Vitamin D Status and Mortality from SARS CoV-2: A Prospective Study of Unvaccinated Caucasian Adults
et al., Nutrients, doi:10.3390/nu14163252, Aug 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 232 hospitalized COVID-19 pneumonia patients, showing higher risk of mortality with vitamin D deficiency.
This is the 143rd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
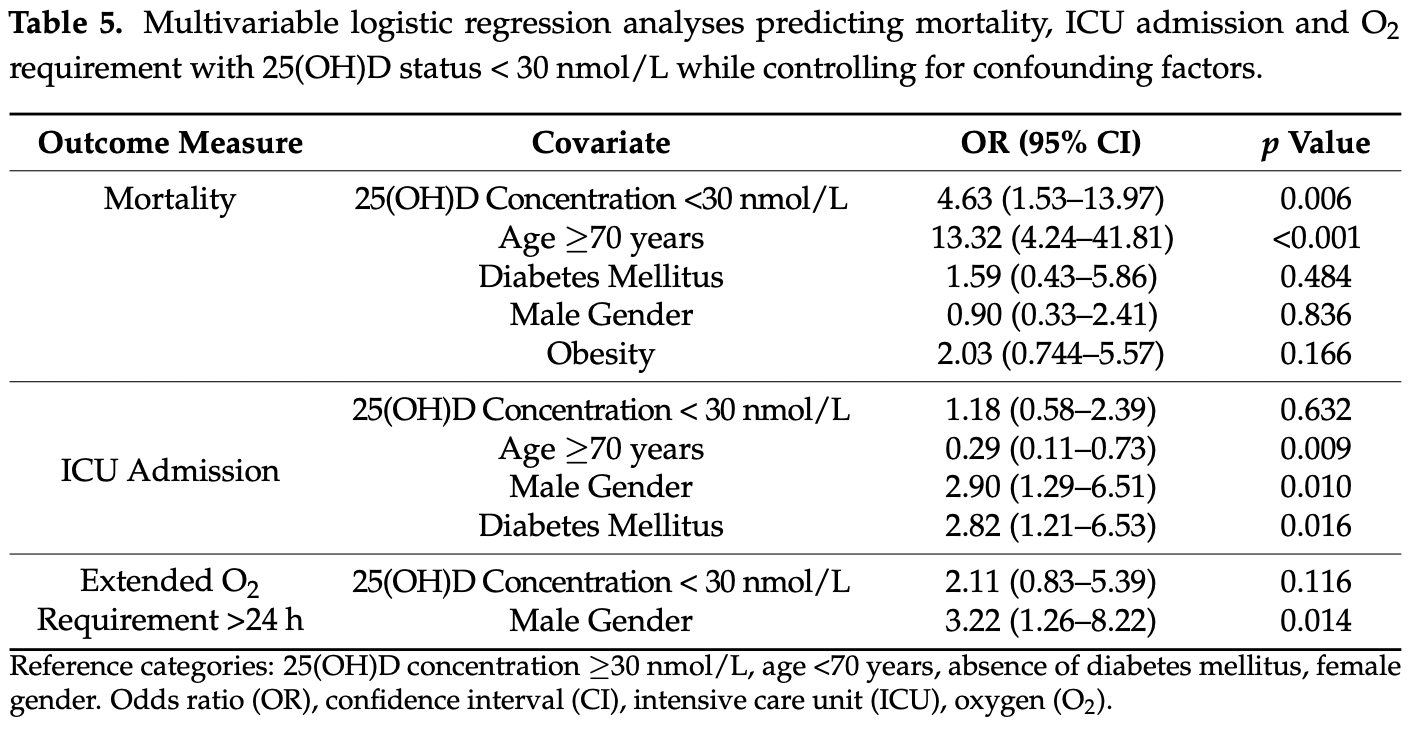
risk of death, 78.4% lower, OR 0.22, p = 0.006, high D levels (≥30nmol/L) 144, low D levels (<30nmol/L) 88, adjusted per study, inverted to make OR<1 favor high D levels (≥30nmol/L), multivariable, RR approximated with OR.
|
|
risk of ICU admission, 15.3% lower, OR 0.85, p = 0.63, high D levels (≥30nmol/L) 144, low D levels (<30nmol/L) 88, adjusted per study, inverted to make OR<1 favor high D levels (≥30nmol/L), multivariable, RR approximated with OR.
|
|
risk of progression, 52.6% lower, OR 0.47, p = 0.12, high D levels (≥30nmol/L) 144, low D levels (<30nmol/L) 88, adjusted per study, inverted to make OR<1 favor high D levels (≥30nmol/L), extended oxygen requirement, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Barrett et al., 9 Aug 2022, prospective, Ireland, peer-reviewed, mean age 56.0, 19 authors, study period March 2020 - April 2021.
Contact: johnfaul@rcsi.ie (corresponding author).
Vitamin D Status and Mortality from SARS CoV-2: A Prospective Study of Unvaccinated Caucasian Adults
Nutrients, doi:10.3390/nu14163252
COVID-19 and a low vitamin D state share common risk factors, which might explain why vitamin D deficiency has been linked with higher COVID-19 mortality. Moreover, measures of serum vitamin D may become lower during systemic inflammatory responses, further confounding the association via reverse causality. In this prospective study (recruited over 12 months), we examined whether the association between a low vitamin D state and in-hospital mortality due to SARS-CoV-2 pneumonia in unvaccinated subjects is explained by (i) the presence of shared risk factors (e.g., obesity, advanced age) or (ii) a reduction in serum 25(OH)D due to COVID-19 (i.e., reverse causality). In this cohort of 232 (mean age = 56 years) patients (all had SARS-CoV-2 diagnosed via PCR AND required supplemental oxygen therapy), we failed to find an association between serum vitamin D and levels of CRP, or other inflammatory markers. However, the hazard ratio for mortality for subjects over 70 years of age (13.2) and for subjects with a serum 25(OH)D level less than 30 nmol•L −1 (4.6) remained significantly elevated even after adjustment for gender, obesity and the presence of diabetes mellitus. Subjects <70 years and >70 years had significantly higher mortality with a serum 25(OH)D less than 30 nmol•L −1 (11.8% and 55%), than with a serum 25(OH)D greater than 30 nmol•L −1 (2.2% and 25%). Unvaccinated Caucasian adults with a low vitamin D state have higher mortality due to SARS CoV-2 pneumonia, which is not explained by confounders and is not closely linked with elevated serum CRP.
References
Akbar, Wibowo, Pranata, Setiabudiawan, Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated With Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis, Front. Nutr, doi:10.3389/fnut.2021.660420
Angelidi, Belanger, Lorinsky, Karamanis, Chamorro-Pareja et al., Vitamin D Status Is Associated With In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients, Mayo Clin. Proc, doi:10.1016/j.mayocp.2021.01.001
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study, Nutrients, doi:10.3390/nu12113377
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med. J, doi:10.1136/postgradmedj-2020-138712
Benskin, A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency, Front. Public Health, doi:10.3389/fpubh.2020.00513
Bian, Jin, Shou, Effects of Monthly Intramuscular High-Dose Vitamin D2 on Serum 25-Hydroxyvitamin D and Immune Parameters in Very Elderly Chinese Patients with Vitamin D Deficiency, Int. J. Endocrinol, doi:10.1155/2021/1343913
Black, Walton, Flynn, Cashman, Kiely, Small Increments in Vitamin D Intake by Irish Adults over a Decade Show That Strategic Initiatives to Fortify the Food Supply Are Needed, J. Nutr, doi:10.3945/jn.114.209106
Borsche, Glauner, Von Mendel, COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu13103596
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy, BMC Infect. Dis, doi:10.1186/s12879-021-06281-7
Cashman, Muldowney, Mcnulty, Nugent, Fitzgerald et al., Vitamin D status of Irish adults: Findings from the National Adult Nutrition Survey, Br. J. Nutr, doi:10.1017/S0007114512003212
Charoenngam, Holick, Immunologic Effects of Vitamin D on Human Health and Disease, Nutrients, doi:10.3390/nu12072097
De Smet, De Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality, Am. J. Clin. Pathol, doi:10.1093/ajcp/aqaa252
Efird, Anderson, Jindal, Redding, Thompson et al., The Interaction of Vitamin D and Corticosteroids: A Mortality Analysis of 26,508 Veterans Who Tested Positive for SARS-CoV-2, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19010447
Faul, Kerley, Love, O'neill, Cody et al., Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection, Ir. Med. J
Griffin, Wall, Blake, Griffin, Robinson et al., Higher risk of vitamin D insufficiency/deficiency for rural than urban dwellers, J. Steroid. Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2019.105547
Haussler, Jurutka, Mizwicki, Norman, Vitamin D receptor (VDR)-mediated actions of 1α,25(OH)2 vitamin D3: Genomic and non-genomic mechanisms, Best Pract. Res. Clin. Endocrinol. Metab, doi:10.1016/j.beem.2011.05.010
Hii, Ferrante, The Non-Genomic Actions of Vitamin, D. Nutrients, doi:10.3390/nu8030135
Hyppönen, Berry, Cortina-Borja, Power, 25-Hydroxyvitamin D and pre-clinical alterations in inflammatory and hemostatic markers: A cross sectional analysis in the 1958 British Birth Cohort, PLoS ONE, doi:10.1371/journal.pone.0010801
Israel, Cicurel, Feldhamer, Stern, Dror et al., Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: A retrospective case-control study, Intern. Emerg. Med, doi:10.1007/s11739-021-02902-w
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci. Rep, doi:10.1038/s41598-020-77093-z
Jeong, Vacanti, Systemic vitamin intake impacting tissue proteomes, Nutr. Metab, doi:10.1186/s12986-020-00491-7
Jevalikar, Mithal, Singh, Sharma, Farooqui et al., Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19, Sci. Rep, doi:10.1038/s41598-021-85809-y
Kazemi, Mohammadi, Aghababaee, Golzarand, Clark et al., Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis, Adv. Nutr, doi:10.1093/advances/nmab012
Laird, O'halloran, Carey, Healy, O'connor et al., The prevalence of vitamin D deficiency and the determinants of 25(OH)D concentration in older Irish adults: Data from the Irish Longitudinal Study on Ageing (TILDA), J. Gerontol. A Biol. Sci. Med. Sci, doi:10.1093/gerona/glx168
Lippi, Plebani, Henry, Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis, Clin. Chim. Acta, doi:10.1016/j.cca.2020.03.022
Patchen, Clark, Gaddis, Hancock, Cassano, Genetically predicted serum vitamin D and COVID-19: A Mendelian randomisation study, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2021-000255
Petrelli, Luciani, Perego, Dognini, Colombelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2021.105883
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Reid, Bolland, Grey, Effects of vitamin D supplements on bone mineral density: A systematic review and metaanalysis, Lancet, doi:10.1016/S0140-6736(13)61647-5
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: Vitamin D deficiency and COVID-19 severityplausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J. Intern. Med, doi:10.1111/joim.13149
Romero-Ortuno, Cogan, Browne, Healy, Casey et al., Seasonal variation of serum vitamin D and the effect of vitamin D supplementation in Irish community-dwelling older people, Age Ageing, doi:10.1093/ageing/afq138
Rostami, Mansouritorghabeh, D-dimer level in COVID-19 infection: A systematic review, Expert Rev. Hematol, doi:10.1080/17474086.2020.1831383
Skversky, Kumar, Abramowitz, Kaskel, Melamed, Association of glucocorticoid use and low 25-hydroxyvitamin D levels: Results from the National Health and Nutrition Examination Survey (NHANES): 2001-2006, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-1600
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence, Metabolism, doi:10.1016/j.metabol.2020.154434
Sunnetcioglu, Sunnetcioglu, Gurbuz, Bedirhanoglu, Erginoguz et al., Serum 25(OH)D Deficiency and High D-Dimer Levels are Associated with COVID-19 Pneumonia, Clin Lab, doi:10.7754/Clin.Lab.2020.201050
The, Group, Dexamethasone in Hospitalized Patients with COVID-19, N. Engl. J. Med, doi:10.1056/NEJMoa2021436
Vassiliou, Jahaj, Pratikaki, Orfanos, Dimopoulou et al., Low 25-Hydroxyvitamin D Levels on Admission to the Intensive Care Unit May Predispose COVID-19 Pneumonia Patients to a Higher 28-Day Mortality Risk: A Pilot Study on a Greek ICU Cohort, Nutrients, doi:10.3390/nu12123773
Walsh, Mccartney, Laird, Mccarroll, Byrne et al., Understanding a Low Vitamin D State in the Context of COVID-19, Front. Pharmacol, doi:10.3389/fphar.2022.835480
Wang, C-reactive protein levels in the early stage of COVID-19, Médecine Mal. Infect, doi:10.1016/j.medmal.2020.03.007
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Yao, Cao, Wang, Shi, Liu et al., D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: A case control study, J. Intensive Care, doi:10.1186/s40560-020-00466-z
Zhang, Huang, Administration with corticosteroid relieving pain following total knee arthroplasty: A meta-analysis, Medicine, doi:10.1097/MD.0000000000023567
DOI record:
{
"DOI": "10.3390/nu14163252",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14163252",
"abstract": "<jats:p>COVID-19 and a low vitamin D state share common risk factors, which might explain why vitamin D deficiency has been linked with higher COVID-19 mortality. Moreover, measures of serum vitamin D may become lower during systemic inflammatory responses, further confounding the association via reverse causality. In this prospective study (recruited over 12 months), we examined whether the association between a low vitamin D state and in-hospital mortality due to SARS-CoV-2 pneumonia in unvaccinated subjects is explained by (i) the presence of shared risk factors (e.g., obesity, advanced age) or (ii) a reduction in serum 25(OH)D due to COVID-19 (i.e., reverse causality). In this cohort of 232 (mean age = 56 years) patients (all had SARS-CoV-2 diagnosed via PCR AND required supplemental oxygen therapy), we failed to find an association between serum vitamin D and levels of CRP, or other inflammatory markers. However, the hazard ratio for mortality for subjects over 70 years of age (13.2) and for subjects with a serum 25(OH)D level less than 30 nmol·L−1 (4.6) remained significantly elevated even after adjustment for gender, obesity and the presence of diabetes mellitus. Subjects <70 years and >70 years had significantly higher mortality with a serum 25(OH)D less than 30 nmol·L−1 (11.8% and 55%), than with a serum 25(OH)D greater than 30 nmol·L−1 (2.2% and 25%). Unvaccinated Caucasian adults with a low vitamin D state have higher mortality due to SARS CoV-2 pneumonia, which is not explained by confounders and is not closely linked with elevated serum CRP.</jats:p>",
"alternative-id": [
"nu14163252"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3761-5079",
"affiliation": [],
"authenticated-orcid": false,
"family": "Barrett",
"given": "Robert",
"sequence": "first"
},
{
"affiliation": [],
"family": "Youssef",
"given": "Modar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shah",
"given": "Irfan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ioana",
"given": "Julia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lawati",
"given": "Abdullah Al",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bukhari",
"given": "Abdullah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hegarty",
"given": "Suzanne",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cormican",
"given": "Liam J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Judge",
"given": "Eoin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burke",
"given": "Conor M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cody",
"given": "Catriona",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Feely",
"given": "Joseph",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hutchinson",
"given": "Katrina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tormey",
"given": "William",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Neill",
"given": "Eoghan O’",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shea",
"given": "Aoife O’",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Connolly",
"given": "Meabh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McCartney",
"given": "Daniel M. A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Faul",
"given": "John L.",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T08:20:32Z",
"timestamp": 1660119632000
},
"deposited": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T09:18:58Z",
"timestamp": 1660123138000
},
"indexed": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T09:42:08Z",
"timestamp": 1660124528435
},
"is-referenced-by-count": 0,
"issue": "16",
"issued": {
"date-parts": [
[
2022,
8,
9
]
]
},
"journal-issue": {
"issue": "16",
"published-online": {
"date-parts": [
[
2022,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T00:00:00Z",
"timestamp": 1660003200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/16/3252/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3252",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
8,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
9
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1007/s11739-021-02902-w",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.7754/Clin.Lab.2020.201050",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1111/joim.13149",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3389/fnut.2021.660420",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1210/jc.2011-1600",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/j.metabol.2020.154434",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"article-title": "Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection",
"author": "Faul",
"first-page": "84",
"journal-title": "Ir. Med. J.",
"key": "ref13",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1017/S0007114512003212",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1155/2021/1343913",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.3389/fpubh.2020.00513",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3390/nu12123773",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1056/NEJMoa2021436",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.3390/ijerph19010447",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1097/MD.0000000000023567",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/S0140-6736(13)61647-5",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.3945/jn.114.209106",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1093/ageing/afq138",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1016/j.jsbmb.2019.105547",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1093/gerona/glx168",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1093/advances/nmab012",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/j.jsbmb.2021.105883",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1038/s41598-021-85809-y",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1136/bmjnph-2021-000255",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1016/j.medmal.2020.03.007",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1186/s40560-020-00466-z",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1080/17474086.2020.1831383",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1371/journal.pone.0010801",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/j.cca.2020.03.022",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.3390/nu13103596",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.3389/fphar.2022.835480",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1016/j.beem.2011.05.010",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.3390/nu8030135",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1186/s12986-020-00491-7",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.3390/nu12072097",
"doi-asserted-by": "publisher",
"key": "ref42"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/14/16/3252"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Vitamin D Status and Mortality from SARS CoV-2: A Prospective Study of Unvaccinated Caucasian Adults",
"type": "journal-article",
"volume": "14"
}
