Vitamin D deficiency in critically ill COVID-19 ARDS patients
et al., Clinical Nutrition, doi:10.1016/j.clnu.2021.03.001, Mar 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
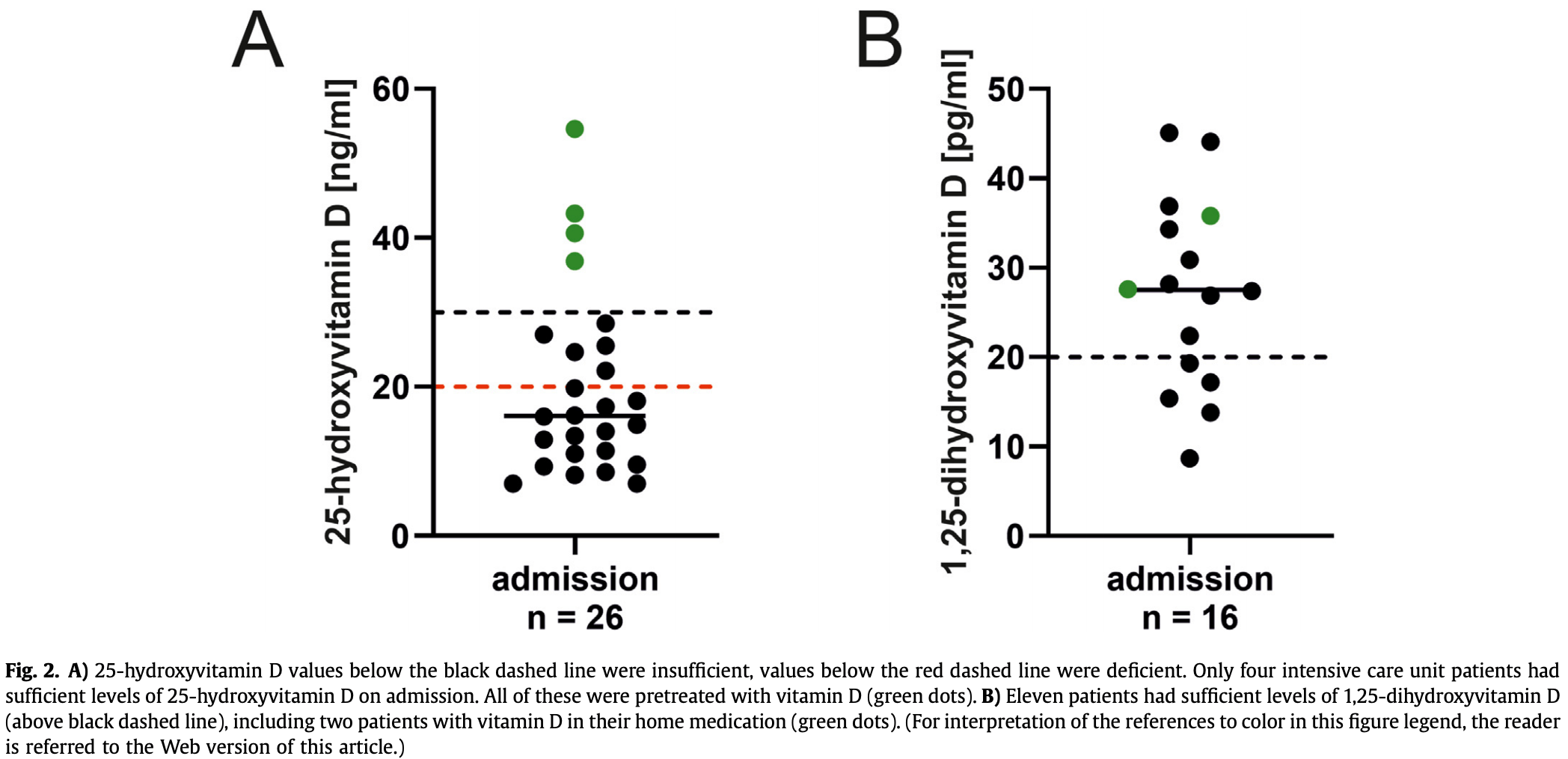
Retrospective 26 ICU patients showing that the majority of patients had vitamin D deficiency. There was no statistically significant association of 25-hydroxyvitamin D status and clinical course, however low levels of 1,25-dihydroxyvitamin D were associated with prolonged mechanical ventilation and a worse APACHE II score. Clinical outcomes based on baseline vitamin D status are not provided.
Notz et al., 7 Mar 2021, peer-reviewed, 12 authors.
Vitamin D deficiency in critically ill COVID-19 ARDS patients
Clinical Nutrition, doi:10.1016/j.clnu.2021.03.001
Background & aims: Vitamin D's pleiotropic effects include immune modulation, and its supplementation has been shown to prevent respiratory tract infections. The effectivity of vitamin D as a therapeutic intervention in critical illness remains less defined. The current study analyzed clinical and immunologic effects of vitamin D levels in patients suffering from coronavirus disease 2019 (COVID-19) induced acute respiratory distress syndrome (ARDS). Methods: This was a single-center retrospective study in patients receiving intensive care with a confirmed SARS-CoV-2 infection and COVID-19 ARDS. 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D serum levels, pro-and anti-inflammatory cytokines and immune cell subsets were measured on admission as well as after 10e15 days. Clinical parameters were extracted from the patient data management system. Standard operating procedures included the daily administration of vitamin D 3 via enteral feeding. Results: A total of 39 patients with COVID-19 ARDS were eligible, of which 26 were included in this study as data on vitamin D status was available. 96% suffered from severe COVID-19 ARDS. All patients without prior vitamin D supplementation (n ¼ 22) had deficient serum levels of 25-hydroxyvitamin D. Vitamin D supplementation resulted in higher serum levels of 25-hydroxyvitamin D but not did not increase 1,25dihydroxyvitamin D levels after 10e15 days. Clinical parameters did not differ between patients with sufficient or deficient levels of 25-hydroxyvitamin D. Only circulating plasmablasts were higher in patients with 25-hydroxyvitamin D levels !30 ng/ml (p ¼ 0.029). Patients with 1,25-dihydroxyvitamin D levels below 20 pg/ml required longer mechanical ventilation (p ¼ 0.045) and had a worse acute physiology and chronic health evaluation (APACHE) II score (p ¼ 0.048).
Conclusion: The vast majority of COVID-19 ARDS patients had vitamin D deficiency. 25-hydroxyvitamin D status was not related to changes in clinical course, whereas low levels of 1,25-dihydroxyvitamin D were associated with prolonged mechanical ventilation and a worse APACHE II score.
Author contributions QN, PK, CL, and PM contributed substantially to the conception and design of the study, the acquisition, analysis, interpretation of the data and drafted the article. CS contributed substantially to the conception and design of the study, interpretation of the data and revised the manuscript. JH, TS, MS, PH contributed substantially to the acquisition of the data. JS, DR, KA contributed substantially to the interpretation of the data and critical revision of the article. All authors provided final approval of the version submitted for publication.
Conflict of interest None.
References
Amrein, Schnedl, Holl, Riedl, Christopher et al., Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial, Jama
Amrein, Zajic, Schnedl, Waltensdorfer, Fruhwald et al., Vitamin D status and its association with season, hospital and sepsis mortality in critical illness, Crit Care
Anderson, Do, Toh, Hoe, Reitsma et al., Vitamin D induces differential effects on inflammatory responses during bacterial and/or viral stimulation of human peripheral blood mononuclear cells, Front Immunol
Belderbos, Houben, Wilbrink, Lentjes, Bloemen et al., Cord blood vitamin D deficiency is associated with respiratory syncytial virus bronchiolitis, Pediatrics
Berry, Hesketh, Power, Hypp€ Onen E, Vitamin D status has a linear association with seasonal infections and lung function in British adults, Br J Nutr
Corman, Landt, Kaiser, Molenkamp, Meijer et al., Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR, Euro Surveill
Enez-Sousa, Martínez, Medrano, Andez-Rodríguez, Resino, Vitamin D in human immunodeficiency virus infection: influence on immunity and disease, Front Immunol
Fig, None
Fink, Origin and function of circulating plasmablasts during acute viral infections, Front Immunol
Fitch, Becker, Hayglass, Vitamin D [1,25(OH)2D3] differentially regulates human innate cytokine responses to bacterial versus viral pattern recognition receptor stimuli, J Immunol
Ginde, Brower, Caterino, Finck, Banner-Goodspeed et al., Early high-dose vitamin D(3) for critically ill, vitamin Ddeficient patients, N Engl J Med
Ho, Celis-Morales, Gray, Katikireddi, Niedzwiedz et al., Modifiable and non-modifiable risk factors for COVID-19, and comparison to risk factors for influenza and pneumonia: results from a UK Biobank prospective cohort study, BMJ Open
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metabol
Holick, Vitamin D deficiency, N Engl J Med
Khammissa, Fourie, Motswaledi, Ballyram, Lemmer et al., The biological activities of vitamin D and its receptor in relation to calcium and bone homeostasis, cancer, immune and cardiovascular systems, skin biology, and oral health, BioMed Res Int
Kolls, Ray, Wenzel, High-dose vitamin D3 for critically ill vitamin Ddeficient patients, N Engl J Med
Langlois, Szwec, 'aragon, Heyland, Manzanares, Vitamin D supplementation in the critically ill: a systematic review and meta-analysis, Clin Nutr
Leaf, Raed, Donnino, Ginde, Waikar, Randomized controlled trial of calcitriol in severe sepsis, Am J Respir Crit Care Med
Maloney, Almarines, Goolkasian, Vitamin D levels and monospot tests in military personnel with acute pharyngitis: a retrospective chart review, PloS One
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ
Martucci, Mcnally, Parekh, Zajic, Tuzzolino et al., Trying to identify who may benefit most from future vitamin D intervention trials: a post hoc analysis from the VITDAL-ICU study excluding the early deaths, Crit Care
Mcnally, Nama, 'hearn, Sampson, Amrein et al., Vitamin D deficiency in critically ill children: a systematic review and meta-analysis, Crit Care
Morbach, Eichhorn, Liese, Girschick, Reference values for B cell subpopulations from infancy to adulthood, Clin Exp Immunol
Ney, Heyland, Amrein, Marx, Grottke et al., The relevance of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentration for postoperative infections and postoperative organ dysfunctions in cardiac surgery patients: the eVIDenCe study, Clin Nutr
Palacios, Gonzalez, Is vitamin D deficiency a major global public health problem?, J Steroid Biochem Mol Biol
Raisi-Estabragh, Mccracken, Bethell, Cooper, Cooper et al., Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank, J Public Health (Oxf)
Ranieri, Rubenfeld, Thompson, Ferguson, Acute respiratory distress syndrome: the Berlin Definition, Jama
Sundaram, Coleman, Vitamin D and influenza, Adv Nutr
Tang, Jackson, Walsh, Greeves, Fraser, The dynamic relationships between the active and catabolic vitamin D metabolites, their ratios, and associations with PTH, Sci Rep
Telcian, Zdrenghea, Edwards, Laza-Stanca, Mallia et al., Vitamin D increases the antiviral activity of bronchial epithelial cells in vitro, Antivir Res
Vandenbroucke, Elm, Altman, Gøtzsche, Mulrow et al., Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration, Ann Intern Med
Warnatz, Schlesier, Flow cytometric phenotyping of common variable immunodeficiency, Cytometry B Clin Cytometry
Zaidan, Wang, High-dose vitamin D3 for critically ill vitamin D-deficient patients, N Engl J Med
DOI record:
{
"DOI": "10.1016/j.clnu.2021.03.001",
"ISSN": [
"0261-5614"
],
"URL": "http://dx.doi.org/10.1016/j.clnu.2021.03.001",
"alternative-id": [
"S0261561421001357"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Vitamin D deficiency in critically ill COVID-19 ARDS patients"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Clinical Nutrition"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.clnu.2021.03.001"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Elsevier Ltd and European Society for Clinical Nutrition and Metabolism. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4042-4436",
"affiliation": [],
"authenticated-orcid": false,
"family": "Notz",
"given": "Quirin",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-2169-3761",
"affiliation": [],
"authenticated-orcid": false,
"family": "Herrmann",
"given": "Johannes",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Schlesinger",
"given": "Tobias",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5324-981X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kranke",
"given": "Peter",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1719-3158",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sitter",
"given": "Magdalena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Helmer",
"given": "Philipp",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1372-7623",
"affiliation": [],
"authenticated-orcid": false,
"family": "Stumpner",
"given": "Jan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6805-9330",
"affiliation": [],
"authenticated-orcid": false,
"family": "Roeder",
"given": "Daniel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Amrein",
"given": "Karin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stoppe",
"given": "Christian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2574-624X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lotz",
"given": "Christopher",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2666-8696",
"affiliation": [],
"authenticated-orcid": false,
"family": "Meybohm",
"given": "Patrick",
"sequence": "additional"
}
],
"container-title": "Clinical Nutrition",
"container-title-short": "Clinical Nutrition",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"clinicalnutritionjournal.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
8
]
],
"date-time": "2021-03-08T02:59:47Z",
"timestamp": 1615172387000
},
"deposited": {
"date-parts": [
[
2024,
2,
13
]
],
"date-time": "2024-02-13T13:36:21Z",
"timestamp": 1707831381000
},
"indexed": {
"date-parts": [
[
2024,
4,
2
]
],
"date-time": "2024-04-02T15:05:49Z",
"timestamp": 1712070349163
},
"is-referenced-by-count": 19,
"issue": "12",
"issued": {
"date-parts": [
[
2022,
12
]
]
},
"journal-issue": {
"issue": "12",
"published-print": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
12,
1
]
],
"date-time": "2022-12-01T00:00:00Z",
"timestamp": 1669852800000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0261561421001357?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0261561421001357?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "3089-3095",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
12
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"article-title": "Is vitamin D deficiency a major global public health problem?",
"author": "Palacios",
"doi-asserted-by": "crossref",
"first-page": "138",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "10.1016/j.clnu.2021.03.001_bib1",
"volume": "144 Pt A",
"year": "2014"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "i6583",
"journal-title": "BMJ",
"key": "10.1016/j.clnu.2021.03.001_bib2",
"volume": "356",
"year": "2017"
},
{
"article-title": "Vitamin D [1,25(OH)2D3] differentially regulates human innate cytokine responses to bacterial versus viral pattern recognition receptor stimuli",
"author": "Fitch",
"first-page": "2965",
"issue": "7",
"journal-title": "J Immunol (Baltimore, Md : 1950)",
"key": "10.1016/j.clnu.2021.03.001_bib3",
"volume": "196",
"year": "2016"
},
{
"DOI": "10.3389/fimmu.2020.00602",
"article-title": "Vitamin D induces differential effects on inflammatory responses during bacterial and/or viral stimulation of human peripheral blood mononuclear cells",
"author": "Anderson",
"doi-asserted-by": "crossref",
"first-page": "602",
"journal-title": "Front Immunol",
"key": "10.1016/j.clnu.2021.03.001_bib4",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1017/S0007114511001991",
"article-title": "Vitamin D status has a linear association with seasonal infections and lung function in British adults",
"author": "Berry",
"doi-asserted-by": "crossref",
"first-page": "1433",
"issue": "9",
"journal-title": "Br J Nutr",
"key": "10.1016/j.clnu.2021.03.001_bib5",
"volume": "106",
"year": "2011"
},
{
"DOI": "10.1186/s13054-017-1875-y",
"article-title": "Vitamin D deficiency in critically ill children: a systematic review and meta-analysis",
"author": "McNally",
"doi-asserted-by": "crossref",
"first-page": "287",
"issue": "1",
"journal-title": "Crit Care (London, England)",
"key": "10.1016/j.clnu.2021.03.001_bib6",
"volume": "21",
"year": "2017"
},
{
"DOI": "10.1016/j.clnu.2017.05.006",
"article-title": "Vitamin D supplementation in the critically ill: a systematic review and meta-analysis",
"author": "Langlois",
"doi-asserted-by": "crossref",
"first-page": "1238",
"issue": "4",
"journal-title": "Clin Nutr (Edinburgh, Scotland)",
"key": "10.1016/j.clnu.2021.03.001_bib7",
"volume": "37",
"year": "2018"
},
{
"DOI": "10.7326/0003-4819-147-8-200710160-00010-w1",
"article-title": "Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration",
"author": "Vandenbroucke",
"doi-asserted-by": "crossref",
"first-page": "W163",
"issue": "8",
"journal-title": "Ann Intern Med",
"key": "10.1016/j.clnu.2021.03.001_bib8",
"volume": "147",
"year": "2007"
},
{
"DOI": "10.2807/1560-7917.ES.2020.25.3.2000045",
"article-title": "Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR",
"author": "Corman",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "Euro Surveill",
"key": "10.1016/j.clnu.2021.03.001_bib9",
"volume": "25",
"year": "2020"
},
{
"article-title": "Acute respiratory distress syndrome: the Berlin Definition",
"author": "Ranieri",
"first-page": "2526",
"issue": "23",
"journal-title": "Jama",
"key": "10.1016/j.clnu.2021.03.001_bib10",
"volume": "307",
"year": "2012"
},
{
"DOI": "10.1056/NEJMra070553",
"article-title": "Vitamin D deficiency",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "266",
"issue": "3",
"journal-title": "N Engl J Med",
"key": "10.1016/j.clnu.2021.03.001_bib11",
"volume": "357",
"year": "2007"
},
{
"DOI": "10.1002/cyto.b.20432",
"article-title": "Flow cytometric phenotyping of common variable immunodeficiency",
"author": "Warnatz",
"doi-asserted-by": "crossref",
"first-page": "261",
"issue": "5",
"journal-title": "Cytometry B Clin Cytometry",
"key": "10.1016/j.clnu.2021.03.001_bib12",
"volume": "74",
"year": "2008"
},
{
"DOI": "10.1111/j.1365-2249.2010.04206.x",
"article-title": "Reference values for B cell subpopulations from infancy to adulthood",
"author": "Morbach",
"doi-asserted-by": "crossref",
"first-page": "271",
"issue": "2",
"journal-title": "Clin Exp Immunol",
"key": "10.1016/j.clnu.2021.03.001_bib13",
"volume": "162",
"year": "2010"
},
{
"DOI": "10.1371/journal.pone.0101180",
"article-title": "Vitamin D levels and monospot tests in military personnel with acute pharyngitis: a retrospective chart review",
"author": "Maloney",
"doi-asserted-by": "crossref",
"issue": "7",
"journal-title": "PloS One",
"key": "10.1016/j.clnu.2021.03.001_bib14",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.3389/fimmu.2018.00458",
"article-title": "Vitamin D in human immunodeficiency virus infection: influence on immunity and disease",
"author": "Jiménez-Sousa",
"doi-asserted-by": "crossref",
"first-page": "458",
"journal-title": "Front Immunol",
"key": "10.1016/j.clnu.2021.03.001_bib15",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1542/peds.2010-3054",
"article-title": "Cord blood vitamin D deficiency is associated with respiratory syncytial virus bronchiolitis",
"author": "Belderbos",
"doi-asserted-by": "crossref",
"first-page": "e1513",
"issue": "6",
"journal-title": "Pediatrics",
"key": "10.1016/j.clnu.2021.03.001_bib16",
"volume": "127",
"year": "2011"
},
{
"DOI": "10.3945/an.112.002162",
"article-title": "Vitamin D and influenza",
"author": "Sundaram",
"doi-asserted-by": "crossref",
"first-page": "517",
"issue": "4",
"journal-title": "Adv Nutr (Bethesda, Md)",
"key": "10.1016/j.clnu.2021.03.001_bib17",
"volume": "3",
"year": "2012"
},
{
"DOI": "10.1136/bmjopen-2020-040402",
"article-title": "Modifiable and non-modifiable risk factors for COVID-19, and comparison to risk factors for influenza and pneumonia: results from a UK Biobank prospective cohort study",
"author": "Ho",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "BMJ Open",
"key": "10.1016/j.clnu.2021.03.001_bib18",
"volume": "10",
"year": "2020"
},
{
"article-title": "Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank",
"author": "Raisi-Estabragh",
"first-page": "451",
"issue": "3",
"journal-title": "J Public Health (Oxf)",
"key": "10.1016/j.clnu.2021.03.001_bib19",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1038/s41598-019-43462-6",
"article-title": "The dynamic relationships between the active and catabolic vitamin D metabolites, their ratios, and associations with PTH",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "6974",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10.1016/j.clnu.2021.03.001_bib20",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1210/jc.2011-0385",
"article-title": "Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "1911",
"issue": "7",
"journal-title": "J Clin Endocrinol Metabol",
"key": "10.1016/j.clnu.2021.03.001_bib21",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.1155/2018/9276380",
"article-title": "The biological activities of vitamin D and its receptor in relation to calcium and bone homeostasis, cancer, immune and cardiovascular systems, skin biology, and oral health",
"author": "Khammissa",
"doi-asserted-by": "crossref",
"first-page": "9276380",
"journal-title": "BioMed Res Int",
"key": "10.1016/j.clnu.2021.03.001_bib22",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.1016/j.antiviral.2016.11.004",
"article-title": "Vitamin D increases the antiviral activity of bronchial epithelial cells in vitro",
"author": "Telcian",
"doi-asserted-by": "crossref",
"first-page": "93",
"journal-title": "Antivir Res",
"key": "10.1016/j.clnu.2021.03.001_bib23",
"volume": "137",
"year": "2017"
},
{
"DOI": "10.1164/rccm.201405-0988OC",
"article-title": "Randomized controlled trial of calcitriol in severe sepsis",
"author": "Leaf",
"doi-asserted-by": "crossref",
"first-page": "533",
"issue": "5",
"journal-title": "Am J Respir Crit Care Med",
"key": "10.1016/j.clnu.2021.03.001_bib24",
"volume": "190",
"year": "2014"
},
{
"DOI": "10.1016/j.clnu.2018.11.033",
"article-title": "The relevance of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentration for postoperative infections and postoperative organ dysfunctions in cardiac surgery patients: the eVIDenCe study",
"author": "Ney",
"doi-asserted-by": "crossref",
"first-page": "2756",
"issue": "6",
"journal-title": "Clin Nutr (Edinburgh, Scotland)",
"key": "10.1016/j.clnu.2021.03.001_bib25",
"volume": "38",
"year": "2019"
},
{
"DOI": "10.3389/fimmu.2012.00078",
"article-title": "Origin and function of circulating plasmablasts during acute viral infections",
"author": "Fink",
"doi-asserted-by": "crossref",
"first-page": "78",
"journal-title": "Front Immunol",
"key": "10.1016/j.clnu.2021.03.001_bib26",
"volume": "3",
"year": "2012"
},
{
"DOI": "10.1056/NEJMc2000993",
"article-title": "High-dose vitamin D3 for critically ill vitamin D-deficient patients",
"author": "Zaidan",
"doi-asserted-by": "crossref",
"first-page": "1669",
"issue": "17",
"journal-title": "N Engl J Med",
"key": "10.1016/j.clnu.2021.03.001_bib27",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1186/cc13790",
"article-title": "Vitamin D status and its association with season, hospital and sepsis mortality in critical illness",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "R47",
"issue": "2",
"journal-title": "Crit Care (London, England)",
"key": "10.1016/j.clnu.2021.03.001_bib28",
"volume": "18",
"year": "2014"
},
{
"DOI": "10.1001/jama.2014.13204",
"article-title": "Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "1520",
"issue": "15",
"journal-title": "Jama",
"key": "10.1016/j.clnu.2021.03.001_bib29",
"volume": "312",
"year": "2014"
},
{
"DOI": "10.1056/NEJMoa1911124",
"article-title": "Early high-dose vitamin D(3) for critically ill, vitamin D-deficient patients",
"author": "Ginde",
"doi-asserted-by": "crossref",
"first-page": "2529",
"issue": "26",
"journal-title": "N Engl J Med",
"key": "10.1016/j.clnu.2021.03.001_bib30",
"volume": "381",
"year": "2019"
},
{
"DOI": "10.1186/s13054-019-2472-z",
"article-title": "Trying to identify who may benefit most from future vitamin D intervention trials: a post hoc analysis from the VITDAL-ICU study excluding the early deaths",
"author": "Martucci",
"doi-asserted-by": "crossref",
"first-page": "200",
"issue": "1",
"journal-title": "Crit Care (London, England)",
"key": "10.1016/j.clnu.2021.03.001_bib31",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1056/NEJMc2000993",
"article-title": "High-dose vitamin D3 for critically ill vitamin D-deficient patients",
"author": "Kolls",
"doi-asserted-by": "crossref",
"first-page": "1669",
"issue": "17",
"journal-title": "N Engl J Med",
"key": "10.1016/j.clnu.2021.03.001_bib32",
"volume": "382",
"year": "2020"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0261561421001357"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Vitamin D deficiency in critically ill COVID-19 ARDS patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "41"
}
