Is Serum 25-Hydroxyvitamin D Level Associated with Severity of COVID-19? A Retrospective Study
et al., Journal of Clinical Medicine, doi:10.3390/jcm12175520, Aug 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
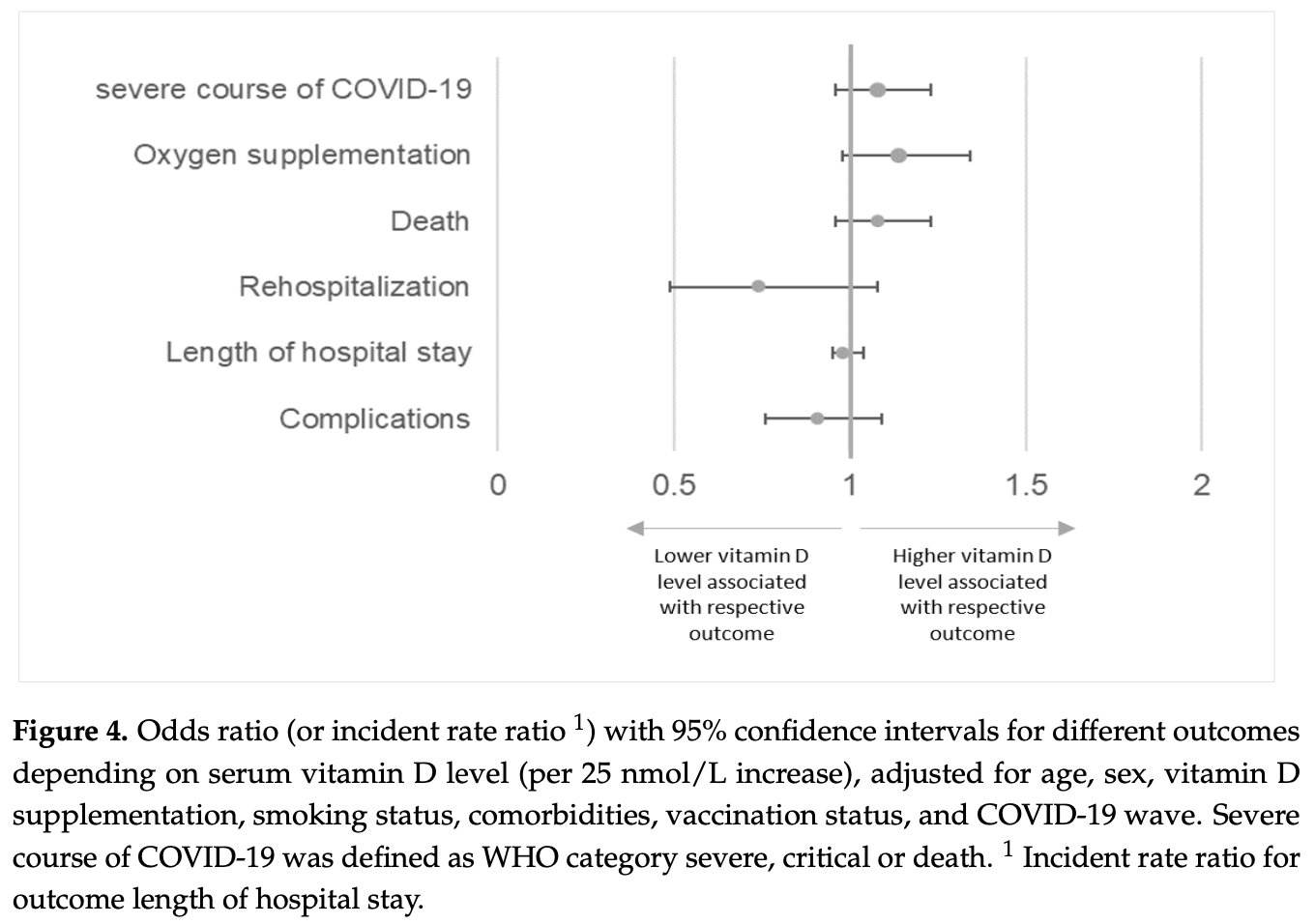
Retrospective 763 hospitalized COVID-19 patients showing no significant difference in outcomes based on serum levels. Unadjusted results show non-significantly lower risk of critical severity, death, and complications with vitamin D sufficiency, while the adjusted results show non-significant increases for critical severity and death. Authors present categorical unadjusted results, while adjusted results are only presented for continuous levels, raising questions. Authors adjust for vitamin D supplementation, which may have attenuated benefits. Vitamin D levels were measured within 30 days before or after hospital admission, confounding results due to the change in levels based on timing with respect to infection. Authors do not provide results for outcomes based on supplementation, which may be of greater interest and would provide additional data on low dose supplementation.
Mbata et al., 25 Aug 2023, retrospective, Switzerland, peer-reviewed, 9 authors, study period January 2020 - December 2021.
Contact: joerg.leuppi@ksbl.ch (corresponding author).
Is Serum 25-Hydroxyvitamin D Level Associated with Severity of COVID-19? A Retrospective Study
Journal of Clinical Medicine, doi:10.3390/jcm12175520
1) Background: SARS-COV2 infection has a clinical spectrum ranging from asymptomatic infection to COVID-19 with acute respiratory distress syndrome (ARDS). Although vitamin D deficiency is often found in patients with ARDS, its role in COVID-19 is not clear. The aim of this study was to explore a possible association between serum 25-hydroxyvitamin D levels and the severity of COVID-19 in hospitalised patients. (2) Methods: In this retrospective observational study, we analysed data from 763 patients hospitalised for COVID-19 in 2020 and 2021. Patients were included in the study if serum 25-hydroxyvitamin D was assessed 30 days before or after hospital admission. Vitamin D deficiency was defined as <50 nmol/L (<20 ng/mL). The primary outcome was COVID-19 severity. (3) Results: The overall median serum 25-hydroxyvitamin D level was 54 nmol/L (IQR 35-76); 47% of the patients were vitamin D deficient. Most patients had mild to moderate COVID-19 and no differences were observed between vitamin D deficient and non-deficient patients (81% vs. 84% of patients, respectively p = 0.829). (4) Conclusion: No association was found between serum 25-hydroxyvitamin D levels and COVID-19 severity in this large observational study conducted over 2 years of the pandemic.
Informed Consent Statement: All patients whose written informed consent was obtained and those whose consent exception was permitted by the ethics committee were included in the study. Patients who had declined general consent for the use of health-related data and samples for research purposes were excluded. Conflicts of Interest: Jörg D. Leuppi has received unrestricted grant money unrelated to the project from AstraZeneca AG Switzerland, Boehringer GmbH Switzerland, GSK AG Switzerland and Merck Sharp & Dohme AG Switzerland. All authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abbas, Robalo Nunes, Martischang, Zingg, Iten et al., Nosocomial transmission and outbreaks of coronavirus disease 2019: The need to protect both patients and healthcare workers, Antimicrob. Resist. Infect. Control, doi:10.1186/s13756-020-00875-7
Alsafar, Grant, Hijazi, Uddin, Alkaabi et al., COVID-19 Disease Severity and Death in Relation to Vitamin D Status among SARS-CoV-2-Positive UAE Residents, doi:10.3390/nu13051714
Amrein, Scherkl, Hoffmann, Neuwersch-Sommeregger, Kostenberger et al., Vitamin D deficiency 2.0: An update on the current status worldwide, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0558-y
Amrein, Schnedl, Holl, Riedl, Christopher et al., Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU randomized clinical trial, doi:10.1001/jama.2014.13204
Andrade, Grandoff, Schneider, Vitamin D Intake and Factors Associated with Self-Reported Vitamin D Deficiency Among US Adults: A 2021 Cross-Sectional Study, Front. Nutr, doi:10.3389/fnut.2022.899300
Angelidi, Belanger, Lorinsky, Karamanis, Chamorro-Pareja et al., Vitamin D Status Is Associated with In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients, Mayo Clin. Proc, doi:10.1016/j.mayocp.2021.01.001
Bahar-Shany, Ravid, Koren, Upregulation of MMP-9 production by TNFalpha in keratinocytes and its attenuation by vitamin D, J. Cell Physiol, doi:10.1002/jcp.22004
Barlow, Beaumont, Cosseau, Mackellar, Wilkinson et al., The human cathelicidin LL-37 preferentially promotes apoptosis of infected airway epithelium, Am. J. Respir. Cell Mol. Biol, doi:10.1165/rcmb.2009-0250OC
Bergman, Lindh, Bjorkhem-Bergman, Lindh, Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, PLoS ONE, doi:10.1371/journal.pone.0065835
Brigham, Hospital, None
Calabrese, Zorzi, Monteleone, Del Vecchio Blanco, Onset of ulcerative colitis during SARS-CoV-2 infection, Dig. Liver Dis, doi:10.1016/j.dld.2020.06.003
Carpagnano, Di Lecce, Quaranta, Zito, Buonamico et al., Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J. Endocrinol. Investig, doi:10.1007/s40618-020-01370-x
Charoenngam, Shirvani, Reddy, Vodopivec, Apovian et al., Association of Vitamin D Status with Hospital Morbidity and Mortality in Adult Hospitalized Patients with COVID-19, Endocr. Pract, doi:10.1016/j.eprac.2021.02.013
Chen, Mei, Xie, Yuan, Ma et al., Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs, Nutr. J, doi:10.1186/s12937-021-00744-y
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study, Lancet
Dancer, Parekh, Lax, Souza, Zheng et al., Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
Dawson-Hughes, Patient Education: Vitamin D Deficiency (Beyond the Basics). Available online
De Smet, De Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D Level on Hospital Admission Associated with COVID-19 Stage and Mortality, Am. J. Clin. Pathol, doi:10.1093/ajcp/aqaa252
De-Madaria, Capurso, COVID-19 and acute pancreatitis: Examining the causality, Nat. Rev. Gastroenterol. Hepatol. 2021, doi:10.1038/s41575-020-00389-y
Diebold, Martinez, Adam, Bassetti, Osthoff et al., Temporal trends of COVID-19 related in-hospital mortality and demographics in Switzerland-A retrospective single centre cohort study, Swiss Med. Wkly, doi:10.4414/smw.2021.20572
Drame, Cofais, Hentzien, Proye, Coulibaly et al., Relation between Vitamin D and COVID-19 in Aged People: A Systematic Review, Nutrients
Gallagher, Jindal, Smith, Vitamin D supplementation in young White and African American women, J. Bone Miner. Res, doi:10.1002/jbmr.2010
Georgoulis, Kontogianni, Kechribari, Tenta, Fragopoulou et al., Associations between serum vitamin D status and the cardiometabolic profile of patients with obstructive sleep apnea, doi:10.1007/s42000-023-00456-4
Gorbalenya, Baker, Baric, De Groot, Drosten et al., Severe acute respiratory syndrome-related coronavirus: The species and its viruses-A statement of the Coronavirus Study Group, doi:10.1101/2020.02.07.937862
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Harris, Taylor, Minor, Elliott, Fernandez et al., The REDCap consortium: Building an international community of software platform partners, J. Biomed. Inform, doi:10.1016/j.jbi.2019.103208
Harris, Taylor, Thielke, Payne, Gonzalez et al., Research electronic data capture (REDCap)-A metadatadriven methodology and workflow process for providing translational research informatics support, J. Biomed. Inform, doi:10.1016/j.jbi.2008.08.010
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Corrigendum to "Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metabol Syndr: Clin Res Rev, doi:10.1016/j.dsx.2020.07.021
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur. J. Nutr
Hernandez, Nan, Fernandez-Ayala, Garcia-Unzueta, Hernandez-Hernandez et al., Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgaa733
Holick, Resurrection of vitamin D deficiency and rickets, J. Clin. Investig, doi:10.1172/JCI29449
Holick, Vitamin D status: Measurement, interpretation, and clinical application, Ann. Epidemiol, doi:10.1016/j.annepidem.2007.12.001
Holick, Vitamin, Deficiency, None, N. Engl. J. Med, doi:10.1056/NEJMra070553
Hribar, Cobbold, Church, Potential Role of Vitamin D in the Elderly to Resist COVID-19 and to Slow Progression of Parkinson's Disease, Brain. Sci, doi:10.3390/brainsci10050284
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.08.018
Jaun, Boesing, Luthi-Corridori, Abig, Makhdoomi et al., High-dose vitamin D substitution in patients with COVID-19: Study protocol for a randomized, double-blind, placebo-controlled, multi-center study-VitCov Trial, Trials, doi:10.1186/s13063-022-06016-2
Karahan, Katkat, Impact of Serum 25(OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey, J. Nutr. Health Aging, doi:10.1007/s12603-020-1479-0
Kazemi, Mohammadi, Aghababaee, Golzarand, Clark et al., Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis, Adv. Nutr. 2021, doi:10.1093/advances/nmab012
Ko, Kim, Lee, Choi, Woo et al., Vitamin D deficiency is associated with disease activity in patients with Crohn's disease, Intest. Res, doi:10.5217/ir.2018.00022
Marshall, Murthy, Diaz, Adhikari, Angus et al., A minimal common outcome measure set for COVID-19 clinical research, doi:10.1016/S1473-3099(20)30483-7
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics with COVID-19 Test Results, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2020.19722
Mendy, Apewokin, Wells, Morrow, Factors Associated with Hospitalization and Disease Severity in a Racially and Ethnically Diverse Population of COVID-19 Patients, doi:10.1101/2020.06.25.20137323
Mineva, Schleicher, Chaudhary-Webb, Maw, Botelho et al., A candidate reference measurement procedure for quantifying serum concentrations of 25-hydroxyvitamin D(3) and 25-hydroxyvitamin D(2) using isotope-dilution liquid chromatography-tandem mass spectrometry, Anal. Bioanal. Chem, doi:10.1007/s00216-015-8733-z
Notz, Herrmann, Schlesinger, Kranke, Sitter et al., Vitamin D deficiency in critically ill COVID-19 ARDS patients, Clin. Nutr, doi:10.1016/j.clnu.2021.03.001
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Raisi-Estabragh, Mccracken, Bethell, Cooper, Cooper et al., Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: Study of 1326 cases from the UK Biobank, J. Public Health, doi:10.1093/pubmed/fdaa095
Reis, Fernandes, Sales, Santos, Dos Santos et al., Influence of vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: A multicenter prospective cohort study, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqab151
Sabico, Enani, Sheshah, Aljohani, Aldisi et al., Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate Covid-19: A Randomized Clinical Trial, Nutrients, doi:10.3390/nu13072170
Syed Mohd, Mishra, Ashraf, Vitamin D and Its Relationship with the Pathways Related to Thrombosis and Various Diseases
Teymoori-Rad, Shokri, Salimi, Marashi, The interplay between vitamin D and viral infections, Rev. Med. Virol, doi:10.1002/rmv.2032
Ulitsky, Ananthakrishnan, Naik, Skaros, Zadvornova et al., Vitamin D deficiency in patients with inflammatory bowel disease: Association with disease activity and quality of life, J. Parenter. Enteral. Nutr
Wu, Liu, Deng, The Role of Vitamin D in Immune System and Inflammatory Bowel Disease, J. Inflamm. Res, doi:10.2147/JIR.S363840
Yang, Chen, Schmidt, Anderson, Wang et al., Ll-37, the Neutrophil Granule-And Epithelial Cell-Derived Cathelicidin, Utilizes Formyl Peptide Receptor-Like 1 (Fprl1) as a Receptor to Chemoattract Human Peripheral Blood Neutrophils, Monocytes, and T Cells, J. Exp. Med, doi:10.1084/jem.192.7.1069
Zhu, Zhang, Wang, Li, Yang et al., A Novel Coronavirus from Patients with Pneumonia in China, N. Engl. J. Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.3390/jcm12175520",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm12175520",
"abstract": "<jats:p>(1) Background: SARS-COV2 infection has a clinical spectrum ranging from asymptomatic infection to COVID-19 with acute respiratory distress syndrome (ARDS). Although vitamin D deficiency is often found in patients with ARDS, its role in COVID-19 is not clear. The aim of this study was to explore a possible association between serum 25-hydroxyvitamin D levels and the severity of COVID-19 in hospitalised patients. (2) Methods: In this retrospective observational study, we analysed data from 763 patients hospitalised for COVID-19 in 2020 and 2021. Patients were included in the study if serum 25-hydroxyvitamin D was assessed 30 days before or after hospital admission. Vitamin D deficiency was defined as <50 nmol/L (<20 ng/mL). The primary outcome was COVID-19 severity. (3) Results: The overall median serum 25-hydroxyvitamin D level was 54 nmol/L (IQR 35–76); 47% of the patients were vitamin D deficient. Most patients had mild to moderate COVID-19 and no differences were observed between vitamin D deficient and non-deficient patients (81% vs. 84% of patients, respectively p = 0.829). (4) Conclusion: No association was found between serum 25-hydroxyvitamin D levels and COVID-19 severity in this large observational study conducted over 2 years of the pandemic.</jats:p>",
"alternative-id": [
"jcm12175520"
],
"author": [
{
"ORCID": "http://orcid.org/0009-0006-8505-6290",
"affiliation": [
{
"name": "Cantonal Hospital Baselland, University Center of Internal Medicine, Rheinstrasse 26, 4410 Liestal, Switzerland"
},
{
"name": "Faculty of Medicine, University of Basel, Klingelbergstrasse 61, 4056 Basel, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Mbata",
"given": "Munachimso Kizito",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Cantonal Hospital Baselland, University Center of Internal Medicine, Rheinstrasse 26, 4410 Liestal, Switzerland"
},
{
"name": "Center for Rehabilitation and Geriatrics, Cantonal Hospital Baselland, Gemeindeholzweg, 4101 Bruderholz, Switzerland"
}
],
"family": "Hunziker",
"given": "Mireille",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Cantonal Hospital Baselland, University Center of Internal Medicine, Rheinstrasse 26, 4410 Liestal, Switzerland"
}
],
"family": "Makhdoomi",
"given": "Anja",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Cantonal Hospital Baselland, University Center of Internal Medicine, Rheinstrasse 26, 4410 Liestal, Switzerland"
},
{
"name": "Faculty of Medicine, University of Basel, Klingelbergstrasse 61, 4056 Basel, Switzerland"
}
],
"family": "Lüthi-Corridori",
"given": "Giorgia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8605-1893",
"affiliation": [
{
"name": "Cantonal Hospital Baselland, University Center of Internal Medicine, Rheinstrasse 26, 4410 Liestal, Switzerland"
},
{
"name": "Faculty of Medicine, University of Basel, Klingelbergstrasse 61, 4056 Basel, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Boesing",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Cantonal Hospital Baselland, University Center of Internal Medicine, Rheinstrasse 26, 4410 Liestal, Switzerland"
}
],
"family": "Giezendanner",
"given": "Stéphanie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Central Laboratories, Cantonal Hospital Baselland, Rheinstrasse 26, 4410 Liestal, Switzerland"
}
],
"family": "Muser",
"given": "Jürgen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine, University of Basel, Klingelbergstrasse 61, 4056 Basel, Switzerland"
},
{
"name": "Hospital Pharmacy, Cantonal Hospital Baselland, Rheinstrasse 26, 4410 Liestal, Switzerland"
},
{
"name": "Department of Patient Safety, Medical Directorate, University Hospital Basel, Schanzenstrasse 55, 4056 Basel, Switzerland"
}
],
"family": "Leuppi-Taegtmeyer",
"given": "Anne B.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5554-0675",
"affiliation": [
{
"name": "Cantonal Hospital Baselland, University Center of Internal Medicine, Rheinstrasse 26, 4410 Liestal, Switzerland"
},
{
"name": "Faculty of Medicine, University of Basel, Klingelbergstrasse 61, 4056 Basel, Switzerland"
}
],
"authenticated-orcid": false,
"family": "Leuppi",
"given": "Jörg D.",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
8,
25
]
],
"date-time": "2023-08-25T12:42:20Z",
"timestamp": 1692967340000
},
"deposited": {
"date-parts": [
[
2023,
8,
25
]
],
"date-time": "2023-08-25T14:03:02Z",
"timestamp": 1692972182000
},
"funder": [
{
"award": [
"160072",
"185592"
],
"name": "Swiss National Science Foundation"
},
{
"award": [
"2018DR108"
],
"name": "Swiss Personalized Health Network"
}
],
"indexed": {
"date-parts": [
[
2023,
8,
26
]
],
"date-time": "2023-08-26T09:14:56Z",
"timestamp": 1693041296580
},
"is-referenced-by-count": 0,
"issue": "17",
"issued": {
"date-parts": [
[
2023,
8,
25
]
]
},
"journal-issue": {
"issue": "17",
"published-online": {
"date-parts": [
[
2023,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
25
]
],
"date-time": "2023-08-25T00:00:00Z",
"timestamp": 1692921600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/12/17/5520/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "5520",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
8,
25
]
]
},
"published-online": {
"date-parts": [
[
2023,
8,
25
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "World Health Organization (2020). Coronavirus Disease 2019 (COVID-19) Situation Report—51, World Health Organization."
},
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A Novel Coronavirus from Patients with Pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"journal-title": "N. Engl. J. Med.",
"key": "ref_2",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1101/2020.02.07.937862",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Gorbalenya, A.E., Baker, S.C., Baric, R.S., de Groot, R.J., Drosten, C., Gulyaeva, A.A., Haagmans, B.L., Lauber, C., Leontovich, A.M., and Neuman, B.W. (2020). Severe acute respiratory syndrome-related coronavirus: The species and its viruses—A statement of the Coronavirus Study Group. bioRxiv."
},
{
"DOI": "10.1016/j.clnu.2021.03.001",
"article-title": "Vitamin D deficiency in critically ill COVID-19 ARDS patients",
"author": "Notz",
"doi-asserted-by": "crossref",
"first-page": "3089",
"journal-title": "Clin. Nutr.",
"key": "ref_4",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"article-title": "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "507",
"journal-title": "Lancet",
"key": "ref_5",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1186/s13756-020-00875-7",
"article-title": "Nosocomial transmission and outbreaks of coronavirus disease 2019: The need to protect both patients and healthcare workers",
"author": "Abbas",
"doi-asserted-by": "crossref",
"first-page": "7",
"journal-title": "Antimicrob. Resist. Infect. Control",
"key": "ref_6",
"volume": "10",
"year": "2021"
},
{
"key": "ref_7",
"unstructured": "John Hopkins University & Medicine (2021, December 16). Mortality Analysis. Available online: https://coronavirus.jhu.edu/data/mortality."
},
{
"DOI": "10.4414/smw.2021.20572",
"article-title": "Temporal trends of COVID-19 related in-hospital mortality and demographics in Switzerland—A retrospective single centre cohort study",
"author": "Diebold",
"doi-asserted-by": "crossref",
"first-page": "w20572",
"journal-title": "Swiss Med. Wkly.",
"key": "ref_8",
"volume": "151",
"year": "2021"
},
{
"key": "ref_9",
"unstructured": "Federal Office of Public Health FOPH (2021, December 17). COVID-19 Switzerland, Information on the Current Situation, as of 4 June 2021. Available online: https://www.covid19.admin.ch/de/epidemiologic/case?demoView=graph."
},
{
"DOI": "10.1172/JCI29449",
"article-title": "Resurrection of vitamin D deficiency and rickets",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "2062",
"journal-title": "J. Clin. Investig.",
"key": "ref_10",
"volume": "116",
"year": "2006"
},
{
"DOI": "10.1056/NEJMra070553",
"article-title": "Vitamin D deficiency",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "266",
"journal-title": "N. Engl. J. Med.",
"key": "ref_11",
"volume": "357",
"year": "2007"
},
{
"DOI": "10.3390/brainsci10050284",
"doi-asserted-by": "crossref",
"key": "ref_12",
"unstructured": "Hribar, C.A., Cobbold, P.H., and Church, F.C. (2020). Potential Role of Vitamin D in the Elderly to Resist COVID-19 and to Slow Progression of Parkinson’s Disease. Brain. Sci., 10."
},
{
"DOI": "10.1002/rmv.2032",
"article-title": "The interplay between vitamin D and viral infections",
"author": "Shokri",
"doi-asserted-by": "crossref",
"first-page": "e2032",
"journal-title": "Rev. Med. Virol.",
"key": "ref_13",
"volume": "29",
"year": "2019"
},
{
"DOI": "10.20944/preprints202003.0235.v2",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Grant, W.B., Lahore, H., McDonnell, S.L., Baggerly, C.A., French, C.B., Aliano, J.L., and Bhattoa, H.P. (2020). Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients, 12."
},
{
"DOI": "10.1186/s12937-021-00744-y",
"article-title": "Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "89",
"journal-title": "Nutr. J.",
"key": "ref_15",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of Vitamin D Status and Other Clinical Characteristics with COVID-19 Test Results",
"author": "Meltzer",
"doi-asserted-by": "crossref",
"first-page": "e2019722",
"journal-title": "JAMA Netw. Open",
"key": "ref_16",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1101/2020.06.25.20137323",
"doi-asserted-by": "crossref",
"key": "ref_17",
"unstructured": "Mendy, A., Apewokin, S., Wells, A.A., and Morrow, A.L. (2020). Factors Associated with Hospitalization and Disease Severity in a Racially and Ethnically Diverse Population of COVID-19 Patients. medRxiv."
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "crossref",
"key": "ref_18",
"unstructured": "Radujkovic, A., Hippchen, T., Tiwari-Heckler, S., Dreher, S., Boxberger, M., and Merle, U. (2020). Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients, 12."
},
{
"DOI": "10.1007/s00394-020-02372-4",
"article-title": "Vitamin D and COVID-19 infection and mortality in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "545",
"journal-title": "Eur. J. Nutr.",
"key": "ref_19",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"article-title": "Vitamin D Status Is Associated with In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients",
"author": "Angelidi",
"doi-asserted-by": "crossref",
"first-page": "875",
"journal-title": "Mayo Clin. Proc.",
"key": "ref_20",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1479-0",
"article-title": "Impact of Serum 25(OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey",
"author": "Karahan",
"doi-asserted-by": "crossref",
"first-page": "189",
"journal-title": "J. Nutr. Health Aging",
"key": "ref_21",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.eprac.2021.02.013",
"article-title": "Association of Vitamin D Status with Hospital Morbidity and Mortality in Adult Hospitalized Patients with COVID-19",
"author": "Charoenngam",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Endocr. Pract.",
"key": "ref_22",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.3390/nu13051714",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "AlSafar, H., Grant, W.B., Hijazi, R., Uddin, M., Alkaabi, N., Tay, G., Mahboub, B., and Al Anouti, F. (2021). COVID-19 Disease Severity and Death in Relation to Vitamin D Status among SARS-CoV-2-Positive UAE Residents. Nutrients, 13."
},
{
"DOI": "10.1007/s40618-020-01370-x",
"article-title": "Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19",
"author": "Carpagnano",
"doi-asserted-by": "crossref",
"first-page": "765",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref_24",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"article-title": "Serum 25(OH)D Level on Hospital Admission Associated with COVID-19 Stage and Mortality",
"author": "Herroelen",
"doi-asserted-by": "crossref",
"first-page": "381",
"journal-title": "Am. J. Clin. Pathol.",
"key": "ref_25",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.07.021",
"article-title": "Corrigendum to “Vitamin D concentrations and COVID-19 infection in UK Biobank” [Diabetes Metabol Syndr: Clin Res Rev 2020 14 (4) 561–5]",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "1315",
"journal-title": "Diabetes Metab. Syndr.",
"key": "ref_26",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1093/pubmed/fdaa095",
"article-title": "Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: Study of 1326 cases from the UK Biobank",
"author": "McCracken",
"doi-asserted-by": "crossref",
"first-page": "451",
"journal-title": "J. Public Health",
"key": "ref_27",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"article-title": "Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS)",
"author": "Dancer",
"doi-asserted-by": "crossref",
"first-page": "617",
"journal-title": "Thorax",
"key": "ref_28",
"volume": "70",
"year": "2015"
},
{
"DOI": "10.1186/s13063-022-06016-2",
"article-title": "High-dose vitamin D substitution in patients with COVID-19: Study protocol for a randomized, double-blind, placebo-controlled, multi-center study-VitCov Trial",
"author": "Jaun",
"doi-asserted-by": "crossref",
"first-page": "114",
"journal-title": "Trials",
"key": "ref_29",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0065835",
"doi-asserted-by": "crossref",
"key": "ref_30",
"unstructured": "Bergman, P., Lindh, A.U., Bjorkhem-Bergman, L., and Lindh, J.D. (2013). Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE, 8."
},
{
"DOI": "10.3390/nu13072170",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Sabico, S., Enani, M.A., Sheshah, E., Aljohani, N.J., Aldisi, D.A., Alotaibi, N.H., Alshingetti, N., Alomar, S.Y., Alnaami, A.M., and Amer, O.E. (2021). Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate Covid-19: A Randomized Clinical Trial. Nutrients, 13."
},
{
"DOI": "10.1001/jama.2014.13204",
"article-title": "Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU randomized clinical trial",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "1520",
"journal-title": "JAMA",
"key": "ref_32",
"volume": "312",
"year": "2014"
},
{
"DOI": "10.1016/S1473-3099(20)30483-7",
"article-title": "A minimal common outcome measure set for COVID-19 clinical research",
"author": "Marshall",
"doi-asserted-by": "crossref",
"first-page": "e192",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_33",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.jbi.2019.103208",
"article-title": "The REDCap consortium: Building an international community of software platform partners",
"author": "Harris",
"doi-asserted-by": "crossref",
"first-page": "103208",
"journal-title": "J. Biomed. Inform.",
"key": "ref_34",
"volume": "95",
"year": "2019"
},
{
"DOI": "10.1016/j.jbi.2008.08.010",
"article-title": "Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support",
"author": "Harris",
"doi-asserted-by": "crossref",
"first-page": "377",
"journal-title": "J. Biomed. Inform.",
"key": "ref_35",
"volume": "42",
"year": "2009"
},
{
"DOI": "10.1007/s00216-015-8733-z",
"article-title": "A candidate reference measurement procedure for quantifying serum concentrations of 25-hydroxyvitamin D(3) and 25-hydroxyvitamin D(2) using isotope-dilution liquid chromatography-tandem mass spectrometry",
"author": "Mineva",
"doi-asserted-by": "crossref",
"first-page": "5615",
"journal-title": "Anal. Bioanal. Chem.",
"key": "ref_36",
"volume": "407",
"year": "2015"
},
{
"DOI": "10.1016/j.annepidem.2007.12.001",
"article-title": "Vitamin D status: Measurement, interpretation, and clinical application",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "73",
"journal-title": "Ann. Epidemiol.",
"key": "ref_37",
"volume": "19",
"year": "2009"
},
{
"key": "ref_38",
"unstructured": "Bess Dawson-Hughes, M. (2023, August 16). Patient Education: Vitamin D Deficiency (Beyond the Basics). Available online: https://www.uptodate.com/contents/vitamin-d-deficiency-beyond-the-basics."
},
{
"key": "ref_39",
"unstructured": "Brigham and Women’s Hospital (2022, June 15). COVID Protocols—Treatments. Available online: https://covidprotocols.org/en/chapters/treatments/."
},
{
"key": "ref_40",
"unstructured": "National Institutes of Health (2022, June 15). COVID-19 Treatment Guidelines—Therapies, Available online: https://www.covid19treatmentguidelines.nih.gov/therapies/."
},
{
"DOI": "10.1210/clinem/dgaa733",
"article-title": "Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection",
"author": "Hernandez",
"doi-asserted-by": "crossref",
"first-page": "e1343",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_41",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"article-title": "Nutritional status of patients with COVID-19",
"author": "Im",
"doi-asserted-by": "crossref",
"first-page": "390",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_42",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1183/23120541.sleepandbreathing-2023.63",
"doi-asserted-by": "crossref",
"key": "ref_43",
"unstructured": "Georgoulis, M., Kontogianni, M.D., Kechribari, I., Tenta, R., Fragopoulou, E., Lamprou, K., Perraki, E., Vagiakis, E., and Yiannakouris, N. (2023). Associations between serum vitamin D status and the cardiometabolic profile of patients with obstructive sleep apnea. Hormones."
},
{
"DOI": "10.3390/nu13041339",
"doi-asserted-by": "crossref",
"key": "ref_44",
"unstructured": "Drame, M., Cofais, C., Hentzien, M., Proye, E., Coulibaly, P.S., Demoustier-Tampere, D., Destailleur, M.H., Lotin, M., Cantagrit, E., and Cebille, A. (2021). Relation between Vitamin D and COVID-19 in Aged People: A Systematic Review. Nutrients, 13."
},
{
"DOI": "10.1093/advances/nmab012",
"article-title": "Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis",
"author": "Kazemi",
"doi-asserted-by": "crossref",
"first-page": "1636",
"journal-title": "Adv. Nutr.",
"key": "ref_45",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1093/ajcn/nqab151",
"article-title": "Influence of vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: A multicenter prospective cohort study",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "598",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_46",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1038/s41430-020-0558-y",
"article-title": "Vitamin D deficiency 2.0: An update on the current status worldwide",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "1498",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "ref_47",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.3389/fnut.2022.899300",
"article-title": "Vitamin D Intake and Factors Associated with Self-Reported Vitamin D Deficiency Among US Adults: A 2021 Cross-Sectional Study",
"author": "Andrade",
"doi-asserted-by": "crossref",
"first-page": "899300",
"journal-title": "Front. Nutr.",
"key": "ref_48",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1002/jbmr.2010",
"article-title": "Vitamin D supplementation in young White and African American women",
"author": "Gallagher",
"doi-asserted-by": "crossref",
"first-page": "173",
"journal-title": "J. Bone Miner. Res.",
"key": "ref_49",
"volume": "29",
"year": "2014"
},
{
"article-title": "Upregulation of MMP-9 production by TNFalpha in keratinocytes and its attenuation by vitamin D",
"author": "Ravid",
"first-page": "729",
"journal-title": "J. Cell Physiol.",
"key": "ref_50",
"volume": "222",
"year": "2010"
},
{
"DOI": "10.1165/rcmb.2009-0250OC",
"article-title": "The human cathelicidin LL-37 preferentially promotes apoptosis of infected airway epithelium",
"author": "Barlow",
"doi-asserted-by": "crossref",
"first-page": "692",
"journal-title": "Am. J. Respir. Cell Mol. Biol.",
"key": "ref_51",
"volume": "43",
"year": "2010"
},
{
"DOI": "10.1084/jem.192.7.1069",
"article-title": "Ll-37, the Neutrophil Granule–And Epithelial Cell–Derived Cathelicidin, Utilizes Formyl Peptide Receptor–Like 1 (Fprl1) as a Receptor to Chemoattract Human Peripheral Blood Neutrophils, Monocytes, and T Cells",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "1069",
"journal-title": "J. Exp. Med.",
"key": "ref_52",
"volume": "192",
"year": "2000"
},
{
"key": "ref_53",
"unstructured": "Syed Mohd, S.S., Mishra, A., and Ashraf, M.Z. (2021). Vitamin D, IntechOpen."
},
{
"DOI": "10.2147/JIR.S363840",
"article-title": "The Role of Vitamin D in Immune System and Inflammatory Bowel Disease",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "3167",
"journal-title": "J. Inflamm. Res.",
"key": "ref_54",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.5217/ir.2018.00022",
"article-title": "Vitamin D deficiency is associated with disease activity in patients with Crohn’s disease",
"author": "Ko",
"doi-asserted-by": "crossref",
"first-page": "70",
"journal-title": "Intest. Res.",
"key": "ref_55",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1177/0148607110381267",
"article-title": "Vitamin D deficiency in patients with inflammatory bowel disease: Association with disease activity and quality of life",
"author": "Ulitsky",
"doi-asserted-by": "crossref",
"first-page": "308",
"journal-title": "J. Parenter. Enteral. Nutr.",
"key": "ref_56",
"volume": "35",
"year": "2011"
},
{
"DOI": "10.1016/j.dld.2020.06.003",
"article-title": "Onset of ulcerative colitis during SARS-CoV-2 infection",
"author": "Calabrese",
"doi-asserted-by": "crossref",
"first-page": "1228",
"journal-title": "Dig. Liver Dis.",
"key": "ref_57",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1038/s41575-020-00389-y",
"article-title": "COVID-19 and acute pancreatitis: Examining the causality",
"author": "Capurso",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Nat. Rev. Gastroenterol. Hepatol.",
"key": "ref_58",
"volume": "18",
"year": "2021"
}
],
"reference-count": 58,
"references-count": 58,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/12/17/5520"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Is Serum 25-Hydroxyvitamin D Level Associated with Severity of COVID-19? A Retrospective Study",
"type": "journal-article",
"volume": "12"
}
