Shedding of mitochondrial Voltage-Dependent Anion Channel-1 (VDAC1) Reflects COVID-19 Severity and Reveals Macrophage Dysfunction
et al., bioRxiv, doi:10.1101/2025.07.07.663218, Jul 2025
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
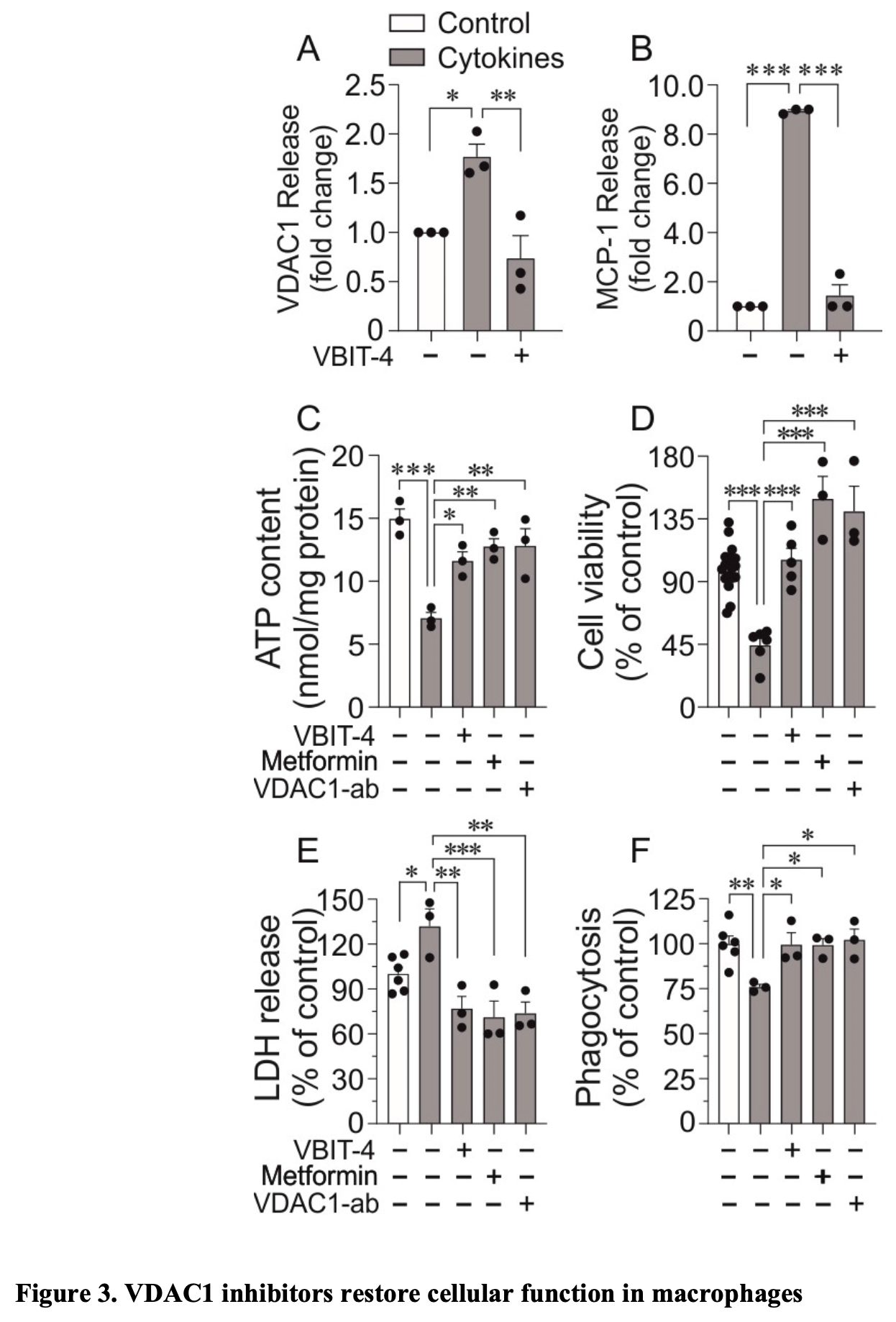
In vitro, ex vivo, and retrospective observational study showing that VDAC1 (Voltage-Dependent Anion Channel-1) levels reflect COVID-19 severity and that VDAC1 inhibitors (VBIT-4, metformin, and VDAC1-specific antibody) restore macrophage function. The results suggest serum VDAC1 as a biomarker for COVID-19 severity and VDAC1 inhibitors as potential therapeutic agents for severe COVID-19.
Sjögren et al., 8 Jul 2025, retrospective, USA, preprint, 8 authors.
Contact: s_albert.salehi@med.lu.se.
Shedding of mitochondrial Voltage-Dependent Anion Channel-1 (VDAC1) Reflects COVID-19 Severity and Reveals Macrophage Dysfunction
doi:10.1101/2025.07.07.663218
COVID-19 severity correlates with lymphopenia and increased pro-inflammatory cytokines. However, the dysfunction of tissue macrophages in COVID-19 patients during the inflammatory cytokine storm has not been fully elucidated. Hospitalized COVID-19 patients were divided into three groups based on their symptomatic severity: exhibiting mild, moderate, or severe symptoms. Patients exhibited successively increased serum levels of mitochondrial voltage-dependent anion channel 1 (VDAC1) at days 0, 3, 7, 10, and 14, returning to those of non-infected subjects at day 28. Serum level of VDAC1 was positively correlated with COVID-19 severity and with increased white blood cell (WBC), neutrophil, lymphocyte, procalcitonin (PCT), and gamma-glutamyltransferase (GT) levels. Peripheral blood mononuclear cells (PBMCs) from hospitalized COVID-19 patients showed increased VDAC1 content concomitant with a reduced ATP content. Culture of monocytes, isolated from healthy individuals, and differentiated into polarized M1 macrophages, together with a cytokine mixture (IL-1β, IFN-γ, and TNF-α), to mimic the inflammatory cytokine storm, for 24 h markedly increased VDAC1 and Monocyte chemoattractant protein-1 (MCP-1) release in culture medium. The presence of the cytokine mixture reduced the ATP content, cell viability, and the phagocytic capability of macrophages. Co-staining of VDAC1 and the plasma membrane marker Na + /K + -ATPase showed that cytokine-treatment mistargeted VDAC1 to the cell surface of macrophages. All these effects were prevented by VDAC1 inhibition using VBIT-4, VDAC1-specific antibody (VDAC1-ab), or metformin. Our findings indicate that increased VDAC1 expression and cell surface mistargeting in immune cells might be associated with cell dysfunction, potentially contributing to the severity of COVID-19 infection. .
Author contributions M.S. conceived and designed the experiments. M.S., A.S., and C.B.W. supervised the project. M.S., P.D., and A.S. performed the experiments and analysed the data. K.L. was involved as an immunologist and macrophage expert. M.R. collected the clinical samples, and A.N. purified the PBMC. M.S. and A.S. wrote the first draft of the manuscript, which was substantially revised by C.B.W. All co-authors proofread the manuscript and provided valuable suggestions. All clinical parameters are the median of the highest value for each patient (except for lymphocytes and platelets),
Declaration of Interests
Tables and Figures
Study where the lowest value for each patient is given. Group 1: Mild disease -No oxygen, Group 2: Moderate disease -1-6 L of oxygen/ minute, Group 3: Severe disease -More than 6 L of oxygen per minute.
References
Ajaz, Mcphail, Singh, Mujib, Trovato et al., Mitochondrial metabolic manipulation by SARS-CoV-2 in peripheral blood mononuclear cells of patients with COVID-19, Am J Physiol Cell Physiol
Akanda, Tofighi, Brask, Tamm, Elinder et al., Voltage-dependent anion channels (VDAC) in the plasma membrane play a critical role in apoptosis in differentiated hippocampal neurons but not in neural stem cells, Cell Cycle
Al-Amily, Sjögren, Duner, Tariq, Wollheim et al., Ablation of GPR56 Causes beta-Cell Dysfunction by ATP Loss through Mistargeting of Mitochondrial VDAC1 to the Plasma Membrane, Biomolecules
Arteaga-Blanco, Temerozo, Tine, Dantas-Pereira, Sacramento et al., Extracellular vesicles from primary human macrophages stimulated with VIP or PACAP mediate anti-SARS-CoV-2 activities in monocytes through NF-kappaB signaling pathway, Microbes Infect
Baik, Ramanujan, Becker, Fett, Underhill et al., Hexokinase dissociation from mitochondria promotes oligomerization of VDAC that facilitates NLRP3 inflammasome assembly and activation, Sci Immunol
Ben-Hail, Begas-Shvartz, Shalev, Shteinfer-Kuzmine, Gruzman et al., Novel Compounds Targeting the Mitochondrial Protein VDAC1 Inhibit Apoptosis and Protect against Mitochondrial Dysfunction, J Biol Chem
Bhowal, Ghosh, Ghatak, De, Pathophysiological involvement of host mitochondria in SARS-CoV-2 infection that causes COVID-19: a comprehensive evidential insight, Mol Cell Biochem
Bisen, Agrawal, Sanap, Ravi Kumar, Kumar et al., COVID-19 retreats and world recovers: A silver lining in the dark cloud, Health Care Sci
Bläckberg, Fernström, Sarbrant, Rasmussen, Sunnerhagen, Antibody kinetics and clinical course of COVID-19 a prospective observational study, PLoS One
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Lancet Healthy Longev
Campbell, Colgan, Neutrophils and inflammatory metabolism in antimicrobial functions of the mucosa, J Leukoc Biol
Chen, Liu, Liu, Liu, Liu et al., Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia, Zhonghua Jie He He Hu Xi Za Zhi
Codo, Davanzo, Monteiro, Souza, Muraro et al., Elevated Glucose Levels Favor SARS-CoV-2 Infection and Monocyte Response through a HIF-1alpha/Glycolysis-Dependent Axis, Cell Metab
Cory, Emmons, Yarbro, Davis, Pence, Metformin Suppresses Monocyte Immunometabolic Activation by SARS-CoV-2 Spike Protein Subunit 1, Front Immunol
Crouse, Grimes, Li, Might, Ovalle et al., Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes, Front Endocrinol
Dharra, Sharma, Datta, Emerging aspects of cytokine storm in COVID-19: The role of proinflammatory cytokines and therapeutic prospects, Cytokine
Duner, Salehi, COVID-19 and possible pharmacological preventive options, Journal of Clinical Medicine Research
Emelyanova, Bai, Yan, Bosnjak, Kress et al., Biphasic effect of metformin on human cardiac energetics, Transl Res
Faraj, IL1beta, IL-6, and TNF-alpha cytokines cooperate to modulate a complicated medical condition among COVID-19 patients: case-control study, Ann Med Surg (Lond)
Ferreira, Soares, De Azevedo-Quintanilha, Dias, Fintelman-Rodrigues et al., SARS-CoV-2 engages inflammasome and pyroptosis in human primary monocytes, Cell Death Discov
Guan, Zheng, Song, He, Xu et al., MAVS regulates apoptotic cell death by decreasing K48linked ubiquitination of voltage-dependent anion channel 1, Mol Cell Biol
Guarino, Zinghirino, Mela, Pappalardo, Ichas et al., NRF-1 and HIF-1alpha contribute to modulation of human VDAC1 gene promoter during starvation and hypoxia in HeLa cells, Biochim Biophys Acta Bioenerg
Guarnieri, Dybas, Fazelinia, Kim, Frere et al., Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts, Sci Transl Med
Guarnieri, Haltom, Albrecht, Lie, Olali et al., SARS-CoV-2 mitochondrial metabolic and epigenomic reprogramming in COVID-19, Pharmacol Res
Gunnarsdottir, Hagerling, Bergenfelz, Mehmeti, Kallberg et al., Inflammatory macrophage derived TNFalpha downregulates estrogen receptor alpha via FOXO3a inactivation in human breast cancer cells, Exp Cell Res
Gurshaney, Morales-Alvarez, Ezhakunnel, Manalo, Huynh et al., Metabolic dysregulation impairs lymphocyte function during severe SARS-CoV-2 infection, Commun Biol
Hu, Guo, Overholser, Wang, Mitochondrial VDAC1: A Potential Therapeutic Target of Inflammation-Related Diseases and Clinical Opportunities, Cells
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Huang, Yin, Pan, Huang, Chen et al., The Interaction between SARS-CoV-2 Nucleocapsid Protein and UBC9 Inhibits MAVS Ubiquitination by Enhancing Its SUMOylation, Viruses
Junqueira, Crespo, Ranjbar, De Lacerda, Lewandrowski et al., FcgammaR-mediated SARS-CoV-2 infection of monocytes activates inflammation, Nature
Karki, Sharma, Tuladhar, Williams, Zalduondo et al., Synergism of TNF-alpha and IFN-gamma Triggers Inflammatory Cell Death, Tissue Damage, and Mortality in SARS-CoV-2 Infection and Cytokine Shock Syndromes, Cell
Kim, Gupta, Blanco, Yang, Shteinfer-Kuzmine et al., VDAC oligomers form mitochondrial pores to release mtDNA fragments and promote lupus-like disease, Science
Kumar, Nagarajan, Uchil, Analysis of Cell Viability by the Lactate Dehydrogenase Assay, Cold Spring Harb Protoc
Li, Yao, Gu, Che, Ma et al., Plasminogen kringle 5 induces endothelial cell apoptosis by triggering a voltage-dependent anion channel 1 (VDAC1) positive feedback loop, J Biol Chem
Lindeboom, Worlock, Dratva, Yoshida, Scobie et al., Human SARS-CoV-2 challenge uncovers local and systemic response dynamics, Nature
Majtnerova, Capek, Petira, Handl, Rousar, Quantitative spectrofluorometric assay detecting nuclear condensation and fragmentation in intact cells, Sci Rep
Mccarthy, Metformin as a potential treatment for COVID-19, Expert Opin Pharmacother
Neumann, Kuteykin-Teplyakov, Heumann, Neuronal Protection by Ha-RAS-GTPase Signaling through Selective Downregulation of Plasmalemmal Voltage-Dependent Anion Channel-1, Int J Mol Sci
Nomani, Varahram, Tabarsi, Hashemian, Jamaati et al., Decreased neutrophil-mediated bacterial killing in COVID-19 patients, Scand J Immunol
Parkos, Neutrophil-Epithelial Interactions: A Double-Edged Sword, Am J Pathol
Peyneau, Granger, Wicky, Khelifi-Touhami, Timsit et al., Innate immune deficiencies are associated with severity and poor prognosis in patients with COVID-19, Sci Rep
Sefik, Qu, Junqueira, Kaffe, Mirza et al., Inflammasome activation in infected macrophages drives COVID-19 pathology, Nature
Shalova, Lim, Chittezhath, Zinkernagel, Beasley et al., Human monocytes undergo functional re-programming during sepsis mediated by hypoxia-inducible factor-1alpha, Immunity
Shoshan-Barmatz, Pinto, Zweckstetter, Raviv, Keinan et al., VDAC, a multi-functional mitochondrial protein regulating cell life and death, Mol Aspects Med
Shoshan-Barmatz, Shteinfer-Kuzmine, Verma, VDAC1 at the Intersection of Cell Metabolism, Apoptosis, and Diseases, Biomolecules
Shteinfer-Kuzmine, Verma, Bornshten, Ben Chetrit, Ben-Ya'acov et al., Elevated serum mtDNA in COVID-19 patients is linked to SARS-CoV-2 envelope protein targeting mitochondrial VDAC1, inducing apoptosis and mtDNA release, Apoptosis
Singh, Chaubey, Chen, Suravajhala, Decoding SARS-CoV-2 hijacking of host mitochondria in COVID-19 pathogenesis, Am J Physiol Cell Physiol
Smilansky, Dangoor, Nakdimon, Ben-Hail, Mizrachi et al., The Voltage-dependent Anion Channel 1 Mediates Amyloid beta Toxicity and Represents a Potential Target for Alzheimer Disease Therapy, J Biol Chem
Smith, Hartley, Cocheme, Murphy, Mitochondrial pharmacology, Trends in pharmacological sciences
Tariq, Sjögren, Salehi, Sulindac prevents increased mitochondrial VDAC1 expression and cell surface mistargeting induced by pathological conditions in retinal cells, Biochem Biophys Res Commun
Thompson, Cascino, Ordonez, Zhou, Vaghasia et al., Metabolic programs define dysfunctional immune responses in severe COVID-19 patients, Cell Rep
Tomasello, Messina, Lartigue, Schembri, Medina et al., Outer membrane VDAC1 controls permeability transition of the inner mitochondrial membrane in cellulo during stress-induced apoptosis, Cell Res
Valle, Kim-Schulze, Huang, Beckmann, Nirenberg et al., An inflammatory cytokine signature predicts COVID-19 severity and survival, Nat Med
Verma, Pittala, Alhozeel, Shteinfer-Kuzmine, Ohana et al., The role of the mitochondrial protein VDAC1 in inflammatory bowel disease: a potential therapeutic target, Mol Ther
Vora, Lieberman, Wu, Inflammasome activation at the crux of severe COVID-19, Nat Rev Immunol
Wang, Zhao, Liu, Li, SARS-CoV-2 modulation of RIG-I-MAVS signaling: Potential mechanisms of impairment on host antiviral immunity and therapeutic approaches, MedComm Futur Med
Xian, Karin, Oxidized mitochondrial DNA: a protective signal gone awry, Trends Immunol
Xian, Liu, Rundberg Nilsson, Gatchalian, Crother et al., Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation, Immunity
Xian, Watari, Sanchez-Lopez, Offenberger, Onyuru et al., Oxidized DNA fragments exit mitochondria via mPTP-and VDAC-dependent channels to activate NLRP3 inflammasome and interferon signaling, Immunity
Ye, Wang, Mao, The pathogenesis and treatment of the `Cytokine Storm' in COVID-19, J Infect
Yeung-Luk, Narayanan, Ghosh, Wally, Lee et al., SARS-CoV-2 infection alters mitochondrial and cytoskeletal function in human respiratory epithelial cells mediated by expression of spike protein, mBio
Zhang, Al-Amily, Mohammed, Luan, Asplund et al., Preserving Insulin Secretion in Diabetes by Inhibiting VDAC1 Overexpression and Surface Translocation in beta Cells, Cell Metab
Zhang, Mears, Shakib, Beynor, Shanaj et al., IFN-gamma and TNF-alpha drive a CXCL10 + CCL2 + macrophage phenotype expanded in severe COVID-19 and other diseases with tissue inflammation, bioRxiv
Zhu, Cai, Fan, Lou, Hua et al., Clinical value of immuneinflammatory parameters to assess the severity of coronavirus disease 2019, Int J Infect Dis
DOI record:
{
"DOI": "10.1101/2025.07.07.663218",
"URL": "http://dx.doi.org/10.1101/2025.07.07.663218",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>COVID-19 severity correlates with lymphopenia and increased pro-inflammatory cytokines. However, the dysfunction of tissue macrophages in COVID-19 patients during the inflammatory cytokine storm has not been fully elucidated.</jats:p>\n <jats:p>Hospitalized COVID-19 patients were divided into three groups based on their symptomatic severity: exhibiting mild, moderate, or severe symptoms. Patients exhibited successively increased serum levels of mitochondrial voltage-dependent anion channel 1 (VDAC1) at days 0, 3, 7, 10, and 14, returning to those of non-infected subjects at day 28. Serum level of VDAC1 was positively correlated with COVID-19 severity and with increased white blood cell (WBC), neutrophil, lymphocyte, procalcitonin (PCT), and gamma-glutamyltransferase (GT) levels. Peripheral blood mononuclear cells (PBMCs) from hospitalized COVID-19 patients showed increased VDAC1 content concomitant with a reduced ATP content.</jats:p>\n <jats:p>Culture of monocytes, isolated from healthy individuals, and differentiated into polarized M1 macrophages, together with a cytokine mixture (IL-1β, IFN-γ, and TNF-α), to mimic the inflammatory cytokine storm, for 24 h markedly increased VDAC1 and Monocyte chemoattractant protein-1 (MCP-1) release in culture medium. The presence of the cytokine mixture reduced the ATP content, cell viability, and the phagocytic capability of macrophages. Co-staining of VDAC1 and the plasma membrane marker Na<jats:sup>+</jats:sup>/K<jats:sup>+</jats:sup>-ATPase showed that cytokine-treatment mistargeted VDAC1 to the cell surface of macrophages. All these effects were prevented by VDAC1 inhibition using VBIT-4, VDAC1-specific antibody (VDAC1-ab), or metformin.</jats:p>\n <jats:p>Our findings indicate that increased VDAC1 expression and cell surface mistargeting in immune cells might be associated with cell dysfunction, potentially contributing to the severity of COVID-19 infection.</jats:p>\n <jats:p>The data also indicate serum VDAC1 as a biomarker of COVID-19 severity and the use of VDAC1 inhibitors as potential drug candidates restoring macrophages and PBMCs function in individuals severely affected by COVID-19.</jats:p>",
"accepted": {
"date-parts": [
[
2025,
7,
8
]
]
},
"author": [
{
"ORCID": "https://orcid.org/0000-0003-3443-4539",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sjögren",
"given": "Marie",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0003-4171-5646",
"affiliation": [],
"authenticated-orcid": false,
"family": "Dunér",
"given": "Pontus",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-8081-2142",
"affiliation": [],
"authenticated-orcid": false,
"family": "De Marinis",
"given": "Yang",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-8636-730X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Neumann",
"given": "Ariane",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-8254-3137",
"affiliation": [],
"authenticated-orcid": false,
"family": "Leandersson",
"given": "Karin",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-1588-5473",
"affiliation": [],
"authenticated-orcid": false,
"family": "Rasmussen",
"given": "Magnus",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-4570-9879",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wollheim",
"given": "Claes B.",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-6120-3539",
"affiliation": [],
"authenticated-orcid": false,
"family": "Salehi",
"given": "Albert",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
7,
11
]
],
"date-time": "2025-07-11T04:00:26Z",
"timestamp": 1752206426000
},
"deposited": {
"date-parts": [
[
2025,
7,
11
]
],
"date-time": "2025-07-11T04:00:35Z",
"timestamp": 1752206435000
},
"group-title": "Pathology",
"indexed": {
"date-parts": [
[
2025,
7,
11
]
],
"date-time": "2025-07-11T04:40:01Z",
"timestamp": 1752208801532,
"version": "3.41.2"
},
"institution": [
{
"name": "bioRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
7,
8
]
]
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
7,
8
]
],
"date-time": "2025-07-08T00:00:00Z",
"timestamp": 1751932800000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2025.07.07.663218",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2025,
7,
8
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2025,
7,
8
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference": [
{
"DOI": "10.1152/ajpcell.00426.2020",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.1"
},
{
"DOI": "10.4161/cc.7.20.6831",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.2"
},
{
"DOI": "10.1016/j.micinf.2024.105400",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.3",
"unstructured": "Arteaga-Blanco, L. A. , J. R. Temerozo , L. P. S. Tine , L. Dantas-Pereira , C. Q. Sacramento , N. Fintelman-Rodrigues , B. M. Toja , S. S. Gomes Dias , C. S. de Freitas , C. C. Espirito-Santo , Y. P. Silva , R. L. Frozza , P. T. Bozza , R. F. S. Menna-Barreto , T. M. L. Souza , and D. C. Bou- Habib . 2024. ’Extracellular vesicles from primary human macrophages stimulated with VIP or PACAP mediate anti-SARS-CoV-2 activities in monocytes through NF-kappaB signaling pathway’, Microbes Infect: 105400."
},
{
"DOI": "10.1126/sciimmunol.ade7652",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.4",
"unstructured": "Baik, S. H. , V. K. Ramanujan , C. Becker , S. Fett , D. M. Underhill , and A. J. Wolf . 2023. ’Hexokinase dissociation from mitochondria promotes oligomerization of VDAC that facilitates NLRP3 inflammasome assembly and activation’, Sci Immunol, 8: eade7652."
},
{
"DOI": "10.1074/jbc.M116.744284",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.5"
},
{
"DOI": "10.1007/s11010-022-04593-z",
"article-title": "Pathophysiological involvement of host mitochondria in SARS-CoV-2 infection that causes COVID-19: a comprehensive evidential insight",
"doi-asserted-by": "crossref",
"first-page": "1325",
"journal-title": "Mol Cell Biochem",
"key": "2025071021001985000_2025.07.07.663218v1.6",
"volume": "478",
"year": "2023"
},
{
"DOI": "10.1002/hcs2.57",
"article-title": "COVID-19 retreats and world recovers: A silver lining in the dark cloud",
"doi-asserted-by": "crossref",
"first-page": "264",
"journal-title": "Health Care Sci",
"key": "2025071021001985000_2025.07.07.663218v1.7",
"volume": "2",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0248918",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.8"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis",
"doi-asserted-by": "crossref",
"first-page": "e34",
"journal-title": "Lancet Healthy Longev",
"key": "2025071021001985000_2025.07.07.663218v1.9",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1189/jlb.3MR1114-556R",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.10"
},
{
"article-title": "[Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia]",
"first-page": "203",
"journal-title": "Zhonghua Jie He He Hu Xi Za Zhi",
"key": "2025071021001985000_2025.07.07.663218v1.11",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.07.007",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.12"
},
{
"DOI": "10.3389/fimmu.2021.733921",
"article-title": "Metformin Suppresses Monocyte Immunometabolic Activation by SARS-CoV-2 Spike Protein Subunit 1",
"doi-asserted-by": "crossref",
"first-page": "733921",
"journal-title": "Front Immunol",
"key": "2025071021001985000_2025.07.07.663218v1.13",
"volume": "12",
"year": "2021"
},
{
"article-title": "Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes",
"first-page": "600439",
"journal-title": "Front Endocrinol (Lausanne",
"key": "2025071021001985000_2025.07.07.663218v1.14",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/S41591-020-1051-9",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.15"
},
{
"DOI": "10.1016/j.cyto.2023.156287",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.16"
},
{
"DOI": "10.14740/jocmr4383",
"article-title": "COVID-19 and possible pharmacological preventive options",
"doi-asserted-by": "crossref",
"first-page": "758",
"journal-title": "Journal of Clinical Medicine Research",
"key": "2025071021001985000_2025.07.07.663218v1.17",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.trsl.2020.10.002",
"article-title": "Biphasic effect of metformin on human cardiac energetics",
"doi-asserted-by": "crossref",
"first-page": "5",
"journal-title": "Transl Res",
"key": "2025071021001985000_2025.07.07.663218v1.18",
"volume": "229",
"year": "2021"
},
{
"DOI": "10.1097/MS9.0000000000000679",
"article-title": "IL1beta, IL-6, and TNF-alpha cytokines cooperate to modulate a complicated medical condition among COVID-19 patients: case-control study",
"doi-asserted-by": "crossref",
"first-page": "2291",
"journal-title": "Ann Med Surg (Lond",
"key": "2025071021001985000_2025.07.07.663218v1.19",
"volume": "85",
"year": "2023"
},
{
"DOI": "10.1038/s41420-021-00428-w",
"article-title": "SARS-CoV-2 engages inflammasome and pyroptosis in human primary monocytes",
"doi-asserted-by": "crossref",
"first-page": "43",
"journal-title": "Cell Death Discov",
"key": "2025071021001985000_2025.07.07.663218v1.20",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1128/MCB.00030-13",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.21"
},
{
"DOI": "10.1016/j.bbabio.2020.148289",
"article-title": "NRF-1 and HIF-1alpha contribute to modulation of human VDAC1 gene promoter during starvation and hypoxia in HeLa cells",
"doi-asserted-by": "crossref",
"first-page": "148289",
"journal-title": "Biochim Biophys Acta Bioenerg",
"key": "2025071021001985000_2025.07.07.663218v1.22",
"volume": "1861",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abq1533",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.23",
"unstructured": "Guarnieri, J. W. , J. M. Dybas , H. Fazelinia , M. S. Kim , J. Frere , Y. Zhang , Y. Soto Albrecht , D. G. Murdock , A. Angelin , L. N. Singh , S. L. Weiss , S. M. Best , M. T. Lott , S. Zhang , H. Cope , V. Zaksas , A. Saravia-Butler , C. Meydan , J. Foox , C. Mozsary , Y. Bram , Y. Kidane , W. Priebe , M. R. Emmett , R. Meller , S. Demharter , V. Stentoft-Hansen , M. Salvatore , D. Galeano , F. J. Enguita , P. Grabham , N. S. Trovao , U. Singh , J. Haltom , M. T. Heise , N. J. Moorman , V. K. Baxter , E. A. Madden , S. A. Taft-Benz , E. J. Anderson , W. A. Sanders , R. J. Dickmander , S. B. Baylin , E. S. Wurtele , P. M. Moraes-Vieira , D. Taylor , C. E. Mason , J. C. Schisler , R. E. Schwartz , A. Beheshti , and D. C. Wallace . 2023. ’Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts’, Sci Transl Med, 15: eabq1533."
},
{
"DOI": "10.1016/j.phrs.2024.107170",
"article-title": "SARS-CoV-2 mitochondrial metabolic and epigenomic reprogramming in COVID-19",
"doi-asserted-by": "crossref",
"first-page": "107170",
"journal-title": "Pharmacol Res",
"key": "2025071021001985000_2025.07.07.663218v1.24",
"volume": "204",
"year": "2024"
},
{
"DOI": "10.1016/j.yexcr.2020.111932",
"article-title": "Inflammatory macrophage derived TNFalpha downregulates estrogen receptor alpha via FOXO3a inactivation in human breast cancer cells",
"doi-asserted-by": "crossref",
"first-page": "111932",
"journal-title": "Exp Cell Res",
"key": "2025071021001985000_2025.07.07.663218v1.25",
"volume": "390",
"year": "2020"
},
{
"DOI": "10.1038/s42003-023-04730-4",
"article-title": "Metabolic dysregulation impairs lymphocyte function during severe SARS-CoV-2 infection",
"doi-asserted-by": "crossref",
"first-page": "374",
"journal-title": "Commun Biol",
"key": "2025071021001985000_2025.07.07.663218v1.26",
"volume": "6",
"year": "2023"
},
{
"DOI": "10.3390/cells11193174",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.27",
"unstructured": "Hu, H. , L. Guo , J. Overholser , and X. Wang . 2022. ’Mitochondrial VDAC1: A Potential Therapeutic Target of Inflammation-Related Diseases and Clinical Opportunities’, Cells, 11."
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.28"
},
{
"DOI": "10.3390/v15122304",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.29",
"unstructured": "Huang, C. , Y. Yin , P. Pan , Y. Huang , S. Chen , J. Chen , J. Wang , G. Xu , X. Tao , X. Xiao , J. Li , J. Yang , Z. Jin , B. Li , Z. Tong , W. Du , L. Liu , and Z. Liu . 2023. ’The Interaction between SARS-CoV-2 Nucleocapsid Protein and UBC9 Inhibits MAVS Ubiquitination by Enhancing Its SUMOylation’, Viruses, 15."
},
{
"DOI": "10.1038/s41586-022-04702-4",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.30"
},
{
"DOI": "10.1016/j.cell.2020.11.025",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.31"
},
{
"DOI": "10.1126/science.aav4011",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.32"
},
{
"DOI": "10.1101/pdb.prot095497",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.33",
"unstructured": "Kumar, P. , A. Nagarajan , and P. D. Uchil . 2018. ’Analysis of Cell Viability by the Lactate Dehydrogenase Assay’, Cold Spring Harb Protoc, 2018."
},
{
"DOI": "10.1074/jbc.M114.567792",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.34"
},
{
"DOI": "10.1038/s41586-024-07575-x",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.35"
},
{
"DOI": "10.1038/s41598-021-91380-3",
"article-title": "Quantitative spectrofluorometric assay detecting nuclear condensation and fragmentation in intact cells",
"doi-asserted-by": "crossref",
"first-page": "11921",
"journal-title": "Sci Rep",
"key": "2025071021001985000_2025.07.07.663218v1.36",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1080/14656566.2023.2215385",
"article-title": "Metformin as a potential treatment for COVID-19",
"doi-asserted-by": "crossref",
"first-page": "1199",
"journal-title": "Expert Opin Pharmacother",
"key": "2025071021001985000_2025.07.07.663218v1.37",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.3390/biom13030557",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.38",
"unstructured": "Mohammad Al-Amily, I. , M. Sjögren , P. Duner , M. Tariq , C. B. Wollheim , and A. Salehi . 2023. ’Ablation of GPR56 Causes beta-Cell Dysfunction by ATP Loss through Mistargeting of Mitochondrial VDAC1 to the Plasma Membrane’, Biomolecules, 13."
},
{
"DOI": "10.3390/ijms25053030",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.39",
"unstructured": "Neumann, S. , K. Kuteykin-Teplyakov , and R. Heumann . 2024. ’Neuronal Protection by Ha-RAS- GTPase Signaling through Selective Downregulation of Plasmalemmal Voltage-Dependent Anion Channel-1’, Int J Mol Sci, 25."
},
{
"DOI": "10.1111/sji.13083",
"article-title": "Decreased neutrophil-mediated bacterial killing in COVID- 19 patients",
"doi-asserted-by": "crossref",
"first-page": "e13083",
"journal-title": "Scand J Immunol",
"key": "2025071021001985000_2025.07.07.663218v1.40",
"volume": "94",
"year": "2021"
},
{
"DOI": "10.1016/j.ajpath.2016.02.001",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.41"
},
{
"DOI": "10.1038/s41598-021-04705-7",
"article-title": "Innate immune deficiencies are associated with severity and poor prognosis in patients with COVID-19",
"doi-asserted-by": "crossref",
"first-page": "638",
"journal-title": "Sci Rep",
"key": "2025071021001985000_2025.07.07.663218v1.42",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1038/s41586-022-04802-1",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.43"
},
{
"DOI": "10.1016/j.immuni.2015.02.001",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.44"
},
{
"DOI": "10.1016/j.mam.2010.03.002",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.45"
},
{
"DOI": "10.3390/biom10111485",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.46",
"unstructured": "Shoshan-Barmatz, V. , A. Shteinfer-Kuzmine , and A. Verma . 2020. ’VDAC1 at the Intersection of Cell Metabolism, Apoptosis, and Diseases’, Biomolecules, 10."
},
{
"DOI": "10.1007/s10495-024-02025-5",
"article-title": "Elevated serum mtDNA in COVID-19 patients is linked to SARS-CoV-2 envelope protein targeting mitochondrial VDAC1, inducing apoptosis and mtDNA release’",
"doi-asserted-by": "crossref",
"first-page": "2025",
"journal-title": "Apoptosis",
"key": "2025071021001985000_2025.07.07.663218v1.47",
"volume": "29",
"year": "2024"
},
{
"DOI": "10.1152/ajpcell.00224.2020",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.48"
},
{
"DOI": "10.1074/jbc.M115.691493",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.49"
},
{
"DOI": "10.1016/j.tips.2012.03.010",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.50"
},
{
"DOI": "10.1016/j.bbrc.2024.150558",
"article-title": "Sulindac prevents increased mitochondrial VDAC1 expression and cell surface mistargeting induced by pathological conditions in retinal cells",
"doi-asserted-by": "crossref",
"first-page": "150558",
"journal-title": "Biochem Biophys Res Commun",
"key": "2025071021001985000_2025.07.07.663218v1.51",
"volume": "739",
"year": "2024"
},
{
"DOI": "10.1016/j.celrep.2021.108863",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.52",
"unstructured": "Thompson, E. A. , K. Cascino , A. A. Ordonez , W. Zhou , A. Vaghasia , A. Hamacher-Brady , N. R. Brady , I. H. Sun , R. Wang , A. Z. Rosenberg , M. Delannoy , R. Rothman , K. Fenstermacher , L. Sauer , K. Shaw-Saliba , E. M. Bloch , A. D. Redd , A. A. R. Tobian , M. Horton , K. Smith , A. Pekosz , F. R. D’Alessio, S. Yegnasubramanian, H. Ji, A. L. Cox, and J. D. Powell. 2021. ’Metabolic programs define dysfunctional immune responses in severe COVID-19 patients’, Cell Rep, 34: 108863."
},
{
"DOI": "10.1038/cr.2009.98",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.53"
},
{
"DOI": "10.1016/j.ymthe.2021.06.024",
"article-title": "The role of the mitochondrial protein VDAC1 in inflammatory bowel disease: a potential therapeutic target",
"doi-asserted-by": "crossref",
"first-page": "726",
"journal-title": "Mol Ther",
"key": "2025071021001985000_2025.07.07.663218v1.54",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.1038/s41577-021-00588-x",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.55"
},
{
"DOI": "10.1002/mef2.29",
"article-title": "SARS-CoV-2 modulation of RIG-I-MAVS signaling: Potential mechanisms of impairment on host antiviral immunity and therapeutic approaches",
"doi-asserted-by": "crossref",
"first-page": "e29",
"journal-title": "MedComm Futur Med",
"key": "2025071021001985000_2025.07.07.663218v1.56",
"volume": "1",
"year": "2022"
},
{
"DOI": "10.1016/j.it.2023.01.006",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.57"
},
{
"DOI": "10.1016/j.immuni.2021.05.004",
"article-title": "Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation",
"doi-asserted-by": "crossref",
"first-page": "1463",
"journal-title": "Immunity",
"key": "2025071021001985000_2025.07.07.663218v1.58",
"volume": "54",
"year": "2021"
},
{
"DOI": "10.1016/j.immuni.2022.06.007",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.59"
},
{
"DOI": "10.1016/j.jinf.2020.03.037",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.60",
"unstructured": "Ye, Q. , B. Wang , and J. Mao . 2020. ’The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID- 19’, J Infect."
},
{
"article-title": "SARS-CoV-2 infection alters mitochondrial and cytoskeletal function in human respiratory epithelial cells mediated by expression of spike protein",
"first-page": "e0082023",
"journal-title": "mBio",
"key": "2025071021001985000_2025.07.07.663218v1.61",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1016/j.cmet.2018.09.008",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.62"
},
{
"DOI": "10.1101/2020.08.05.238360",
"doi-asserted-by": "crossref",
"key": "2025071021001985000_2025.07.07.663218v1.63",
"unstructured": "Zhang, F. , J. R. Mears , L. Shakib , J. I. Beynor , S. Shanaj , I. Korsunsky , A. Nathan , Arthritis Accelerating Medicines Partnership Rheumatoid, Consortium Systemic Lupus Erythematosus, L. T. Donlin, and S. Raychaudhuri. 2020. ’IFN- gamma and TNF- alpha drive a CXCL10 + CCL2 + macrophage phenotype expanded in severe COVID-19 and other diseases with tissue inflammation’, bioRxiv."
},
{
"DOI": "10.1016/j.ijid.2020.04.041",
"doi-asserted-by": "publisher",
"key": "2025071021001985000_2025.07.07.663218v1.64"
}
],
"reference-count": 64,
"references-count": 64,
"relation": {},
"resource": {
"primary": {
"URL": "http://biorxiv.org/lookup/doi/10.1101/2025.07.07.663218"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "Shedding of mitochondrial Voltage-Dependent Anion Channel-1 (VDAC1) Reflects COVID-19 Severity and Reveals Macrophage Dysfunction",
"type": "posted-content"
}
