Association of Trace Element Levels with Outcomes in Critically Ill COVID-19 Patients
et al., Nutrients, doi:10.3390/nu15153308, Jul 2023
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 345 COVID-19 patients in Switzerland, showing significantly different zinc levels with ICU patients < hospitalized patients < outpatients.
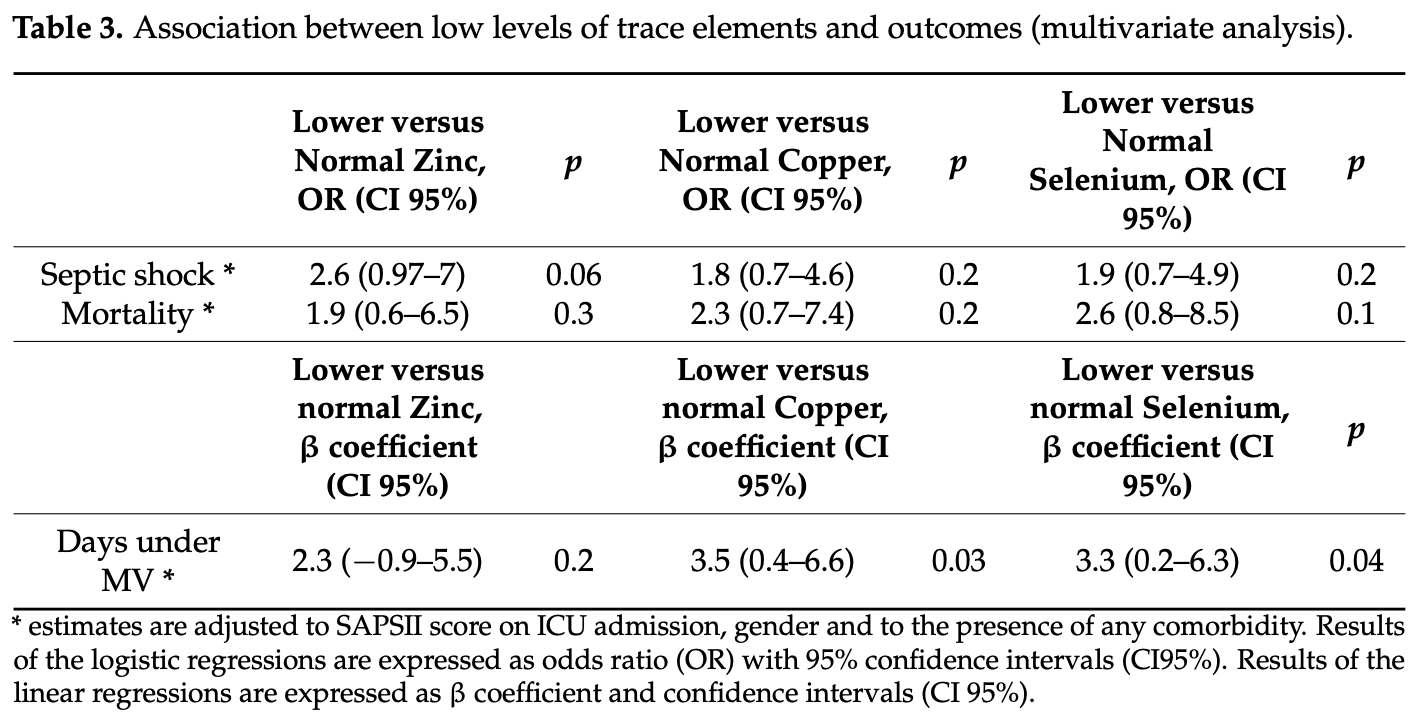
For ICU patients, there was higher mortality, septic shock, and mechanical ventilation days with lower zinc levels, without statistical significance.
Study covers selenium and zinc.
|
risk of death, 47.4% lower, OR 0.53, p = 0.30, high zinc levels (≥8.2μmol/L) 59, low zinc levels (<8.2μmol/L) 59, adjusted per study, inverted to make OR<1 favor high zinc levels (≥8.2μmol/L), multivariable, RR approximated with OR.
|
|
septic shock, 61.5% lower, OR 0.38, p = 0.06, high zinc levels (≥8.2μmol/L) 59, low zinc levels (<8.2μmol/L) 59, adjusted per study, inverted to make OR<1 favor high zinc levels (≥8.2μmol/L), multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wozniak et al., 26 Jul 2023, retrospective, Switzerland, peer-reviewed, 14 authors, study period 9 March, 2020 - 19 May, 2020.
Association of Trace Element Levels with Outcomes in Critically Ill COVID-19 Patients
Nutrients, doi:10.3390/nu15153308
The primary objective of this study was to compare the plasma levels of copper, selenium, and zinc between critically ill COVID-19 patients and less severe COVID-19 patients. The secondary objective was to investigate the association of these trace element levels with adverse outcomes, including the duration of mechanical ventilation, occurrence of septic shock, and mortality in critically ill COVID-19 patients. All COVID-19 patients admitted to the ICU of the Geneva University Hospitals between 9 March 2020 and 19 May 2020 were included in the study. Plasma levels of copper, selenium and zinc were measured on admission to the ICU and compared with levels measured in COVID-19 patients hospitalized on the ward and in non-hospitalized COVID-19 patients. To analyze the association of trace elements with clinical outcomes, multivariate linear and logistic regressions were performed. Patients in the ICU had significantly lower levels of selenium and zinc and higher levels of copper compared to COVID-19 patients hospitalized on the ward and in non-hospitalized COVID-19 patients. In ICU patients, lower zinc levels tended to be associated with more septic shock and increased mortality compared to those with higher zinc levels (p = 0.07 for both). Having lower copper or selenium levels was associated with a longer time under mechanical ventilation (p = 0.01 and 0.04, respectively). These associations remained significant in multivariate analyses (p = 0.03 for copper and p = 0.04 for selenium). These data support the need for interventional studies to assess the potential benefit of zinc, copper and selenium supplementation in severe COVID-19 patients.
References
Abani, Abbas, Abbas, Abbas, Abbasi et al., Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial, Lancet, doi:10.1016/S0140-6736(21)00676-0
Al Sulaiman, Aljuhani, Al Shaya, Kharbosh, Kensara et al., Evaluation of zinc sulfate as an adjunctive therapy in COVID-19 critically ill patients: A two center propensity-score matched study, Crit. Care, doi:10.1186/s13054-021-03785-1
Allingstrup, Selenium supplementation for critically ill adults, Cochrane. Database. Syst. Rev, doi:10.1002/14651858.CD003703.pub3
Arrieta, Martinez-Vaello, Bengoa, Jiménez-Mendiguchia, Rosillo et al., Serum zinc and copper in people with COVID-19 and zinc supplementation in parenteral nutrition, Nutrition, doi:10.1016/j.nut.2021.111467
Balboni, Zagnoli, Filippini, Fairweather-Tait, Vinceti, Zinc and selenium supplementation in COVID-19 prevention and treatment: A systematic review of the experimental studies, J. Trace Elem. Med. Biol, doi:10.1016/j.jtemb.2022.126956
Basak, Doruk, Engin, Can iron, zinc, copper and selenium status be a prognostic determinant in COVID-19 patients?, Environ. Toxicol. Pharmacol
Bayraktar, Bayraktar, Ozturk, Ibrahim, Evaluation of the Relationship Between Aquaporin-1, Hepcidin, Zinc, Copper, and ˙Iron Levels and Oxidative Stress in the Serum of Critically Ill Patients with COVID-19, Biol. Trace Elem. Res, doi:10.1007/s12011-022-03400-6
Ben Abdallah, Mhalla, Trabelsi, Sekma, Youssef et al., Twice-Daily Oral Zinc in the Treatment of Patients With Coronavirus Disease 2019: A Randomized Double-Blind Controlled Trial, Clin. Infect Dis, doi:10.1093/cid/ciac807
Beran, Mhanna, Srour, Ayesh, Stewart et al., Clinical significance of micronutrient supplements in patients with coronavirus disease 2019: A comprehensive systematic review and meta-analysis, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.12.033
Berger, Shenkin, Schweinlin, Amrein, Augsburger et al., None, ESPEN micronutrient guideline, doi:10.1016/j.clnu.2022.02.015
Berger, Talwar, Shenkin, Pitfalls in the interpretation of blood tests used to assess and monitor micronutrient nutrition status, Nutr. Clin. Pract, doi:10.1002/ncp.10924
Delgado-Roche, Mesta, Oxidative Stress as Key Player in Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) Infection, Arch. Med. Res, doi:10.1016/j.arcmed.2020.04.019
Demircan, Chillon, Bracken, Bulgarelli, Campi et al., Association of COVID-19 mortality with serum selenium, zinc and copper: Six observational studies across, Europe. Front. Immunol, doi:10.3389/fimmu.2022.1022673
Eden, Mcauliffe, Crocombe, Neville, Ray, Nutritional parameters and outcomes in patients admitted to intensive care with COVID-19: A retrospective single-centre service evaluation, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2021-000270
Fakhrolmobasheri, Mazaheri-Tehrani, Kieliszek, Zeinalian, Abbasi et al., COVID-19 and Selenium Deficiency: A Systematic Review, Biol. Trace Elem. Res, doi:10.1007/s12011-021-02997-4
Fooladi, Matin, Mahmoodpoor, Copper as a potential adjunct therapy for critically ill COVID-19 patients, Clin. Nutr, doi:10.1016/j.clnesp.2020.09.022
Fromonot, Gette, Ben Lassoued, Guéant, Guéant-Rodriguez et al., Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19, Clin. Nutr, doi:10.1016/j.clnu.2021.04.042
Gordon, Asher, Becker, Irreversible inhibition of herpes simplex virus replication in BSC 1 cells by zinc ions, Antimicrob. Agents Chemother, doi:10.1128/AAC.8.3.377
Grasselli, Greco, Zanella, Albano, Antonelli et al., Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in, doi:10.1001/jamainternmed.2020.3539
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease 2019 in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Guiomar, Brasiel, The key role of zinc in elderly immunity: A possible approach in the COVID-19 crisis, Clin. Nutr
Heller, Sun, Hackler, Seelig, Seibert et al., Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker, Redox. Biol, doi:10.1016/j.redox.2020.101764
Horby, Lim, Emberson, Mafham, Bell et al., Dexamethasone in Hospitalized Patients with Covid-19
Jafari, Thomas, Haselbach, Watfa, Pantet et al., Trace element intakes should be revisited in burn nutrition protocols: A cohort study, Clin. Nutr, doi:10.1016/j.clnu.2017.03.028
Karimi, Shobeiri, Kulasinghe, Rezaei, Novel Systemic Inflammation Markers to Predict COVID-19 Prognosis, Front. Immunol. 2021, doi:10.3389/fimmu.2021.741061
Khatiwada, Subedi, A Mechanistic Link Between Selenium and Coronavirus Disease 2019 (COVID-19), Curr. Nutr. Rep, doi:10.1007/s13668-021-00354-4
Laing, Petrovic, Lachat, De Boevre, Klingenberg et al., Course and survival of covid-19 patients with comorbidities in relation to the trace element status at hospital admission, Nutrients, doi:10.3390/nu13103304
Lee, Bang, Lee, Lee, Kang et al., Serum Concentrations of Trace Elements Zinc, Copper, Selenium, and Manganese in Critically Ill Patients, doi:10.1007/s12011-018-1429-4
Manzanares, Dhaliwal, Jiang, Murch, Heyland, Antioxidant micronutrients in the critically ill: A systematic review and meta-analysis, Crit. Care, doi:10.1186/cc11316
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium deficiency is associated with mortality risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Moore, June, Cytokine release syndrome in severe COVID-19, Science, doi:10.1126/science.abb8925
Primmaz, Le Terrier, Suh, Ventura, Boroli et al., Preparedness and Reorganization of Care for Coronavirus Disease 2019 Patients in a Swiss ICU: Characteristics and Outcomes of 129 Patients, doi:10.1097/CCE.0000000000000173
Shenkin, Berger, Micronutrients, A low blood concentration is not equivalent to deficiency, Clin. Nutr, doi:10.1016/j.clnu.2022.09.015
Singer, Deutschman, Seymour, Shankar-Hari, Annane et al., The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), JAMA, doi:10.1001/jama.2016.0287
Sobczyk, Gaunt, The Effect of Circulating Zinc, Selenium, Copper and Vitamin K1 on COVID-19 Outcomes: A Mendelian Randomization Study, Nutrients, doi:10.3390/nu14020233
Stringhini, Wisniak, Piumatti, Azman, Lauer et al., Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study, Lancet, doi:10.1016/S0140-6736(20)31304-0
Velthuis, Van Den Worml, Sims, Baric, Snijder et al., Zn 2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog, doi:10.1371/journal.ppat.1001176
Voelkle, Gregoriano, Neyer, Koch, Kutz et al., Prevalence of Micronutrient Deficiencies in Patients Hospitalized with COVID-19: An Observational Cohort Study, Nutrients
Wessels, Rolles, Rink, The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis, Front. Immunol, doi:10.3389/fimmu.2020.01712
Yasui, Yasui, Suzuki, Saitou, Yamamoto et al., Analysis of the predictive factors for a critical illness of COVID-19 during treatment-Relationship between serum zinc level and critical illness of COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.09.008
Zhang, Liu, Potential interventions for novel coronavirus in China: A systematic review, J. Med. Virol
Ścibior, Wnuk, Elements and COVID-19: A Comprehensive Overview of Studies on Their Blood/Urinary Levels and Supplementation with an Update on, Clinical Trials. Biology, doi:10.3390/biology11020215
DOI record:
{
"DOI": "10.3390/nu15153308",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu15153308",
"abstract": "<jats:p>The primary objective of this study was to compare the plasma levels of copper, selenium, and zinc between critically ill COVID-19 patients and less severe COVID-19 patients. The secondary objective was to investigate the association of these trace element levels with adverse outcomes, including the duration of mechanical ventilation, occurrence of septic shock, and mortality in critically ill COVID-19 patients. All COVID-19 patients admitted to the ICU of the Geneva University Hospitals between 9 March 2020 and 19 May 2020 were included in the study. Plasma levels of copper, selenium and zinc were measured on admission to the ICU and compared with levels measured in COVID-19 patients hospitalized on the ward and in non-hospitalized COVID-19 patients. To analyze the association of trace elements with clinical outcomes, multivariate linear and logistic regressions were performed. Patients in the ICU had significantly lower levels of selenium and zinc and higher levels of copper compared to COVID-19 patients hospitalized on the ward and in non-hospitalized COVID-19 patients. In ICU patients, lower zinc levels tended to be associated with more septic shock and increased mortality compared to those with higher zinc levels (p = 0.07 for both). Having lower copper or selenium levels was associated with a longer time under mechanical ventilation (p = 0.01 and 0.04, respectively). These associations remained significant in multivariate analyses (p = 0.03 for copper and p = 0.04 for selenium). These data support the need for interventional studies to assess the potential benefit of zinc, copper and selenium supplementation in severe COVID-19 patients.</jats:p>",
"alternative-id": [
"nu15153308"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5404-4621",
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Wozniak",
"given": "Hannah",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-5455-5576",
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Le Terrier",
"given": "Christophe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5828-5825",
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Primmaz",
"given": "Steve",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"family": "Suh",
"given": "Noémie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Forensic Toxicology and Chemistry Unit, CURML, Lausanne University Hospital, Geneva University Hospitals, 1205 Geneva, Switzerland"
}
],
"family": "Lenglet",
"given": "Sébastien",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6790-2285",
"affiliation": [
{
"name": "Forensic Toxicology and Chemistry Unit, CURML, Lausanne University Hospital, Geneva University Hospitals, 1205 Geneva, Switzerland"
},
{
"name": "Faculty Unit of Toxicology, CURML, Faculty of Biology and Medicine, University of Lausanne, 1015 Lausanne, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Thomas",
"given": "Aurélien",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Laboratory Medicine, Diagnostics Department, Geneva University Hospitals, Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"family": "Vuilleumier",
"given": "Nicolas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7075-1182",
"affiliation": [
{
"name": "Division of Laboratory Medicine, Diagnostics Department, Geneva University Hospitals, Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Pagano",
"given": "Sabrina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"family": "de Watteville",
"given": "Aude",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unit of Population Epidemiology, Division of Primary Care Medicine, Geneva University Hospitals, 1205 Geneva, Switzerland"
}
],
"family": "Stringhini",
"given": "Silvia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unit of Population Epidemiology, Division of Primary Care Medicine, Geneva University Hospitals, 1205 Geneva, Switzerland"
},
{
"name": "Department of Community Medicine, Primary Care and Emergency Medicine, Geneva University Hospital, 1205 Geneva, Switzerland"
}
],
"family": "Guessous",
"given": "Idris",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3870-6370",
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Quintard",
"given": "Hervé",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5107-8217",
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Heidegger",
"given": "Claudia Paula",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Intensive Care, Geneva University Hospitals, the Faculty of Medicine, University of Geneva, 1205 Geneva, Switzerland"
}
],
"family": "Pugin",
"given": "Jérôme",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
7,
27
]
],
"date-time": "2023-07-27T06:07:17Z",
"timestamp": 1690438037000
},
"deposited": {
"date-parts": [
[
2023,
7,
27
]
],
"date-time": "2023-07-27T07:26:01Z",
"timestamp": 1690442761000
},
"funder": [
{
"name": "Vasco Sanz fund"
}
],
"indexed": {
"date-parts": [
[
2023,
7,
28
]
],
"date-time": "2023-07-28T04:25:36Z",
"timestamp": 1690518336674
},
"is-referenced-by-count": 0,
"issue": "15",
"issued": {
"date-parts": [
[
2023,
7,
26
]
]
},
"journal-issue": {
"issue": "15",
"published-online": {
"date-parts": [
[
2023,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
7,
26
]
],
"date-time": "2023-07-26T00:00:00Z",
"timestamp": 1690329600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/15/15/3308/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3308",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
7,
26
]
]
},
"published-online": {
"date-parts": [
[
2023,
7,
26
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical Characteristics of Coronavirus Disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"journal-title": "N. Engl. J. Med.",
"key": "ref_1",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2021.741061",
"article-title": "Novel Systemic Inflammation Markers to Predict COVID-19 Prognosis",
"author": "Karimi",
"doi-asserted-by": "crossref",
"first-page": "741061",
"journal-title": "Front. Immunol.",
"key": "ref_2",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1126/science.abb8925",
"article-title": "Cytokine release syndrome in severe COVID-19",
"author": "Moore",
"doi-asserted-by": "crossref",
"first-page": "473",
"journal-title": "Science",
"key": "ref_3",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2021436",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "RECOVERY Collaborative Group, Horby, P., Lim, W.S., Emberson, J.R., Mafham, M., Bell, J.L., Linsell, L., Staplin, N., Brightling, C., and Ustianowski, A. (2021). Dexamethasone in Hospitalized Patients with Covid-19. N. Engl. J. Med., 384, 693–704."
},
{
"DOI": "10.1016/S0140-6736(21)00676-0",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "RECOVERY Collaborative Group, Abani, O., Abbas, A., Abbas, F., Abbas, M., Abbasi, S., Abbass, H., Abbott, A., Abdallah, N., and Abdelaziz, A. (2021). Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet, 397, 1637–1645."
},
{
"DOI": "10.1001/jamainternmed.2020.3539",
"article-title": "Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in Lombardy, Italy",
"author": "Grasselli",
"doi-asserted-by": "crossref",
"first-page": "1345",
"journal-title": "JAMA Intern. Med.",
"key": "ref_6",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2022.1022673",
"article-title": "Association of COVID-19 mortality with serum selenium, zinc and copper: Six observational studies across Europe",
"author": "Demircan",
"doi-asserted-by": "crossref",
"first-page": "1022673",
"journal-title": "Front. Immunol.",
"key": "ref_7",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3390/nu14091862",
"doi-asserted-by": "crossref",
"key": "ref_8",
"unstructured": "Voelkle, M., Gregoriano, C., Neyer, P., Koch, D., Kutz, A., Bernasconi, L., Conen, A., Mueller, B., and Schuetz, P. (2022). Prevalence of Micronutrient Deficiencies in Patients Hospitalized with COVID-19: An Observational Cohort Study. Nutrients, 14."
},
{
"DOI": "10.1016/j.ijid.2020.09.008",
"article-title": "Analysis of the predictive factors for a critical illness of COVID-19 during treatment—Relationship between serum zinc level and critical illness of COVID-19",
"author": "Yasui",
"doi-asserted-by": "crossref",
"first-page": "230",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_9",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2021-000270",
"article-title": "Nutritional parameters and outcomes in patients admitted to intensive care with COVID-19: A retrospective single-centre service evaluation",
"author": "Eden",
"doi-asserted-by": "crossref",
"first-page": "416",
"journal-title": "BMJ Nutr. Prev. Health",
"key": "ref_10",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.01712",
"article-title": "The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis",
"author": "Wessels",
"doi-asserted-by": "crossref",
"first-page": "1712",
"journal-title": "Front. Immunol.",
"key": "ref_11",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.clnu.2022.02.015",
"article-title": "ESPEN micronutrient guideline",
"author": "Berger",
"doi-asserted-by": "crossref",
"first-page": "1357",
"journal-title": "Clin. Nutr.",
"key": "ref_12",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Velthuis, A.J.W., van den Worml, S.H.E., Sims, A.C., Baric, R.S., Snijder, E.J., and van Hemert, M.J. (2010). Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog., 6."
},
{
"DOI": "10.1002/jmv.25707",
"article-title": "Potential interventions for novel coronavirus in China: A systematic review",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "479",
"journal-title": "J. Med. Virol.",
"key": "ref_14",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1128/AAC.8.3.377",
"article-title": "Irreversible inhibition of herpes simplex virus replication in BSC 1 cells by zinc ions",
"author": "Gordon",
"doi-asserted-by": "crossref",
"first-page": "377",
"journal-title": "Antimicrob. Agents Chemother.",
"key": "ref_15",
"volume": "8",
"year": "1975"
},
{
"DOI": "10.3390/biology11020215",
"doi-asserted-by": "crossref",
"key": "ref_16",
"unstructured": "Ścibior, A., and Wnuk, E. (2022). Elements and COVID-19: A Comprehensive Overview of Studies on Their Blood/Urinary Levels and Supplementation with an Update on Clinical Trials. Biology, 11."
},
{
"DOI": "10.1016/j.etap.2022.103937",
"article-title": "Can iron, zinc, copper and selenium status be a prognostic determinant in COVID-19 patients?",
"author": "Basak",
"doi-asserted-by": "crossref",
"first-page": "103937",
"journal-title": "Environ. Toxicol. Pharmacol.",
"key": "ref_17",
"volume": "95",
"year": "2022"
},
{
"DOI": "10.1016/j.clnesp.2020.06.003",
"article-title": "The key role of zinc in elderly immunity: A possible approach in the COVID-19 crisis",
"author": "Guiomar",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Clin. Nutr. ESPEN",
"key": "ref_18",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1016/j.clnesp.2020.09.022",
"article-title": "Copper as a potential adjunct therapy for critically ill COVID-19 patients",
"author": "Fooladi",
"doi-asserted-by": "crossref",
"first-page": "90",
"journal-title": "Clin. Nutr. ESPEN",
"key": "ref_19",
"volume": "40",
"year": "2020"
},
{
"article-title": "Preparedness and Reorganization of Care for Coronavirus Disease 2019 Patients in a Swiss ICU: Characteristics and Outcomes of 129 Patients",
"author": "Primmaz",
"first-page": "0173",
"journal-title": "Crit Care Explor.",
"key": "ref_20",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1101/2020.05.02.20088898",
"doi-asserted-by": "crossref",
"key": "ref_21",
"unstructured": "Stringhini, S., Wisniak, A., Piumatti, G., Azman, A.S., Lauer, S.A., Baysson, H., De Ridder, D., Petrovic, D., Schrempft, S., and Marcus, K. (2020). Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study. Lancet, 19–21."
},
{
"article-title": "The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)",
"author": "Singer",
"first-page": "299",
"journal-title": "JAMA",
"key": "ref_22",
"volume": "66",
"year": "2016"
},
{
"DOI": "10.1016/j.clnu.2017.03.028",
"article-title": "Trace element intakes should be revisited in burn nutrition protocols: A cohort study",
"author": "Jafari",
"doi-asserted-by": "crossref",
"first-page": "958",
"journal-title": "Clin. Nutr.",
"key": "ref_23",
"volume": "37",
"year": "2018"
},
{
"DOI": "10.1016/j.clnu.2022.09.015",
"article-title": "Micronutrients: A low blood concentration is not equivalent to deficiency",
"author": "Shenkin",
"doi-asserted-by": "crossref",
"first-page": "2562",
"journal-title": "Clin. Nutr.",
"key": "ref_24",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1016/j.clnu.2021.04.042",
"article-title": "Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19",
"author": "Fromonot",
"doi-asserted-by": "crossref",
"first-page": "3115",
"journal-title": "Clin. Nutr.",
"key": "ref_25",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.3390/nu13103304",
"doi-asserted-by": "crossref",
"key": "ref_26",
"unstructured": "Du Laing, G., Petrovic, M., Lachat, C., De Boevre, M., Klingenberg, G.J., Sun, Q., De Saeger, S., De Clercq, J., Ide, L., and Vandekerckhove, L. (2021). Course and survival of covid-19 patients with comorbidities in relation to the trace element status at hospital admission. Nutrients, 13."
},
{
"DOI": "10.1007/s12011-021-02997-4",
"article-title": "COVID-19 and Selenium Deficiency: A Systematic Review",
"author": "Fakhrolmobasheri",
"doi-asserted-by": "crossref",
"first-page": "3945",
"journal-title": "Biol. Trace Elem. Res.",
"key": "ref_27",
"volume": "200",
"year": "2021"
},
{
"DOI": "10.1007/s12011-018-1429-4",
"article-title": "Serum Concentrations of Trace Elements Zinc, Copper, Selenium, and Manganese in Critically Ill Patients",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "316",
"journal-title": "Biol. Trace Elem. Res.",
"key": "ref_28",
"volume": "188",
"year": "2019"
},
{
"DOI": "10.1016/j.arcmed.2020.04.019",
"article-title": "Oxidative Stress as Key Player in Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) Infection",
"author": "Mesta",
"doi-asserted-by": "crossref",
"first-page": "384",
"journal-title": "Arch. Med. Res.",
"key": "ref_29",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.1016/j.nut.2021.111467",
"article-title": "Serum zinc and copper in people with COVID-19 and zinc supplementation in parenteral nutrition",
"author": "Arrieta",
"doi-asserted-by": "crossref",
"first-page": "111467",
"journal-title": "Nutrition",
"key": "ref_30",
"volume": "91–92",
"year": "2021"
},
{
"DOI": "10.1007/s13668-021-00354-4",
"article-title": "A Mechanistic Link Between Selenium and Coronavirus Disease 2019 (COVID-19)",
"author": "Khatiwada",
"doi-asserted-by": "crossref",
"first-page": "125",
"journal-title": "Curr. Nutr. Rep.",
"key": "ref_31",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.20944/preprints202007.0113.v1",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Moghaddam, A., Heller, R.A., Sun, Q., Seelig, J., Cherkezov, A., Seibert, L., Hackler, J., Seemann, P., Diegmann, J., and Pilz, M. (2020). Selenium deficiency is associated with mortality risk from COVID-19. Nutrients, 12."
},
{
"DOI": "10.1007/s12011-022-03400-6",
"article-title": "Evaluation of the Relationship Between Aquaporin-1, Hepcidin, Zinc, Copper, and İron Levels and Oxidative Stress in the Serum of Critically Ill Patients with COVID-19",
"author": "Bayraktar",
"doi-asserted-by": "crossref",
"first-page": "5013",
"journal-title": "Biol. Trace Elem. Res.",
"key": "ref_33",
"volume": "200",
"year": "2022"
},
{
"DOI": "10.1016/j.redox.2020.101764",
"article-title": "Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker",
"author": "Heller",
"doi-asserted-by": "crossref",
"first-page": "101764",
"journal-title": "Redox. Biol.",
"key": "ref_34",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1002/ncp.10924",
"article-title": "Pitfalls in the interpretation of blood tests used to assess and monitor micronutrient nutrition status",
"author": "Berger",
"doi-asserted-by": "crossref",
"first-page": "56",
"journal-title": "Nutr. Clin. Pract.",
"key": "ref_35",
"volume": "38",
"year": "2023"
},
{
"DOI": "10.1016/j.clnesp.2021.12.033",
"article-title": "Clinical significance of micronutrient supplements in patients with coronavirus disease 2019: A comprehensive systematic review and meta-analysis",
"author": "Beran",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "Clin. Nutr. ESPEN",
"key": "ref_36",
"volume": "48",
"year": "2022"
},
{
"DOI": "10.3390/nu14020233",
"doi-asserted-by": "crossref",
"key": "ref_37",
"unstructured": "Sobczyk, M.K., and Gaunt, T.R. (2022). The Effect of Circulating Zinc, Selenium, Copper and Vitamin K1 on COVID-19 Outcomes: A Mendelian Randomization Study. Nutrients, 14."
},
{
"DOI": "10.1016/j.jtemb.2022.126956",
"article-title": "Zinc and selenium supplementation in COVID-19 prevention and treatment: A systematic review of the experimental studies",
"author": "Balboni",
"doi-asserted-by": "crossref",
"first-page": "126956",
"journal-title": "J. Trace Elem. Med. Biol.",
"key": "ref_38",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciac807",
"article-title": "Twice-Daily Oral Zinc in the Treatment of Patients With Coronavirus Disease 2019: A Randomized Double-Blind Controlled Trial",
"author": "Mhalla",
"doi-asserted-by": "crossref",
"first-page": "185",
"journal-title": "Clin. Infect Dis.",
"key": "ref_39",
"volume": "76",
"year": "2023"
},
{
"article-title": "Evaluation of zinc sulfate as an adjunctive therapy in COVID-19 critically ill patients: A two center propensity-score matched study",
"author": "Aljuhani",
"first-page": "1",
"journal-title": "Crit. Care",
"key": "ref_40",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1186/cc11316",
"article-title": "Antioxidant micronutrients in the critically ill: A systematic review and meta-analysis",
"author": "Manzanares",
"doi-asserted-by": "crossref",
"first-page": "R66",
"journal-title": "Crit. Care",
"key": "ref_41",
"volume": "16",
"year": "2012"
},
{
"article-title": "Selenium supplementation for critically ill adults",
"author": "Allingstrup",
"first-page": "206",
"journal-title": "Cochrane. Database. Syst. Rev.",
"key": "ref_42",
"volume": "34",
"year": "2015"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/15/15/3308"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Association of Trace Element Levels with Outcomes in Critically Ill COVID-19 Patients",
"type": "journal-article",
"volume": "15"
}
