic for COVID-19/LUAD by regulating glucose metabolism, Scientific Reports, doi:10.1038/s41598-024-63081-0.
3.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
4.
Lockwood, T., Coordination chemistry suggests that independently observed benefits of metformin and Zn2+ against COVID-19 are not independent, BioMetals, doi:10.1007/s10534-024-00590-5.
5.
Maurmann et al., Immunoregulatory effect of metformin in monocytes exposed to SARS-CoV-2 spike protein subunit 1, bioRxiv, doi:10.1101/2025.09.12.675877.
6.
Rao et al., Pathological Glucose Levels Enhance Entry Factor Expression and Hepatic SARS‐CoV‐2 Infection, Journal of Cellular and Molecular Medicine, doi:10.1111/jcmm.70581.
7.
Joshi et al., Severe SARS‐CoV‐2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α‐IFN axis, Clinical and Translational Medicine, doi:10.1002/ctm2.70275.
8.
Chang et al., SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin, Biomedicines, doi:10.3390/biomedicines12061223.
9.
Yang et al., SARS-CoV-2 infection causes dopaminergic neuron senescence, Cell Stem Cell, doi:10.1016/j.stem.2023.12.012.
10.
Miguel et al., Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney, Redox Biology, doi:10.1016/j.redox.2023.102957.
11.
Ventura-López et al., Treatment with metformin glycinate reduces SARS-CoV-2 viral load: An in vitro model and randomized, double-blind, Phase IIb clinical trial, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113223.
12.
Parthasarathy et al., Metformin Suppresses SARS-CoV-2 in Cell Culture, bioRxiv, doi:10.1101/2021.11.18.469078.
13.
Lee et al., SARS-CoV-2 spike protein causes synaptic dysfunction and p-tau and α-synuclein aggregation leading cognitive impairment: The protective role of metformin, PLOS One, doi:10.1371/journal.pone.0336015.
14.
Taher et al., Anti‑inflammatory effect of metformin against an experimental model of LPS‑induced cytokine storm, Experimental and Therapeutic Medicine, doi:10.3892/etm.2023.12114.
15.
Wang et al., Effects of metformin on acute respiratory distress syndrome in preclinical studies: a systematic review and meta-analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1215307.
16.
Zhang et al., SARS-CoV-2 ORF3a Protein as a Therapeutic Target against COVID-19 and Long-Term Post-Infection Effects, Pathogens, doi:10.3390/pathogens13010075.
17.
Monsalve et al., NETosis: A key player in autoimmunity, COVID-19, and long COVID, Journal of Translational Autoimmunity, doi:10.1016/j.jtauto.2025.100280.
Joshi et al., 8 Apr 2025, peer-reviewed, 14 authors, study period June 2020 - April 2021.
Contact: prasenjit@rcb.res.in.
Severe SARS‐CoV‐2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α‐IFN axis
Clinical and Translational Medicine, doi:10.1002/ctm2.70275
Severe SARS-CoV-2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α-IFN axis Dear Editor, Studies report a higher prevalence of COVID-19 and worse outcomes in diabetic patients, typically 1.5-3-fold greater than similar populations without diabetes 1 and the individuals taking the hypoglycaemic drug metformin have better survival. 2, 3 We investigated the mechanisms for the above reports and observed that the hyperglycaemic mice with either type 1 or type 2 diabetes (T1D/T2D) have elevated SARS-CoV-2 infection in the lungs at day-5 post infection (5DPI, Figure 1 A , B) with aggressive inflammation, indicated by infiltration of immune cells (Figure 1C,D) and accumulation of cytokines TNFα and IL6 (Figure S1C,D) as compared to non-diabetic counterparts, (T2D mice data in Figure 1L-O, Figure S2C-D). Both T1D/T2D mice showed decreased levels of interferons in lung tissue lysate (type-1 and -2; IFN-α/IFNβ/IFN-γ, Figure 1H-J/S-U) alongside decreased expression of IFNA1/IFNB1/IFNG1 and IFN-regulatory factor (IRF)-3/IRF-7 genes (Figure-1E-G/P-R, Figures S1E,F and S2E,F) in the lung tissue and in the spleen (Figures S1I-M and S2I-M) but elevated HIF-1α in the lungs (Figure 1K,V and Figures S1G and S2G ). The supplementation with metformin and/or alpha-ketoglutarate (αKG, previously used by us 4,5 ) significantly reduced viral load, and rescued inflamed lungs and IFNs synthesis (Figure-1K,V and Figure S1 H/S2 H). Unlike IFNs, the levels of IgG and the neutralization antibody titre against SARS-CoV-2 were found unaltered between WT and diabetic (T1D/T2D) mice even after metformin+αKG treatment (Figures S1N-Q and S2N,O ). The repetition of above experiment in K-18 mice and high fat diet induced T2D model of K-18 showed similar observations (Figure S4A-M ). In mechanism, we described that hyperglycaemic microenvironment (25 mM glucose) increased SARS-CoV-2 infection (Figure 2A ) and decreased IFNA1/IFNB1 expression in the insulin resistant Huh-7 cells model (Figure
References
Agarwal, Kaur, Asuru, Dietary alpha-ketoglutarate inhibits SARS CoV-2 infection and rescues inflamed lungs to restore O 2 saturation by inhibiting P-AKT, Clin Transl Med
Apicella, Campopiano, Mantuano, COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diab Endocrinol
Codo, Gasta˜o, Gustavo, De Brito Monteiro, Lauar, Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1α/glycolysis-dependent axis, Cell Metab
Feldman, Savelieff, Hayek, Pennathur, Kretzler et al., COVID-19 and Diabetes: a collision and collusion of two diseases, Diabetes
Frasca, Diaz, Romero, Blomberg, Metformin enhances B cell function and antibody responses of elderly individuals with type 2 diabetes mellitus, Front Aging
Lim, Bae, Kwon, COVID-19 and diabetes mellitus: from pathophysiology to clinical management, Nat Rev Endocrinol
Martin, Cadar, Panier, The effect of metformin on influenza vaccine responses in nondiabetic older adults: a pilot trial, Immun Ageing
Peng, Du, Diamond, HIF-1α is a negative regulator of interferon regulatory factors: implications for interferon production by hypoxic monocytes, PNAS
Shrimali, Agarwal, Kaur, α-ketoglutarate inhibits thrombosis and inflammation by prolyl hydroxylase-2 mediated inactivation of P-AKT, EBioMedicine
Xu, He, Yu, Effects of different treatments for type 2 diabetes mellitus on mortality of coronavirus disease from 2019 to 2021 in China: a multi-institutional retrospective study, Mole Biomed
DOI record:
{
"DOI": "10.1002/ctm2.70275",
"ISSN": [
"2001-1326",
"2001-1326"
],
"URL": "http://dx.doi.org/10.1002/ctm2.70275",
"alternative-id": [
"10.1002/ctm2.70275"
],
"author": [
{
"ORCID": "https://orcid.org/0000-0002-6601-6692",
"affiliation": [
{
"name": "Department of Biotechnology Regional Centre for Biotechnology, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"authenticated-orcid": false,
"family": "Joshi",
"given": "Garima",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Biotechnology Regional Centre for Biotechnology, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Verma",
"given": "Garima",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biotechnology Regional Centre for Biotechnology, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Kaur",
"given": "Simrandeep",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Ramasamy",
"given": "Ellango",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biotechnology Regional Centre for Biotechnology, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Chauhan",
"given": "Navya",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Singh",
"given": "Savita",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Jana",
"given": "Pradipta",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Rizvi",
"given": "Zaigham Abbas",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Kshetrapal",
"given": "Pallavi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Bhatnagar",
"given": "Shinjini",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "ESIC Medical College and Hospital Faridabad Haryana India"
}
],
"family": "Pandey",
"given": "Anil Kumar",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Awasthi",
"given": "Amit",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Translational Health Science Technology Institute, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Das",
"given": "Bhabatosh",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biotechnology Regional Centre for Biotechnology, National Capital Region Biotech Science Cluster Faridabad Haryana India"
}
],
"family": "Guchhait",
"given": "Prasenjit",
"sequence": "additional"
}
],
"container-title": "Clinical and Translational Medicine",
"container-title-short": "Clinical &amp; Translational Med",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
4,
9
]
],
"date-time": "2025-04-09T05:40:48Z",
"timestamp": 1744177248000
},
"deposited": {
"date-parts": [
[
2025,
4,
9
]
],
"date-time": "2025-04-09T05:40:50Z",
"timestamp": 1744177250000
},
"indexed": {
"date-parts": [
[
2025,
4,
10
]
],
"date-time": "2025-04-10T04:09:25Z",
"timestamp": 1744258165211,
"version": "3.40.4"
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2025,
4
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2025,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 7,
"start": {
"date-parts": [
[
2025,
4,
8
]
],
"date-time": "2025-04-08T00:00:00Z",
"timestamp": 1744070400000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/ctm2.70275",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"prefix": "10.1002",
"published": {
"date-parts": [
[
2025,
4
]
]
},
"published-online": {
"date-parts": [
[
2025,
4,
8
]
]
},
"published-print": {
"date-parts": [
[
2025,
4
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.2337/dbi20-0032",
"article-title": "COVID‐19 and Diabetes: a collision and collusion of two diseases",
"author": "Feldman EL",
"doi-asserted-by": "crossref",
"first-page": "2549",
"issue": "12",
"journal-title": "Diabetes",
"key": "e_1_2_1_8_2_1",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"article-title": "COVID‐19 in people with diabetes: understanding the reasons for worse outcomes",
"author": "Apicella M",
"doi-asserted-by": "crossref",
"first-page": "782",
"issue": "9",
"journal-title": "Lancet Diab Endocrinol",
"key": "e_1_2_1_8_3_1",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1186/s43556-024-00183-1",
"article-title": "Effects of different treatments for type 2 diabetes mellitus on mortality of coronavirus disease from 2019 to 2021 in China: a multi‐institutional retrospective study",
"author": "Xu K",
"doi-asserted-by": "crossref",
"first-page": "18",
"issue": "1",
"journal-title": "Mole Biomed",
"key": "e_1_2_1_8_4_1",
"volume": "5",
"year": "2024"
},
{
"DOI": "10.1016/j.ebiom.2021.103672",
"article-title": "α‐ketoglutarate inhibits thrombosis and inflammation by prolyl hydroxylase‐2 mediated inactivation of P‐AKT",
"author": "Shrimali NM",
"doi-asserted-by": "crossref",
"journal-title": "EBioMedicine",
"key": "e_1_2_1_8_5_1",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1002/ctm2.1041",
"article-title": "Dietary alpha‐ketoglutarate inhibits SARS CoV‐2 infection and rescues inflamed lungs to restore O2 saturation by inhibiting P‐AKT",
"author": "Agarwal S",
"doi-asserted-by": "crossref",
"first-page": "2",
"issue": "9",
"journal-title": "Clin Transl Med",
"key": "e_1_2_1_8_6_1",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.cmet.2020.07.007",
"article-title": "Elevated glucose levels favor SARS‐CoV‐2 infection and monocyte response through a HIF‐1α/glycolysis‐dependent axis",
"author": "Codo AC",
"doi-asserted-by": "crossref",
"first-page": "437",
"issue": "3",
"journal-title": "Cell Metab",
"key": "e_1_2_1_8_7_1",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1038/s41574-020-00435-4",
"article-title": "COVID‐19 and diabetes mellitus: from pathophysiology to clinical management",
"author": "Lim S",
"doi-asserted-by": "crossref",
"first-page": "11",
"issue": "1",
"journal-title": "Nat Rev Endocrinol",
"key": "e_1_2_1_8_8_1",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1073/pnas.2106017118",
"article-title": "HIF‐1α is a negative regulator of interferon regulatory factors: implications for interferon production by hypoxic monocytes",
"author": "Peng T",
"doi-asserted-by": "crossref",
"issue": "26",
"journal-title": "PNAS",
"key": "e_1_2_1_8_9_1",
"volume": "118",
"year": "2021"
},
{
"DOI": "10.3389/fragi.2021.715981",
"article-title": "Metformin enhances B cell function and antibody responses of elderly individuals with type 2 diabetes mellitus",
"author": "Frasca D",
"doi-asserted-by": "crossref",
"journal-title": "Front Aging",
"key": "e_1_2_1_8_10_1",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1186/s12979-023-00343-x",
"article-title": "The effect of metformin on influenza vaccine responses in nondiabetic older adults: a pilot trial",
"author": "Martin DE",
"doi-asserted-by": "crossref",
"first-page": "18",
"issue": "1",
"journal-title": "Immun Ageing",
"key": "e_1_2_1_8_11_1",
"volume": "20",
"year": "2023"
}
],
"reference-count": 10,
"references-count": 10,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/ctm2.70275"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Severe SARS‐CoV‐2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α‐IFN axis",
"type": "journal-article",
"volume": "15"
}
