Effects of metformin on acute respiratory distress syndrome in preclinical studies: a systematic review and meta-analysis
et al., Frontiers in Pharmacology, doi:10.3389/fphar.2023.1215307, Sep 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Systematic review and meta-analysis of 15 non-COVID-19 preclinical studies of metformin for acute respiratory distress syndrome (ARDS) or acute lung injury (ALI), showing that metformin inhibits pulmonary inflammation and oxidative stress, minimizes lung injury, and improves survival in animal models.
18 preclinical studies support the efficacy of metformin for COVID-19:
A systematic review and meta-analysis of 15 non-COVID-19 preclinical studies showed that metformin inhibits pulmonary inflammation and oxidative stress, minimizes lung injury, and improves survival in animal models of acute respiratory distress syndrome (ARDS) or acute lung injury (ALI)15.
Metformin inhibits SARS-CoV-2 in vitro11,12, minimizes LPS-induced cytokine storm in a mouse model14, minimizes lung damage and fibrosis in a mouse model of LPS-induced ARDS10, may protect against SARS-CoV-2-induced neurological disorders9, may be beneficial via inhibitory effects on ORF3a-mediated inflammasome activation16, reduces UUO and FAN-induced kidney fibrosis10, increases mitochondrial function and decreases TGF-β-induced fibrosis, apoptosis, and inflammation markers in lung epithelial cells10, may reduce inflammation, oxidative stress, and thrombosis via regulating glucose metabolism2, attenuates spike protein S1-induced inflammatory response and α-synuclein aggregation8, may protect against COVID-19 cognitive impairment by suppressing HIF-1α stabilization and reducing neurodegenerative protein aggregation13, may reduce COVID-19 severity and long COVID by inhibiting NETosis via suppression of protein kinase C activation17, enhances interferon responses and reduces SARS-CoV-2 infection and inflammation in diabetic models by suppressing HIF-1α signaling7, may improve COVID-19 outcomes by preventing VDAC1 mistargeting to the plasma membrane, reducing ATP loss, and preserving immune cell function during cytokine storm18, reduces hyperglycemia-induced hepatic ACE2/TMPRSS2 up-regulation and SARS-CoV-2 entry6, may reduce COVID-19 severity by suppressing monocyte inflammatory responses and glycolytic activation via AMPK pathway modulation5, and may improve outcomes via modulation of immune responses with increased anti-inflammatory T lymphocyte gene expression and via enhanced gut microbiota diversity19.
1.
Tavares et al., Investigation of Interactions Between the Protein MPro and the Vanadium Complex VO(metf)2∙H2O: A Computational Approach for COVID-19 Treatment, Biophysica, doi:10.3390/biophysica5010004.
2.
Hou et al., Metformin is a potential therapeutic for COVID-19/LUAD by regulating glucose metabolism, Scientific Reports, doi:10.1038/s41598-024-63081-0.
3.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
4.
Lockwood, T., Coordination chemistry suggests that independently observed benefits of metformin and Zn2+ against COVID-19 are not independent, BioMetals, doi:10.1007/s10534-024-00590-5.
5.
Maurmann et al., Immunoregulatory effect of metformin in monocytes exposed to SARS-CoV-2 spike protein subunit 1, bioRxiv, doi:10.1101/2025.09.12.675877.
6.
Rao et al., Pathological Glucose Levels Enhance Entry Factor Expression and Hepatic SARS‐CoV‐2 Infection, Journal of Cellular and Molecular Medicine, doi:10.1111/jcmm.70581.
7.
Joshi et al., Severe SARS‐CoV‐2 infection in diabetes was rescued in mice supplemented with metformin and/or αKG, and patients taking metformin, via HIF1α‐IFN axis, Clinical and Translational Medicine, doi:10.1002/ctm2.70275.
8.
Chang et al., SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin, Biomedicines, doi:10.3390/biomedicines12061223.
9.
Yang et al., SARS-CoV-2 infection causes dopaminergic neuron senescence, Cell Stem Cell, doi:10.1016/j.stem.2023.12.012.
10.
Miguel et al., Enhanced fatty acid oxidation through metformin and baicalin as therapy for COVID-19 and associated inflammatory states in lung and kidney, Redox Biology, doi:10.1016/j.redox.2023.102957.
11.
Ventura-López et al., Treatment with metformin glycinate reduces SARS-CoV-2 viral load: An in vitro model and randomized, double-blind, Phase IIb clinical trial, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113223.
12.
Parthasarathy et al., Metformin Suppresses SARS-CoV-2 in Cell Culture, bioRxiv, doi:10.1101/2021.11.18.469078.
13.
Lee et al., SARS-CoV-2 spike protein causes synaptic dysfunction and p-tau and α-synuclein aggregation leading cognitive impairment: The protective role of metformin, PLOS One, doi:10.1371/journal.pone.0336015.
14.
Taher et al., Anti‑inflammatory effect of metformin against an experimental model of LPS‑induced cytokine storm, Experimental and Therapeutic Medicine, doi:10.3892/etm.2023.12114.
15.
Wang et al., Effects of metformin on acute respiratory distress syndrome in preclinical studies: a systematic review and meta-analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1215307.
16.
Zhang et al., SARS-CoV-2 ORF3a Protein as a Therapeutic Target against COVID-19 and Long-Term Post-Infection Effects, Pathogens, doi:10.3390/pathogens13010075.
17.
Monsalve et al., NETosis: A key player in autoimmunity, COVID-19, and long COVID, Journal of Translational Autoimmunity, doi:10.1016/j.jtauto.2025.100280.
Wang et al., 28 Sep 2023, China, peer-reviewed, 3 authors.
Contact: wwwlll838940@163.com.
Effects of metformin on acute respiratory distress syndrome in preclinical studies: a systematic review and meta-analysis
Frontiers in Pharmacology, doi:10.3389/fphar.2023.1215307
Introduction: In this study, we conducted a systematic review and meta-analysis to judge the effects of metformin on acute respiratory distress syndrome (ARDS) in a comprehensive and quantitative manner.
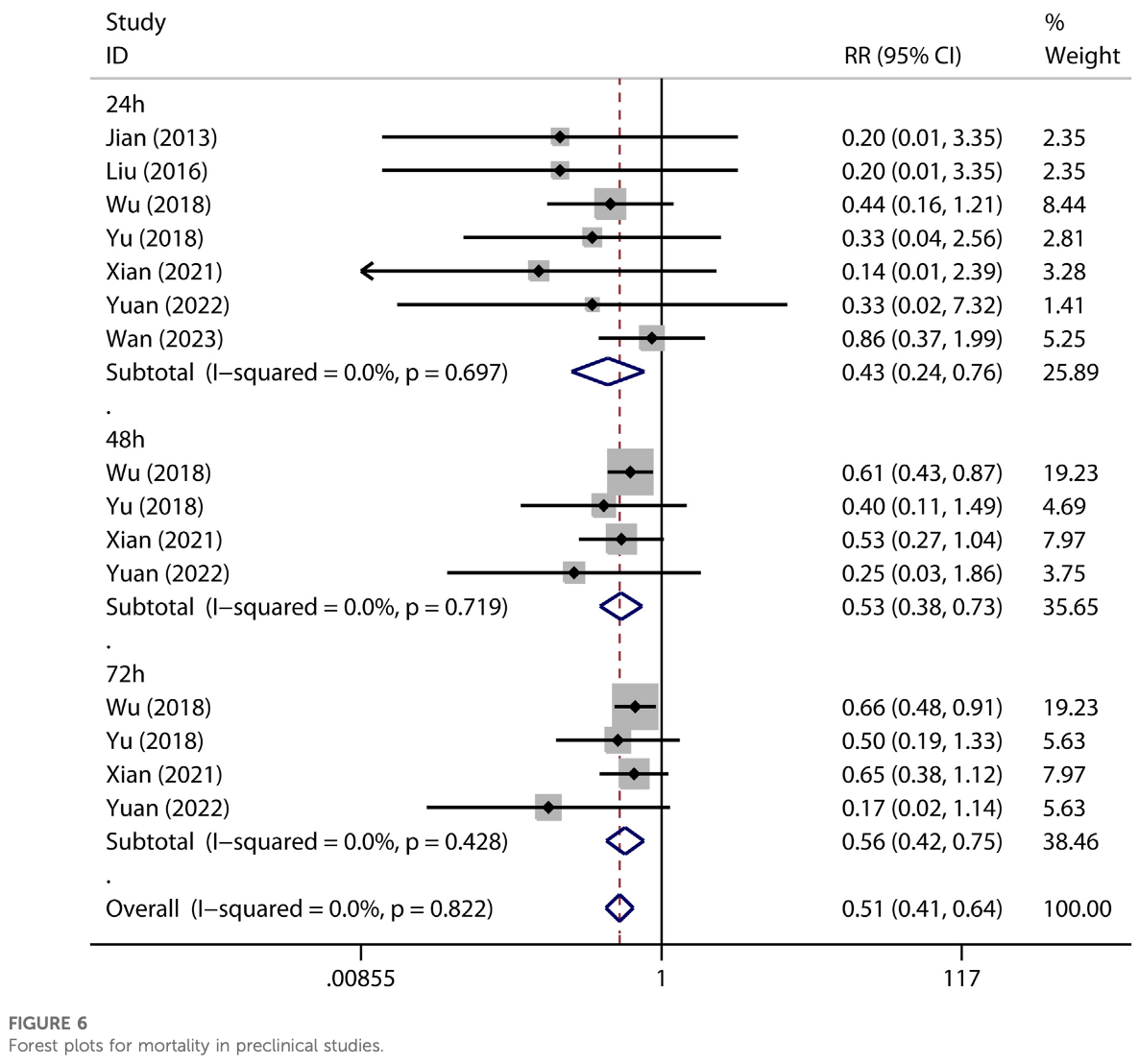
Methods: We included studies that tested the effects of metformin on ALI or ARDS in in vivo studies. We excluded literature from which data could not be extracted or obtained. Electronic search was conducted to retrieve relevant literature from public databases, including PubMed, Web of Science, Embase, Scopus, and the Cochrane Central Register of Controlled Trials (inception to July 2023). Moreover, ProQuest Dissertations and Theses Global, Google Scholar, and Baidu scholar were inquired. Retrieved literature was screened and evaluated by pairs of reviewers independently according to pre-stated criteria. The Systematic Review Center for Laboratory Animal Experimentation risk of bias tool was used to evaluate the methodological quality of eligible literature. No restriction was exerted on publication status or language. Results: Fifteen preclinical studies were analyzed in this meta-analysis. Pooled results showed metformin effectively decreased pulmonary wet-to-dry weight ratios [SMD = -2.67 (-3.53 to -1.81), I 2 = 56.6%], protein content [SMD = -3.74 (-6.76 to -0.72), I 2 = 86.7%] and neutrophils [SMD = -3.47 (-4.69 to -2.26), I 2 = 0%] in BALF, pulmonary malondialdehyde [SMD = -1.98 (-3.77 to -0.20), I 2 = 74.2%] and myeloperoxidase activity [SMD = -3.15 (-4.79 to -1.52), I 2 = 74.5%], lung injury scores [SMD = -4.19 (-5.65 to -2.74), I 2 = 69.1%], and mortality at 24 h [RR = 0.43 (0.24-0.76), I 2 = 0%] as well as 48 and 72 h.
Conclusion: Metformin inhibited pulmonary inflammation and oxidative stress and improved experimental lung injury and survival rates in animal models of ARDS. Results from randomized controlled trials are needed.
Author contributions LW and Y-FT conceived and designed the study. W-QD and LW performed the literature search. LW and Y-FT selected trials and extracted data. LW and W-QD assessed the risk of bias of trials. LW and W-QD analyzed the data. LW and W-QD wrote the manuscript. Y-FT revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1215307/ full#supplementary-material
References
Boyle, Van Wickle, Hill, Marchese, Kalyanaraman et al., Mitochondria-targeted drugs stimulate mitophagy and abrogate colon cancer cell proliferation, J. Biol. Chem, doi:10.1074/jbc.RA117.001469
Christiansen, Johansen, Christensen, O'brien, Tønnesen et al., Preadmission metformin use and mortality among intensive care patients with diabetes: a cohort study, Crit. care, doi:10.1186/cc12886
Ghavimi, Sheidaei, Vaez, Zolali, Asgharian et al., Metformin-attenuated sepsis-induced oxidative damages: a novel role for metformin, Iran. J. basic Med. Sci, doi:10.22038/IJBMS.2018.24610.6126
Gómez, Del Rio-Pertuz, Priyanka, Manrique-Caballero, Chang et al., Association of metformin use during hospitalization and mortality in critically ill adults with type 2 diabetes mellitus and sepsis, Crit. care Med, doi:10.1097/CCM.0000000000005468
He, Xu, Wang, Chao, Xu et al., AMPK as a potential pharmacological target for alleviating LPS-induced acute lung injury partly via NLRC4 inflammasome pathway inhibition, Exp. Gerontol, doi:10.1016/j.exger.2019.110661
Higgins, Altman, Gøtzsche, Jüni, Moher et al., The Cochrane Collaboration's tool for assessing risk of bias in randomised trials, BMJ Clin. Res. ed), doi:10.1136/bmj.d5928
Hooijmans, Rovers, De Vries, Leenaars, Ritskes-Hoitinga et al., SYRCLE's risk of bias tool for animal studies, BMC Med. Res. Methodol, doi:10.1186/1471-2288-14-43
Jian, Alexeyev, Wolkowicz, Zmijewski, Creighton, Metformin-stimulated AMPK-α1 promotes microvascular repair in acute lung injury, Am. J. physiology Lung Cell. Mol. physiology, doi:10.1152/ajplung.00173.2013
Jo, Choi, Lee, Park, Lee et al., Effect of preadmission metformin use on clinical outcome of acute respiratory distress syndrome among critically ill patients with diabetes, Tuberc. Respir. Dis, doi:10.4046/trd.2017.80.3.296
Li, Zhao, Guo, Duan, Ding, Association of preadmission metformin use and prognosis in patients with sepsis and diabetes mellitus: A systematic review and meta-analysis, Front. Endocrinol, doi:10.3389/fendo.2021.811776
Liu, Bone, Jiang, Park, Tadie et al., AMPactivated protein kinase and glycogen synthase kinase 3β modulate the severity of sepsis-induced lung injury, Mol. Med. Camb. Mass), doi:10.2119/molmed.2015.00198
Medeiros, Oliveira, De Oliveira, Mónica, Antunes, Methylglyoxal exacerbates lipopolysaccharide-induced acute lung injury via RAGE-induced ROS generation: Protective effects of metformin, J. Inflamm. Res, doi:10.2147/JIR.S337115
Meyer, Gattinoni, Calfee, Acute respiratory distress syndrome, Lancet, doi:10.1016/S0140-6736(21)00439-6
Oh, Song, Prior metformin therapy and 30-day mortality in patients with acute respiratory distress syndrome: a nationwide cohort study, Ann. Palliat. Med, doi:10.21037/apm.2020.04.25
Poly, Islam, Li, Lin, Hsu et al., Metformin use is associated with decreased mortality in COVID-19 patients with diabetes: Evidence from retrospective studies and biological mechanism, J. Clin. Med, doi:10.3390/jcm10163507
Ranieri, Rubenfeld, Thompson, Ferguson, Caldwell et al., Acute respiratory distress syndrome: the Berlin Definition, Jama, doi:10.1001/jama.2012.5669
Reitz, Marroquin, Zenati, Kennedy, Korytkowski et al., Association between preoperative metformin exposure and postoperative outcomes in adults with type 2 diabetes, JAMA Surg, doi:10.1001/jamasurg.2020.0416
Schranc, Fodor, Südy, Tolnai, Babik et al., Exaggerated ventilator-induced lung injury in an animal model of type 2 diabetes mellitus: A randomized experimental study, Front. physiology, doi:10.3389/fphys.2022.889032
Sul, Lewis, Dee, Burns, Oshima et al., Release of extracellular superoxide dismutase into alveolar fluid protects against acute lung injury and inflammation in Staphylococcus aureus pneumonia, Am. J. physiology Lung Cell. Mol. physiology, doi:10.1152/ajplung.00217.2022
Taheri, Emami, Asadipour, Kasirzadeh, Rouini et al., A randomized controlled trial on the efficacy, safety, and pharmacokinetics of metformin in severe traumatic brain injury, J. neurology, doi:10.1007/s00415-019-09366-1
Tao, Xu, Luo, Li, Inhibitors of soluble epoxide hydrolase on acute lung injury: a meta-analysis of preclinical studies, Inflammopharmacology, doi:10.1007/s10787-022-01063-2
Triggle, Mohammed, Bshesh, Marei, Ye et al., Metformin: Is it a drug for all reasons and diseases?, Metabolism Clin. Exp, doi:10.1016/j.metabol.2022.155223
Tsaknis, Siempos, Kopterides, Maniatis, Magkou et al., Metformin attenuates ventilator-induced lung injury, Crit. care, doi:10.1186/cc11439
Uddin, Akhter, Kubra, Siejka, Barabutis, Metformin in acute respiratory distress syndrome: An opinion, Exp. Gerontol, doi:10.1016/j.exger.2020.111197
Vaez, Najafi, Toutounchi, Barar, Barzegari et al., Metformin alleviates lipopolysaccharide-induced acute lung injury through suppressing toll-like receptor 4 signaling. Iran, J. allergy, asthma, Immunol
Wan, Wang, Niu, Duo, Liu et al., Effect of metformin on sepsis-associated acute lung injury and gut microbiota in aged rats with sepsis, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2023.1139436
Wang, None
Wang, Song, Feng, Liu, Zhu et al., Activation of AMPK attenuates LPS-induced acute lung injury by upregulation of PGC1α and SOD1, Exp. Ther. Med, doi:10.3892/etm.2016.3465
Wheaton, Weinberg, Hamanaka, Soberanes, Sullivan et al., Metformin inhibits mitochondrial complex I of cancer cells to reduce tumorigenesis, eLife, doi:10.7554/eLife.02242
Wu, Cen, Feng, Zhou, Tang et al., Metformin activates the protective effects of the AMPK pathway in acute lung injury caused by paraquat poisoning, Oxidative Med. Cell. Longev, doi:10.1155/2019/1709718
Wu, Tian, Huang, Yang, Dai et al., Metformin alleviated endotoxemia-induced acute lung injury via restoring AMPK-dependent suppression of mTOR, Chemico-biological Interact, doi:10.1016/j.cbi.2018.05.018
Xian, Liu, Rundberg Nilsson, Gatchalian, Crother et al., Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation, Immunity, doi:10.1016/j.immuni.2021.05.004
Yu, Zhu, Huang, Zhao, Wen et al., Metformin relieves acute respiratory distress syndrome by reducing miR-138 expression, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_201808_15737
Yuan, Li, Hou, Yang, Meng et al., Metformin regulates alveolar macrophage polarization to protect against acute lung injury in rats caused by paraquat poisoning, Front. Pharmacol, doi:10.3389/fphar.2022.811372
Zhang, Sun, Ding, Hong, Li et al., Metformin mitigates gas explosion-induced blast lung injuries through AMPK-mediated energy metabolism and NOX2-related oxidation pathway in rats, Exp. Ther. Med, doi:10.3892/etm.2022.11456
Zhang, Zhang, Li, Huang, Jiang et al., Metformin alleviates LPS-induced acute lung injury by regulating the SIRT1/NF-κB/ NLRP3 pathway and inhibiting endothelial cell pyroptosis, Front. Pharmacol, doi:10.3389/fphar.2022.801337
Zheng, Ley, Hu, Global aetiology and epidemiology of type 2 diabetes mellitus and its complications, Nat. Rev. Endocrinol, doi:10.1038/nrendo.2017.151
Zhong, Liang, Sanchez-Lopez, He, Shalapour et al., New mitochondrial DNA synthesis enables NLRP3 inflammasome activation, Nature, doi:10.1038/s41586-018-0372-z
Zmijewski, Lorne, Zhao, Tsuruta, Sha et al., Mitochondrial respiratory complex I regulates neutrophil activation and severity of lung injury, Am. J. Respir. Crit. care Med, doi:10.1164/rccm.200710-1602OC
DOI record:
{
"DOI": "10.3389/fphar.2023.1215307",
"ISSN": [
"1663-9812"
],
"URL": "http://dx.doi.org/10.3389/fphar.2023.1215307",
"abstract": "<jats:p><jats:bold>Introduction:</jats:bold> In this study, we conducted a systematic review and meta-analysis to judge the effects of metformin on acute respiratory distress syndrome (ARDS) in a comprehensive and quantitative manner.</jats:p><jats:p><jats:bold>Methods:</jats:bold> We included studies that tested the effects of metformin on ALI or ARDS in <jats:italic>in vivo</jats:italic> studies. We excluded literature from which data could not be extracted or obtained. Electronic search was conducted to retrieve relevant literature from public databases, including PubMed, Web of Science, Embase, Scopus, and the Cochrane Central Register of Controlled Trials (inception to July 2023). Moreover, ProQuest Dissertations and Theses Global, Google Scholar, and Baidu scholar were inquired. Retrieved literature was screened and evaluated by pairs of reviewers independently according to pre-stated criteria. The Systematic Review Center for Laboratory Animal Experimentation risk of bias tool was used to evaluate the methodological quality of eligible literature. No restriction was exerted on publication status or language.</jats:p><jats:p><jats:bold>Results:</jats:bold> Fifteen preclinical studies were analyzed in this meta-analysis. Pooled results showed metformin effectively decreased pulmonary wet-to-dry weight ratios [SMD = −2.67 (−3.53 to −1.81), I<jats:sup>2</jats:sup> = 56.6%], protein content [SMD = −3.74 (−6.76 to −0.72), I<jats:sup>2</jats:sup> = 86.7%] and neutrophils [SMD = −3.47 (−4.69 to −2.26), I<jats:sup>2</jats:sup> = 0%] in BALF, pulmonary malondialdehyde [SMD = −1.98 (−3.77 to −0.20), I<jats:sup>2</jats:sup> = 74.2%] and myeloperoxidase activity [SMD = −3.15 (−4.79 to −1.52), I<jats:sup>2</jats:sup> = 74.5%], lung injury scores [SMD = −4.19 (−5.65 to −2.74), I<jats:sup>2</jats:sup> = 69.1%], and mortality at 24 h [RR = 0.43 (0.24–0.76), I<jats:sup>2</jats:sup> = 0%] as well as 48 and 72 h.</jats:p><jats:p><jats:bold>Conclusion:</jats:bold> Metformin inhibited pulmonary inflammation and oxidative stress and improved experimental lung injury and survival rates in animal models of ARDS. Results from randomized controlled trials are needed.</jats:p>",
"alternative-id": [
"10.3389/fphar.2023.1215307"
],
"author": [
{
"affiliation": [],
"family": "Wang",
"given": "Liu",
"sequence": "first"
},
{
"affiliation": [],
"family": "Tian",
"given": "Yan-Fen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Deng",
"given": "Wen-Qing",
"sequence": "additional"
}
],
"container-title": "Frontiers in Pharmacology",
"container-title-short": "Front. Pharmacol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
9,
28
]
],
"date-time": "2023-09-28T13:16:13Z",
"timestamp": 1695906973000
},
"deposited": {
"date-parts": [
[
2023,
9,
28
]
],
"date-time": "2023-09-28T13:16:32Z",
"timestamp": 1695906992000
},
"indexed": {
"date-parts": [
[
2023,
9,
29
]
],
"date-time": "2023-09-29T15:47:54Z",
"timestamp": 1696002474381
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
9,
28
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
28
]
],
"date-time": "2023-09-28T00:00:00Z",
"timestamp": 1695859200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fphar.2023.1215307/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
9,
28
]
]
},
"published-online": {
"date-parts": [
[
2023,
9,
28
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1074/jbc.RA117.001469",
"article-title": "Mitochondria-targeted drugs stimulate mitophagy and abrogate colon cancer cell proliferation",
"author": "Boyle",
"doi-asserted-by": "publisher",
"first-page": "14891",
"journal-title": "J. Biol. Chem.",
"key": "B1",
"volume": "293",
"year": "2018"
},
{
"DOI": "10.1186/cc12886",
"article-title": "Preadmission metformin use and mortality among intensive care patients with diabetes: a cohort study",
"author": "Christiansen",
"doi-asserted-by": "publisher",
"first-page": "R192",
"journal-title": "Crit. care (London, Engl.",
"key": "B2",
"volume": "17",
"year": "2013"
},
{
"DOI": "10.22038/IJBMS.2018.24610.6126",
"article-title": "Metformin-attenuated sepsis-induced oxidative damages: a novel role for metformin",
"author": "Ghavimi",
"doi-asserted-by": "publisher",
"first-page": "469",
"journal-title": "Iran. J. basic Med. Sci.",
"key": "B3",
"volume": "21",
"year": "2018"
},
{
"DOI": "10.1097/CCM.0000000000005468",
"article-title": "Association of metformin use during hospitalization and mortality in critically ill adults with type 2 diabetes mellitus and sepsis",
"author": "Gómez",
"doi-asserted-by": "publisher",
"first-page": "935",
"journal-title": "Crit. care Med.",
"key": "B4",
"volume": "50",
"year": "2022"
},
{
"DOI": "10.1016/j.exger.2019.110661",
"article-title": "AMPK as a potential pharmacological target for alleviating LPS-induced acute lung injury partly via NLRC4 inflammasome pathway inhibition",
"author": "He",
"doi-asserted-by": "publisher",
"first-page": "110661",
"journal-title": "Exp. Gerontol.",
"key": "B5",
"volume": "125",
"year": "2019"
},
{
"DOI": "10.1136/bmj.d5928",
"article-title": "The Cochrane Collaboration's tool for assessing risk of bias in randomised trials",
"author": "Higgins",
"doi-asserted-by": "publisher",
"first-page": "d5928",
"journal-title": "BMJ Clin. Res. ed)",
"key": "B6",
"volume": "343",
"year": "2011"
},
{
"DOI": "10.1186/1471-2288-14-43",
"article-title": "SYRCLE's risk of bias tool for animal studies",
"author": "Hooijmans",
"doi-asserted-by": "publisher",
"first-page": "43",
"journal-title": "BMC Med. Res. Methodol.",
"key": "B7",
"volume": "14",
"year": "2014"
},
{
"DOI": "10.1152/ajplung.00173.2013",
"article-title": "Metformin-stimulated AMPK-α1 promotes microvascular repair in acute lung injury",
"author": "Jian",
"doi-asserted-by": "publisher",
"first-page": "L844",
"journal-title": "Am. J. physiology Lung Cell. Mol. physiology",
"key": "B8",
"volume": "305",
"year": "2013"
},
{
"DOI": "10.4046/trd.2017.80.3.296",
"article-title": "Effect of preadmission metformin use on clinical outcome of acute respiratory distress syndrome among critically ill patients with diabetes",
"author": "Jo",
"doi-asserted-by": "publisher",
"first-page": "296",
"journal-title": "Tuberc. Respir. Dis.",
"key": "B9",
"volume": "80",
"year": "2017"
},
{
"DOI": "10.3389/fendo.2021.811776",
"article-title": "Association of preadmission metformin use and prognosis in patients with sepsis and diabetes mellitus: A systematic review and meta-analysis",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "811776",
"journal-title": "Front. Endocrinol.",
"key": "B10",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.2119/molmed.2015.00198",
"article-title": "AMP-activated protein kinase and glycogen synthase kinase 3β modulate the severity of sepsis-induced lung injury",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "937",
"journal-title": "Mol. Med. Camb. Mass)",
"key": "B11",
"volume": "21",
"year": "2016"
},
{
"DOI": "10.2147/JIR.S337115",
"article-title": "Methylglyoxal exacerbates lipopolysaccharide-induced acute lung injury via RAGE-induced ROS generation: Protective effects of metformin",
"author": "Medeiros",
"doi-asserted-by": "publisher",
"first-page": "6477",
"journal-title": "J. Inflamm. Res.",
"key": "B12",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(21)00439-6",
"article-title": "Acute respiratory distress syndrome",
"author": "Meyer",
"doi-asserted-by": "publisher",
"first-page": "622",
"journal-title": "Lancet (London, Engl.",
"key": "B13",
"volume": "398",
"year": "2021"
},
{
"DOI": "10.21037/apm.2020.04.25",
"article-title": "Prior metformin therapy and 30-day mortality in patients with acute respiratory distress syndrome: a nationwide cohort study",
"author": "Oh",
"doi-asserted-by": "publisher",
"first-page": "903",
"journal-title": "Ann. Palliat. Med.",
"key": "B14",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3390/jcm10163507",
"article-title": "Metformin use is associated with decreased mortality in COVID-19 patients with diabetes: Evidence from retrospective studies and biological mechanism",
"author": "Poly",
"doi-asserted-by": "publisher",
"first-page": "3507",
"journal-title": "J. Clin. Med.",
"key": "B15",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1001/jama.2012.5669",
"article-title": "Acute respiratory distress syndrome: the Berlin Definition",
"author": "Ranieri",
"doi-asserted-by": "publisher",
"first-page": "2526",
"journal-title": "Jama",
"key": "B16",
"volume": "307",
"year": "2012"
},
{
"DOI": "10.1001/jamasurg.2020.0416",
"article-title": "Association between preoperative metformin exposure and postoperative outcomes in adults with type 2 diabetes",
"author": "Reitz",
"doi-asserted-by": "publisher",
"first-page": "e200416",
"journal-title": "JAMA Surg.",
"key": "B17",
"volume": "155",
"year": "2020"
},
{
"DOI": "10.3389/fphys.2022.889032",
"article-title": "Exaggerated ventilator-induced lung injury in an animal model of type 2 diabetes mellitus: A randomized experimental study",
"author": "Schranc",
"doi-asserted-by": "publisher",
"first-page": "889032",
"journal-title": "Front. physiology",
"key": "B18",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1152/ajplung.00217.2022",
"article-title": "Release of extracellular superoxide dismutase into alveolar fluid protects against acute lung injury and inflammation in Staphylococcus aureus pneumonia",
"author": "Sul",
"doi-asserted-by": "publisher",
"first-page": "L445",
"journal-title": "Am. J. physiology Lung Cell. Mol. physiology",
"key": "B19",
"volume": "324",
"year": "2023"
},
{
"DOI": "10.1007/s00415-019-09366-1",
"article-title": "A randomized controlled trial on the efficacy, safety, and pharmacokinetics of metformin in severe traumatic brain injury",
"author": "Taheri",
"doi-asserted-by": "publisher",
"first-page": "1988",
"journal-title": "J. neurology",
"key": "B20",
"volume": "266",
"year": "2019"
},
{
"DOI": "10.1007/s10787-022-01063-2",
"article-title": "Inhibitors of soluble epoxide hydrolase on acute lung injury: a meta-analysis of preclinical studies",
"author": "Tao",
"doi-asserted-by": "publisher",
"first-page": "2027",
"journal-title": "Inflammopharmacology",
"key": "B21",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.1016/j.metabol.2022.155223",
"article-title": "Metformin: Is it a drug for all reasons and diseases?",
"author": "Triggle",
"doi-asserted-by": "publisher",
"first-page": "155223",
"journal-title": "Metabolism Clin. Exp.",
"key": "B22",
"volume": "133",
"year": "2022"
},
{
"DOI": "10.1186/cc11439",
"article-title": "Metformin attenuates ventilator-induced lung injury",
"author": "Tsaknis",
"doi-asserted-by": "publisher",
"first-page": "R134",
"journal-title": "Crit. care (London, Engl.",
"key": "B23",
"volume": "16",
"year": "2012"
},
{
"DOI": "10.1016/j.exger.2020.111197",
"article-title": "Metformin in acute respiratory distress syndrome: An opinion",
"author": "Uddin",
"doi-asserted-by": "publisher",
"first-page": "111197",
"journal-title": "Exp. Gerontol.",
"key": "B24",
"volume": "145",
"year": "2021"
},
{
"article-title": "Metformin alleviates lipopolysaccharide-induced acute lung injury through suppressing toll-like receptor 4 signaling",
"author": "Vaez",
"first-page": "498",
"journal-title": "Iran. J. allergy, asthma, Immunol.",
"key": "B25",
"volume": "15",
"year": "2016"
},
{
"DOI": "10.3389/fcimb.2023.1139436",
"article-title": "Effect of metformin on sepsis-associated acute lung injury and gut microbiota in aged rats with sepsis",
"author": "Wan",
"doi-asserted-by": "publisher",
"first-page": "1139436",
"journal-title": "Front. Cell. Infect. Microbiol.",
"key": "B26",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.3892/etm.2016.3465",
"article-title": "Activation of AMPK attenuates LPS-induced acute lung injury by upregulation of PGC1α and SOD1",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1551",
"journal-title": "Exp. Ther. Med.",
"key": "B27",
"volume": "12",
"year": "2016"
},
{
"DOI": "10.7554/eLife.02242",
"article-title": "Metformin inhibits mitochondrial complex I of cancer cells to reduce tumorigenesis",
"author": "Wheaton",
"doi-asserted-by": "publisher",
"first-page": "e02242",
"journal-title": "eLife",
"key": "B28",
"volume": "3",
"year": "2014"
},
{
"DOI": "10.1016/j.cbi.2018.05.018",
"article-title": "Metformin alleviated endotoxemia-induced acute lung injury via restoring AMPK-dependent suppression of mTOR",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Chemico-biological Interact.",
"key": "B29",
"volume": "291",
"year": "2018"
},
{
"DOI": "10.1155/2019/1709718",
"article-title": "Metformin activates the protective effects of the AMPK pathway in acute lung injury caused by paraquat poisoning",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "1709718",
"journal-title": "Oxidative Med. Cell. Longev.",
"key": "B30",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.1016/j.immuni.2021.05.004",
"article-title": "Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation",
"author": "Xian",
"doi-asserted-by": "publisher",
"first-page": "1463",
"journal-title": "Immunity",
"key": "B31",
"volume": "54",
"year": "2021"
},
{
"DOI": "10.26355/eurrev_201808_15737",
"article-title": "Metformin relieves acute respiratory distress syndrome by reducing miR-138 expression",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "5355",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "B32",
"volume": "22",
"year": "2018"
},
{
"DOI": "10.3389/fphar.2022.811372",
"article-title": "Metformin regulates alveolar macrophage polarization to protect against acute lung injury in rats caused by paraquat poisoning",
"author": "Yuan",
"doi-asserted-by": "publisher",
"first-page": "811372",
"journal-title": "Front. Pharmacol.",
"key": "B33",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3892/etm.2022.11456",
"article-title": "Metformin mitigates gas explosion-induced blast lung injuries through AMPK-mediated energy metabolism and NOX2-related oxidation pathway in rats",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "529",
"journal-title": "Exp. Ther. Med.",
"key": "B34",
"volume": "24",
"year": ""
},
{
"DOI": "10.3389/fphar.2022.801337",
"article-title": "Metformin alleviates LPS-induced acute lung injury by regulating the SIRT1/NF-κB/NLRP3 pathway and inhibiting endothelial cell pyroptosis",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "801337",
"journal-title": "Front. Pharmacol.",
"key": "B35",
"volume": "13",
"year": ""
},
{
"DOI": "10.1038/nrendo.2017.151",
"article-title": "Global aetiology and epidemiology of type 2 diabetes mellitus and its complications",
"author": "Zheng",
"doi-asserted-by": "publisher",
"first-page": "88",
"journal-title": "Nat. Rev. Endocrinol.",
"key": "B36",
"volume": "14",
"year": "2018"
},
{
"DOI": "10.1038/s41586-018-0372-z",
"article-title": "New mitochondrial DNA synthesis enables NLRP3 inflammasome activation",
"author": "Zhong",
"doi-asserted-by": "publisher",
"first-page": "198",
"journal-title": "Nature",
"key": "B37",
"volume": "560",
"year": "2018"
},
{
"DOI": "10.1164/rccm.200710-1602OC",
"article-title": "Mitochondrial respiratory complex I regulates neutrophil activation and severity of lung injury",
"author": "Zmijewski",
"doi-asserted-by": "publisher",
"first-page": "168",
"journal-title": "Am. J. Respir. Crit. care Med.",
"key": "B38",
"volume": "178",
"year": "2008"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fphar.2023.1215307/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Pharmacology"
],
"subtitle": [],
"title": "Effects of metformin on acute respiratory distress syndrome in preclinical studies: a systematic review and meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "14"
}
