Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: A propensity score-matched analysis
et al., American Journal of Hematology, doi:10.1002/ajh.26102, Jan 2021
Retrospective 638 matched hospitalized patients in the USA, 319 treated with aspirin, showing lower mortality with treatment.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 47.8% lower, HR 0.52, p = 0.004, treatment 319, control 319, PSM.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Meizlish et al., 21 Jan 2021, retrospective, propensity score matching, USA, peer-reviewed, 22 authors.
Intermediate‐dose anticoagulation, aspirin, and in‐hospital mortality in COVID ‐19: A propensity score‐matched analysis
American Journal of Hematology, doi:10.1002/ajh.26102
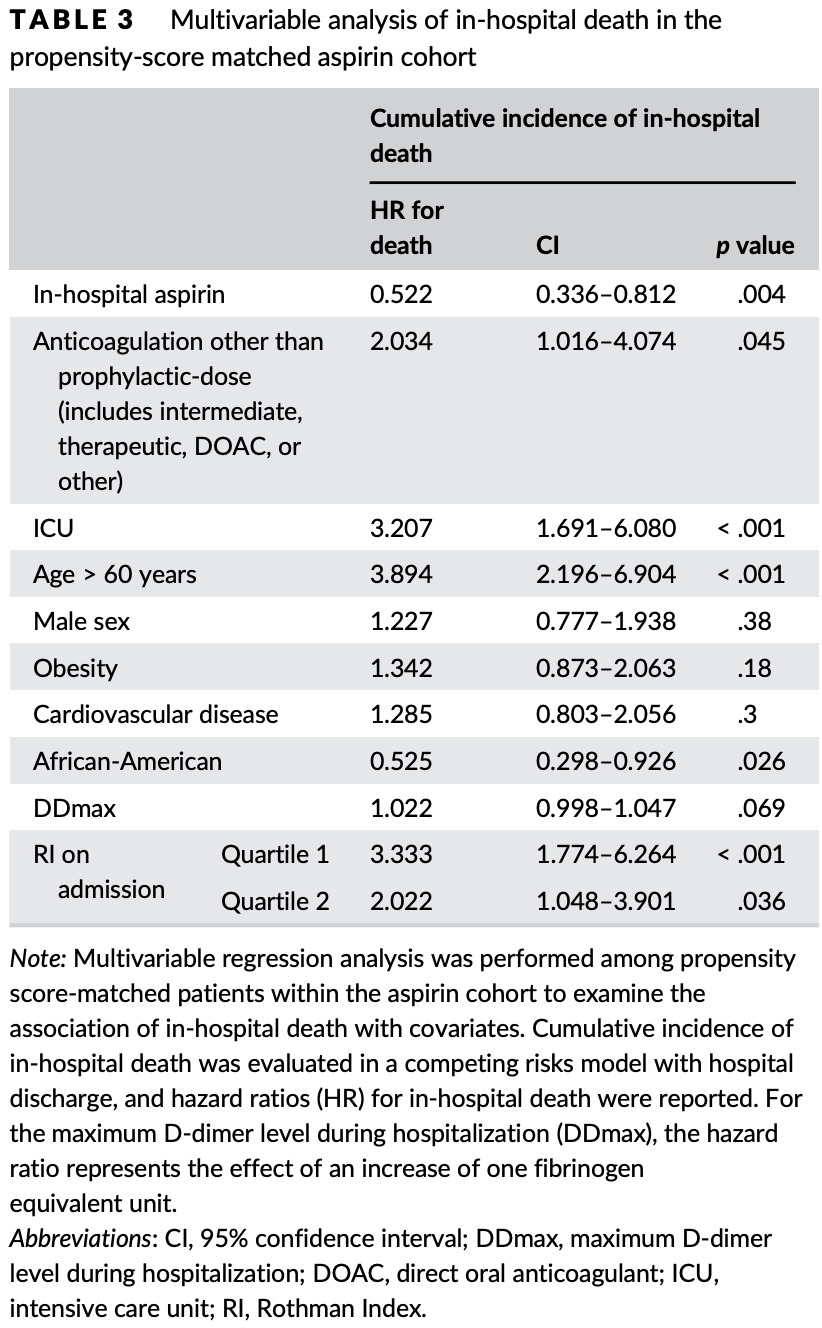
Thrombotic complications occur at high rates in hospitalized patients with COVID-19, yet the impact of intensive antithrombotic therapy on mortality is uncertain. We examined in-hospital mortality with intermediate-compared to prophylactic-dose anticoagulation, and separately with in-hospital aspirin compared to no antiplatelet therapy, in a large, retrospective study of 2785 hospitalized adult COVID-19 patients. In this analysis, we established two separate, nested cohorts of patients (a) who received intermediate-or prophylactic-dose anticoagulation ("anticoagulation cohort", N = 1624), or (b) who were not on home antiplatelet therapy and received either in-hospital aspirin or no antiplatelet therapy ("aspirin cohort", N = 1956). To minimize bias and adjust for confounding factors, we incorporated propensity score matching and multivariable regression utilizing various markers of illness severity and other patient-specific covariates, yielding treatment groups with well-balanced
ETHICS APPROVAL STATEMENT This study was approved by the Yale Institutional Review Board (HIC 2000027792).
PATIENT CONSENT STATEMENT Patient consent was not mandated for this study. Permission to reproduce material from other sources: No material from other sources is included in this study.
CLINICAL TRIAL REGISTRATION This study was not a clinical trial.
SUPPORTING INFORMATION Additional supporting information may be found online in the Supporting Information section at the end of this article.
References
Ackermann, Verleden, Kuehnel, Pulmonary vascular Endothelialitis, thrombosis, and angiogenesis in Covid-19, N Engl J Med
Adam, Zacharowski, Miesbach, A comprehensive assessment of the coagulation profile in critically ill COVID-19 patients, Thromb Res
Al-Samkari, Leaf, Dzik, COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection, Blood
Alarhayem, Muir, Jenkins, Application of electronic medical record-derived analytics in critical care: Rothman index predicts mortality and readmissions in surgical intensive care unit patients, J Trauma Acute Care Surg
Barnes, Burnett, Allen, Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum, J Thromb Thrombolysis
Barrett, Moore, Yaffe, Moore, ISTH interim guidance on recognition and management of coagulopathy in COVID-19: a comment, J Thromb Haemost
Blombery, Scully, Management of thrombotic thrombocytopenic purpura: current perspectives, J Blood Med
Carsana, Sonzogni, Nasr, Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-Centre descriptive study, Lancet Infect Dis
Chow, Khanna, Kethireddy, Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19, Anesth Analg, doi:10.1213/ANE.0000000000005292
Chowdhury, Moores, Connors, Anticoagulation in hospitalized patients with Covid-19, N Engl J Med
Connors, Levy, COVID-19 and its implications for thrombosis and anticoagulation, Blood
Ferguson, Volk, Vondracek, Flanigan, Chernaik, Empiric therapeutic anticoagulation and mortality in critically ill patients with respiratory failure from SARS-CoV-2: a retrospective cohort study, J Clin Pharmacol
Ferrandis, Llau, Quintana, COVID-19: opening a new paradigm in thromboprophylaxis for critically ill patients?, Crit Care
Fine, Gray, A proportional hazards model for the subdistribution of a competing risk, J Am Stat Assoc
Geleris, Sun, Platt, Observational study of hydroxychloroquine in hospitalized patients with Covid-19, N Engl J Med
Goshua, Pine, Meizlish, Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, crosssectional study, Lancet Haematol
Gray, A class of K-sample tests for comparing the cumulative incidence of a competing risk, Ann Stat
Gupta, Hayek, Wang, Factors associated with death in critically ill patients with coronavirus disease 2019 in the US, JAMA Intern Med
Hernan, Logan, Observational studies analyzed like randomized experiments: an application to postmenopausal hormone therapy and coronary heart disease, Epidemiology
Hgs, Leaf, Thrombosis, bleeding, and the effect of anticoagulation on survival in critically ill patients with COVID-19 in the United States, Res Pract Thromb Haemost, doi:10.7326/M20-6739
Ho, Dusendang, Schmittdiel, Kavecansky, Tavakoli et al., Anticoagulant and antiplatelet use not associated with improvement in severe outcomes in COVID-19 patients, Blood
Hottz, Azevedo-Quintanilha, Palhinha, Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19, Blood
Ionescu, Nair, Konde, Increasing doses of anticoagulation are associated with improved survival in hospitalized COVID-19 patients
Kashi, Jacquin, Dakhil, Severe arterial thrombosis associated with Covid-19 infection, Thromb Res
Lowenstein, Solomon, Severe COVID-19 is a microvascular disease, Circulation
Manne, Denorme, Middleton, Platelet gene expression and function in patients with COVID-19, Blood
Merkler, Parikh, Mir, Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza, JAMA Neurol
Moores, Tritschler, Brosnahan, Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST guideline and expert panel report, Chest
Nadkarni, Bagiella, Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19, J Am Coll Cardiol
Nakazawa, Ishizu, Immunothrombosis in severe COVID-19, EBioMedicine
Nopp, Moik, Jilma, Pabinger, Ay, Risk of venous thromboembolism in patients with COVID-19: a systematic review and metaanalysis, Res Pract Thromb Haemost
Paranjpe, Fuster, Lala, Association of Treatment Dose Anticoagulation with in-Hospital Survival among Hospitalized Patients with COVID-19, J Am Coll Cardiol
Pesavento, Ceccato, Pasquetto, The hazard of (sub)therapeutic doses of anticoagulants in non-critically ill patients with Covid-19: the Padua province experience, J Thromb Haemost
Petrilli, Jones, Yang, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in new York City: prospective cohort study, BMJ
Reynolds, Adhikari, Pulgarin, Renin-angiotensinaldosterone system inhibitors and risk of Covid-19, N Engl J Med
Rothman, Rothman, Beals, Development and validation of a continuous measure of patient condition using the electronic medical record, J Biomed Inform
Spyropoulos, Levy, Ageno, Scientific and standardization committee communication: clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost
Sturmer, Wyss, Glynn, Brookhart, Propensity scores for confounder adjustment when assessing the effects of medical interventions using nonexperimental study designs, J Intern Med
Taccone, Gevenois, Peluso, Higher intensity Thromboprophylaxis regimens and pulmonary embolism in critically ill coronavirus disease 2019 patients, Crit Care Med
Tang, Bai, Chen, Gong, Li et al., Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy, J Thromb Haemost
Tang, Li, Wang, Sun, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, J Thromb Haemost
Trigonis, Holt, Yuan, Incidence of venous thromboembolism in critically ill coronavirus disease 2019 patients receiving prophylactic anticoagulation, Crit Care Med
Wengerter, Pei, Asuzu, Davis, Rothman index variability predicts clinical deterioration and rapid response activation, Am J Surg
Zhang, Yan, Fan, D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19, J Thromb Haemost
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1002/ajh.26102",
"ISSN": [
"0361-8609",
"1096-8652"
],
"URL": "http://dx.doi.org/10.1002/ajh.26102",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Thrombotic complications occur at high rates in hospitalized patients with COVID‐19, yet the impact of intensive antithrombotic therapy on mortality is uncertain. We examined in‐hospital mortality with intermediate‐ compared to prophylactic‐dose anticoagulation, and separately with in‐hospital aspirin compared to no antiplatelet therapy, in a large, retrospective study of 2785 hospitalized adult COVID‐19 patients. In this analysis, we established two separate, nested cohorts of patients (a) who received intermediate‐ or prophylactic‐dose anticoagulation (“anticoagulation cohort”, N = 1624), or (b) who were not on home antiplatelet therapy and received either in‐hospital aspirin or no antiplatelet therapy (“aspirin cohort”, N = 1956). To minimize bias and adjust for confounding factors, we incorporated propensity score matching and multivariable regression utilizing various markers of illness severity and other patient‐specific covariates, yielding treatment groups with well‐balanced covariates in each cohort. The primary outcome was cumulative incidence of in‐hospital death. Among propensity score‐matched patients in the anticoagulation cohort (N = 382), in a multivariable regression model, intermediate‐ compared to prophylactic‐dose anticoagulation was associated with a significantly lower cumulative incidence of in‐hospital death (hazard ratio 0.518 [0.308–0.872]). Among propensity‐score matched patients in the aspirin cohort (N = 638), in a multivariable regression model, in‐hospital aspirin compared to no antiplatelet therapy was associated with a significantly lower cumulative incidence of in‐hospital death (hazard ratio 0.522 [0.336–0.812]). In this propensity score‐matched, observational study of COVID‐19, intermediate‐dose anticoagulation and aspirin were each associated with a lower cumulative incidence of in‐hospital death.</jats:p>",
"alternative-id": [
"10.1002/ajh.26102"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2021-01-18"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2021-01-18"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2021-02-22"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4306-5061",
"affiliation": [
{
"name": "Yale School of Medicine New Haven Connecticut USA"
}
],
"authenticated-orcid": false,
"family": "Meizlish",
"given": "Matthew L.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-1624-4427",
"affiliation": [
{
"name": "Section of Hematology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"authenticated-orcid": false,
"family": "Goshua",
"given": "George",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Dana‐Farber Cancer Institute Boston Massachusetts USA"
}
],
"family": "Liu",
"given": "Yiwen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Fine",
"given": "Rebecca",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy Yale‐New Haven Hospital New Haven Connecticut USA"
}
],
"family": "Amin",
"given": "Kejal",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Hematology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Chang",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy Yale‐New Haven Hospital New Haven Connecticut USA"
},
{
"name": "School of Pharmacy University of Connecticut Storrs Connecticut USA"
}
],
"family": "DeFilippo",
"given": "Nicholas",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Joint Data Analytics Team Yale New Haven Hospital New Haven Connecticut USA"
}
],
"family": "Keating",
"given": "Craig",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Hematology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Liu",
"given": "Yuxin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Mankbadi",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy Yale‐New Haven Hospital New Haven Connecticut USA"
}
],
"family": "McManus",
"given": "Dayna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Wang",
"given": "Stephen Y.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Allergy and Immunology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Price",
"given": "Christina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Hematology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Bona",
"given": "Robert D.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Vascular Surgery, Department of Surgery Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Ochoa Chaar",
"given": "Cassius Iyad",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Cardiology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Chun",
"given": "Hyung J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Hematology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Pine",
"given": "Alexander B.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Hematology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
},
{
"name": "Department of Laboratory Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Rinder",
"given": "Henry M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"family": "Siner",
"given": "Jonathan M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Dana‐Farber Cancer Institute Boston Massachusetts USA"
}
],
"family": "Neuberg",
"given": "Donna S.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy Yale‐New Haven Hospital New Haven Connecticut USA"
},
{
"name": "Clinical Redesign Yale New Haven Health New Haven Connecticut USA"
}
],
"family": "Owusu",
"given": "Kent A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5968-3948",
"affiliation": [
{
"name": "Section of Hematology, Department of Medicine Yale School of Medicine New Haven Connecticut USA"
}
],
"authenticated-orcid": false,
"family": "Lee",
"given": "Alfred Ian",
"sequence": "additional"
}
],
"container-title": "American Journal of Hematology",
"container-title-short": "American J Hematol",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2021,
1,
21
]
],
"date-time": "2021-01-21T20:21:22Z",
"timestamp": 1611260482000
},
"deposited": {
"date-parts": [
[
2023,
8,
27
]
],
"date-time": "2023-08-27T02:29:22Z",
"timestamp": 1693103362000
},
"funder": [
{
"DOI": "10.13039/100000002",
"award": [
"HL139116",
"GM136651",
"HL142818"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100005881",
"doi-asserted-by": "publisher",
"name": "Hemostasis and Thrombosis Research Society"
},
{
"DOI": "10.13039/100001422",
"doi-asserted-by": "publisher",
"name": "American Society of Hematology"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
24
]
],
"date-time": "2024-03-24T07:35:30Z",
"timestamp": 1711265730716
},
"is-referenced-by-count": 113,
"issue": "4",
"issued": {
"date-parts": [
[
2021,
2,
22
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2021,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://onlinelibrary.wiley.com/termsAndConditions#vor",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
22
]
],
"date-time": "2021-02-22T00:00:00Z",
"timestamp": 1613952000000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/ajh.26102",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1002/ajh.26102",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/ajh.26102",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"page": "471-479",
"prefix": "10.1002",
"published": {
"date-parts": [
[
2021,
2,
22
]
]
},
"published-online": {
"date-parts": [
[
2021,
2,
22
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1182/blood.2020006520",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_2_1"
},
{
"DOI": "10.1016/j.thromres.2020.05.025",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_3_1"
},
{
"DOI": "10.1001/jamaneurol.2020.2730",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_4_1"
},
{
"DOI": "10.1016/S1473-3099(20)30434-5",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_5_1"
},
{
"DOI": "10.1056/NEJMoa2015432",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_6_1"
},
{
"DOI": "10.1002/rth2.12439",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_7_1"
},
{
"DOI": "10.1097/CCM.0000000000004472",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_8_1"
},
{
"DOI": "10.1136/bmj.m1966",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_9_1"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_10_1"
},
{
"DOI": "10.1111/jth.14860",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_11_1"
},
{
"DOI": "10.1182/blood.2020006000",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_12_1"
},
{
"DOI": "10.1186/s13054-020-03052-9",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_13_1"
},
{
"DOI": "10.1016/j.thromres.2020.06.026",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_14_1"
},
{
"DOI": "10.1056/NEJMclde2028217",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_15_1"
},
{
"DOI": "10.1016/j.jacc.2020.08.041",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_16_1"
},
{
"DOI": "10.1016/j.jacc.2020.05.001",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_17_1"
},
{
"DOI": "10.1111/jth.14768",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_18_1"
},
{
"DOI": "10.1002/jcph.1749",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_19_1"
},
{
"DOI": "10.1111/jth.15022",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_20_1"
},
{
"DOI": "10.1182/blood-2020-134835",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_21_1"
},
{
"article-title": "Thrombosis, bleeding, and the effect of anticoagulation on survival in critically ill patients with COVID‐19 in the United States",
"author": "Al‐Samkari HGS",
"journal-title": "Res Pract Thromb Haemost",
"key": "e_1_2_12_22_1",
"year": "2020"
},
{
"DOI": "10.1182/blood-2020-134254",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_23_1"
},
{
"key": "e_1_2_12_24_1",
"unstructured": "NIH ACTIV Trial of blood thinners pauses enrollment of critically ill COVID‐19 patients. NIH News Releaseshttps://www.nih.gov/news‐events/news‐releases/nih‐activ‐trial‐blood‐thinners‐pauses‐enrollment‐critically‐ill‐covid‐19‐patients."
},
{
"key": "e_1_2_12_25_1",
"unstructured": "Full‐dose blood thinners decreased need for life support and improved outcome in hospitalized COVID‐19 patients. NHLBI News Statement.https://www.nhlbi.nih.gov/news/2021/full‐dose‐blood‐thinners‐decreased‐need‐life‐support‐and‐improved‐outcome‐hospitalized."
},
{
"DOI": "10.1016/j.ebiom.2020.102942",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_26_1"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.050354",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_27_1"
},
{
"DOI": "10.1016/S2352-3026(20)30216-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_28_1"
},
{
"DOI": "10.1182/blood.2020007252",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_29_1"
},
{
"DOI": "10.1182/blood.2020007214",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_30_1"
},
{
"DOI": "10.1213/ANE.0000000000005292",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_31_1"
},
{
"DOI": "10.1097/EDE.0b013e3181875e61",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_32_1"
},
{
"DOI": "10.1111/joim.12197",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_33_1"
},
{
"DOI": "10.1056/NEJMoa2012410",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_34_1"
},
{
"DOI": "10.1056/NEJMoa2008975",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_35_1"
},
{
"DOI": "10.1097/TA.0000000000002191",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_36_1"
},
{
"DOI": "10.1016/j.amjsurg.2017.07.031",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_37_1"
},
{
"DOI": "10.1016/j.jbi.2013.06.011",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_38_1"
},
{
"key": "e_1_2_12_39_1",
"unstructured": "Defining Adult Overweight and Obesity. Centers for Disease Control and Preventionhttps://wwwcdcgov/obesity/adult/defininghtml."
},
{
"DOI": "10.1080/01621459.1999.10474144",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_40_1"
},
{
"DOI": "10.1214/aos/1176350951",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_41_1"
},
{
"DOI": "10.1001/jamainternmed.2020.3596",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_42_1"
},
{
"DOI": "10.1111/jth.14859",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_43_1"
},
{
"DOI": "10.1007/s11239-020-02138-z",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_44_1"
},
{
"DOI": "10.1016/j.chest.2020.05.559",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_45_1"
},
{
"DOI": "10.1111/jth.14929",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_46_1"
},
{
"DOI": "10.1111/jth.14817",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_47_1"
},
{
"DOI": "10.1097/CCM.0000000000004548",
"doi-asserted-by": "publisher",
"key": "e_1_2_12_48_1"
},
{
"article-title": "Management of thrombotic thrombocytopenic purpura: current perspectives",
"author": "Blombery P",
"first-page": "15",
"journal-title": "J Blood Med",
"key": "e_1_2_12_49_1",
"volume": "5",
"year": "2014"
}
],
"reference-count": 48,
"references-count": 48,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.1101/2021.01.12.21249577",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/ajh.26102"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Hematology"
],
"subtitle": [],
"title": "Intermediate‐dose anticoagulation, aspirin, and in‐hospital mortality in <scp>COVID</scp>‐19: A propensity score‐matched analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "96"
}