Does aspirin have an effect on risk of death in patients with COVID-19? A meta-analysis
et al., European Journal of Clinical Pharmacology, doi:10.1007/s00228-022-03356-5, PROSPERO CRD42021241027, Jun 2022
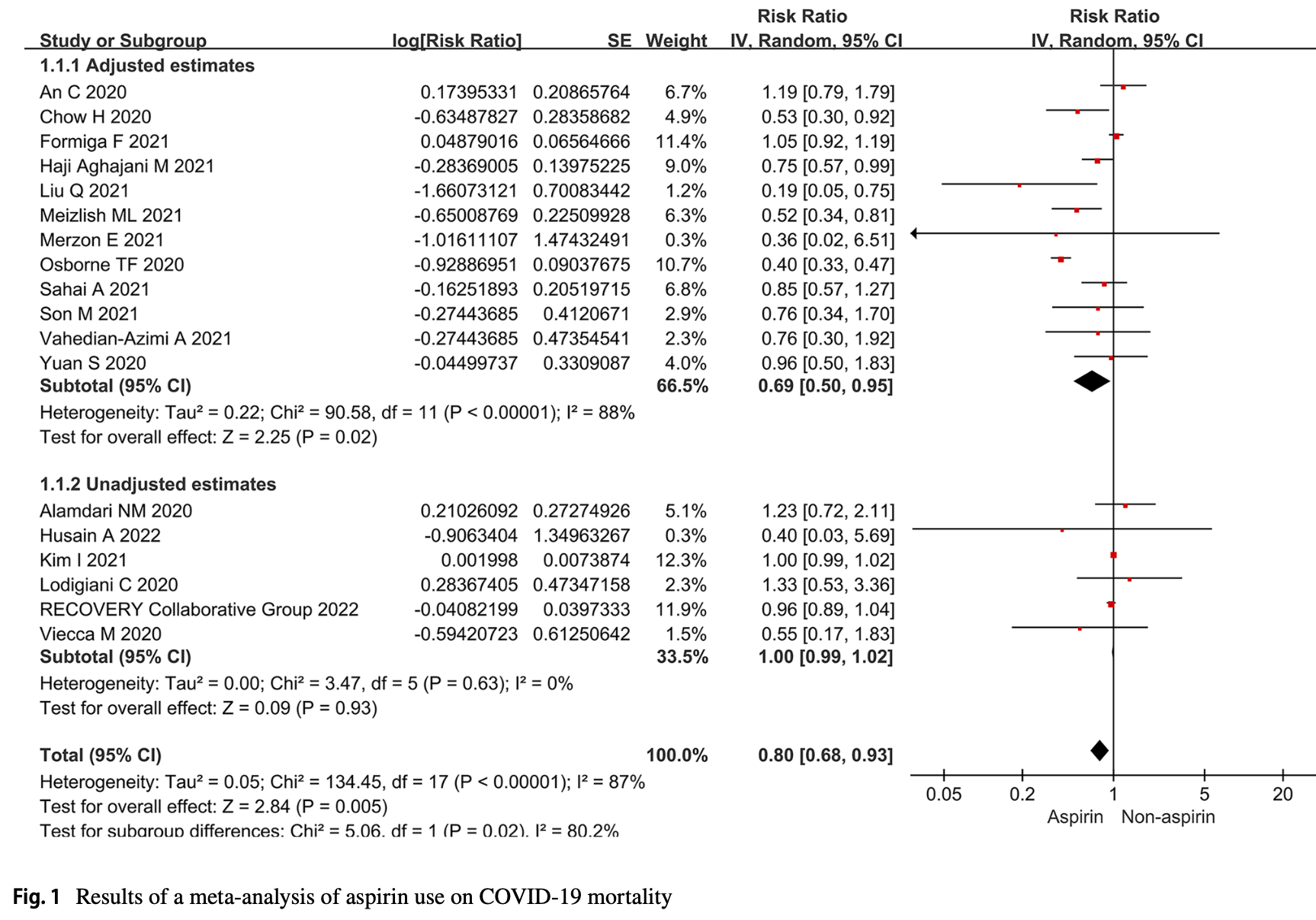
Meta-analysis of 18 studies with 49,041 COVID-19 patients showing significantly lower mortality with aspirin treatment.
4 meta-analyses show significant improvements with aspirin for mortality1-3,
mechanical ventilation1, and
progression4.
Currently there are 79 aspirin for COVID-19 studies, showing 8% lower mortality [2‑14%], 5% lower ventilation [-5‑15%], 3% lower ICU admission [-11‑16%], 1% higher hospitalization [-4‑6%], and 5% fewer cases [-5‑14%].
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments5.
|
risk of death, 20.0% lower, RR 0.80, p = 0.005.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Banaser et al., A systematic review and meta-analysis on efficacy of low dose aspirin on the management of COVID-19, International Journal of Medicine in Developing Countries, doi:10.24911/IJMDC.51-1640383699.
2.
Srinivasan et al., Aspirin use is associated with decreased inpatient mortality in patients with COVID-19: A meta-analysis, American Heart Journal Plus: Cardiology Research and Practice, doi:10.1016/j.ahjo.2022.100191.
3.
Baral et al., All-cause and In-hospital Mortality after Aspirin Use in Patients Hospitalized with COVID-19: A Systematic Review and Meta-analysis, Biology Methods and Protocols, doi:10.1093/biomethods/bpac027.
Ma et al., 22 Jun 2022, China, peer-reviewed, 13 authors, trial PROSPERO CRD42021241027.
Contact: yhsun_ahmu_edu@yeah.net.
Does aspirin have an effect on risk of death in patients with COVID-19? A meta-analysis
European Journal of Clinical Pharmacology, doi:10.1007/s00228-022-03356-5
Purpose The coronavirus disease 2019 (COVID-19) pandemic has shown unprecedented impact world-wide since the eruption in late 2019. Importantly, emerging reports suggest an increased risk of thromboembolism development in patients with COVID-19. Meanwhile, it is found that aspirin reduced mortality in critically ill patients with non-COVID-19 acute respiratory distress syndrome. Therefore, a meta-analysis was performed to investigate the effects of aspirin on COVID-19 mortality. Methods A systematic literature search was conducted in 10 electronic databases and 4 registries. Random effects models were used to calculate pooled relative risks (RRs) with 95% confidence intervals (Cis) to estimate the effect of aspirin on COVID-19 mortality. Relevant subgroup analyses and sensitivity analyses were also performed.
Results The results showed that aspirin use was associated with a reduction in COVID-19 mortality (adjusted RR 0.69; 95% CI 0.50-0.95; P < 0.001). Subgroup analysis found that the low-dose group was associated with a reduced COVID-19 mortality (adjusted RR 0.64; 95% CI 0.48-0.85; P < 0.01). Aspirin use was associated with reduced COVID-19 mortality in Europe and America (crude RR 0.71; 95% CI 0.52-0.98; P = 0.04), and results from cohort studies suggested that aspirin use was a protective factor for COVID-19 mortality (adjusted RR 0.73; 95% CI 0.52-0.99; P = 0.04). Meanwhile, aspirin use was not associated with bleeding risk (crude RR 1.22; 95% CI 0.80-1.87; P = 0.96). Conclusions This meta-analysis found that aspirin use was associated with a reduction in mortality in patients with COVID-19 and not with an increased risk of bleeding.
Supplementary information The online version contains supplementary material available at https:// doi. org/ 10. 1007/ s00228-022-03356-5.
Author contribution
Declarations Ethics approval and consent to participate This article does not contain any studies with human participants or animals performed by any of the authors. We did not use individual data but published data. These data have been widely utilized in research and are generally available. Therefore, we confirm that any aspect of the work covered in this manuscript has been conducted with ethical approval. And this study has been registered (registration number: CRD42021241027) with the PROSPERO (International Prospective Register of Systematic Reviews) and was conducted according to the Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA) statement. Consent for publication All individuals gave written informed consent for publication. The authors are responsible for the reported research, and have participated in the concept and design, analysis and interpretation of data, drafting or revising of the manuscript, and have approved the manuscript as submitted.
Conflict of interest The authors declare no competing interests.
Research involving human participants and/or animals This article does not contain any studies with human participants or animals performed by any of the authors. We did not use individual data but published data. These data have been widely utilized in research and..
References
Aghajani, Moradi, Amini, Decreased inhospital mortality associated with aspirin administration in hospitalized patients due to severe COVID-19, J Med Virol, doi:10.1002/jmv.27053
Alamdari, Afaghi, Rahimi, Mortality risk factors among hospitalized COVID-19 patients in a major referral center in Iran, Tohoku J Exp Med, doi:10.1620/tjem.252.73
An, Lim, Kim, Machine learning prediction for mortality of patients diagnosed with COVID-19: a nationwide Korean cohort study, Sci Rep, doi:10.1038/s41598-020-75767-2
Asiimwe, Pushpakom, Turner, Cardiovascular drugs and COVID-19 clinical outcomes: a living systematic review and meta-analysis, Br J Clin Pharmacol, doi:10.1111/bcp.14927
Asiimwe, Pushpakom, Turner, Cardiovascular drugs and COVID-19 clinical outcomes: a systematic review and meta-analysis of randomized controlled trials, Br J Clin Pharmacol, doi:10.1111/bcp.15331.10.1111/bcp.15331
Bae, Ahn, Tantry, Should antithrombotic treatment strategies in East Asians differ from Caucasians?, Curr Vasc Pharmacol, doi:10.2174/1570161116666180117103238
Barnes, Burnett, Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum, J Thromb Thrombolysis, doi:10.1007/s11239-020-02138-z
Bianconi, Violi, Fallarino, Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?, Drugs, doi:10.1007/s40265-020-01365-1
Bozzani, Arici, Tavazzi, Acute arterial and deep venous thromboembolism in COVID-19 patients: risk factors and personalized therapy, Surgery, doi:10.1016/j.surg.2020.09.009
Chabert, Damien, Verhoeven, Acetylsalicylic acid differentially limits the activation and expression of cell death markers in human platelets exposed to Staphylococcus aureus strains, Sci Rep, doi:10.1038/s41598-017-06024-2
Chen, Xu, Taooka, Cyclooxygenase 2 1195G > A polymorphism is associated with chronic obstructive pulmonary disease in Japanese and Chinese patients, Chin Med J (Engl), doi:10.3760/cma.j.issn.0366-6999.20121456
Chow, Khanna, Kethireddy, Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019, Anesth Analg, doi:10.1213/ANE.0000000000005292
Crombie, GRADE: an emerging consensus on rating quality of evidence and strength of recommendations, BMJ, doi:10.1136/bmj.39489.470347.AD
Diaz, Trachtenberg, Abraham, Aspirin bioactivity for prevention of cardiovascular injury in COVID-19, Front Cardiovasc Med, doi:10.3389/fcvm.2020.562708
Dobesh, Trujillo, Coagulopathy, venous thromboembolism, and anticoagulation in patients with COVID-19, Pharmacotherapy, doi:10.1002/phar.2465
Du, Jiang, He, Antiplatelet therapy for critically ill patients: a pairwise and Bayesian network meta-analysis, Shock, doi:10.1097/SHK.0000000000001057
Egger, Smith, Schneider, Bias in metaanalysis detected by a simple, graphical test, BMJ, doi:10.1136/bmj.315.7109.629
Formiga, Rubio-Rivas, Mora-Luján, Does admission acetylsalicylic acid uptake in hospitalized COVID-19 patients have a protective role? Data from the Spanish SEMI-COVID-19 Registry, Intern Emerg Med, doi:10.1007/s11739-021-02870-1
Glatthaar-Saalmüller, Mair, Saalmüller, Antiviral activity of aspirin against RNA viruses of the respiratory tract-an in vitro study, Influenza Other Respir Viruses, doi:10.1111/irv.12421
Gu, Tyagi, Jain, Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation, Nat Rev Cardiol, doi:10.1007/10.1038/s41569-020-00469-1
Haidich, Meta-analysis in medical research, Hippokratia
Hannachi, Baudoin, Prasanth, The distinct effects of aspirin on platelet aggregation induced by infectious bacteria, Platelets, doi:10.1080/09537104.2019.1704717
Higgins, Altman, Gøtzsche, The Cochrane Collaboration's tool for assessing risk of bias in randomised trials, BMJ, doi:10.1136/bmj.d5928
Higgins, Green, Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration
Husain, Sayem, Kamal, Beneficial effect of low dose aspirin in adult patients with COVID-19: a retrospective observational study in Bangladesh, Mymensingh Med J
Kim, Yoon, Kim, Aspirin is related to worse clinical outcomes of COVID-19, Medicina (Kaunas), doi:10.3390/medicina57090931
Liu, Huang, Li, Effect of low-dose aspirin on mortality and viral duration of the hospitalized adults with COVID-19, Medicine (Baltimore), doi:10.1097/MD.0000000000024544
Lodigiani, Iapichino, Carenzo, Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy Thromb Res, doi:10.1016/j.thromres.2020.04.024
Martha, Pranata, Lim, Active prescription of low-dose aspirin during or prior to hospitalization and mortality in COVID-19: a systematic review and meta-analysis of adjusted effect estimates, Int J Infect Dis, doi:10.1016/j.ijid.2021.05.016
Mazur, Wurzer, Ehrhardt, Acetylsalicylic acid (ASA) blocks influenza virus propagation via its NF-kappaBinhibiting activity, Cell Microbiol, doi:10.1111/j.1462-5822.2007.00902.x
Mcbane Rd 2nd, Roldan, Anticoagulation in COVID-19: a systematic review, meta-analysis, and rapid guidance from Mayo Clinic, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.08.030
Mei, Luo, Hu, Thrombocytopenia and thrombosis in hospitalized patients with COVID-19, J Hematol Oncol, doi:10.1186/s13045-020-01003-z
Meizlish, Goshua, Liu, Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis, Am J Hematol, doi:10.1002/ajh.26102
Melenotte, Silvin, Goubet, Immune responses during COVID-19 infection, Oncoimmunology, doi:10.1080/2162402X.2020.1807836
Merzon, Green, Vinker, The use of aspirin for primary prevention of cardiovascular disease is associated with a lower likelihood of COVID-19 infection, FEBS J, doi:10.1111/febs.15784.10.1111/febs.15784
Minno, Ambrosino, Calcaterra, COVID-19 and venous thromboembolism: a meta-analysis of literature studies, Semin Thromb Hemost, doi:10.1055/s-0040-1715456
Moher, Liberati, Tetzlaff, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, BMJ, doi:10.1136/bmj.b2535
Nishiga, Wang, Han, COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives, Nat Rev Cardiol, doi:10.1038/s41569-020-0413-9
Osborne, Veigulis, Arreola, Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration, PLoS ONE, doi:10.1371/journal.pone.0246825
Porfidia, Pola, Venous thromboembolism in COVID-19 patients, J Thromb Haemost, doi:10.1111/jth.14842
Pranata, Lim, Yonas, Thrombocytopenia as a prognostic marker in COVID-19 patients: diagnostic test accuracy meta-analysis, Epidemiol Infect, doi:10.1017/S0950268821000236
Primache, Binda, Benedittis, In vitro activity of acetylsalicylic acid on replication of varicella-zoster virus, New Microbiol
Ronksley, Brien, Turner, Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis, BMJ, doi:10.1136/bmj.d671
Sahai, Bhandari, Godwin, Effect of aspirin on short-term outcomes in hospitalized patients with COVID-19, Vasc Med, doi:10.1177/1358863X211012754
Salah, Mehta, Meta-analysis of the effect of aspirin on mortality in COVID-19, Am J Cardiol, doi:10.1016/j.amjcard.2020.12.073
Schrör, Aspirin and platelets: the antiplatelet action of aspirin and its role in thrombosis treatment and prophylaxis, Semin Thromb Hemost, doi:10.1055/s-2007-996108
Sivaloganathan, Ladikou, Chevassut, COVID-19 mortality in patients on anticoagulants and antiplatelet agents, Br J Haematol, doi:10.1016/10.1111/bjh.16968
Son, Noh, Lee, Effect of aspirin on coronavirus disease 2019: a nationwide case-control study in South Korea, Medicine (Baltimore), doi:10.1097/MD.0000000000026670
Speir, Yu, Ferrans, Aspirin attenuates cytomegalovirus infectivity and gene expression mediated by cyclooxygenase-2 in coronary artery smooth muscle cells, Circ Res, doi:10.1161/01.res.83.2.210
Stang, Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses, Eur J Epidemiol
Stare, Maucort-Boulch, Odds ratio, hazard ratio and relative risk, Metodoloski zvezki
Sánchez-García, Ibarra, Ar, Use of proteomic analysis tools to identify HCV-proteins down-regulated by acetylsalicylic acid, Ann Hepatol, doi:10.1016/s1665-2681(19)31313-4
Tufanaru, Munn, Stephenson, Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness, Int J Evid Based Healthc, doi:10.1097/XEB.0000000000000065
Vahedian-Azimi, Rahimibashar, Najafi, Association of in-hospital use of statins, aspirin, and renin-angiotensinaldosterone inhibitors with mortality and ICU admission due to COVID-19, Adv Exp Med Biol, doi:10.1007/978-3-030-71697-4_17
Viecca, Radovanovic, Forleo, Enhanced platelet inhibition treatment improves hypoxemia in patients with severe Covid-19 and hypercoagulability. A case control, proof of concept study, Pharmacol Res, doi:10.1016/j.phrs.2020.104950
Wang, Li, Gu, Effect of antiplatelet therapy on acute respiratory distress syndrome and mortality in critically ill patients: a meta-analysis, PLoS One, doi:10.1371/journal.pone.0154754
Weng, Li, Li, The association of four common polymorphisms from four candidate genes (COX-1, COX-2, ITGA2B, ITGA2) with aspirin insensitivity: a meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0078093
Yang, Yang, Wang, Thrombocytopenia and its association with mortality in patients with COVID-19, J Thromb Haemost, doi:10.1111/jth.14848
Yuan, Chen, Li, Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease, J Cell Mol Med, doi:10.1111/jcmm.16198
Zhang, What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes, JAMA, doi:10.1001/jama.280.19.1690
Zhou Revised The Paper. Shaodi, Ma, Su, Chenyu Sun had primary responsibility for final content
DOI record:
{
"DOI": "10.1007/s00228-022-03356-5",
"ISSN": [
"0031-6970",
"1432-1041"
],
"URL": "http://dx.doi.org/10.1007/s00228-022-03356-5",
"alternative-id": [
"3356"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "14 March 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "14 June 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "22 June 2022"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "This article does not contain any studies with human participants or animals performed by any of the authors. We did not use individual data but published data. These data have been widely utilized in research and are generally available. Therefore, we confirm that any aspect of the work covered in this manuscript has been conducted with ethical approval. And this study has been registered (registration number: CRD42021241027) with the PROSPERO (International Prospective Register of Systematic Reviews) and was conducted according to the Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA) statement."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "All individuals gave written informed consent for publication. The authors are responsible for the reported research, and have participated in the concept and design, analysis and interpretation of data, drafting or revising of the manuscript, and have approved the manuscript as submitted."
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare no competing interests."
},
{
"group": {
"label": "Research involving human participants and/or animals",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "This article does not contain any studies with human participants or animals performed by any of the authors. We did not use individual data but published data. These data have been widely utilized in research and are generally available."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Ma",
"given": "Shaodi",
"sequence": "first"
},
{
"affiliation": [],
"family": "Su",
"given": "Wanying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Chenyu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lowe",
"given": "Scott",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhou",
"given": "Zhen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Haixia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qu",
"given": "Guangbo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xia",
"given": "Weihang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xie",
"given": "Peng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wu",
"given": "Birong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gao",
"given": "Juan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Feng",
"given": "Linya",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8651-8059",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sun",
"given": "Yehuan",
"sequence": "additional"
}
],
"container-title": "European Journal of Clinical Pharmacology",
"container-title-short": "Eur J Clin Pharmacol",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T22:02:50Z",
"timestamp": 1655935370000
},
"deposited": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T07:07:29Z",
"timestamp": 1660115249000
},
"indexed": {
"date-parts": [
[
2024,
7,
10
]
],
"date-time": "2024-07-10T16:37:59Z",
"timestamp": 1720629479302
},
"is-referenced-by-count": 14,
"issue": "9",
"issued": {
"date-parts": [
[
2022,
6,
22
]
]
},
"journal-issue": {
"issue": "9",
"published-print": {
"date-parts": [
[
2022,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T00:00:00Z",
"timestamp": 1655856000000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T00:00:00Z",
"timestamp": 1655856000000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00228-022-03356-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s00228-022-03356-5/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00228-022-03356-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "1403-1420",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2022,
6,
22
]
]
},
"published-online": {
"date-parts": [
[
2022,
6,
22
]
]
},
"published-print": {
"date-parts": [
[
2022,
9
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "3356_CR1",
"unstructured": "Center for Systems Science and Engineering at Johns Hopkins University (2022) COVID-19 dashboard. https://coronavirus.jhu.edu/map.html. Accessed 25 Feb 2022"
},
{
"DOI": "10.1017/S0950268821000236",
"author": "R Pranata",
"doi-asserted-by": "publisher",
"journal-title": "Epidemiol Infect",
"key": "3356_CR2",
"unstructured": "Pranata R, Lim MA, Yonas E et al (2021) Thrombocytopenia as a prognostic marker in COVID-19 patients: diagnostic test accuracy meta-analysis. Epidemiol Infect 149:e40. https://doi.org/10.1017/S0950268821000236",
"volume": "149",
"year": "2021"
},
{
"DOI": "10.1186/s13045-020-01003-z",
"doi-asserted-by": "publisher",
"key": "3356_CR3",
"unstructured": "Mei H, Luo L, Hu Y (2020) Thrombocytopenia and thrombosis in hospitalized patients with COVID-19. J Hematol Oncol 13(1):161. https://doi.org/10.1186/s13045-020-01003-z"
},
{
"DOI": "10.1111/jth.14848",
"author": "X Yang",
"doi-asserted-by": "publisher",
"first-page": "1469",
"issue": "6",
"journal-title": "J Thromb Haemost",
"key": "3356_CR4",
"unstructured": "Yang X, Yang Q, Wang Y et al (2020) Thrombocytopenia and its association with mortality in patients with COVID-19. J Thromb Haemost 18(6):1469–1472. https://doi.org/10.1111/jth.14848",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1007/s11239-020-02138-z",
"author": "GD Barnes",
"doi-asserted-by": "publisher",
"first-page": "72",
"issue": "1",
"journal-title": "J Thromb Thrombolysis",
"key": "3356_CR5",
"unstructured": "Barnes GD, Burnett A, Allen A et al (2020) Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis 50(1):72–81. https://doi.org/10.1007/s11239-020-02138-z",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1038/s41569-020-0413-9",
"author": "M Nishiga",
"doi-asserted-by": "publisher",
"first-page": "543",
"issue": "9",
"journal-title": "Nat Rev Cardiol",
"key": "3356_CR6",
"unstructured": "Nishiga M, Wang DW, Han Y et al (2020) COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol 17(9):543–558. https://doi.org/10.1038/s41569-020-0413-9",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1055/s-0040-1715456",
"author": "A Di Minno",
"doi-asserted-by": "publisher",
"first-page": "763",
"issue": "7",
"journal-title": "Semin Thromb Hemost",
"key": "3356_CR7",
"unstructured": "Di Minno A, Ambrosino P, Calcaterra I et al (2020) COVID-19 and venous thromboembolism: a meta-analysis of literature studies. Semin Thromb Hemost 46(7):763–771. https://doi.org/10.1055/s-0040-1715456",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.surg.2020.09.009",
"author": "A Bozzani",
"doi-asserted-by": "publisher",
"first-page": "987",
"issue": "6",
"journal-title": "Surgery",
"key": "3356_CR8",
"unstructured": "Bozzani A, Arici V, Tavazzi G et al (2020) Acute arterial and deep venous thromboembolism in COVID-19 patients: risk factors and personalized therapy. Surgery 168(6):987–992. https://doi.org/10.1016/j.surg.2020.09.009",
"volume": "168",
"year": "2020"
},
{
"DOI": "10.1111/jth.14842",
"author": "A Porfidia",
"doi-asserted-by": "publisher",
"first-page": "1516",
"issue": "6",
"journal-title": "J Thromb Haemost",
"key": "3356_CR9",
"unstructured": "Porfidia A, Pola R (2020) Venous thromboembolism in COVID-19 patients. J Thromb Haemost 18(6):1516–1517. https://doi.org/10.1111/jth.14842",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1002/phar.2465",
"author": "PP Dobesh",
"doi-asserted-by": "publisher",
"first-page": "1130",
"issue": "11",
"journal-title": "Pharmacotherapy",
"key": "3356_CR10",
"unstructured": "Dobesh PP, Trujillo TC (2020) Coagulopathy, venous thromboembolism, and anticoagulation in patients with COVID-19. Pharmacotherapy 40(11):1130–1151. https://doi.org/10.1002/phar.2465",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.08.030",
"author": "RD McBane 2nd",
"doi-asserted-by": "publisher",
"first-page": "2467",
"issue": "11",
"journal-title": "Mayo Clin Proc",
"key": "3356_CR11",
"unstructured": "McBane RD 2nd, Torres Roldan VD, Niven AS et al (2020) Anticoagulation in COVID-19: a systematic review, meta-analysis, and rapid guidance from Mayo Clinic. Mayo Clin Proc 95(11):2467–2486. https://doi.org/10.1016/j.mayocp.2020.08.030",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1016/10.1111/bjh.16968",
"author": "H Sivaloganathan",
"doi-asserted-by": "publisher",
"first-page": "e192",
"issue": "4",
"journal-title": "Br J Haematol",
"key": "3356_CR12",
"unstructured": "Sivaloganathan H, Ladikou EE, Chevassut T (2020) COVID-19 mortality in patients on anticoagulants and antiplatelet agents. Br J Haematol 190(4):e192–e195. https://doi.org/10.1016/10.1111/bjh.16968",
"volume": "190",
"year": "2020"
},
{
"DOI": "10.1055/s-2007-996108",
"author": "K Schrör",
"doi-asserted-by": "publisher",
"first-page": "349",
"issue": "4",
"journal-title": "Semin Thromb Hemost",
"key": "3356_CR13",
"unstructured": "Schrör K (1997) Aspirin and platelets: the antiplatelet action of aspirin and its role in thrombosis treatment and prophylaxis. Semin Thromb Hemost 23(4):349–356. https://doi.org/10.1055/s-2007-996108",
"volume": "23",
"year": "1997"
},
{
"DOI": "10.1007/10.1038/s41569-020-00469-1",
"author": "SX Gu",
"doi-asserted-by": "publisher",
"first-page": "194",
"issue": "3",
"journal-title": "Nat Rev Cardiol",
"key": "3356_CR14",
"unstructured": "Gu SX, Tyagi T, Jain K et al (2021) Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol 18(3):194–209. https://doi.org/10.1007/10.1038/s41569-020-00469-1",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1097/SHK.0000000000001057",
"author": "F Du",
"doi-asserted-by": "publisher",
"first-page": "616",
"issue": "6",
"journal-title": "Shock",
"key": "3356_CR15",
"unstructured": "Du F, Jiang P, He S et al (2018) Antiplatelet therapy for critically ill patients: a pairwise and Bayesian network meta-analysis. Shock 49(6):616–624. https://doi.org/10.1097/SHK.0000000000001057",
"volume": "49",
"year": "2018"
},
{
"DOI": "10.1371/journal.pone.0154754",
"author": "L Wang",
"doi-asserted-by": "publisher",
"issue": "5",
"journal-title": "PLoS ONE",
"key": "3356_CR16",
"unstructured": "Wang L, Li H, Gu X et al (2016) Effect of antiplatelet therapy on acute respiratory distress syndrome and mortality in critically ill patients: a meta-analysis. PLoS One 11(5):e0154754. https://doi.org/10.1371/journal.pone.0154754",
"volume": "11",
"year": "2016"
},
{
"DOI": "10.1111/jcmm.16198",
"author": "S Yuan",
"doi-asserted-by": "publisher",
"first-page": "1263",
"issue": "2",
"journal-title": "J Cell Mol Med",
"key": "3356_CR17",
"unstructured": "Yuan S, Chen P, Li H et al (2021) Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease. J Cell Mol Med 25(2):1263–1273. https://doi.org/10.1111/jcmm.16198",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1213/ANE.0000000000005292",
"doi-asserted-by": "publisher",
"key": "3356_CR18",
"unstructured": "Chow JH, Khanna AK, Kethireddy S et al (2021) Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019. Anesth Analg 132(4):930–941. https://doi.org/10.1213/ANE.0000000000005292"
},
{
"DOI": "10.1136/bmj.b2535",
"author": "D Moher",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "3356_CR19",
"unstructured": "Moher D, Liberati A, Tetzlaff J et al (2020) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535",
"volume": "339",
"year": "2020"
},
{
"DOI": "10.1136/bmj.d5928",
"author": "JP Higgins",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "3356_CR20",
"unstructured": "Higgins JP, Altman DG, Gøtzsche PC et al (2020) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928",
"volume": "343",
"year": "2020"
},
{
"DOI": "10.1007/s10654-010-9491-z",
"author": "A Stang",
"doi-asserted-by": "publisher",
"first-page": "603",
"journal-title": "Eur J Epidemiol",
"key": "3356_CR21",
"unstructured": "Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605",
"volume": "25",
"year": "2010"
},
{
"key": "3356_CR22",
"unstructured": "Higgins JPT, Green S [webpage on the Internet] (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. Available from: https://handbook.cochrane.org/. Updated March 2011"
},
{
"key": "3356_CR23",
"unstructured": "Crombie I (1996) Pocket guide to critical appraisal. 1st ed. London: John Wiley & Sons"
},
{
"DOI": "10.1136/bmj.39489.470347.AD",
"author": "GH Guyatt",
"doi-asserted-by": "publisher",
"first-page": "924",
"issue": "7650",
"journal-title": "BMJ",
"key": "3356_CR24",
"unstructured": "Guyatt GH, Oxman AD, Vist GE et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924–926. https://doi.org/10.1136/bmj.39489.470347.AD",
"volume": "336",
"year": "2008"
},
{
"author": "J Stare",
"first-page": "59",
"issue": "1",
"journal-title": "Metodoloski zvezki",
"key": "3356_CR25",
"unstructured": "Stare J, Maucort-Boulch D (1998) Odds ratio, hazard ratio and relative risk. Metodoloski zvezki 13(1):59–67",
"volume": "13",
"year": "1998"
},
{
"key": "3356_CR26",
"unstructured": "A glossary of EBM terms. BMJ Best Practice https://bestpractice.bmj.com/info/us/toolkit/ebm-tools/a-glossary-of-ebm-terms/. Accessed 25 May 2022"
},
{
"DOI": "10.1136/bmj.d671",
"author": "PE Ronksley",
"doi-asserted-by": "publisher",
"first-page": "479",
"journal-title": "BMJ",
"key": "3356_CR27",
"unstructured": "Ronksley PE, Brien SE, Turner BJ et al (2011) Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 342:479. https://doi.org/10.1136/bmj.d671",
"volume": "342",
"year": "2011"
},
{
"DOI": "10.1001/jama.280.19.1690",
"author": "JYK Zhang",
"doi-asserted-by": "publisher",
"first-page": "1690",
"journal-title": "JAMA",
"key": "3356_CR28",
"unstructured": "Zhang JYK (1998) What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280:1690–1691. https://doi.org/10.1001/jama.280.19.1690",
"volume": "280",
"year": "1998"
},
{
"DOI": "10.1097/XEB.0000000000000065",
"author": "C Tufanaru",
"doi-asserted-by": "publisher",
"first-page": "196",
"issue": "3",
"journal-title": "Int J Evid Based Healthc",
"key": "3356_CR29",
"unstructured": "Tufanaru C, Munn Z, Stephenson M et al (2015) Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Based Healthc 13(3):196–207. https://doi.org/10.1097/XEB.0000000000000065",
"volume": "13",
"year": "2015"
},
{
"author": "AB Haidich",
"first-page": "29",
"issue": "Suppl 1",
"journal-title": "Hippokratia",
"key": "3356_CR30",
"unstructured": "Haidich AB (2010) Meta-analysis in medical research. Hippokratia 14(Suppl 1):29–37",
"volume": "14",
"year": "2010"
},
{
"DOI": "10.1136/bmj.315.7109.629",
"author": "M Egger",
"doi-asserted-by": "publisher",
"first-page": "629",
"issue": "7109",
"journal-title": "BMJ",
"key": "3356_CR31",
"unstructured": "Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629",
"volume": "315",
"year": "1997"
},
{
"DOI": "10.1007/s11739-021-02870-1",
"author": "F Formiga",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Intern Emerg Med",
"key": "3356_CR32",
"unstructured": "Formiga F, Rubio-Rivas M, Mora-Luján JM et al (2021) Does admission acetylsalicylic acid uptake in hospitalized COVID-19 patients have a protective role? Data from the Spanish SEMI-COVID-19 Registry. Intern Emerg Med 29:1–15. https://doi.org/10.1007/s11739-021-02870-1",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27053",
"author": "M Haji Aghajani",
"doi-asserted-by": "publisher",
"first-page": "5390",
"issue": "9",
"journal-title": "J Med Virol",
"key": "3356_CR33",
"unstructured": "Haji Aghajani M, Moradi O, Amini H et al (2021) Decreased in-hospital mortality associated with aspirin administration in hospitalized patients due to severe COVID-19. J Med Virol 93(9):5390–5395. https://doi.org/10.1002/jmv.27053",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.3390/medicina57090931",
"author": "I Kim",
"doi-asserted-by": "publisher",
"first-page": "931",
"issue": "9",
"journal-title": "Medicina (Kaunas)",
"key": "3356_CR34",
"unstructured": "Kim I, Yoon S, Kim M et al (2021) Aspirin is related to worse clinical outcomes of COVID-19. Medicina (Kaunas) 57(9):931. https://doi.org/10.3390/medicina57090931",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1016/j.thromres.2020.04.024",
"author": "C Lodigiani",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "Italy Thromb Res",
"key": "3356_CR35",
"unstructured": "Lodigiani C, Iapichino G, Carenzo L et al (2020) Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan. Italy Thromb Res 191:9–14. https://doi.org/10.1016/j.thromres.2020.04.024",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.1002/ajh.26102",
"author": "ML Meizlish",
"doi-asserted-by": "publisher",
"first-page": "471",
"issue": "4",
"journal-title": "Am J Hematol",
"key": "3356_CR36",
"unstructured": "Meizlish ML, Goshua G, Liu Y et al (2021) Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis. Am J Hematol 96(4):471–479. https://doi.org/10.1002/ajh.26102",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0246825",
"author": "TF Osborne",
"doi-asserted-by": "publisher",
"issue": "2",
"journal-title": "PLoS ONE",
"key": "3356_CR37",
"unstructured": "Osborne TF, Veigulis ZP, Arreola DM et al (2021) Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration. PLoS ONE 16(2):e0246825. https://doi.org/10.1371/journal.pone.0246825",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1177/1358863X211012754",
"author": "A Sahai",
"doi-asserted-by": "publisher",
"first-page": "626",
"issue": "6",
"journal-title": "Vasc Med",
"key": "3356_CR38",
"unstructured": "Sahai A, Bhandari R, Godwin M et al (2021) Effect of aspirin on short-term outcomes in hospitalized patients with COVID-19. Vasc Med 26(6):626–632. https://doi.org/10.1177/1358863X211012754",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1007/978-3-030-71697-4_17",
"author": "A Vahedian-Azimi",
"doi-asserted-by": "publisher",
"first-page": "205",
"journal-title": "Adv Exp Med Biol",
"key": "3356_CR39",
"unstructured": "Vahedian-Azimi A, Rahimibashar F, Najafi A et al (2021) Association of in-hospital use of statins, aspirin, and renin-angiotensin-aldosterone inhibitors with mortality and ICU admission due to COVID-19. Adv Exp Med Biol 1327:205–214. https://doi.org/10.1007/978-3-030-71697-4_17",
"volume": "1327",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-75767-2",
"author": "C An",
"doi-asserted-by": "publisher",
"first-page": "18716",
"issue": "1",
"journal-title": "Sci Rep",
"key": "3356_CR40",
"unstructured": "An C, Lim H, Kim DW et al (2020) Machine learning prediction for mortality of patients diagnosed with COVID-19: a nationwide Korean cohort study. Sci Rep 10(1):18716. https://doi.org/10.1038/s41598-020-75767-2",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1097/MD.0000000000024544",
"author": "Q Liu",
"doi-asserted-by": "publisher",
"issue": "6",
"journal-title": "Medicine (Baltimore)",
"key": "3356_CR41",
"unstructured": "Liu Q, Huang N, Li A et al (2021) Effect of low-dose aspirin on mortality and viral duration of the hospitalized adults with COVID-19. Medicine (Baltimore) 100(6):e24544. https://doi.org/10.1097/MD.0000000000024544",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.1097/MD.0000000000026670",
"author": "M Son",
"doi-asserted-by": "publisher",
"issue": "30",
"journal-title": "Medicine (Baltimore)",
"key": "3356_CR42",
"unstructured": "Son M, Noh MG, Lee JH et al (2021) Effect of aspirin on coronavirus disease 2019: a nationwide case-control study in South Korea. Medicine (Baltimore) 100(30):e26670. https://doi.org/10.1097/MD.0000000000026670",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.1016/j.phrs.2020.104950",
"doi-asserted-by": "publisher",
"key": "3356_CR43",
"unstructured": "Viecca M, Radovanovic D, Forleo GB et al (2020) Enhanced platelet inhibition treatment improves hypoxemia in patients with severe Covid-19 and hypercoagulability. A case control, proof of concept study. Pharmacol Res 158:104950. https://doi.org/10.1016/j.phrs.2020.104950"
},
{
"DOI": "10.1111/febs.15784.10.1111/febs.15784",
"author": "E Merzon",
"doi-asserted-by": "publisher",
"journal-title": "FEBS J",
"key": "3356_CR44",
"unstructured": "Merzon E, Green I, Vinker S et al (2021) The use of aspirin for primary prevention of cardiovascular disease is associated with a lower likelihood of COVID-19 infection. FEBS J. https://doi.org/10.1111/febs.15784.10.1111/febs.15784",
"year": "2021"
},
{
"DOI": "10.1620/tjem.252.73",
"author": "NM Alamdari",
"doi-asserted-by": "publisher",
"first-page": "73",
"issue": "1",
"journal-title": "Tohoku J Exp Med",
"key": "3356_CR45",
"unstructured": "Alamdari NM, Afaghi S, Rahimi FS et al (2020) Mortality risk factors among hospitalized COVID-19 patients in a major referral center in Iran. Tohoku J Exp Med 252(1):73–84. https://doi.org/10.1620/tjem.252.73",
"volume": "252",
"year": "2020"
},
{
"author": "A Husain",
"first-page": "194",
"issue": "1",
"journal-title": "Mymensingh Med J",
"key": "3356_CR46",
"unstructured": "Husain A, Sayem MA, Kamal SM et al (2022) Beneficial effect of low dose aspirin in adult patients with COVID-19: a retrospective observational study in Bangladesh. Mymensingh Med J 31(1):194–199 (PMID: 34999702)",
"volume": "31",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(21)01825-0",
"author": "RECOVERY Collaborative Group",
"doi-asserted-by": "publisher",
"first-page": "143",
"issue": "10320",
"journal-title": "Lancet",
"key": "3356_CR47",
"unstructured": "RECOVERY Collaborative Group (2022) Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 399(10320):143–151. https://doi.org/10.1016/S0140-6736(21)01825-0",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1016/j.amjcard.2020.12.073",
"author": "HM Salah",
"doi-asserted-by": "publisher",
"first-page": "159",
"issue": "158",
"journal-title": "Am J Cardiol",
"key": "3356_CR48",
"unstructured": "Salah HM, Mehta JL (2021) Meta-analysis of the effect of aspirin on mortality in COVID-19. Am J Cardiol 142(158):159. https://doi.org/10.1016/j.amjcard.2020.12.073",
"volume": "142",
"year": "2021"
},
{
"DOI": "10.1111/bcp.14927",
"author": "IG Asiimwe",
"doi-asserted-by": "publisher",
"first-page": "4534",
"issue": "12",
"journal-title": "Br J Clin Pharmacol",
"key": "3356_CR49",
"unstructured": "Asiimwe IG, Pushpakom S, Turner RM et al (2021) Cardiovascular drugs and COVID-19 clinical outcomes: a living systematic review and meta-analysis. Br J Clin Pharmacol 87(12):4534–4545. https://doi.org/10.1111/bcp.14927",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.1111/bcp.15331.10.1111/bcp.15331",
"author": "IG Asiimwe",
"doi-asserted-by": "publisher",
"journal-title": "Br J Clin Pharmacol",
"key": "3356_CR50",
"unstructured": "Asiimwe IG, Pushpakom SP, Turner RM et al (2022) Cardiovascular drugs and COVID-19 clinical outcomes: a systematic review and meta-analysis of randomized controlled trials. Br J Clin Pharmacol. https://doi.org/10.1111/bcp.15331.10.1111/bcp.15331",
"year": "2022"
},
{
"DOI": "10.1080/2162402X.2020.1807836",
"author": "C Melenotte",
"doi-asserted-by": "publisher",
"first-page": "1807836",
"issue": "1",
"journal-title": "Oncoimmunology",
"key": "3356_CR51",
"unstructured": "Melenotte C, Silvin A, Goubet AG et al (2020) Immune responses during COVID-19 infection. Oncoimmunology 9(1):1807836. https://doi.org/10.1080/2162402X.2020.1807836",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3389/fcvm.2020.562708",
"author": "T Diaz",
"doi-asserted-by": "publisher",
"journal-title": "Front Cardiovasc Med",
"key": "3356_CR52",
"unstructured": "Diaz T, Trachtenberg BH, Abraham SJK et al (2020) Aspirin bioactivity for prevention of cardiovascular injury in COVID-19. Front Cardiovasc Med 7:562708. https://doi.org/10.3389/fcvm.2020.562708",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1007/s40265-020-01365-1",
"author": "V Bianconi",
"doi-asserted-by": "publisher",
"first-page": "1383",
"issue": "14",
"journal-title": "Drugs",
"key": "3356_CR53",
"unstructured": "Bianconi V, Violi F, Fallarino F et al (2020) Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19? Drugs 80(14):1383–1396. https://doi.org/10.1007/s40265-020-01365-1",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1111/irv.12421",
"author": "B Glatthaar-Saalmüller",
"doi-asserted-by": "publisher",
"first-page": "85",
"issue": "1",
"journal-title": "Influenza Other Respir Viruses",
"key": "3356_CR54",
"unstructured": "Glatthaar-Saalmüller B, Mair KH, Saalmüller A (2017) Antiviral activity of aspirin against RNA viruses of the respiratory tract-an in vitro study. Influenza Other Respir Viruses 11(1):85–92. https://doi.org/10.1111/irv.12421",
"volume": "11",
"year": "2017"
},
{
"DOI": "10.1161/01.res.83.2.210",
"author": "E Speir",
"doi-asserted-by": "publisher",
"first-page": "210",
"issue": "2",
"journal-title": "Circ Res",
"key": "3356_CR55",
"unstructured": "Speir E, Yu ZX, Ferrans VJ et al (1998) Aspirin attenuates cytomegalovirus infectivity and gene expression mediated by cyclooxygenase-2 in coronary artery smooth muscle cells. Circ Res 83(2):210–216. https://doi.org/10.1161/01.res.83.2.210",
"volume": "83",
"year": "1998"
},
{
"author": "V Primache",
"first-page": "397",
"issue": "4",
"journal-title": "New Microbiol",
"key": "3356_CR56",
"unstructured": "Primache V, Binda S, De Benedittis G et al (1998) In vitro activity of acetylsalicylic acid on replication of varicella-zoster virus. New Microbiol 21(4):397–401 (PMID: 9812322)",
"volume": "21",
"year": "1998"
},
{
"DOI": "10.1016/s1665-2681(19)31313-4",
"author": "A Sánchez-García",
"doi-asserted-by": "publisher",
"first-page": "732",
"issue": "725",
"journal-title": "Ann Hepatol",
"key": "3356_CR57",
"unstructured": "Sánchez-García A, Ríos-Ibarra CP, Rincón-Sánchez AR et al (2013) Use of proteomic analysis tools to identify HCV-proteins down-regulated by acetylsalicylic acid. Ann Hepatol 12(725):732. https://doi.org/10.1016/s1665-2681(19)31313-4",
"volume": "12",
"year": "2013"
},
{
"DOI": "10.1111/j.1462-5822.2007.00902.x",
"author": "I Mazur",
"doi-asserted-by": "publisher",
"first-page": "1683",
"issue": "7",
"journal-title": "Cell Microbiol",
"key": "3356_CR58",
"unstructured": "Mazur I, Wurzer WJ, Ehrhardt C et al (2007) Acetylsalicylic acid (ASA) blocks influenza virus propagation via its NF-kappaB-inhibiting activity. Cell Microbiol 9(7):1683–1694. https://doi.org/10.1111/j.1462-5822.2007.00902.x",
"volume": "9",
"year": "2007"
},
{
"DOI": "10.1371/journal.pone.0078093",
"author": "Z Weng",
"doi-asserted-by": "publisher",
"issue": "11",
"journal-title": "PLoS ONE",
"key": "3356_CR59",
"unstructured": "Weng Z, Li X, Li Y et al (2013) The association of four common polymorphisms from four candidate genes (COX-1, COX-2, ITGA2B, ITGA2) with aspirin insensitivity: a meta-analysis. PLoS ONE 8(11):e78093. https://doi.org/10.1371/journal.pone.0078093",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.3760/cma.j.issn.0366-6999.20121456",
"author": "LJ Chen",
"doi-asserted-by": "publisher",
"first-page": "2215",
"issue": "12",
"journal-title": "Chin Med J (Engl)",
"key": "3356_CR60",
"unstructured": "Chen LJ, Xu W, Taooka Y et al (2013) Cyclooxygenase 2 1195G > A polymorphism is associated with chronic obstructive pulmonary disease in Japanese and Chinese patients. Chin Med J (Engl) 126(12):2215–2221. https://doi.org/10.3760/cma.j.issn.0366-6999.20121456",
"volume": "126",
"year": "2013"
},
{
"DOI": "10.2174/1570161116666180117103238",
"author": "JS Bae",
"doi-asserted-by": "publisher",
"first-page": "459",
"issue": "5",
"journal-title": "Curr Vasc Pharmacol",
"key": "3356_CR61",
"unstructured": "Bae JS, Ahn JH, Tantry US et al (2018) Should antithrombotic treatment strategies in East Asians differ from Caucasians? Curr Vasc Pharmacol 16(5):459–476. https://doi.org/10.2174/1570161116666180117103238",
"volume": "16",
"year": "2018"
},
{
"DOI": "10.1080/09537104.2019.1704717",
"author": "N Hannachi",
"doi-asserted-by": "publisher",
"first-page": "1028",
"issue": "8",
"journal-title": "Platelets",
"key": "3356_CR62",
"unstructured": "Hannachi N, Baudoin JP, Prasanth A et al (2020) The distinct effects of aspirin on platelet aggregation induced by infectious bacteria. Platelets 31(8):1028–1038. https://doi.org/10.1080/09537104.2019.1704717",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1038/s41598-017-06024-2",
"author": "A Chabert",
"doi-asserted-by": "publisher",
"first-page": "5610",
"issue": "1",
"journal-title": "Sci Rep",
"key": "3356_CR63",
"unstructured": "Chabert A, Damien P, Verhoeven PO et al (2017) Acetylsalicylic acid differentially limits the activation and expression of cell death markers in human platelets exposed to Staphylococcus aureus strains. Sci Rep 7(1):5610. https://doi.org/10.1038/s41598-017-06024-2",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1016/j.ijid.2021.05.016",
"author": "JW Martha",
"doi-asserted-by": "publisher",
"first-page": "6",
"journal-title": "Int J Infect Dis",
"key": "3356_CR64",
"unstructured": "Martha JW, Pranata R, Lim MA et al (2021) Active prescription of low-dose aspirin during or prior to hospitalization and mortality in COVID-19: a systematic review and meta-analysis of adjusted effect estimates. Int J Infect Dis 108:6–12. https://doi.org/10.1016/j.ijid.2021.05.016",
"volume": "108",
"year": "2021"
}
],
"reference-count": 64,
"references-count": 64,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s00228-022-03356-5"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Does aspirin have an effect on risk of death in patients with COVID-19? A meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "78"
}