Vitamin D Deficiency in COVID-19 Patients and Role of Calcifediol Supplementation
et al., Nutrients, doi:10.3390/nu15153392, Jul 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
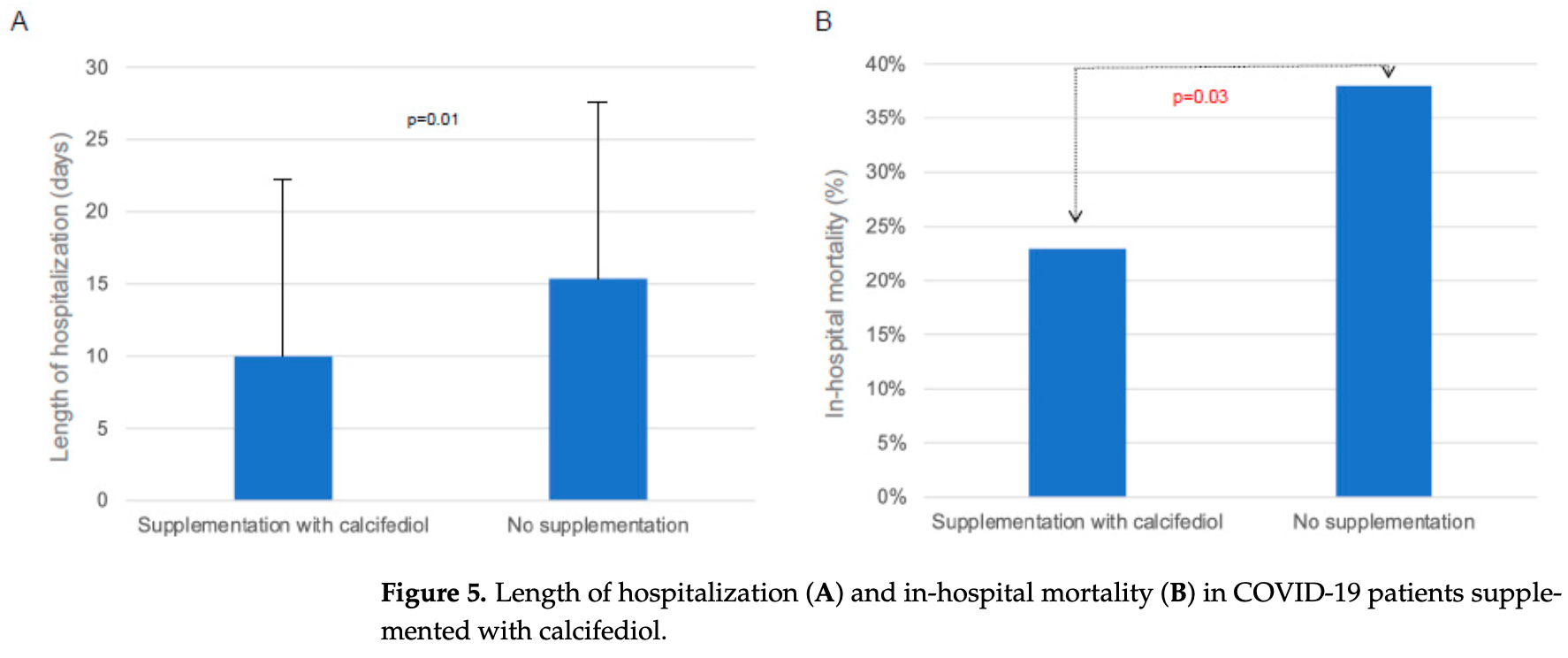
Retrospective 288 hospitalized COVID-19 patients in Italy, showing lower mortality and shorter hospitalization with calcifediol. Results may underestimate the benefits because only higher risk patients with vitamin D deficiency received supplementation. Treated patients also had significantly higher BMI.
83% of patients had vitamin D insufficiency (levels <30 ng/mL). Lower vitamin D levels correlated with higher inflammation markers. Patients with severe vitamin D deficiency (<10 ng/mL) had significantly higher mortality compared to those with levels >10 ng/mL.
Meta-analysis shows that late stage treatment with calcitriol / calcifediol (or
paricalcitol, alfacalcidol, etc.) is more effective than cholecalciferol: 66% [47‑78%] lower risk vs. 45% [34‑54%] lower risk.
Cholecalciferol requires two hydroxylation steps to become activated - first
in the liver to calcifediol, then in the kidney to calcitriol. Calcitriol,
paricalcitol, and alfacalcidol are active vitamin D analogs that do not
require conversion. This allows them to have more rapid onset of action
compared to cholecalciferol. The time delay for cholecalciferol to increase
serum calcifediol levels can be 2-3 days, and the delay for converting
calcifediol to active calcitriol can be up to 7 days.
This is the 121st of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
|
risk of death, 38.8% lower, RR 0.61, p = 0.04, treatment 13 of 56 (23.2%), control 88 of 232 (37.9%), NNT 6.8.
|
|
risk of oxygen therapy, 23.1% lower, RR 0.77, p = 0.22, treatment 18 of 56 (32.1%), control 97 of 232 (41.8%), NNT 10.
|
|
hospitalization time, 34.6% lower, relative time 0.65, p = 0.01, treatment 56, control 232.
|
|
risk of death, 49.8% lower, RR 0.50, p = 0.005, cutoff 10ng/mL, outcome based on serum levels.
|
|
risk of death, 35.9% lower, RR 0.64, p = 0.04, cutoff 20ng/mL, outcome based on serum levels.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Mingiano et al., 30 Jul 2023, retrospective, Italy, peer-reviewed, 11 authors, study period November 2020 - February 2021, dosage calcifediol 450μg days 1-2, patients with deficiency only.
Contact: merlotti4@unisi.it (corresponding author), mingiano2@student.unisi.it, guido.cavati@student.unisi.it, pirrotta@student.unisi.it, m.calabrese5@student.unisi.it, ranuccio.nuti@unisi.it, stefano.gonnelli@unisi.it, bruno.frediani@unisi.it, luigi.gennari@unisi.it, tommaso.picchioni@uslcentro.toscana.it, alberto.fortini@uslcentro.toscana.it, daniela.merlotti@ao-siena.toscana.it.
Vitamin D Deficiency in COVID-19 Patients and Role of Calcifediol Supplementation
Nutrients, doi:10.3390/nu15153392
Hypovitaminosis D has been associated with worse outcome in respiratory tract infections, with conflicting opinions regarding its role in Coronavirus-19 disease . Our study aimed to evaluate the possible relationship between 25-OH vitamin D (25OHD) values and the following conditions in patients hospitalized for COVID-19: prognosis, mortality, invasive (IV) and non-invasive (NIV) mechanical ventilation, and orotracheal intubation (OTI). A further objective was the analysis of a possible positive effect of supplementation with calcifediol on COVID-19 severity and prognosis. We analyzed 288 patients hospitalized at the San Giovanni di Dio Hospital in Florence and the Santa Maria alle Scotte Hospital in Siena, from November 2020 to February 2021. The 25OHD levels correlated positively with the partial pressure of oxygen and FiO2 (PaO2/FiO2) ratio (r = 0.17; p < 0.05). Furthermore, when we analyzed the patients according to the type of respiratory support, we found that 25OHD levels were markedly reduced in patients who underwent non-invasive ventilation and orotracheal intubation (OTI). The evaluation of the length of hospitalization in our population evidenced a longer duration of hospitalization in patients with severe 25OHD deficiency (<10 ng/mL). Moreover, we found a statistically significant difference in the mortality rate between patients who had 25OHD levels below 10 ng/mL and those with levels above this threshold in the total population (50.8% vs. 25.5%, p = 0.005), as well as between patients with 25OHD levels below 20 ng/mL and those with levels above that threshold (38.4% vs. 24.6%, p = 0.04). Moreover, COVID-19 patients supplemented with calcifediol presented a significantly reduced length of hospitalization (p < 0.05). Interestingly, when we analyzed the possible effects of calcifediol on mortality rate in patients with COVID-19, we found that the percentage of deaths was significantly higher in patients who did not receive any supplementation than in those who were treated with calcifediol (p < 0.05) In conclusion, we have demonstrated with our study the best prognosis of COVID-19 patients with adequate vitamin D levels and patients treated with calcifediol supplementation.
Funding: This research received no external funding.
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Azienda Ospedaliera Universitaria Senese (protocol code: Livelli_VIT_D_COVID19, date of approval: 30 November 2020). Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflict of interest.
References
Akbar, Wibowo, Pranata, Setiabudiawan, Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated with Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J. Infect. Public Health, doi:10.1016/j.jiph.2020.06.021
Bakaloudi, Chourdakis, A critical update on the role of mild and serious vitamin D deficiency prevalence and the COVID-19 epidemic in Europe, Nutrition, doi:10.1016/j.nut.2021.111441
Bičíková, Máčová, Hill, Vitamin D as a Possible COVID-19 Prevention Strategy, Int. J. Mol. Sci, doi:10.3390/ijms231810532
Bouillon, Schuit, Antonio, Rastinejad, Vitamin D Binding Protein: A Historic Overview, Front. Endocrinol, doi:10.3389/fendo.2019.00910
Cai, Sex difference and smoking predisposition in patients with COVID-19, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30117-X
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy, BMC Infect. Dis
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Channappanavar, Perlman, Pathogenic human coronavirus infections: Causes and consequences of cytokine storm and immunopathology, Semin. Immunopathol, doi:10.1007/s00281-017-0629-x
Charoenngam, Shirvani, Holick, Vitamin D for skeletal and non-skeletal health: What we should know, J. Clin. Orthop. Trauma, doi:10.1016/j.jcot.2019.07.004
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front. Public Health
Davoudi, Najafi, Aarabi, Tayebi, Nikaeen et al., Lack of association between vitamin D insufficiency and clinical outcomes of patients with COVID-19 infection, BMC Infect. Dis, doi:10.1186/s12879-021-06168-7
De Niet, Trémège, Coffiner, Rousseau, Calmes et al., Positive Effects of Vitamin D Supplementation in Patients Hospitalized for COVID-19: A Randomized, Double-Blind, Placebo-Controlled Trial, Nutrients, doi:10.3390/nu14153048
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, J. Med. Virol, doi:10.1002/jmv.26832
Ferreira, Kleijwegt, Waelkens, Lage, Nikolic et al., Differential protein pathways in 1,25-dihydroxyvitamin D 3 and dexamethasone modulated tolerogenic human dendritic cells, J. Proteome Res, doi:10.1021/pr200724e
Gombart, Borregaard, Koeffler, Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3, FASEB J
Güven, Gültekin, Association of 25-Hydroxyvitamin D Level with COVID-19-Related in-Hospital Mortality: A Retrospective Cohort Study, J. Am. Nutr. Assoc, doi:10.1080/07315724.2021.1935361
Haussler, Jurutka, Mizwicki, Norman, Vitamin D receptor (VDR)-mediated actions of 1α,25(OH) 2 vitamin D 3 : Genomic and non-genomic mechanisms, Best. Pract. Res. Clin. Endocrinol. Metab, doi:10.1016/j.beem.2011.05.010
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-0385
Ikeda, Wakita, Ohkuri, Chamoto, Kitamura et al., T. 1α,25-Dihydroxyvitamin D3 and all-trans retinoic acid synergistically inhibit the differentiation and expansion of Th17 cells, Immunol. Lett, doi:10.1016/j.imlet.2010.07.002
Jeffery, Wood, Qureshi, Hou, Gardner et al., Availability of 25-hydroxyvitamin D 3 to APCs controls the balance between regulatory and inflammatory T cell responses, J. Immunol, doi:10.4049/jimmunol.1200786
Jolliffe, Camargo, Jr, Sluyter, Aglipay et al., Vitamin D supplementation to prevent acute respiratory infections: A systematic review and meta-analysis of aggregate data from randomised controlled trials, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00051-6
Kundu, Chain, Coussens, Khoo, Noursadeghi, Regulation of CYP27B1 and CYP24A1 hydroxylases limits cell-autonomous activation of vitamin D in dendritic cells, Eur. J. Immunol, doi:10.1002/eji.201344157
Li, Guan, Wu, Wang, Zhou et al., Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia, N. Engl. J. Med, doi:10.1056/NEJMoa2001316
Liu, Schenk, Walker, Dempsey, Kanchanapoomi et al., Convergence of IL-1beta and VDR activation pathways in human TLR2/1-induced antimicrobial responses, PLoS ONE, doi:10.1371/journal.pone.0005810
Liu, Stenger, Li, Wenzel, Tan et al., Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response, Science, doi:10.1126/science.1123933
Maghbooli, Sahraian, Jamalimoghadamsiahkali, Asadi, Zarei et al., Treatment With 25-Hydroxyvitamin D 3 (Calcifediol) Is Associated with a Reduction in the Blood Neutrophil-to-Lymphocyte Ratio Marker of Disease Severity in Hospitalized Patients with COVID-19: A Pilot Multicenter, Randomized, Placebo-Controlled, Double-Blinded Clinical Trial, Endocr. Pract, doi:10.1016/j.eprac.2021.09.016
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Mathieu, Vitamin D and the immune system, doi:10.1138/20110505
Merlotti, Rendina, Muscariello, Picchioni, Alessandri et al., Preventive Role of Vitamin D Supplementation for Acute Phase Reaction after Bisphosphonate Infusion in Paget's Disease, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgz138
Nguyen, Raju, Da Graca, Wang, Mohamed et al., 25-hydroxyvitamin D is a predictor of COVID-19 severity of hospitalized patients, PLoS ONE, doi:10.1371/journal.pone.0268038
Nielsen, Junker, Boelt, Cohen, Munger et al., Vitamin D status and severity of COVID-19, Sci. Rep, doi:10.1038/s41598-022-21513-9
Nogues, Ovejero, Pineda-Moncusí, Bouillon, Arenas et al., Calcifediol Treatment and COVID-19-Related Outcomes, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgab405
Palmer, Lee, Maynard, Oliver, Bikle et al., Lineage-specific effects of 1,25-dihydroxyvitamin D 3 on the development of effector CD4 T cells, J. Biol. Chem, doi:10.1074/jbc.M110.163790
Pereira, Dantas Damascena, Galvão Azevedo, De Almeida Oliveira, Da Mota Santana, Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1841090
Quesada-Gomez, Lopez-Miranda, Entrenas-Castillo, Casado-Díaz, Nogues et al., Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol, Nutrients, doi:10.3390/nu14132716
Reid, Toole, Knox, Talwar, Harten et al., The relation between acute changes in the systemic inflammatory response and plasma 25-hydroxyvitamin D concentrations after elective knee arthroplasty, Am. J. Clin. Nutr, doi:10.3945/ajcn.110.008490
Saponaro, Franzini, Okoye, Antognoli, Campi et al., Is There a Crucial Link Between Vitamin D Status and Inflammatory Response in Patients with COVID-19?, Front. Immunol, doi:10.3389/fimmu.2021.745713
Sha, Qie, Yao, Sun, Wang et al., Sex Differences on Clinical Characteristics, Severity, and Mortality in Adult Patients With COVID-19: A Multicentre Retrospective Study, doi:10.3389/fmed.2021.607059
Shah, Saxena, Mavalankar, Vitamin D supplementation, COVID-19 and disease severity: A meta-analysis, QJM, doi:10.1093/qjmed/hcab009
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence, doi:10.1016/j.metabol.2020.154434
Stroehlein, Wallqvist, Iannizzi, Mikolajewska, Metzendorf et al., Vitamin D supplementation for the treatment of COVID-19: A living systematic review, doi:10.1002/14651858.CD015043
Taylor, Finney-Hayward, Quint, Thomas, Tudhope et al., Defective macrophage phagocytosis of bacteria in COPD, Eur. Respir. J, doi:10.1183/09031936.00036709
Tentolouris, Samakidou, Eleftheriadou, Tentolouris, Jude, The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression, Diabetes Metab. Res. Rev, doi:10.1002/dmrr.3517
Vanherwegen, Gysemans, Mathieu, Vitamin D endocrinology on the cross-road between immunity and metabolism, Mol. Cell Endocrinol, doi:10.1016/j.mce.2017.04.018
Wang, Wang, Li, Chen, Han et al., Human Cathelicidin Inhibits SARS-CoV-2 Infection: Killing Two Birds with One Stone, ACS Infect. Dis, doi:10.1021/acsinfecdis.1c00096
Wang, Zhu, Deluca, Where is the vitamin D receptor?, Arch. Biochem. Biophys, doi:10.1016/j.abb.2012.04.001
Watkins, Lemonovich, Salata, An update on the association of vitamin D deficiency with common infectious diseases, Can. J. Physiol. Pharmacol, doi:10.1139/cjpp-2014-0352
Wimalawansa, Rapidly Increasing Serum 25(OH)D Boosts the Immune System, against Infections-Sepsis and COVID-19, Nutrients, doi:10.3390/nu14142997
Wu, Chen, Cai, Xia, Zhou et al., Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.0994
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., Effects of Vitamin D on COVID-19 Infection and Prognosis: A Systematic Review, Risk Manag. Healthc. Policy, doi:10.2147/RMHP.S291584
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.3390/nu15153392",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu15153392",
"abstract": "<jats:p>Hypovitaminosis D has been associated with worse outcome in respiratory tract infections, with conflicting opinions regarding its role in Coronavirus-19 disease (COVID-19). Our study aimed to evaluate the possible relationship between 25-OH vitamin D (25OHD) values and the following conditions in patients hospitalized for COVID-19: prognosis, mortality, invasive (IV) and non-invasive (NIV) mechanical ventilation, and orotracheal intubation (OTI). A further objective was the analysis of a possible positive effect of supplementation with calcifediol on COVID-19 severity and prognosis. We analyzed 288 patients hospitalized at the San Giovanni di Dio Hospital in Florence and the Santa Maria alle Scotte Hospital in Siena, from November 2020 to February 2021. The 25OHD levels correlated positively with the partial pressure of oxygen and FiO2 (PaO2/FiO2) ratio (r = 0.17; p < 0.05). Furthermore, when we analyzed the patients according to the type of respiratory support, we found that 25OHD levels were markedly reduced in patients who underwent non-invasive ventilation and orotracheal intubation (OTI). The evaluation of the length of hospitalization in our population evidenced a longer duration of hospitalization in patients with severe 25OHD deficiency (<10 ng/mL). Moreover, we found a statistically significant difference in the mortality rate between patients who had 25OHD levels below 10 ng/mL and those with levels above this threshold in the total population (50.8% vs. 25.5%, p = 0.005), as well as between patients with 25OHD levels below 20 ng/mL and those with levels above that threshold (38.4% vs. 24.6%, p = 0.04). Moreover, COVID-19 patients supplemented with calcifediol presented a significantly reduced length of hospitalization (p < 0.05). Interestingly, when we analyzed the possible effects of calcifediol on mortality rate in patients with COVID-19, we found that the percentage of deaths was significantly higher in patients who did not receive any supplementation than in those who were treated with calcifediol (p < 0.05) In conclusion, we have demonstrated with our study the best prognosis of COVID-19 patients with adequate vitamin D levels and patients treated with calcifediol supplementation.</jats:p>",
"alternative-id": [
"nu15153392"
],
"author": [
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Mingiano",
"given": "Christian",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Internal Medicine Unit, Ospedale San Giovanni di Dio, 50143 Florence, Italy"
}
],
"family": "Picchioni",
"given": "Tommaso",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Cavati",
"given": "Guido",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Pirrotta",
"given": "Filippo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Calabrese",
"given": "Marco",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Nuti",
"given": "Ranuccio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Gonnelli",
"given": "Stefano",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Internal Medicine Unit, Ospedale San Giovanni di Dio, 50143 Florence, Italy"
}
],
"family": "Fortini",
"given": "Alberto",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Frediani",
"given": "Bruno",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Surgery and Neuroscience, University of Siena, 53100 Siena, Italy"
}
],
"family": "Gennari",
"given": "Luigi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3338-6339",
"affiliation": [
{
"name": "Department of Medical Sciences, Azienda Ospedaliera Universitaria Senese, 53100 Siena, Italy"
}
],
"authenticated-orcid": false,
"family": "Merlotti",
"given": "Daniela",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
7,
31
]
],
"date-time": "2023-07-31T05:48:50Z",
"timestamp": 1690782530000
},
"deposited": {
"date-parts": [
[
2023,
7,
31
]
],
"date-time": "2023-07-31T06:23:46Z",
"timestamp": 1690784626000
},
"indexed": {
"date-parts": [
[
2023,
8,
1
]
],
"date-time": "2023-08-01T04:28:51Z",
"timestamp": 1690864131850
},
"is-referenced-by-count": 0,
"issue": "15",
"issued": {
"date-parts": [
[
2023,
7,
30
]
]
},
"journal-issue": {
"issue": "15",
"published-online": {
"date-parts": [
[
2023,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
7,
30
]
],
"date-time": "2023-07-30T00:00:00Z",
"timestamp": 1690675200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/15/15/3392/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3392",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
7,
30
]
]
},
"published-online": {
"date-parts": [
[
2023,
7,
30
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1056/NEJMoa2001316",
"article-title": "Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1199",
"journal-title": "N. Engl. J. Med.",
"key": "ref_1",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"article-title": "Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "934",
"journal-title": "JAMA Intern. Med.",
"key": "ref_2",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"journal-title": "Lancet",
"key": "ref_3",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30117-X",
"article-title": "Sex difference and smoking predisposition in patients with COVID-19",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "e20",
"journal-title": "Lancet Respir. Med.",
"key": "ref_4",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2021.607059",
"article-title": "Sex Differences on Clinical Characteristics, Severity, and Mortality in Adult Patients With COVID-19: A Multicentre Retrospective Study",
"author": "Sha",
"doi-asserted-by": "crossref",
"first-page": "607059",
"journal-title": "Front. Med.",
"key": "ref_5",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.jcot.2019.07.004",
"article-title": "Vitamin D for skeletal and non-skeletal health: What we should know",
"author": "Charoenngam",
"doi-asserted-by": "crossref",
"first-page": "1082",
"journal-title": "J. Clin. Orthop. Trauma.",
"key": "ref_6",
"volume": "6",
"year": "2019"
},
{
"DOI": "10.1016/j.abb.2012.04.001",
"article-title": "Where is the vitamin D receptor?",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Arch. Biochem. Biophys.",
"key": "ref_7",
"volume": "523",
"year": "2012"
},
{
"DOI": "10.1016/j.beem.2011.05.010",
"article-title": "Vitamin D receptor (VDR)-mediated actions of 1α,25(OH)₂vitamin D₃: Genomic and non-genomic mechanisms",
"author": "Haussler",
"doi-asserted-by": "crossref",
"first-page": "543",
"journal-title": "Best. Pract. Res. Clin. Endocrinol. Metab.",
"key": "ref_8",
"volume": "25",
"year": "2011"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "i6583",
"journal-title": "BMJ",
"key": "ref_9",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.1016/S2213-8587(21)00051-6",
"article-title": "Vitamin D supplementation to prevent acute respiratory infections: A systematic review and meta-analysis of aggregate data from randomised controlled trials",
"author": "Jolliffe",
"doi-asserted-by": "crossref",
"first-page": "276",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "ref_10",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1002/eji.201344157",
"article-title": "Regulation of CYP27B1 and CYP24A1 hydroxylases limits cell-autonomous activation of vitamin D in dendritic cells",
"author": "Kundu",
"doi-asserted-by": "crossref",
"first-page": "1781",
"journal-title": "Eur. J. Immunol.",
"key": "ref_11",
"volume": "44",
"year": "2014"
},
{
"DOI": "10.1126/science.1123933",
"article-title": "Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1770",
"journal-title": "Science",
"key": "ref_12",
"volume": "311",
"year": "2006"
},
{
"DOI": "10.1371/journal.pone.0005810",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Liu, P.T., Schenk, M., Walker, V.P., Dempsey, P.W., Kanchanapoomi, M., Wheelwright, M., Vazirnia, A., Zhang, X., Steinmeyer, A., and Zügel, U. (2009). Convergence of IL-1beta and VDR activation pathways in human TLR2/1-induced antimicrobial responses. PLoS ONE, 4."
},
{
"DOI": "10.1139/cjpp-2014-0352",
"article-title": "An update on the association of vitamin D deficiency with common infectious diseases",
"author": "Watkins",
"doi-asserted-by": "crossref",
"first-page": "363",
"journal-title": "Can. J. Physiol. Pharmacol.",
"key": "ref_14",
"volume": "93",
"year": "2015"
},
{
"DOI": "10.1183/09031936.00036709",
"article-title": "Defective macrophage phagocytosis of bacteria in COPD",
"author": "Taylor",
"doi-asserted-by": "crossref",
"first-page": "1039",
"journal-title": "Eur. Respir. J.",
"key": "ref_15",
"volume": "35",
"year": "2010"
},
{
"DOI": "10.1021/pr200724e",
"article-title": "Differential protein pathways in 1,25-dihydroxyvitamin D3 and dexamethasone modulated tolerogenic human dendritic cells",
"author": "Ferreira",
"doi-asserted-by": "crossref",
"first-page": "941",
"journal-title": "J. Proteome Res.",
"key": "ref_16",
"volume": "11",
"year": "2012"
},
{
"DOI": "10.1096/fj.04-3284com",
"article-title": "Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3",
"author": "Gombart",
"doi-asserted-by": "crossref",
"first-page": "1067",
"journal-title": "FASEB J.",
"key": "ref_17",
"volume": "19",
"year": "2005"
},
{
"DOI": "10.1021/acsinfecdis.1c00096",
"article-title": "Human Cathelicidin Inhibits SARS-CoV-2 Infection: Killing Two Birds with One Stone",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1545",
"journal-title": "ACS Infect. Dis.",
"key": "ref_18",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.4049/jimmunol.1200786",
"article-title": "Availability of 25-hydroxyvitamin D3 to APCs controls the balance between regulatory and inflammatory T cell responses",
"author": "Jeffery",
"doi-asserted-by": "crossref",
"first-page": "5155",
"journal-title": "J. Immunol.",
"key": "ref_19",
"volume": "189",
"year": "2012"
},
{
"DOI": "10.1016/j.imlet.2010.07.002",
"article-title": "1α,25-Dihydroxyvitamin D3 and all-trans retinoic acid synergistically inhibit the differentiation and expansion of Th17 cells",
"author": "Ikeda",
"doi-asserted-by": "crossref",
"first-page": "7",
"journal-title": "Immunol. Lett.",
"key": "ref_20",
"volume": "134",
"year": "2010"
},
{
"DOI": "10.1074/jbc.M110.163790",
"article-title": "Lineage-specific effects of 1,25-dihydroxyvitamin D3 on the development of effector CD4 T cells",
"author": "Palmer",
"doi-asserted-by": "crossref",
"first-page": "997",
"journal-title": "J. Biol. Chem.",
"key": "ref_21",
"volume": "286",
"year": "2011"
},
{
"DOI": "10.1016/j.mce.2017.04.018",
"article-title": "Vitamin D endocrinology on the cross-road between immunity and metabolism",
"author": "Vanherwegen",
"doi-asserted-by": "crossref",
"first-page": "52",
"journal-title": "Mol. Cell Endocrinol.",
"key": "ref_22",
"volume": "453",
"year": "2017"
},
{
"DOI": "10.1016/j.jiph.2020.06.021",
"article-title": "Role of vitamin D in preventing of COVID-19 infection, progression and severity",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "1373",
"journal-title": "J. Infect. Public Health",
"key": "ref_23",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2021.745713",
"article-title": "Is There a Crucial Link Between Vitamin D Status and Inflammatory Response in Patients with COVID-19?",
"author": "Saponaro",
"doi-asserted-by": "crossref",
"first-page": "1664",
"journal-title": "Front. Immunol.",
"key": "ref_24",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1038/s41598-022-21513-9",
"article-title": "Vitamin D status and severity of COVID-19",
"author": "Nielsen",
"doi-asserted-by": "crossref",
"first-page": "19823",
"journal-title": "Sci. Rep.",
"key": "ref_25",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0268038",
"doi-asserted-by": "crossref",
"key": "ref_26",
"unstructured": "Nguyen, N.N., Raju, M.N.P., da Graca, B., Wang, D., Mohamed, N.A., Mutnal, M.B., Rao, A., Bennett, M., Gokingco, M., and Pham, H. (2022). 25-hydroxyvitamin D is a predictor of COVID-19 severity of hospitalized patients. PLoS ONE, 17."
},
{
"article-title": "Association of 25-Hydroxyvitamin D Level with COVID-19-Related in-Hospital Mortality: A Retrospective Cohort Study",
"first-page": "577",
"journal-title": "J. Am. Nutr. Assoc.",
"key": "ref_27",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1186/s12879-021-06168-7",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Davoudi, A., Najafi, N., Aarabi, M., Tayebi, A., Nikaeen, R., Izadyar, H., Salar, Z., Delavarian, L., Vaseghi, N., and Daftarian, Z. (2021). Lack of association between vitamin D insufficiency and clinical outcomes of patients with COVID-19 infection. BMC Infect. Dis., 21."
},
{
"DOI": "10.3389/fpubh.2021.736665",
"article-title": "Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes",
"author": "Chiodini",
"doi-asserted-by": "crossref",
"first-page": "736665",
"journal-title": "Front. Public Health",
"key": "ref_29",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.2147/RMHP.S291584",
"article-title": "Effects of Vitamin D on COVID-19 Infection and Prognosis: A Systematic Review",
"author": "Yisak",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Risk Manag. Healthc. Policy",
"key": "ref_30",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"article-title": "Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis",
"author": "Pereira",
"doi-asserted-by": "crossref",
"first-page": "1308",
"journal-title": "Crit. Rev. Food Sci. Nutr.",
"key": "ref_31",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.3389/fnut.2021.660420",
"article-title": "Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated with Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis",
"author": "Akbar",
"doi-asserted-by": "crossref",
"first-page": "660420",
"journal-title": "Front. Nutr.",
"key": "ref_32",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1002/dmrr.3517",
"article-title": "The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression",
"author": "Tentolouris",
"doi-asserted-by": "crossref",
"first-page": "e3517",
"journal-title": "Diabetes Metab. Res. Rev.",
"key": "ref_33",
"volume": "38",
"year": "2022"
},
{
"DOI": "10.1093/qjmed/hcab009",
"article-title": "Vitamin D supplementation, COVID-19 and disease severity: A meta-analysis",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "175",
"journal-title": "QJM",
"key": "ref_34",
"volume": "114",
"year": "2021"
},
{
"article-title": "Vitamin D supplementation for the treatment of COVID-19: A living systematic review",
"author": "Stroehlein",
"first-page": "CD015043",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref_35",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab405",
"article-title": "Calcifediol Treatment and COVID-19-Related Outcomes",
"author": "Nogues",
"doi-asserted-by": "crossref",
"first-page": "e4017",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_36",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1210/jc.2011-0385",
"article-title": "Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "1911",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_37",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study",
"author": "Castillo",
"doi-asserted-by": "crossref",
"first-page": "105751",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref_38",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1016/j.nut.2021.111441",
"article-title": "A critical update on the role of mild and serious vitamin D deficiency prevalence and the COVID-19 epidemic in Europe",
"author": "Bakaloudi",
"doi-asserted-by": "crossref",
"first-page": "111441",
"journal-title": "Nutrition",
"key": "ref_39",
"volume": "93",
"year": "2022"
},
{
"DOI": "10.3945/ajcn.110.008490",
"article-title": "The relation between acute changes in the systemic inflammatory response and plasma 25-hydroxyvitamin D concentrations after elective knee arthroplasty",
"author": "Reid",
"doi-asserted-by": "crossref",
"first-page": "1006",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_40",
"volume": "93",
"year": "2011"
},
{
"DOI": "10.1016/j.metabol.2020.154434",
"article-title": "Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence",
"author": "Smolders",
"doi-asserted-by": "crossref",
"first-page": "154434",
"journal-title": "Metabolism",
"key": "ref_41",
"volume": "115",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2019.00910",
"article-title": "Vitamin D Binding Protein: A Historic Overview",
"author": "Bouillon",
"doi-asserted-by": "crossref",
"first-page": "910",
"journal-title": "Front. Endocrinol.",
"key": "ref_42",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26832",
"article-title": "Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease",
"author": "Demir",
"doi-asserted-by": "crossref",
"first-page": "2992",
"journal-title": "J. Med. Virol.",
"key": "ref_43",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgz138",
"article-title": "Preventive Role of Vitamin D Supplementation for Acute Phase Reaction after Bisphosphonate Infusion in Paget’s Disease",
"author": "Merlotti",
"doi-asserted-by": "crossref",
"first-page": "dgz138",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_44",
"volume": "105",
"year": "2020"
},
{
"DOI": "10.1138/20110505",
"article-title": "Vitamin D and the immune system: Getting it right",
"author": "Mathieu",
"doi-asserted-by": "crossref",
"first-page": "178",
"journal-title": "IBMS BoneKey",
"key": "ref_45",
"volume": "8",
"year": "2011"
},
{
"DOI": "10.1007/s00281-017-0629-x",
"article-title": "Pathogenic human coronavirus infections: Causes and consequences of cytokine storm and immunopathology",
"author": "Channappanavar",
"doi-asserted-by": "crossref",
"first-page": "529",
"journal-title": "Semin. Immunopathol.",
"key": "ref_46",
"volume": "39",
"year": "2017"
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "crossref",
"key": "ref_47",
"unstructured": "Campi, I., Gennari, L., Merlotti, D., Mingiano, C., Frosali, A., Giovanelli, L., Torlasco, C., Pengo, M.F., Heilbron, F., and Soranna, D. (2021). Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy. BMC Infect. Dis., 21."
},
{
"DOI": "10.3390/nu14132716",
"doi-asserted-by": "crossref",
"key": "ref_48",
"unstructured": "Quesada-Gomez, J.M., Lopez-Miranda, J., Entrenas-Castillo, M., Casado-Díaz, A., Nogues, Y., Solans, X., Mansur, J.L., and Bouillon, R. (2022). Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol. Nutrients, 14."
},
{
"DOI": "10.3390/nu14153048",
"doi-asserted-by": "crossref",
"key": "ref_49",
"unstructured": "De Niet, S., Trémège, M., Coffiner, M., Rousseau, A.F., Calmes, D., Frix, A.N., Gester, F., Delvaux, M., Dive, A.F., and Guglielmi, E. (2022). Positive Effects of Vitamin D Supplementation in Patients Hospitalized for COVID-19: A Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients, 14."
},
{
"DOI": "10.3390/nu14142997",
"doi-asserted-by": "crossref",
"key": "ref_50",
"unstructured": "Wimalawansa, S.J. (2022). Rapidly Increasing Serum 25(OH)D Boosts the Immune System, against Infections-Sepsis and COVID-19. Nutrients, 14."
},
{
"DOI": "10.1016/j.eprac.2021.09.016",
"article-title": "Treatment With 25-Hydroxyvitamin D3 (Calcifediol) Is Associated with a Reduction in the Blood Neutrophil-to-Lymphocyte Ratio Marker of Disease Severity in Hospitalized Patients with COVID-19: A Pilot Multicenter, Randomized, Placebo-Controlled, Double-Blinded Clinical Trial",
"author": "Maghbooli",
"doi-asserted-by": "crossref",
"first-page": "1242",
"journal-title": "Endocr. Pract.",
"key": "ref_51",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.3390/ijms231810532",
"doi-asserted-by": "crossref",
"key": "ref_52",
"unstructured": "Bičíková, M., Máčová, L., and Hill, M. (2022). Vitamin D as a Possible COVID-19 Prevention Strategy. Int. J. Mol. Sci., 23."
}
],
"reference-count": 52,
"references-count": 52,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/15/15/3392"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Vitamin D Deficiency in COVID-19 Patients and Role of Calcifediol Supplementation",
"type": "journal-article",
"volume": "15"
}
