All-cause and In-hospital Mortality after Aspirin Use in Patients Hospitalized with COVID-19: A Systematic Review and Meta-analysis
et al., Biology Methods and Protocols, doi:10.1093/biomethods/bpac027, Oct 2022
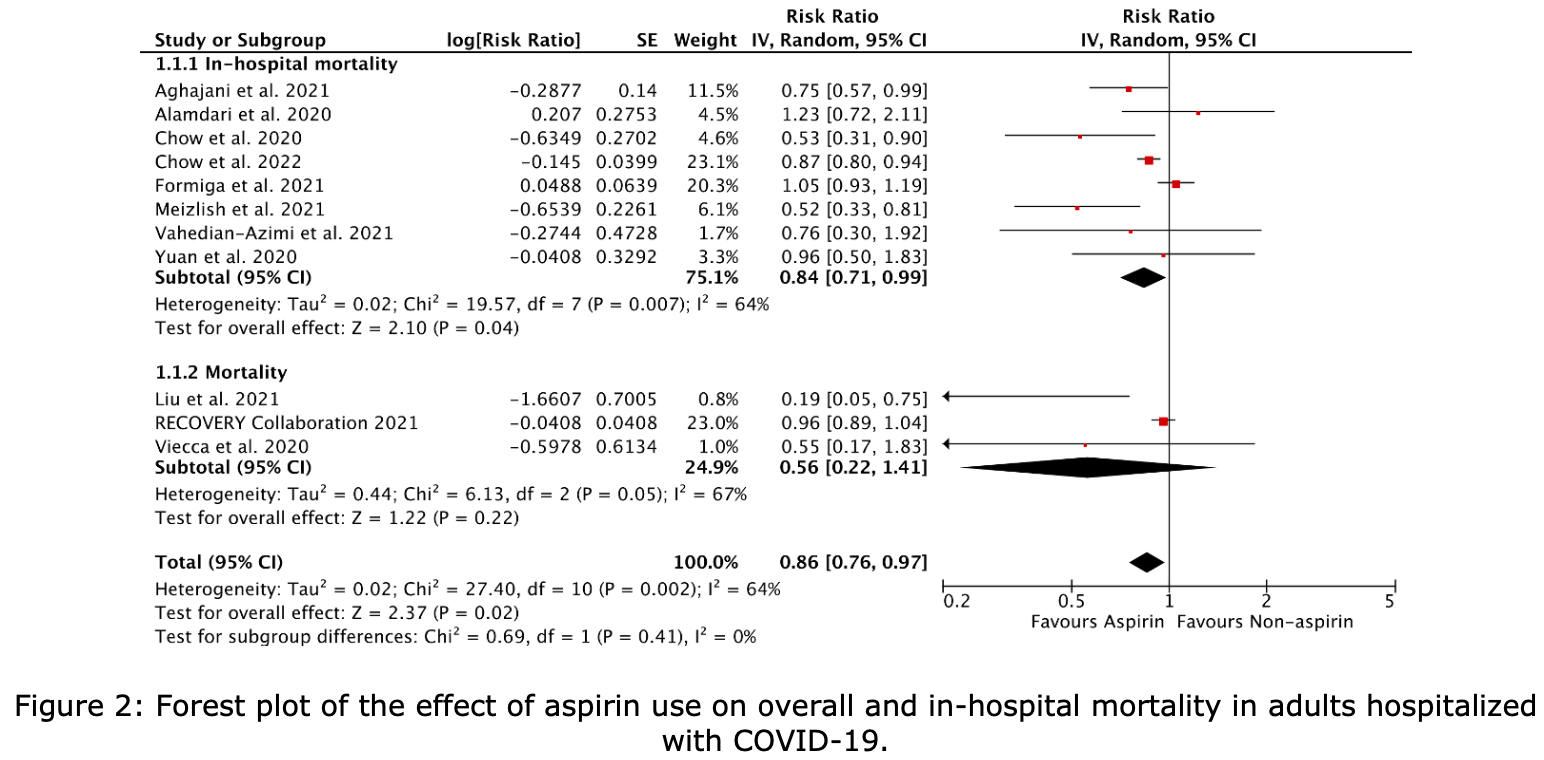
Systematic review and meta analysis of 11 aspirin COVID-19 studies, showing lower in-hospital mortality with treatment.
4 meta-analyses show significant improvements with aspirin for mortality1-3,
mechanical ventilation1, and
progression4.
Currently there are 79 aspirin for COVID-19 studies, showing 8% lower mortality [2‑14%], 5% lower ventilation [-5‑15%], 3% lower ICU admission [-11‑16%], 1% higher hospitalization [-4‑6%], and 5% fewer cases [-5‑14%].
|
risk of death, 14.0% lower, RR 0.86, p = 0.02.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Banaser et al., A systematic review and meta-analysis on efficacy of low dose aspirin on the management of COVID-19, International Journal of Medicine in Developing Countries, doi:10.24911/IJMDC.51-1640383699.
2.
Srinivasan et al., Aspirin use is associated with decreased inpatient mortality in patients with COVID-19: A meta-analysis, American Heart Journal Plus: Cardiology Research and Practice, doi:10.1016/j.ahjo.2022.100191.
Baral et al., 29 Oct 2022, peer-reviewed, 13 authors.
All-cause and In-hospital Mortality after Aspirin Use in Patients Hospitalized with COVID-19: A Systematic Review and Meta-analysis
doi:10.1093/biomethods/bpac027/6779966
64%). Among subgroups of studies reporting in-hospital mortality in COVID-19 hospitalizations, aspirin use was associated with a 16% decrease in in-hospital mortality compared to non-aspirin use (RR 0.84, 95% CI: 0.71-0.99, P=0.007, I 2 = 64%).
Conclusion: Our study shows that aspirin decreases in-hospital mortality in patients hospitalized with COVID-19. Further studies are needed to assess which COVID-19 patient populations benefit most, such as patients on aspirin for primary vs. secondary prevention of atherosclerotic disease. In addition, significant bleeding also needs to be considered when assessing the risk-benefit of aspirin use.
References
Abou-Ismail, Diamond, Kapoor, Arafah, Nayak, The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management, Thromb Res, doi:10.1016/j.thromres.2020.06.029
Aghajani, Moradi, Amini, Tehrani, Pourheidar et al., Decreased in-hospital mortality associated with aspirin administration in hospitalized patients due to severe COVID-19, J Med Virol, doi:10.1002/jmv.27053
Alamdari, Afaghi, Rahimi, Tarki, Tavana et al., Mortality Risk Factors among Hospitalized COVID-19 Patients in a Major Referral Center in Iran, Tohoku J Exp Med, doi:10.1620/tjem.252.73
Central, PMCPMC8013588 supported by a gift donation from Jack Levin and a separate anonymous donation to the Benign Hematology program at Yale, the DeLuca Foundation to fund hematology research at Yale, and the National Institutes of Health
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin Use Is Associated With Decreased Mechanical Ventilation, Intensive Care Unit Admission, and In-Hospital Mortality in Hospitalized Patients With Coronavirus Disease 2019, Anesth Analg, doi:10.1213/ane.0000000000005292
Chow, Rahnavard, Gomberg-Maitland, Chatterjee, Patodi et al., Association of Early Aspirin Use With In-Hospital Mortality in Patients With Moderate COVID-19, JAMA Netw Open, doi:10.1001/jamanetworkopen.2022.3890
Fardman, Zahger, Orvin, Oren, Kofman et al., Acute myocardial infarction in the Covid-19 era: Incidence, clinical characteristics and in-hospital outcomes-A multicenter registry, PLoS One, doi:10.1371/journal.pone.0253524
Formiga, Rubio-Rivas, Mora-Luján, Escudero, Martinez et al., Does admission acetylsalicylic acid uptake in hospitalized COVID-19 patients have a protective role? Data from the Spanish SEMI-COVID-19 Registry, Internal and Emergency Medicine
Hemming, Hughes, Mckenzie, Forbes, Extending the I-squared statistic to describe treatment effect heterogeneity in cluster, multi-centre randomized trials and individual patient data meta-analysis, Stat Methods Med Res, doi:10.1177/0962280220948550
Higgins, Altman, Gøtzsche, Jüni, Moher et al., Cochrane Bias Methods Group
Jiménez, García-Sanchez, Rali, Muriel, Bikdeli et al., Incidence of VTE and Bleeding Among Hospitalized Patients With Coronavirus Disease 2019: A Systematic Review and Meta-analysis, Chest, doi:10.1016/j.chest.2020.11.005
Liu, Huang, Li, Zhou, Liang et al., effect of low-dose aspirin on mortality and viral duration of the hospitalized adults with COVID-19, Medicine, doi:10.1097/md.0000000000024544
Ma, Sahu, Cano, Kuppuswamy, Bajwa et al., Increased complement activation is a distinctive feature of severe SARS-CoV-2 infection, Sci Immunol, doi:10.1126/sciimmunol.abh2259
Ma, Su, Sun, Lowe, Zhou et al., Does aspirin have an effect on risk of death in patients with COVID-19? A meta-analysis
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/s0140-6736(20)30628-0
Meizlish, Goshua, Liu, Fine, Amin et al., Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: A propensity score-matched analysis, Am J Hematol, doi:10.1002/ajh.26102
Osborne, COVID-19 contributes to a prothrombotic and hypercoagulable state (8-9). Increased production of interleukins (IL-6, IL-10) and coagulopathy leads to high fatality rates in hospitalized COVID-19 patients. (28-29) Studies have shown systemic anticoagulation's benefits in reducing mortality in mechanically ventilated patients. (30-31
Osborne, Veigulis, Arreola, Mahajan, Röösli et al., Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration, PLoS One, doi:10.1371/journal.pone.0246825
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: an updated guideline for reporting systematic reviews, Bmj, doi:10.1136/bmj.n71
Paranjpe, Fuster, Russak, Glicksberg, Levin, Association of Treatment Dose Anticoagulation With In-Hospital Survival Among Hospitalized Patients With COVID-19, Journal of the American College of Cardiology, doi:10.1016/j.jacc.2020.05.001
Ranucci, Ballotta, Dedda, Bayshnikova, Poli et al., The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome, J Thromb Haemost, doi:10.1111/jth.14854
Recovery Collaborative Group, Horby, Lim, Emberson, Mafham et al., Dexamethasone in Hospitalized Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2021436
Salah, Mehta, Meta-Analysis of the Effect of Aspirin on Mortality in COVID-19, Am J Cardiol, doi:10.1016/j.amjcard.2020.12.073
Savarapu, Baral, Adhikari, Akanbi, Abdelazeem et al., Aspirin Use is Associated with Decreased Mortality in Patients with COVID-19: A Systematic Review and Meta-analysis
Simon, Understanding the odds ratio and the relative risk, J Androl
Srivastava, Kumar, Use of aspirin in reduction of mortality of COVID-19 patients: A meta-analysis, Int J Clin Pract, doi:10.1111/ijcp.14515
Stang, of nonrandomized studies in meta-analyses
Stare, Maucort-Boulch, Odds ratio, hazard ratio and relative risk, Advances in Methodology and Statistics
Statistical, Group, The Cochrane Collaboration's tool for assessing risk of bias in randomised trials, BMJ, doi:10.1136/bmj.d5928
Vahedian-Azimi, Rahimibashar, Najafi, Kidde, Shahriary et al., Associastion of In-hospital Use of Statins, Aspirin, and Renin-Angiotensin-Aldosterone Inhibitors with Mortality and ICU Admission Due to COVID-19, Adv Exp Med Biol, doi:10.1007/978-3-030-71697-4_17
Viecca, Radovanovic, Forleo, Santus, Enhanced platelet inhibition treatment improves hypoxemia in patients with severe Covid-19 and hypercoagulability. A case control, proof of concept study, Pharmacological Research, doi:10.1016/j.phrs.2020.104950
Wang, Li, Gu, Wang, Liu et al., Effect of Antiplatelet Therapy on Acute Respiratory Distress Syndrome and Mortality in Critically Ill Patients: A Meta-Analysis, PloS one, doi:10.1371/journal.pone.0154754
Wijaya, Andhika, Huang, Purwiga, Budiman, The effects of aspirin on the outcome of COVID-19: A systematic review and metaanalysis, Clin Epidemiol Glob Health, doi:10.1016/j.cegh.2021.100883
Yuan, Chen, Li, Chen, Wang et al., Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease, J Cell Mol Med, doi:10.1111/jcmm.16198
Zhang, Yu, What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes, Jama, doi:10.1001/jama.280.19.1690