Nutritional parameters and outcomes in patients admitted to intensive care with COVID-19: a retrospective single-centre service evaluation
et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000270, Aug 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 72 ICU patients in the UK, showing higher mortality with vitamin D deficiency, not reaching statistical significance.
This is the 85th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
This may explain in part the very high mortality seen in this study.
Results may differ in countries with improved SOC.
|
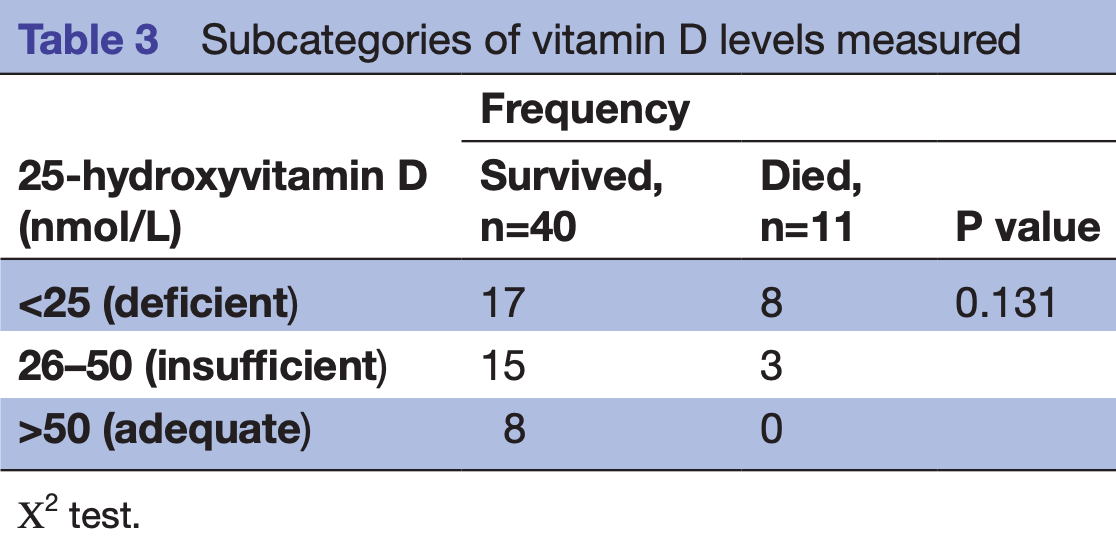
risk of death, 63.9% lower, RR 0.36, p = 0.10, high D levels (≥25nmol/L) 3 of 26 (11.5%), low D levels (<25nmol/L) 8 of 25 (32.0%), NNT 4.9.
|
|
risk of death, 92.9% lower, RR 0.07, p = 0.18, high D levels (≥50nmol/L) 0 of 8 (0.0%), low D levels (<50nmol/L) 11 of 43 (25.6%), NNT 3.9, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Eden et al., 5 Aug 2021, retrospective, United Kingdom, peer-reviewed, 5 authors.
Contact: timothy.eden@nhs.net, @TimothyEdenRD, @ShaneMacZ.
Nutritional parameters and outcomes in patients admitted to intensive care with COVID-19: a retrospective single-centre service evaluation
BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000270
D deficiency may also associate with poorer outcomes and mortality, supporting a possible role of vitamin D in immune function specific to pulmonary inflammation and COVID-19 pathophysiology. There are plausible associations between raised BMI, glycaemic control, vitamin D status and poor prognosis, as seen in wider studies; however, in this service evaluation audit during the first wave of the pandemic in the UK, with a limited data set available for this analysis, the associations did not reach statistical significance. Further research is needed into specific nutritional markers influencing critical care admissions with COVID-19. ► This snapshot audit in a London ICU from the first peak of the COVID-19 pandemic adds to the body of evidence associating overweight/obesity as a risk factor of disease severity and mortality in COVID-19. ► Further data suggesting baseline vitamin D status may influence severity of COVID-19 as higher mortality was observed in individuals with vitamin D deficiency (<25 nmol/L). ► This highlights baseline nutritional parameters that are easily obtainable in the critical care setting and suggests additional nutritional markers worthy of further research.
Contributors TE, JN and SR planned the above service evaluation and determined the data collection. TE and JN collected the relevant data and JN and SR provided the statistical analysis. TE, SM and DC contributed to the report writing and discussion of this service evaluation. SR supervised the undertaking of the work and contributed to the overall revisions prior to submission by TE.
Competing interests None declared. Patient consent for publication Not required. Provenance and peer review Not commissioned; externally peer reviewed by Marcello Scopazzini, NHS Lothian, Edinburgh, UK. Data availability statement All data relevant to the study are included in the article or uploaded as supplemental information. All relevant data and statistical analyses have been included within the submission. For further information and additional data, please contact the first author Timothy Eden ( timothy. eden@ nhs. net). Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology,..
References
Accardi, Caruso, Immune-Inflammatory responses in the elderly: an update, Immun Ageing, doi:10.1186/s12979-018-0117-8
Amrein, Papinutti, Mathew, Vitamin D and critical illness: what endocrinology can learn from intensive care and vice versa, Endocr Connect, doi:10.1530/EC-18-0184
Apicella, Campopiano, Mantuano, COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30238-2
Baker, White, Morgan, Men's health: COVID-19 pandemic highlights need for overdue policy action, Lancet, doi:10.1016/S0140-6736(20)31303-9
Barazzoni, Bischoff, Breda, ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection, Clin Nutr, doi:10.1016/j.clnu.2020.03.022
Barron, Bakhai, Kar, Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a wholepopulation study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30272-2
Berger, Nutrition and micronutrient therapy in critical illness should be individualized, JPEN J Parenter Enteral Nutr, doi:10.1002/jpen.2002
Calder, Nutrition, immunity and COVID-19, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000085
Carpagnano, Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Castillo, Costa, Barrios, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
De, Vega, Barquin, Boros, Could attitudes toward COVID-19 in Spain render men more vulnerable than women?
Faniyi, Lugg, Faustini, Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for COVID-19 like symptoms during the 2020 pandemic, medRxiv, doi:10.1101/2020.10.05.20206706
Finucane, Davenport, Coronavirus, Coronavirus and obesity: could insulin resistance mediate the severity of Covid-19 infection?, Front Public Health, doi:10.3389/fpubh.2020.00184
Griffin, Wall, Blake, Vitamin D status of adults in the community, in outpatient clinics, in hospital, and in nursing homes in the West of Ireland, Journals Gerontol Ser A
Griffith, Sharma, Holliday, Men and COVID-19: a biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions, Prev Chronic Dis, doi:10.5888/pcd17.200247
Hansdottir, Monick, Hinde, Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense, J Immunol, doi:10.4049/jimmunol.181.10.7090
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr, doi:10.1007/s00394-020-02372-4
Hogue, Stearns, Colantuoni, The impact of obesity on outcomes after critical illness: a meta-analysis, Intensive Care Med, doi:10.1007/s00134-009-1424-5
Israel, Cicurel, Feldhamer, The link between vitamin D deficiency and Covid-19 in a large population, medRxiv, doi:10.1101/2020.09.04.20188268
Jong, Chanques, Jaber, Mechanical ventilation in obese ICU patients: from intubation to extubation, Crit Care, doi:10.1186/s13054-017-1641-1
Jong, Jung, Chanques, Obesity and mortality in critically ill patients: another case of the Simpson paradox?, Chest, doi:10.1378/chest.11-3302
Jong, Molinari, Sebbane, Feasibility and effectiveness of prone position in morbidly obese patients with ARDS: a case-control clinical study, Chest, doi:10.1378/chest.12-2115
Kaufman, Niles, Kroll, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Kohlmeier, Avoidance of vitamin D deficiency to slow the COVID-19 pandemic, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000096
Lemyze, Courageux, Maladobry, Implications of obesity for the management of severe coronavirus disease 2019 pneumonia, Crit Care Med, doi:10.1097/CCM.0000000000004455
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Muniyappa, Gubbi, COVID-19 pandemic, coronaviruses, and diabetes mellitus, Am J Physiol Endocrinol Metab, doi:10.1152/ajpendo.00124.2020
Munshi, Hussein, Toraih, Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol, doi:10.1002/jmv.26360
Murad, Coburn, Coto-Yglesias, Glycemic control in non-critically ill hospitalized patients: a systematic review and metaanalysis, J Clin Endocrinol Metab, doi:10.1210/jc.2011-2100
Nair, Venkatesh, Center, Vitamin D deficiency and supplementation in critical illness-the known knowns and known unknowns, Crit Care, doi:10.1186/s13054-018-2185-8
Peckham, De Gruijter, Raine, Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission, Nat Commun, doi:10.1038/s41467-020-19741-6
Peng, Meng, Guan, Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV
Pourshahidi, Vitamin D and obesity: Current perspectives and future directions, doi:10.1017/S0029665114001578
Pugach, Pugach, Strong correlation between prevalence of severe vitamin D deficiency and population mortality rate from COVID-19 in Europe, Wien Klin Wochenschr, doi:10.1007/s00508-021-01833-y
Sama, Ravera, Santema, Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors, Eur Heart J, doi:10.1093/eurheartj/ehaa373
Sharma, Volgman, Michos, Sex differences in mortality from COVID-19 pandemic, JACC: Case Reports, doi:10.1016/j.jaccas.2020.04.027
Simonnet, Chetboun, Poissy, High prevalence of obesity in severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity, doi:10.1002/oby.22831
Steele, Finucane, Griffin, Obesity is associated with altered lung function independently of physical activity and fitness, Obesity, doi:10.1038/oby.2008.584
Vimaleswaran, Berry, Lu, Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts, PLoS Med, doi:10.1371/journal.pmed.1001383
Whittle, Molinger, Macleod, Persistent hypermetabolism and longitudinal energy expenditure in critically ill patients with COVID-19, Crit Care, doi:10.1186/s13054-020-03286-7
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Xin, Guan, Zhi, None, doi:10.3760/cma.j.cn112148-20200220-00105
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
Zittermann, Pilz, Hoffmann, Vitamin D and airway infections: a European perspective, Eur J Med Res, doi:10.1186/s40001-016-0208-y
DOI record:
{
"DOI": "10.1136/bmjnph-2021-000270",
"ISSN": [
"2516-5542"
],
"URL": "http://dx.doi.org/10.1136/bmjnph-2021-000270",
"abstract": "<jats:title>Background</jats:title><jats:p>COVID-19 is an inflammatory syndrome caused by novel coronavirus SARS-CoV-2. Symptoms range from mild infection to severe acute respiratory distress syndrome (ARDS) requiring ventilation and intensive care. At the time of data collection, UK cases were around 300 000 with a fatality rate of 13% necessitating over 10 000 critical care admissions; now there have been over 4 million cases. Nutrition is important to immune function and influences metabolic risk factors such as obesity and glycaemic control, as well as recovery from acute illnesses. Poor nutritional status is associated with worse outcomes in ARDS and viral infections, yet limited research has assessed pre-morbid nutritional status and outcomes in patients critically unwell with COVID-19.</jats:p><jats:sec><jats:title>Objectives</jats:title><jats:p>Investigate the effect of body mass index (BMI), glycaemic control and vitamin D status on outcomes in adult patients with COVID-19 admitted to an intensive care unit (ICU).</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>Retrospective review of all patients admitted to a central London ICU between March and May 2020 with confirmed COVID-19. Electronic patient records data were analysed for patient demographics; comorbidities; admission BMI; and serum vitamin D, zinc, selenium and haemoglobin A1c (HbA1c) concentrations. Serum vitamin D and HbA1c were measured on admission, or within 1 month of admission to ICU. Primary outcome of interest was mortality. Secondary outcomes included time intubated, ICU stay duration and ICU-related morbidity.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Seventy-two patients; 54 (75%) men, mean age 57.1 (±9.8) years, were included. Overall, mortality was 24 (33%). No significant association with mortality was observed across BMI categories. In the survival arm admission, HbA1c (mmol/mol) was lower, 50.2 vs 60.8, but this was not statistically significant. Vitamin D status did not significantly associate with mortality (p=0.131). However, 32% of patients with low vitamin D (<25 IU/L) died, compared with 13% of patients with vitamin D levels >26 IU/L. Serum zinc and selenium, and vitamin B<jats:sub>12</jats:sub> and folate levels were measured in 46% and 26% of patients, respectively.</jats:p></jats:sec><jats:sec><jats:title>Discussion/conclusion</jats:title><jats:p>Increased adiposity and deranged glucose homeostasis may potentially increase risk of COVID-19 infection and severity, possibly relating to impaired lung and metabolic function, increased proinflammatory and prothrombotic mechanisms. Vitamin D deficiency may also associate with poorer outcomes and mortality, supporting a possible role of vitamin D in immune function specific to pulmonary inflammation and COVID-19 pathophysiology. There are plausible associations between raised BMI, glycaemic control, vitamin D status and poor prognosis, as seen in wider studies; however, in this service evaluation audit during the first wave of the pandemic in the UK, with a limited data set available for this analysis, the associations did not reach statistical significance. Further research is needed into specific nutritional markers influencing critical care admissions with COVID-19.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjnph-2021-000270"
],
"author": [
{
"affiliation": [],
"family": "Eden",
"given": "Timothy",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-7166-4299",
"affiliation": [],
"authenticated-orcid": false,
"family": "McAuliffe",
"given": "Shane",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Crocombe",
"given": "Dominic",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Neville",
"given": "Jonathan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ray",
"given": "Sumantra",
"sequence": "additional"
}
],
"container-title": "BMJ Nutrition, Prevention & Health",
"container-title-short": "BMJNPH",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
8,
6
]
],
"date-time": "2021-08-06T16:07:21Z",
"timestamp": 1628266041000
},
"deposited": {
"date-parts": [
[
2021,
12,
30
]
],
"date-time": "2021-12-30T14:42:06Z",
"timestamp": 1640875326000
},
"indexed": {
"date-parts": [
[
2024,
3,
19
]
],
"date-time": "2024-03-19T15:02:39Z",
"timestamp": 1710860559187
},
"is-referenced-by-count": 5,
"issue": "2",
"issued": {
"date-parts": [
[
2021,
8,
6
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2021,
12,
29
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
6
]
],
"date-time": "2021-08-06T00:00:00Z",
"timestamp": 1628208000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjnph-2021-000270",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "416-424",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
8,
6
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
6
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "BMJ",
"reference": [
{
"key": "2021123006401107000_4.2.416.1",
"unstructured": "Intensive Care National Audit and Research Centre (ICNARC) . ICNARC report on COVID-19 in critical care 31 July 2020, 2020."
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.2"
},
{
"DOI": "10.1016/j.clnu.2020.03.022",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.3"
},
{
"DOI": "10.1002/oby.22831",
"article-title": "High prevalence of obesity in severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation",
"author": "Simonnet",
"doi-asserted-by": "crossref",
"first-page": "1195",
"journal-title": "Obesity",
"key": "2021123006401107000_4.2.416.4",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.5"
},
{
"DOI": "10.1038/oby.2008.584",
"article-title": "Obesity is associated with altered lung function independently of physical activity and fitness",
"author": "Steele",
"doi-asserted-by": "crossref",
"first-page": "578",
"journal-title": "Obesity",
"key": "2021123006401107000_4.2.416.6",
"volume": "17",
"year": "2009"
},
{
"article-title": "[Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV]",
"author": "Peng",
"first-page": "450",
"journal-title": "Zhonghua Xin Xue Guan Bing Za Zhi",
"key": "2021123006401107000_4.2.416.7",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"article-title": "Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study",
"author": "Barron",
"doi-asserted-by": "crossref",
"first-page": "813",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2021123006401107000_4.2.416.8",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1210/jc.2011-2100",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.9"
},
{
"DOI": "10.1186/s40001-016-0208-y",
"article-title": "Vitamin D and airway infections: a European perspective",
"author": "Zittermann",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Eur J Med Res",
"key": "2021123006401107000_4.2.416.10",
"volume": "21",
"year": "2016"
},
{
"key": "2021123006401107000_4.2.416.11",
"unstructured": "NDNS: results from Years 1 to 4 (combined) - GOV.UK [Internet]. PHE and FSA (2014b) Statistical Press Notice: National Diet and Nutrition Survey: results from years 1, 2, 3 and 4 combined (2008/09 – 2011/12). Public Health England and Food Standards Agency. [cited 2021 Jan 24]. Available: https://www.gov.uk/government/statistics/national-diet-and-nutrition-survey-results-from-years-1-to-4-combined-of-the-rolling-programme-for-2008-and-2009-to-2011-and-2012"
},
{
"DOI": "10.1007/s00508-021-01833-y",
"article-title": "Strong correlation between prevalence of severe vitamin D deficiency and population mortality rate from COVID-19 in Europe",
"author": "Pugach",
"doi-asserted-by": "crossref",
"first-page": "403",
"journal-title": "Wien Klin Wochenschr",
"key": "2021123006401107000_4.2.416.12",
"volume": "133",
"year": "2021"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.13"
},
{
"DOI": "10.1016/S0140-6736(20)31303-9",
"article-title": "Men's health: COVID-19 pandemic highlights need for overdue policy action",
"author": "Baker",
"doi-asserted-by": "crossref",
"first-page": "1886",
"journal-title": "Lancet",
"key": "2021123006401107000_4.2.416.14",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1186/s12979-018-0117-8",
"article-title": "Immune-Inflammatory responses in the elderly: an update",
"author": "Accardi",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "Immun Ageing",
"key": "2021123006401107000_4.2.416.15",
"volume": "15",
"year": "2018"
},
{
"DOI": "10.1038/s41467-019-13889-6",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.16"
},
{
"DOI": "10.5888/pcd17.200247",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.17"
},
{
"DOI": "10.1093/eurheartj/ehaa373",
"article-title": "Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors",
"author": "Sama",
"doi-asserted-by": "crossref",
"first-page": "1810",
"journal-title": "Eur Heart J",
"key": "2021123006401107000_4.2.416.18",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1016/j.jaccas.2020.04.027",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.19"
},
{
"DOI": "10.31234/osf.io/dyxqn",
"doi-asserted-by": "crossref",
"key": "2021123006401107000_4.2.416.20",
"unstructured": "De La Vega R , Barquin RR , Boros S . Could attitudes toward COVID-19 in Spain render men more vulnerable than women? [cited 2020 Oct 25], 2020. Available: https://psyarxiv.com/dyxqn/"
},
{
"DOI": "10.1097/CCM.0000000000004455",
"article-title": "Implications of obesity for the management of severe coronavirus disease 2019 pneumonia",
"author": "Lemyze",
"doi-asserted-by": "crossref",
"first-page": "e761",
"journal-title": "Crit Care Med",
"key": "2021123006401107000_4.2.416.21",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.00184",
"article-title": "Coronavirus and obesity: could insulin resistance mediate the severity of Covid-19 infection?",
"author": "Finucane",
"doi-asserted-by": "crossref",
"first-page": "184",
"journal-title": "Front Public Health",
"key": "2021123006401107000_4.2.416.22",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.23"
},
{
"DOI": "10.1007/s00134-009-1424-5",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.24"
},
{
"DOI": "10.1378/chest.12-2115",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.25"
},
{
"DOI": "10.1378/chest.11-3302",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.26"
},
{
"DOI": "10.1186/s13054-020-03286-7",
"article-title": "Persistent hypermetabolism and longitudinal energy expenditure in critically ill patients with COVID-19",
"author": "Whittle",
"doi-asserted-by": "crossref",
"first-page": "581",
"journal-title": "Crit Care",
"key": "2021123006401107000_4.2.416.27",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1186/s13054-017-1641-1",
"article-title": "Mechanical ventilation in obese ICU patients: from intubation to extubation",
"author": "De Jong",
"doi-asserted-by": "crossref",
"first-page": "63",
"journal-title": "Crit Care",
"key": "2021123006401107000_4.2.416.28",
"volume": "21",
"year": "2017"
},
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"article-title": "COVID-19 in people with diabetes: understanding the reasons for worse outcomes",
"author": "Apicella",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2021123006401107000_4.2.416.29",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1152/ajpendo.00124.2020",
"article-title": "COVID-19 pandemic, coronaviruses, and diabetes mellitus",
"author": "Muniyappa",
"doi-asserted-by": "crossref",
"first-page": "E736",
"journal-title": "Am J Physiol Endocrinol Metab",
"key": "2021123006401107000_4.2.416.30",
"volume": "318",
"year": "2020"
},
{
"DOI": "10.1007/s00394-020-02372-4",
"article-title": "Vitamin D and COVID-19 infection and mortality in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "545",
"journal-title": "Eur J Nutr",
"key": "2021123006401107000_4.2.416.31",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1101/2020.10.05.20206706",
"doi-asserted-by": "crossref",
"key": "2021123006401107000_4.2.416.32",
"unstructured": "Faniyi AA , Lugg ST , Faustini SE . Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for COVID-19 like symptoms during the 2020 pandemic. medRxiv 2020.doi:10.1101/2020.10.05.20206706"
},
{
"DOI": "10.1101/2020.09.04.20188268",
"doi-asserted-by": "crossref",
"key": "2021123006401107000_4.2.416.33",
"unstructured": "Israel A , Cicurel A , Feldhamer I . The link between vitamin D deficiency and Covid-19 in a large population. medRxiv 2020.doi:10.1101/2020.09.04.20188268"
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.34"
},
{
"author": "Pourshahidi",
"first-page": "115",
"key": "2021123006401107000_4.2.416.35",
"volume": "74",
"volume-title": "Proceedings of the Nutrition Society [Internet",
"year": "2015"
},
{
"DOI": "10.1093/gerona/glaa010",
"doi-asserted-by": "crossref",
"key": "2021123006401107000_4.2.416.36",
"unstructured": "Griffin TP , Wall D , Blake L . Vitamin D status of adults in the community, in outpatient clinics, in hospital, and in nursing homes in the West of Ireland. Journals Gerontol Ser A [Internet] 2020 https://pubmed.ncbi.nlm.nih.gov/31942614/"
},
{
"DOI": "10.1371/journal.pmed.1001383",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.37"
},
{
"DOI": "10.1136/bmjnph-2020-000096",
"article-title": "Avoidance of vitamin D deficiency to slow the COVID-19 pandemic",
"author": "Kohlmeier",
"doi-asserted-by": "crossref",
"first-page": "67",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021123006401107000_4.2.416.38",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1186/s13054-018-2185-8",
"article-title": "Vitamin D deficiency and supplementation in critical illness-the known knowns and known unknowns",
"author": "Nair",
"doi-asserted-by": "crossref",
"first-page": "276",
"journal-title": "Crit Care",
"key": "2021123006401107000_4.2.416.39",
"volume": "22",
"year": "2018"
},
{
"DOI": "10.1530/EC-18-0184",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.40"
},
{
"DOI": "10.4049/jimmunol.181.10.7090",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.41"
},
{
"DOI": "10.1002/jmv.26360",
"article-title": "Vitamin D insufficiency as a potential culprit in critical COVID-19 patients",
"author": "Munshi",
"doi-asserted-by": "crossref",
"first-page": "733",
"journal-title": "J Med Virol",
"key": "2021123006401107000_4.2.416.42",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"article-title": "Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19",
"author": "Carpagnano",
"doi-asserted-by": "crossref",
"first-page": "765",
"journal-title": "J Endocrinol Invest",
"key": "2021123006401107000_4.2.416.43",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "2021123006401107000_4.2.416.44"
},
{
"DOI": "10.1002/jpen.2002",
"article-title": "Nutrition and micronutrient therapy in critical illness should be individualized",
"author": "Berger",
"doi-asserted-by": "crossref",
"first-page": "1380",
"journal-title": "JPEN J Parenter Enteral Nutr",
"key": "2021123006401107000_4.2.416.45",
"volume": "44",
"year": "2020"
}
],
"reference-count": 45,
"references-count": 45,
"relation": {},
"resource": {
"primary": {
"URL": "https://nutrition.bmj.com/lookup/doi/10.1136/bmjnph-2021-000270"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Medicine (miscellaneous)",
"Health (social science)"
],
"subtitle": [],
"title": "Nutritional parameters and outcomes in patients admitted to intensive care with COVID-19: a retrospective single-centre service evaluation",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "4"
}
