Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19
et al., Clinical Nutrition, doi:10.1016/j.clnu.2021.04.042, May 2021
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 240 consecutive patients in France, showing significantly higher zinc deficiency in COVID-19 patients, and significantly greater risk of hospitalization for COVID-19 patients with zinc deficiency. 2020PI087.
|
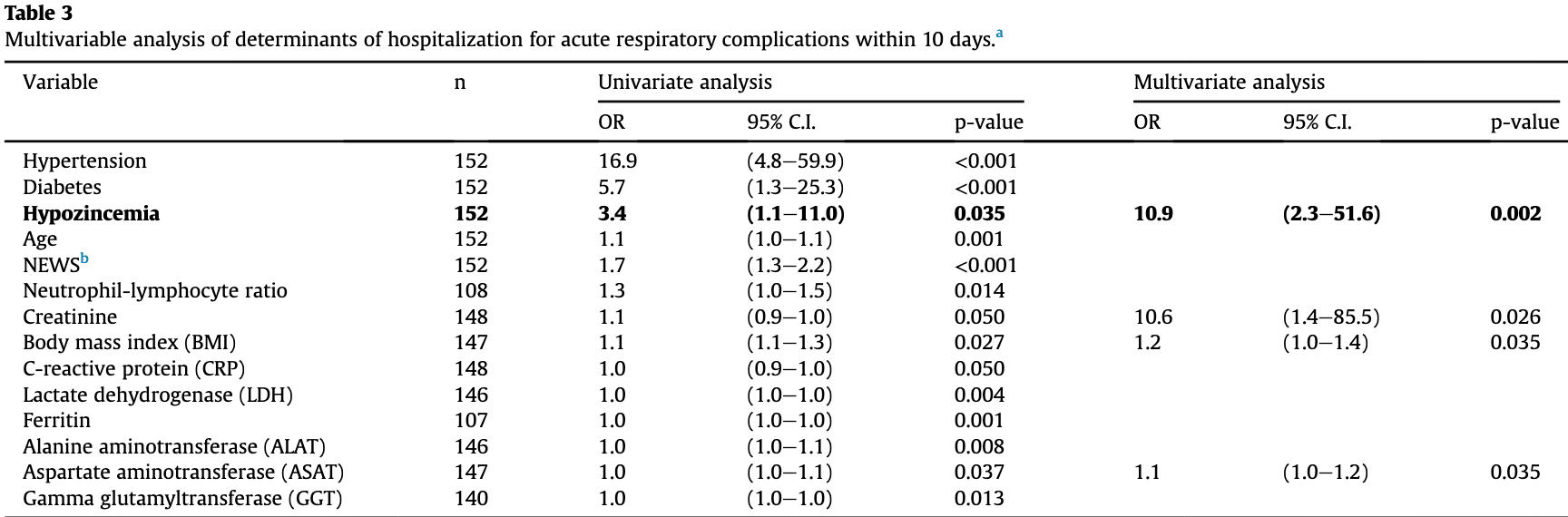
risk of hospitalization, 89.2% lower, RR 0.11, p = 0.002, high zinc levels 6 of 110 (5.5%), low zinc levels 7 of 42 (16.7%), NNT 8.9, inverted to make RR<1 favor high zinc levels, odds ratio converted to relative risk, within COVID-19 patients.
|
|
risk of case, 27.6% lower, RR 0.72, p = 0.003, high zinc levels 110 of 188 (58.5%), low zinc levels 42 of 52 (80.8%), NNT 4.5.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Fromonot et al., 3 May 2021, prospective, France, peer-reviewed, 6 authors.
Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19
Clinical Nutrition, doi:10.1016/j.clnu.2021.04.042
Background & aims: Nutritional predisposition to severe coronavirus disease 2019 (COVID-19) remains unclear. Zinc deficiency could be critical since it is associated with a higher susceptibility to infections. We evaluated the prevalence of hypozincemia in the early stage of COVID-19, its association with risk factors for severe COVID-19 and its prognostic value for hospitalization for respiratory complications within 10 days. Methods: For 152 COVID-19 patients and 88 non-COVID-19 patients admitted to COVID-19 screening centers, national early warning score for COVID-19 (NEWS) and laboratory analyses were performed to identify the risk for severe COVID-19. Multivariable logistic regression analysis assessed whether hypozincemia was an independent predictor of hospitalization for respiratory complications within 10 days (primary judgment criterion). The secondary judgment criteria were high NEWS score (!7), comorbidities and biomarkers associated with severe COVID-19. Results: Hypozincemia was more frequent in COVID-19 patients compared to non-COVID-19 patients (27.6% vs 11.4%; p ¼ 0.003). Older patients (!65 years) and medically assisted nursing home residents were at higher risk of hypozincemia (p < 0.01). Hypozincemia was associated with a worse NEWS score (p < 0.01) and lymphopenia (p < 0.001). Hypozincemia was independently associated with hospitalization for respiratory complications within 10 days (OR ¼ 10.9, 95% CI ¼ 2.3e51.6, p ¼ 0.002). Conclusions: In the early stage of COVID-19, the prevalence of hypozincemia exceeded 20%. Hypozincemia was an independent predictor of hospitalization for respiratory complications within 10 days. This may suggest the importance of early detection and treatment of zinc deficiency in the nutritional management of COVID-19, especially in older people. Therefore, intervention and adjuvant treatment trials are strongly needed.
Conflict of interest The authors declare that they have no conflict of interest.
References
Arnaud, Touvier, Galan, Andriollo-Sanchez, Ruffieux et al., Determinants of serum zinc concentrations in a population of French middle-age subjects (SU.VI.MAX cohort), Eur J Clin Nutr, doi:10.1038/ejcn.2010.118
Barazzoni, Bischoff, Breda, Wickramasinghe, Krznaric et al., Endorsed by the ESPEN council. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection, Clin Nutr, doi:10.1016/j.clnu.2020.03.022
Carlucci, Ahuja, Petrilli, Rajagopalan, Jones et al., Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients, J Med Microbiol, doi:10.1099/jmm.0.001250
De Benoist, Hill, Davidsson, Fontaine, Hotz, Conclusions of the Joint WHO/UNICEF/IAEA/IZiNCG interagency meeting on zinc status indicators, Food Nutr Bull, doi:10.1177/15648265070283s306
Duncan, Talwar, Mcmillan, Stefanowicz, Reilly, Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements, Am J Clin Nutr, doi:10.3945/ajcn.111.023812
Gammoh, Rink, Zinc in infection and inflammation, Nutrients, doi:10.3390/nu9060624
Guan, Ni, Hu, Liang, Ou et al., China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/nejmoa2002032
Heller, Sun, Hackler, Seelig, Seibert et al., Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker, Redox Biol, doi:10.1016/j.redox.2020.101764
Liao, Wang, Kang, Novel coronavirus infection during the 2019e2020 epidemic: preparing intensive care unitsdthe experience in Sichuan Province, China, Intensive Care Med, doi:10.1007/s00134-020-05954-2
Zhao, Li, Ge, Shi, Lv et al., Evaluation of nutrition risk and its association with mortality risk in severely and critically ill COVID-19 patients, J Parenter Enteral Nutr, doi:10.1002/jpen.1953
DOI record:
{
"DOI": "10.1016/j.clnu.2021.04.042",
"ISSN": [
"0261-5614"
],
"URL": "http://dx.doi.org/10.1016/j.clnu.2021.04.042",
"alternative-id": [
"S026156142100234X"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Clinical Nutrition"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.clnu.2021.04.042"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Elsevier Ltd and European Society for Clinical Nutrition and Metabolism. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6726-9125",
"affiliation": [],
"authenticated-orcid": false,
"family": "Fromonot",
"given": "Julien",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-7971-3422",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gette",
"given": "Mickael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ben Lassoued",
"given": "Amin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guéant",
"given": "Jean-Louis",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1402-3716",
"affiliation": [],
"authenticated-orcid": false,
"family": "Guéant-Rodriguez",
"given": "Rosa-Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guieu",
"given": "Régis",
"sequence": "additional"
}
],
"container-title": "Clinical Nutrition",
"container-title-short": "Clinical Nutrition",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"clinicalnutritionjournal.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
5,
4
]
],
"date-time": "2021-05-04T01:24:28Z",
"timestamp": 1620091468000
},
"deposited": {
"date-parts": [
[
2022,
12,
7
]
],
"date-time": "2022-12-07T07:42:59Z",
"timestamp": 1670398979000
},
"indexed": {
"date-parts": [
[
2024,
2,
19
]
],
"date-time": "2024-02-19T13:46:24Z",
"timestamp": 1708350384584
},
"is-referenced-by-count": 16,
"issue": "12",
"issued": {
"date-parts": [
[
2022,
12
]
]
},
"journal-issue": {
"issue": "12",
"published-print": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
12,
1
]
],
"date-time": "2022-12-01T00:00:00Z",
"timestamp": 1669852800000
}
},
{
"URL": "http://www.elsevier.com/open-access/userlicense/1.0/",
"content-version": "am",
"delay-in-days": 364,
"start": {
"date-parts": [
[
2023,
11,
30
]
],
"date-time": "2023-11-30T00:00:00Z",
"timestamp": 1701302400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S026156142100234X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S026156142100234X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "3115-3119",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
12
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.3390/nu9060624",
"article-title": "Zinc in infection and inflammation",
"author": "Gammoh",
"doi-asserted-by": "crossref",
"first-page": "624",
"journal-title": "Nutrients",
"key": "10.1016/j.clnu.2021.04.042_bib1",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1007/s00134-020-05954-2",
"article-title": "Novel coronavirus infection during the 2019–2020 epidemic: preparing intensive care units—the experience in Sichuan Province, China",
"author": "Liao",
"doi-asserted-by": "crossref",
"first-page": "357",
"journal-title": "Intensive Care Med",
"key": "10.1016/j.clnu.2021.04.042_bib2",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1177/15648265070283S306",
"article-title": "Conclusions of the Joint WHO/UNICEF/IAEA/IZiNCG interagency meeting on zinc status indicators",
"author": "de Benoist",
"doi-asserted-by": "crossref",
"first-page": "S480",
"journal-title": "Food Nutr Bull",
"key": "10.1016/j.clnu.2021.04.042_bib3",
"volume": "28",
"year": "2007"
},
{
"DOI": "10.3945/ajcn.111.023812",
"article-title": "Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements",
"author": "Duncan",
"doi-asserted-by": "crossref",
"first-page": "64",
"journal-title": "Am J Clin Nutr",
"key": "10.1016/j.clnu.2021.04.042_bib4",
"volume": "95",
"year": "2012"
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"journal-title": "N Engl J Med",
"key": "10.1016/j.clnu.2021.04.042_bib5",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1038/ejcn.2010.118",
"article-title": "Determinants of serum zinc concentrations in a population of French middle-age subjects (SU.VI.MAX cohort)",
"author": "Arnaud",
"doi-asserted-by": "crossref",
"first-page": "1057",
"journal-title": "Eur J Clin Nutr",
"key": "10.1016/j.clnu.2021.04.042_bib6",
"volume": "64",
"year": "2010"
},
{
"DOI": "10.1016/j.redox.2020.101764",
"article-title": "Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker",
"author": "Heller",
"doi-asserted-by": "crossref",
"first-page": "101764",
"journal-title": "Redox Biol",
"key": "10.1016/j.clnu.2021.04.042_bib7",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1099/jmm.0.001250",
"article-title": "Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients",
"author": "Carlucci",
"doi-asserted-by": "crossref",
"first-page": "1228",
"journal-title": "J Med Microbiol",
"key": "10.1016/j.clnu.2021.04.042_bib8",
"volume": "69",
"year": "2020"
},
{
"article-title": "Evaluation of nutrition risk and its association with mortality risk in severely and critically ill COVID-19 patients",
"author": "Zhao",
"journal-title": "J Parenter Enteral Nutr",
"key": "10.1016/j.clnu.2021.04.042_bib9",
"year": "2020"
},
{
"DOI": "10.1016/j.clnu.2020.03.022",
"article-title": "ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection",
"author": "Barazzoni",
"doi-asserted-by": "crossref",
"first-page": "1631",
"journal-title": "Clin Nutr",
"key": "10.1016/j.clnu.2021.04.042_bib10",
"volume": "39",
"year": "2020"
}
],
"reference-count": 10,
"references-count": 10,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S026156142100234X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Critical Care and Intensive Care Medicine",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "41"
}
