Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration
et al., PLOS ONE, doi:10.1371/journal.pone.0246825, Feb 2021
Retrospective PSM analysis of pre-existing aspirin use in the USA, showing lower mortality with treatment.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
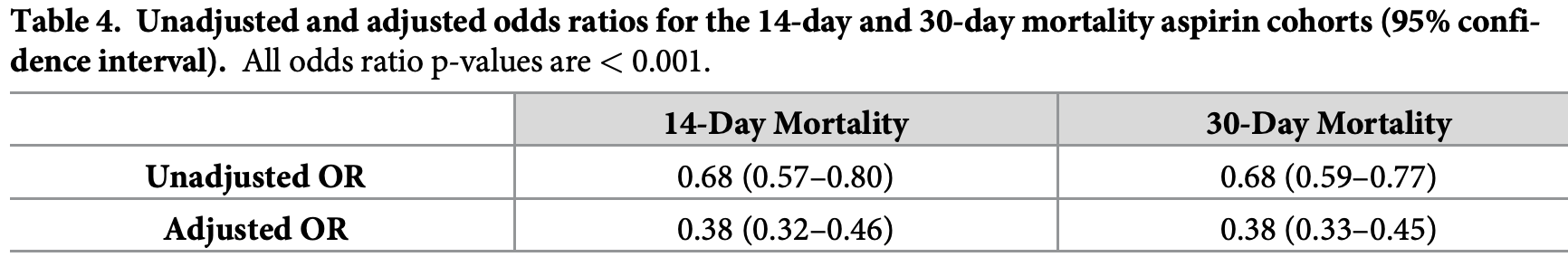
risk of death, 59.4% lower, RR 0.41, p < 0.001, treatment 272 of 6,300 (4.3%), control 661 of 6,300 (10.5%), NNT 16, odds ratio converted to relative risk, 30 days, PSM.
|
|
risk of death, 60.5% lower, RR 0.40, p < 0.001, treatment 170 of 6,814 (2.5%), control 427 of 6,814 (6.3%), NNT 27, odds ratio converted to relative risk, 14 days, PSM.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Osborne et al., 11 Feb 2021, retrospective, propensity score matching, USA, peer-reviewed, 6 authors.
Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration
PLOS ONE, doi:10.1371/journal.pone.0246825
There is growing evidence that thrombotic and inflammatory pathways contribute to the severity of COVID-19. Common medications such as aspirin, that mitigate these pathways, may decrease COVID-19 mortality. This retrospective assessment was designed to quantify the correlation between pre-diagnosis aspirin and mortality for COVID-19 positive patients in our care. Data from the Veterans Health Administration national electronic health record database was utilized for the evaluation. Veterans from across the country with a first positive COVID-19 polymerase chain reaction lab result were included in the evaluation which comprised 35,370 patients from March 2, 2020 to September 13, 2020 for the 14-day mortality cohort and 32,836 patients from March 2, 2020 to August 28, 2020 for the 30-day mortality cohort. Patients were matched via propensity scores and the odds of mortality were then compared. Among COVID-19 positive Veterans, preexisting aspirin prescription was associated with a statistically and clinically significant decrease in overall mortality at 14days (OR 0.38, 95% CI 0.32-0.46) and at 30-days (OR 0.38, 95% CI 0.33-0.45), cutting the odds of mortality by more than half. Findings demonstrated that pre-diagnosis aspirin prescription was strongly associated with decreased mortality rates for Veterans diagnosed with COVID-19. Prospective evaluation is required to more completely assess this correlation and its implications for patient care.
Supporting information S1 Table . The 31 medication variables utilized in the logistic regression analysis. If a unique medication was present in more than 10% of the cohort, it was included as its own variable. All other medications were grouped as "other" by drug class. This resulted in the inclusion of 31 variables across 14 separate medication classes. (DOCX)
S2 Table. The variables utilized to calculate the CAN 1-year mortality model (version 2.5). (DOCX)
Author Contributions Conceptualization: Thomas F. Osborne, Zachary P. Veigulis. Data curation: Zachary P. Veigulis, David M. Arreola, Satish M. Mahajan. Formal analysis: Thomas F. Osborne, Zachary P. Veigulis, David M. Arreola, Satish M. Mahajan, Eliane Ro ¨o ¨sli, Catherine M. Curtin. Investigation: Thomas F. Osborne, Zachary P. Veigulis, David M. Arreola, Satish M. Mahajan, Catherine M. Curtin. Methodology: Thomas F. Osborne, Satish M. Mahajan, Eliane Ro ¨o ¨sli, Catherine M. Curtin. Project administration: Thomas F. Osborne. Supervision: Thomas F. Osborne, Catherine M. Curtin. Validation: Zachary P. Veigulis, Eliane Ro ¨o ¨sli, Catherine M. Curtin. Writing -original draft: Thomas F. Osborne. Writing -review & editing: Zachary P. Veigulis, David M. Arreola, Satish M. Mahajan, Eliane Ro ¨o ¨sli, Catherine M. Curtin.
References
Albandar, Markert, Agrawal, The relationship between aspirin use and mortality in colorectal cancer, Journal of Gastrointestinal Oncology, doi:10.21037/jgo.2018.08.13
Aly, Ibrahim, Should aspirin be used for prophylaxis of COVID-19-induced coagulopathy?, Medical Hypotheses, doi:10.1016/j.mehy.2020.109975
Arentz, Yim, Klaff, Lokhandwala, Riedo et al., Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State, Jama, doi:10.1001/jama.2020.4326
Cheruiyot, Kipkorir, Ngure, Misiani, Munguti et al., Arterial Thrombosis in Coronavirus Disease 2019 Patients: A Rapid Systematic Review, Ann Vasc Surg, doi:10.1016/j.avsg.2020.08.087
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19, Anesthesia & Analgesia
Diaz, Trachtenberg, Abraham, Kosagisharaf, Aa, Aspirin Bioactivity for Prevention of Cardiovascular Injury in COVID-19, Frontiers in Cardiovascular Medicine, doi:10.3389/fcvm.2020.562708
Elgar, Stefaniak, Wohl, The trouble with trust: Time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries, Social Science & Medicine
Kizer, Demakis, Feussner, Reinventing VA health care: systematizing quality improvement and quality innovation, Medical care
Koupenova, Kehrel, Corkrey, Freedman, Thrombosis and platelets: an update, European heart journal, doi:10.1093/eurheartj/ehw550
Li, Wang, Zhou, Chang, Xian et al., Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study, Stroke Vasc Neurol, doi:10.1136/svn-2020-000431
Little, Non-steroidal anti-inflammatory drugs and covid-19
Osborne, Suarez, Edwards, Hernandez-Boussard, Curtin, Patient Electronic Health Records Score for Preoperative Risk Assessment Before Total Knee Arthroplasty, JBJS Open Access, doi:10.2106/JBJS.OA.19.00061
Osborne, Veigulis, Arreola, ¨o ¨sli, Curtin, Automated EHR score to predict COVID-19 outcomes at US Department of Veterans Affairs, Plos One, doi:10.1371/journal.pone.0236554
Pickett, Wilkinson, Income inequality and health: a causal review, Social Science & Medicine, doi:10.1016/j.socscimed.2014.12.031
Wang, Cidade, Larsen, Pearman, Schimpf et al., Main results report, prepared for Strategic Analysis Service
Wichmann, Sperhake, Lu ¨tgehetmann, Steurer, Edler et al., Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study, Annals of internal medicine, doi:10.7326/M20-2003
Yan, Yang, Wang, Ren, Zhang et al., Clinical characteristics and outcomes of patients with severe covid-19 with diabetes, BMJ Open Diabetes Research and Care, doi:10.1136/bmjdrc-2020-001343
¨ller, Mair, Saalmu, Antiviral activity of aspirin against RNA viruses of the respiratory tract-an in vitro study, Influenza and other respiratory viruses, doi:10.1111/irv.12421
DOI record:
{
"DOI": "10.1371/journal.pone.0246825",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0246825",
"abstract": "<jats:p>There is growing evidence that thrombotic and inflammatory pathways contribute to the severity of COVID-19. Common medications such as aspirin, that mitigate these pathways, may decrease COVID-19 mortality. This retrospective assessment was designed to quantify the correlation between pre-diagnosis aspirin and mortality for COVID-19 positive patients in our care. Data from the Veterans Health Administration national electronic health record database was utilized for the evaluation. Veterans from across the country with a first positive COVID-19 polymerase chain reaction lab result were included in the evaluation which comprised 35,370 patients from March 2, 2020 to September 13, 2020 for the 14-day mortality cohort and 32,836 patients from March 2, 2020 to August 28, 2020 for the 30-day mortality cohort. Patients were matched via propensity scores and the odds of mortality were then compared. Among COVID-19 positive Veterans, preexisting aspirin prescription was associated with a statistically and clinically significant decrease in overall mortality at 14-days (OR 0.38, 95% CI 0.32–0.46) and at 30-days (OR 0.38, 95% CI 0.33–0.45), cutting the odds of mortality by more than half. Findings demonstrated that pre-diagnosis aspirin prescription was strongly associated with decreased mortality rates for Veterans diagnosed with COVID-19. Prospective evaluation is required to more completely assess this correlation and its implications for patient care.</jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-8896-2487",
"affiliation": [],
"authenticated-orcid": true,
"family": "Osborne",
"given": "Thomas F.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-9026-1604",
"affiliation": [],
"authenticated-orcid": true,
"family": "Veigulis",
"given": "Zachary P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Arreola",
"given": "David M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mahajan",
"given": "Satish M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0557-6239",
"affiliation": [],
"authenticated-orcid": true,
"family": "Röösli",
"given": "Eliane",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0850-9277",
"affiliation": [],
"authenticated-orcid": true,
"family": "Curtin",
"given": "Catherine M.",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2021,
2,
12
]
],
"date-time": "2021-02-12T00:02:01Z",
"timestamp": 1613088121000
},
"deposited": {
"date-parts": [
[
2021,
2,
12
]
],
"date-time": "2021-02-12T00:02:42Z",
"timestamp": 1613088162000
},
"editor": [
{
"affiliation": [],
"family": "den Uil",
"given": "Corstiaan",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
8
]
],
"date-time": "2024-04-08T19:57:15Z",
"timestamp": 1712606235053
},
"is-referenced-by-count": 74,
"issue": "2",
"issued": {
"date-parts": [
[
2021,
2,
11
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2021,
2,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/publicdomain/zero/1.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
11
]
],
"date-time": "2021-02-11T00:00:00Z",
"timestamp": 1613001600000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0246825",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0246825",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2021,
2,
11
]
]
},
"published-online": {
"date-parts": [
[
2021,
2,
11
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"article-title": "Reinventing VA health care: systematizing quality improvement and quality innovation",
"author": "KW Kizer",
"first-page": "I7",
"journal-title": "Medical care",
"key": "pone.0246825.ref001",
"volume": "2000",
"year": "2000"
},
{
"author": "JZ Wang",
"key": "pone.0246825.ref002",
"volume-title": "Main results report, prepared for Strategic Analysis Service (SAS) Office of Strategic Planning and Analysis (OSPA) Veterans Health Administration",
"year": "2019"
},
{
"key": "pone.0246825.ref003",
"unstructured": "About VHA. Washington, DC: Veterans Health Administration, July 2019. (https://www.va.gov/health/aboutvha.asp). Accessed May 1, 2020"
},
{
"DOI": "10.1136/bmjdrc-2020-001343",
"article-title": "Clinical characteristics and outcomes of patients with severe covid-19 with diabetes",
"author": "Y Yan",
"doi-asserted-by": "crossref",
"first-page": "e001343",
"journal-title": "BMJ Open Diabetes Research and Care",
"key": "pone.0246825.ref004",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.4326",
"article-title": "Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State",
"author": "M Arentz",
"doi-asserted-by": "crossref",
"first-page": "1612",
"issue": "16",
"journal-title": "Jama",
"key": "pone.0246825.ref005",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.2106/JBJS.OA.19.00061",
"article-title": "Patient Electronic Health Records Score for Preoperative Risk Assessment Before Total Knee Arthroplasty",
"author": "TF Osborne",
"doi-asserted-by": "crossref",
"first-page": "e0061",
"journal-title": "JBJS Open Access",
"key": "pone.0246825.ref006",
"volume": "5",
"year": "2020"
},
{
"article-title": "Automated EHR score to predict COVID-19 outcomes at US Department of Veterans Affairs",
"author": "TF Osborne",
"journal-title": "Plos One",
"key": "pone.0246825.ref007",
"year": "2020"
},
{
"DOI": "10.21037/jgo.2018.08.13",
"article-title": "The relationship between aspirin use and mortality in colorectal cancer",
"author": "HJ Albandar",
"doi-asserted-by": "crossref",
"first-page": "1133",
"issue": "6",
"journal-title": "Journal of Gastrointestinal Oncology",
"key": "pone.0246825.ref008",
"volume": "9",
"year": "2018"
},
{
"author": "JH Chow",
"key": "pone.0246825.ref009",
"volume-title": "Aspirin use is associated with decreased mechanical ventilation",
"year": "2020"
},
{
"article-title": "Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study",
"author": "D Wichmann",
"journal-title": "Annals of internal medicine",
"key": "pone.0246825.ref010",
"year": "2020"
},
{
"article-title": "Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study",
"author": "Y Li",
"journal-title": "Stroke Vasc Neurol",
"key": "pone.0246825.ref011",
"year": "2020"
},
{
"DOI": "10.1016/j.mehy.2020.109975",
"article-title": "Should aspirin be used for prophylaxis of COVID-19-induced coagulopathy?",
"author": "AA Mohamed-Hussein",
"doi-asserted-by": "crossref",
"first-page": "109975",
"journal-title": "Medical Hypotheses",
"key": "pone.0246825.ref012",
"volume": "144",
"year": "2020"
},
{
"article-title": "Arterial Thrombosis in Coronavirus Disease 2019 Patients: A Rapid Systematic Review",
"author": "I Cheruiyot",
"first-page": "273",
"journal-title": "Ann Vasc Surg. 2021 Jan",
"key": "pone.0246825.ref013",
"volume": "70"
},
{
"article-title": "Thrombosis and platelets: an update",
"author": "M Koupenova",
"first-page": "785",
"issue": "11",
"journal-title": "European heart journal",
"key": "pone.0246825.ref014",
"volume": "38",
"year": "2017"
},
{
"DOI": "10.3389/fcvm.2020.562708",
"article-title": "Aspirin Bioactivity for Prevention of Cardiovascular Injury in COVID-19",
"author": "T Diaz",
"doi-asserted-by": "crossref",
"first-page": "317",
"journal-title": "Frontiers in Cardiovascular Medicine",
"key": "pone.0246825.ref015",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1111/irv.12421",
"article-title": "Antiviral activity of aspirin against RNA viruses of the respiratory tract—an in vitro study",
"author": "B Glatthaar‐Saalmüller",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Influenza and other respiratory viruses",
"key": "pone.0246825.ref016",
"volume": "11",
"year": "2017"
},
{
"DOI": "10.1136/bmj.m1185",
"author": "P Little",
"doi-asserted-by": "crossref",
"key": "pone.0246825.ref017",
"volume-title": "Non-steroidal anti-inflammatory drugs and covid-19",
"year": "2020"
},
{
"key": "pone.0246825.ref018",
"unstructured": "The use of non-steroidal anti-inflammatory drugs (NSAIDs) in patients with COVID-19: scientific brief, 19 April 2020: World Health Organization; 2020. Report No.: WHO/2019-nCoV/Sci_Brief/NSAIDs/2020.1. Accessed July 24, 2020"
},
{
"DOI": "10.1016/j.socscimed.2014.12.031",
"article-title": "Income inequality and health: a causal review",
"author": "KE Pickett",
"doi-asserted-by": "crossref",
"first-page": "316",
"journal-title": "Social Science & Medicine",
"key": "pone.0246825.ref019",
"volume": "128",
"year": "2015"
},
{
"DOI": "10.1016/j.socscimed.2020.113365",
"article-title": "The trouble with trust: Time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries",
"author": "FJ Elgar",
"doi-asserted-by": "crossref",
"first-page": "113365",
"journal-title": "Social Science & Medicine",
"key": "pone.0246825.ref020",
"volume": "263",
"year": "2020"
}
],
"reference-count": 20,
"references-count": 20,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0246825"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "16"
}