Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: a retrospective case–control study
et al., Internal and Emergency Medicine, doi:10.1007/s11739-021-02902-w, Sep 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 41,757 PCR+ patients in Israel and 417,570 matched controls, showing an inverse correlation between vitamin D levels and the risks of SARS-CoV-2 infection and of severe disease in those infected. COM-0046-20.
This is the 97th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
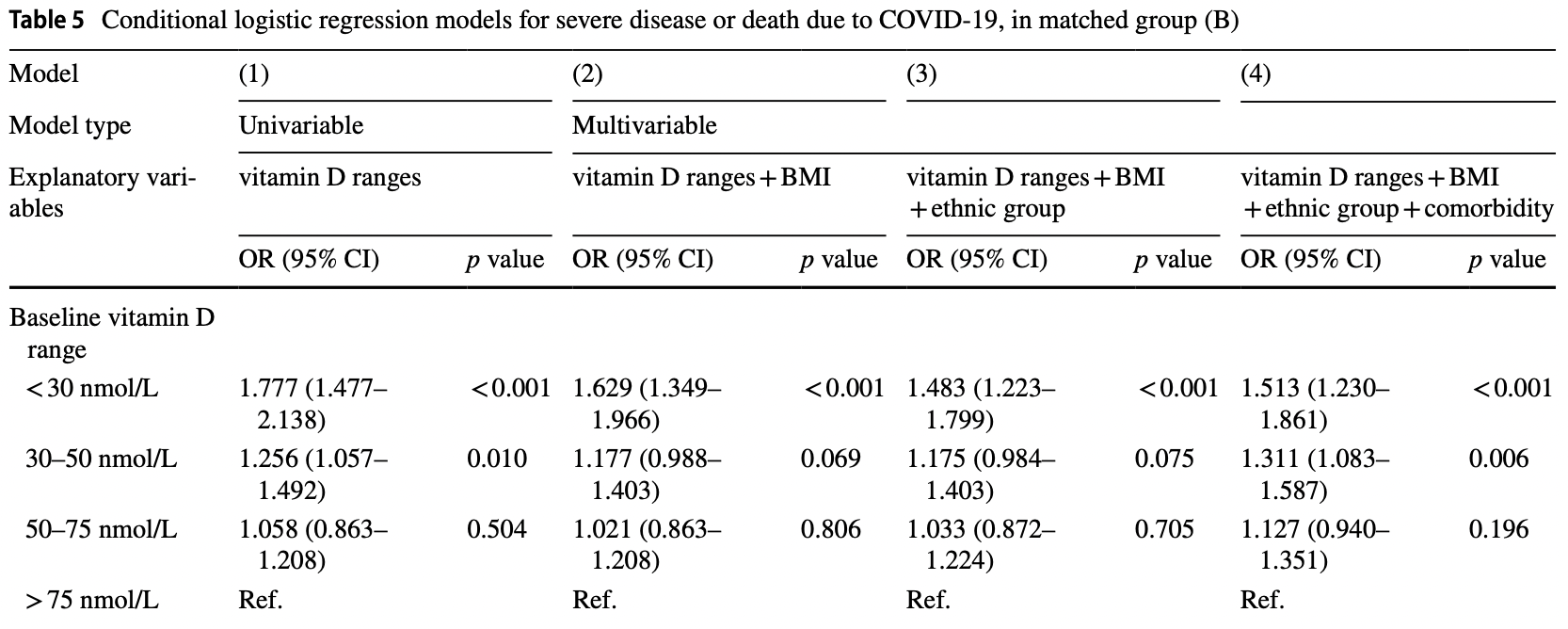
risk of severe case, 33.9% lower, OR 0.66, p < 0.001, high D levels 423 of 1,036 (40.8%) cases,
509 of 934 (54.5%) controls, NNT 7.3, adjusted per study, inverted to make OR<1 favor high D levels, case control OR, >75 nmol/L vs. <30 nmol/L, multivariable.
|
|
risk of case, 19.7% lower, OR 0.80, p < 0.001, high D levels 6,152 of 15,892 (38.7%) cases,
73,810 of 159,193 (46.4%) controls, NNT 39, adjusted per study, inverted to make OR<1 favor high D levels, case control OR, >75 nmol/L vs. <30 nmol/L, among COVID+ cases, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Israel et al., 20 Sep 2021, retrospective, population-based cohort, Israel, peer-reviewed, 9 authors, study period 1 March, 2020 - 31 October, 2020.
Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: a retrospective case–control study
Internal and Emergency Medicine, doi:10.1007/s11739-021-02902-w
Robust evidence of whether vitamin D deficiency is associated with COVID-19 infection and its severity is still lacking. The aim of the study was to evaluate the association between vitamin D levels and the risks of SARS-CoV-2 infection and severe disease in those infected. A retrospective study was carried out among members of Clalit Health Services (CHS), the largest healthcare organization in Israel, between March 1 and October 31, 2020. We created two matched case-control groups of individuals for which vitamin D levels and body mass index (BMI) were available before the pandemic: group (A), in which 41,757 individuals with positive SARS-CoV-2 PCR tests were matched with 417,570 control individuals without evidence of infection, and group (B), in which 2533 patients hospitalized in severe condition for COVID-19 were matched with 2533 patients who were tested positive for SARS-CoV-2, but were not hospitalized. Conditional logistic models were fitted in each of the groups to assess the association between vitamin D levels and outcome. An inverse correlation was demonstrated between the level of vitamin D and the risks of SARS-CoV-2 infection and of severe disease in those infected. Patients with very low vitamin D levels (< 30 nmol/L) had the highest risks for SARS-CoV-2 infection and also for severe COVID-19 when infected-OR 1.246 [95% CI 1.210-1.304] and 1.513 [95% CI 1.230-1.861], respectively. In this large observational population study, we show a significant association between vitamin D deficiency and the risks of SARS-CoV-2 infection and of severe disease in those infected.
Conclusion In this large observational population study, we show a significant association between vitamin D deficiency and the risks of SARS-CoV-2 infection and of severe disease in those infected. Author contributions All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ariel Israel and Ilan Feldhamer. The first draft of the manuscript was written by Ariel Israel and Gil Lavie and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript. Funding None.
Declarations Conflict of interest None.
Human and animal rights statement and Informed consent This study was approved by the CHS Institutional Review Board (IRB) with a waiver of informed consent due to the anonymous nature of the data, approval number: COM-0046-20.
Consent to participate Not applicable.
Consent for publication Not applicable. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Annweiler, Hanotte, De L'eprevier, Sabatier, Lafaie et al., Vitamin D and survival in COVID-19 patients: a quasi-experimental study, J Steroid Biochem Mol Biol
Bmi, None
Carter, Baranauskas, Fly, Considerations for obesity, vitamin D, and physical activity amid the COVID-19 pandemic, Obesity
D'avolio, Avataneo, Manca, 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients
Dror, Giveon, Hoshen, Feldhamer, Balicer et al., Vitamin D levels for preventing acute coronary syndrome and mortality: evidence of a nonlinear association, J Clin Endocrinol Metab
Gil, Plaza-Diaz, Mesa, Vitamin D: classic and novel actions, Ann Nutr Metab
Holick, Medical progress: vitamin D deficiency, N Engl J Med
Israel, Cicurel, Feldhamer, Dror, Giveon et al., The link between vitamin D deficiency and Covid-19 in a large population, doi:10.1101/2020.10.13.20211953
Jude, Ling, Allcock, Yeap, Pappachan, Vitamin D deficiency is associated with higher hospitalization risk from COVID-19: a retrospective case-control study, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab439
Kremer, Campbell, Reinhardt, Gilsanz, Vitamin D status and its relationship to body fat, final height, and peak bone mass in young women, J Clin Endocrinol Metab
Li, Tong, Bare, Devlin, Assessment of the association of vitamin D level with SARS-CoV-2 seropositivity among working-age adults, JAMA Netw Open
Marshall, Murthy, Diaz, Adhikari, Angus et al., A minimal common outcome measure set for COVID-19 clinical research, Lancet Infect Dis
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J
Mirijello, Errico, Marca, Piscitelli, Cosmo-Comment, Comment on Matricardi et, Pediatr Allergy Immunol
Nimavat, Singh, Singh, Singh, Sinha, Vitamin D deficiency and COVID-19: a case-control study at a tertiary care hospital in India, Ann Med Surg
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity, Clin Endocrinol, doi:10.1111/cen.14276
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105719
Rhodes, Subramanian, Laird, Kenny, Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity, Aliment Pharmacol Ther
Rossetti, Martucci, Starchl, Amrein, Micronutrients in Sepsis and COVID-19: a narrative review on what we have learned and what we want to know in future trials, Medicina
Schwalfenberg, A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency, Mol Nutr Food Res
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality, Am J Clin Pathol, doi:10.1093/ajcp/aqaa252
Stroehlein, Wallqvist, Iannizzi, Mikolajewska, Metzendorf et al., Vitamin D supplementation for the treatment of COVID-19: a living systematic review, Cochrane Database Syst Rev, doi:10.1002/14651858.CD015043
Teshome, Adane, Girma, Mekonnen, The impact of vitamin D level on COVID-19 infection: systematic review and meta-analysis, Front Public Health
Vitamin, COVID-19-list results-ClinicalTrials
Wang, Joshi, Leopold, Jackson, Christensen et al., Association of vitamin D deficiency with COVID-19 infection severity: systematic review and meta-analysis, Clin Endocrinol, doi:10.1111/cen.14540
Zhang, Wu, Sun, Vitamin, vitamin D receptor and tissue barriers, Tissue Barriers
DOI record:
{
"DOI": "10.1007/s11739-021-02902-w",
"ISSN": [
"1828-0447",
"1970-9366"
],
"URL": "http://dx.doi.org/10.1007/s11739-021-02902-w",
"alternative-id": [
"2902"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "17 September 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "20 November 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "9 January 2022"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "None."
},
{
"group": {
"label": "Human and animal rights statement and Informed consent",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "This study was approved by the CHS Institutional Review Board (IRB) with a waiver of informed consent due to the anonymous nature of the data, approval number: COM-0046–20."
},
{
"group": {
"label": "Consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "Not applicable."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "Not applicable."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Israel",
"given": "Ariel",
"sequence": "first"
},
{
"affiliation": [],
"family": "Cicurel",
"given": "Assi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Feldhamer",
"given": "Ilan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stern",
"given": "Felicia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dror",
"given": "Yosef",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Giveon",
"given": "Shmuel M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gillis",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Strich",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lavie",
"given": "Gil",
"sequence": "additional"
}
],
"container-title": [
"Internal and Emergency Medicine"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
1,
9
]
],
"date-time": "2022-01-09T00:02:42Z",
"timestamp": 1641686562000
},
"deposited": {
"date-parts": [
[
2022,
1,
9
]
],
"date-time": "2022-01-09T06:10:04Z",
"timestamp": 1641708604000
},
"indexed": {
"date-parts": [
[
2022,
1,
10
]
],
"date-time": "2022-01-10T05:40:39Z",
"timestamp": 1641793239108
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "1828-0447"
},
{
"type": "electronic",
"value": "1970-9366"
}
],
"issued": {
"date-parts": [
[
2022,
1,
9
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
9
]
],
"date-time": "2022-01-09T00:00:00Z",
"timestamp": 1641686400000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
9
]
],
"date-time": "2022-01-09T00:00:00Z",
"timestamp": 1641686400000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11739-021-02902-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11739-021-02902-w/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11739-021-02902-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2022,
1,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
9
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1056/NEJMra070553",
"author": "MF Holick",
"doi-asserted-by": "publisher",
"first-page": "266",
"issue": "3",
"journal-title": "N Engl J Med",
"key": "2902_CR1",
"unstructured": "Holick MF (2007) Medical progress: vitamin D deficiency. N Engl J Med 357(3):266–281",
"volume": "357",
"year": "2007"
},
{
"DOI": "10.3390/medicina57050419",
"author": "M Rossetti",
"doi-asserted-by": "publisher",
"first-page": "419",
"issue": "5",
"journal-title": "Medicina",
"key": "2902_CR2",
"unstructured": "Rossetti M, Martucci G, Starchl C, Amrein K (2021) Micronutrients in Sepsis and COVID-19: a narrative review on what we have learned and what we want to know in future trials. Medicina 57(5):419",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1111/apt.15777",
"author": "JM Rhodes",
"doi-asserted-by": "publisher",
"first-page": "1434",
"issue": "12",
"journal-title": "Aliment Pharmacol Ther",
"key": "2902_CR3",
"unstructured": "Rhodes JM, Subramanian S, Laird E, Kenny RA (2020) Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity. Aliment Pharmacol Ther 51(12):1434–1437",
"volume": "51",
"year": "2020"
},
{
"author": "E Merzon",
"first-page": "644",
"journal-title": "FEBS J",
"key": "2902_CR4",
"unstructured": "Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, Frenkel-Morgenstern M (2020) Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J 13:644",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1111/cen.14276",
"author": "G Panagiotou",
"doi-asserted-by": "publisher",
"journal-title": "Clin Endocrinol",
"key": "2902_CR5",
"unstructured": "Panagiotou G, Tee SA, Ihsan Y, Athar W, Marchitelli G, Kelly D, Boot CS, Stock N, Macfarlane J, Martineau AR, Burns G, Quinton R (2020) Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity. Clin Endocrinol. https://doi.org/10.1111/cen.14276",
"year": "2020"
},
{
"DOI": "10.3390/nu12051359",
"author": "A D’Avolio",
"doi-asserted-by": "publisher",
"first-page": "1359",
"journal-title": "Nutrients",
"key": "2902_CR6",
"unstructured": "D’Avolio A, Avataneo V, Manca A et al (2020) 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients 12:1359",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1210/jc.2013-1185",
"author": "Y Dror",
"doi-asserted-by": "publisher",
"first-page": "2160",
"issue": "5",
"journal-title": "J Clin Endocrinol Metab",
"key": "2902_CR7",
"unstructured": "Dror Y, Giveon SM, Hoshen M, Feldhamer I, Balicer RD, Feldman BS (2013) Vitamin D levels for preventing acute coronary syndrome and mortality: evidence of a nonlinear association. J Clin Endocrinol Metab 98(5):2160–2167",
"volume": "98",
"year": "2013"
},
{
"DOI": "10.1016/S1473-3099(20)30483-7",
"author": "JC Marshall",
"doi-asserted-by": "publisher",
"first-page": "e192",
"issue": "8",
"journal-title": "Lancet Infect Dis",
"key": "2902_CR8",
"unstructured": "Marshall JC, Murthy S, Diaz J, Adhikari N, Angus DC, Arabi YM, Baillie K, Bauer M, Berry S, Blackwood B, Bonten M, Bozza F, Brunkhorst F, Cheng A, Clarke M, Dat VQ, de Jong M, Denholm J, Derde L, Dunning J, Feng X, Fletcher T, Foster N, Fowler R, Gobat N, Gomersall C, Gordon A, Glueck T, Harhay M, Hodgson C, Horby P, Kim YJ, Kojan R, Kumar B, Laffey J, Malvey D, Martin-Loeches I, McArthur C, McAuley D, McBride S, McGuinness S, Merson L, Morpeth S, Needham D, Netea M, Oh MD, Phyu S, Piva S, Qiu R, Salisu-Kabara H, Shi L, Shimizu N, Sinclair J, Tong S, Turgeon A, Uyeki T, van de Veerdonk F, Webb S, Williamson P, Wolf T, Zhang J (2020) A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis 20(8):e192–e197",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1101/2020.10.13.20211953",
"author": "A Israel",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "2902_CR9",
"unstructured": "Israel A, Cicurel A, Feldhamer I, Yosef Dror B, Giveon SM, Gillis D, Strich D, Lavie G (2020) The link between vitamin D deficiency and Covid-19 in a large population. medRxiv. https://doi.org/10.1101/2020.10.13.20211953",
"year": "2020"
},
{
"DOI": "10.1210/jc.2008-1575",
"author": "R Kremer",
"doi-asserted-by": "publisher",
"first-page": "67",
"issue": "1",
"journal-title": "J Clin Endocrinol Metab",
"key": "2902_CR10",
"unstructured": "Kremer R, Campbell PP, Reinhardt T, Gilsanz V (2009) Vitamin D status and its relationship to body fat, final height, and peak bone mass in young women. J Clin Endocrinol Metab 94(1):67–73",
"volume": "94",
"year": "2009"
},
{
"DOI": "10.1002/oby.22838",
"author": "SJ Carter",
"doi-asserted-by": "publisher",
"first-page": "1176",
"issue": "7",
"journal-title": "Obesity",
"key": "2902_CR11",
"unstructured": "Carter SJ, Baranauskas MN, Fly AD (2020) Considerations for obesity, vitamin D, and physical activity amid the COVID-19 pandemic. Obesity 28(7):1176–1177",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"author": "DO Meltzer",
"doi-asserted-by": "publisher",
"first-page": "e2019722",
"issue": "9",
"journal-title": "JAMA Netw Open",
"key": "2902_CR12",
"unstructured": "Meltzer DO, Best TJ, Zhang H, Vokes T, Arora V, Solway J (2020) Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Netw Open 3(9):e2019722",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"author": "D De Smet",
"doi-asserted-by": "publisher",
"journal-title": "Am J Clin Pathol",
"key": "2902_CR13",
"unstructured": "De Smet D, De Smet K, Herroelen P, Gryspeerdt S, Martens GA (2020) Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality. Am J Clin Pathol. https://doi.org/10.1093/ajcp/aqaa252",
"year": "2020"
},
{
"DOI": "10.1002/mnfr.201000174",
"author": "GK Schwalfenberg",
"doi-asserted-by": "publisher",
"first-page": "96",
"issue": "1",
"journal-title": "Mol Nutr Food Res",
"key": "2902_CR14",
"unstructured": "Schwalfenberg GK (2011) A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency. Mol Nutr Food Res 55(1):96–108",
"volume": "55",
"year": "2011"
},
{
"DOI": "10.4161/tisb.23118",
"author": "Y Zhang",
"doi-asserted-by": "publisher",
"first-page": "e23118",
"issue": "1",
"journal-title": "Tissue Barriers",
"key": "2902_CR15",
"unstructured": "Zhang Y, Wu S, Sun J, Vitamin D (2013) vitamin D receptor and tissue barriers. Tissue Barriers 1(1):e23118",
"volume": "1",
"year": "2013"
},
{
"DOI": "10.1159/000486536",
"author": "Á Gil",
"doi-asserted-by": "publisher",
"first-page": "87",
"issue": "2",
"journal-title": "Ann Nutr Metab",
"key": "2902_CR16",
"unstructured": "Gil Á, Plaza-Diaz J, Mesa MD (2018) Vitamin D: classic and novel actions. Ann Nutr Metab 72(2):87–95",
"volume": "72",
"year": "2018"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"author": "JM Quesada-Gomez",
"doi-asserted-by": "publisher",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "2902_CR17",
"unstructured": "Quesada-Gomez JM, Entrenas-Castillo M, Bouillon R (2020) Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166. J Steroid Biochem Mol Biol. https://doi.org/10.1016/j.jsbmb.2020.105719",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2020.105771",
"author": "C Annweiler",
"doi-asserted-by": "publisher",
"first-page": "105771",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "2902_CR18",
"unstructured": "Annweiler C, Hanotte B, Grandin de l’Eprevier C, Sabatier JM, Lafaie L, Célarier T (2020) Vitamin D and survival in COVID-19 patients: a quasi-experimental study. J Steroid Biochem Mol Biol 204:105771",
"volume": "204",
"year": "2020"
},
{
"key": "2902_CR19",
"unstructured": "Vitamin D | COVID-19—list results—ClinicalTrials.gov. (2021) Available at: https://clinicaltrials.gov/ct2/results?cond=COVID-19&term=vitamin+D&cntry=&state=&city=&dist=. Accessed 20 Dec 2020"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11634",
"author": "Y Li",
"doi-asserted-by": "publisher",
"first-page": "e2111634",
"issue": "5",
"journal-title": "JAMA Netw Open",
"key": "2902_CR20",
"unstructured": "Li Y, Tong CH, Bare LA, Devlin JJ (2021) Assessment of the association of vitamin D level with SARS-CoV-2 seropositivity among working-age adults. JAMA Netw Open 4(5):e2111634",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3389/fpubh.2021.624559",
"author": "A Teshome",
"doi-asserted-by": "publisher",
"first-page": "624559",
"journal-title": "Front Public Health",
"key": "2902_CR21",
"unstructured": "Teshome A, Adane A, Girma B, Mekonnen ZA (2021) The impact of vitamin D level on COVID-19 infection: systematic review and meta-analysis. Front Public Health 9:624559",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.amsu.2021.102661",
"author": "N Nimavat",
"doi-asserted-by": "publisher",
"first-page": "102661",
"journal-title": "Ann Med Surg",
"key": "2902_CR22",
"unstructured": "Nimavat N, Singh S, Singh P, Singh SK, Sinha N (2021) Vitamin D deficiency and COVID-19: a case-control study at a tertiary care hospital in India. Ann Med Surg 68:102661",
"volume": "68",
"year": "2021"
},
{
"DOI": "10.1111/cen.14540",
"author": "Z Wang",
"doi-asserted-by": "publisher",
"journal-title": "Clin Endocrinol",
"key": "2902_CR23",
"unstructured": "Wang Z, Joshi A, Leopold K, Jackson S, Christensen S, Nayfeh T, Mohammed K, Creo A, Tebben P, Kumar S (2021) Association of vitamin D deficiency with COVID-19 infection severity: systematic review and meta-analysis. Clin Endocrinol. https://doi.org/10.1111/cen.14540",
"year": "2021"
},
{
"DOI": "10.1002/14651858.CD015043",
"author": "JK Stroehlein",
"doi-asserted-by": "publisher",
"journal-title": "Cochrane Database Syst Rev",
"key": "2902_CR24",
"unstructured": "Stroehlein JK, Wallqvist J, Iannizzi C, Mikolajewska A, Metzendorf MI, Benstoem C, Meybohm P, Becke M, Skoetz N, Stegemann M, Piechotta V (2021) Vitamin D supplementation for the treatment of COVID-19: a living systematic review. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD015043",
"year": "2021"
},
{
"key": "2902_CR25",
"unstructured": "https://www.uptodate.com/contents/vitamin-d-deficiency-beyond-the-basics. Accessed 6 July 2021"
},
{
"DOI": "10.1210/clinem/dgab439",
"author": "EB Jude",
"doi-asserted-by": "publisher",
"journal-title": "J Clin Endocrinol Metab",
"key": "2902_CR26",
"unstructured": "Jude EB, Ling SF, Allcock R, Yeap BX, Pappachan JM (2021) Vitamin D deficiency is associated with higher hospitalization risk from COVID-19: a retrospective case-control study. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgab439",
"year": "2021"
},
{
"DOI": "10.1111/pai.13277",
"author": "A Mirijello",
"doi-asserted-by": "publisher",
"first-page": "997",
"issue": "8",
"journal-title": "Pediatr Allergy Immunol",
"key": "2902_CR27",
"unstructured": "Mirijello A, D’Errico MM, La Marca A, Piscitelli P, De CosmoComment S et al (2020) Comment on Matricardi et al. Pediatr Allergy Immunol 31(8):997",
"volume": "31",
"year": "2020"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"score": 1,
"short-container-title": [
"Intern Emerg Med"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Emergency Medicine",
"Internal Medicine"
],
"subtitle": [],
"title": [
"Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: a retrospective case–control study"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}
