A systematic review and meta-analysis on efficacy of low dose aspirin on the management of COVID-19
et al., International Journal of Medicine in Developing Countries, doi:10.24911/IJMDC.51-1640383699, Dec 2021
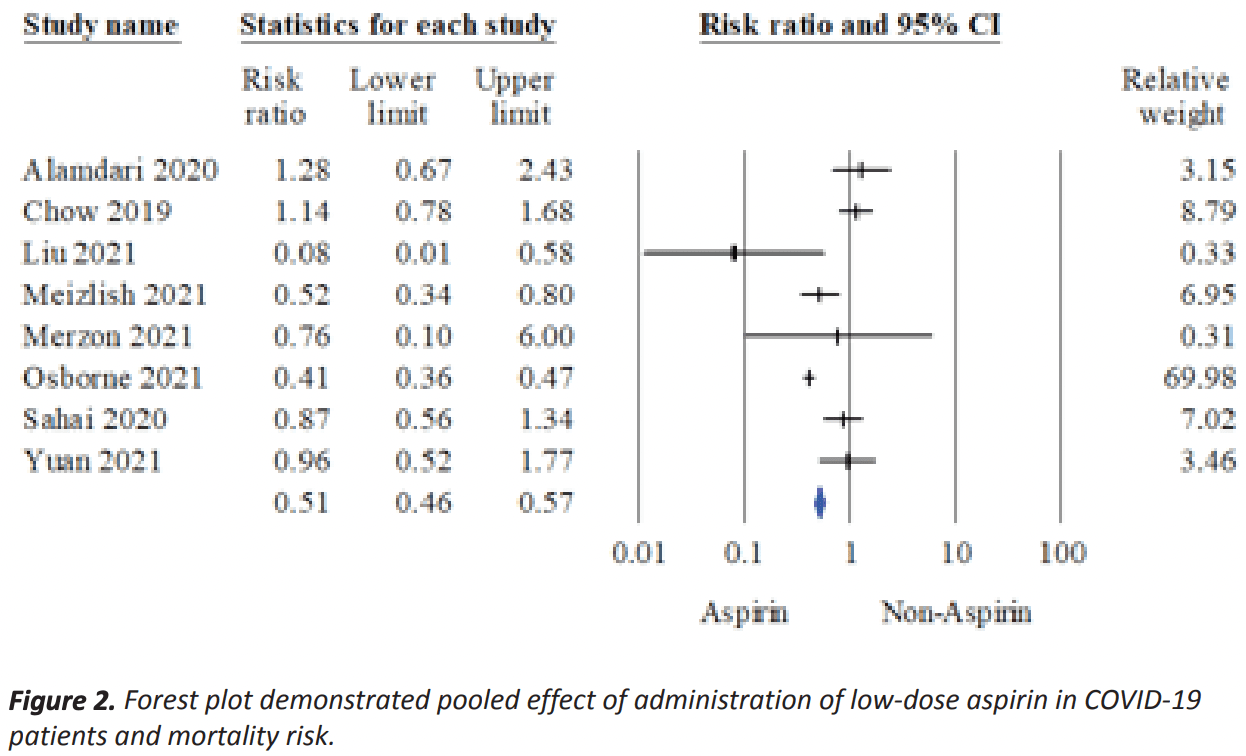
Meta analysis of 8 studies showing significantly lower mortality and mechanical ventilation with low dose aspirin.
4 meta-analyses show significant improvements with aspirin for mortality1-3,
mechanical ventilation1, and
progression4.
Currently there are 79 aspirin for COVID-19 studies, showing 8% lower mortality [2‑14%], 5% lower ventilation [-5‑15%], 3% lower ICU admission [-11‑16%], 1% higher hospitalization [-4‑6%], and 5% fewer cases [-5‑14%].
|
risk of death, 49.0% lower, RR 0.51, p < 0.001.
|
|
risk of mechanical ventilation, 30.0% lower, RR 0.70, p = 0.006.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Banaser et al., A systematic review and meta-analysis on efficacy of low dose aspirin on the management of COVID-19, International Journal of Medicine in Developing Countries, doi:10.24911/IJMDC.51-1640383699.
2.
Srinivasan et al., Aspirin use is associated with decreased inpatient mortality in patients with COVID-19: A meta-analysis, American Heart Journal Plus: Cardiology Research and Practice, doi:10.1016/j.ahjo.2022.100191.
Banaser et al., 24 Dec 2021, peer-reviewed, 5 authors.
A systematic review and meta-analysis on efficacy of low dose aspirin on the management of COVID-19
International Journal of Medicine in Developing Countries, doi:10.24911/ijmdc.51-1640383699
COVID-19 pandemic has increased thrombotic risk by 35%. This pandemic led to millions of deaths due to various comorbidities and organ failure. Repurposing aspirin usage to manage COVID-19 hospitalized patients is a logical approach for preventing cardiovascular disease and comorbidities that increase mortality risk. However, several earlier investigations found inconsistent outcomes. This study aims to assess primary and secondary effects in COVID-19 patients with or without aspirin. We performed a multi-database electronic search including Cochrane, Embase, Scopus, and PubMed from date of inception to November 2021 using search terms: ("Coronavirus Disease 2019" OR "COVID-19" OR "SARS-CoV-2" OR "2019-nCoV") AND ("Acetylsalicylic acid" OR "acetylsalicylate" OR "aspirin" OR "antiplatelet") AND ("mortality" OR "severe" OR "severity"). Eight retrospective studies met the study criteria comprising 7,171 aspirin users and 8,327 non-aspirin users in COVID-19. Aspirin administration significantly reduces mortality risk (RR: 0.51, 95% CI: 0.46-0.57, I 2 = 85.05, p-value <0.001, τ 2 = 0.028, Z-value: -11.44, p-value <0.001). Aspirin used in COVID-19 patients demonstrated reduced bleeding risk (RR: 0.80, 95 CI%: 0.34-1.9) and reduced risk for the necessity of mechanical ventilation (RR: 0.70; 95% CI: 0.54-0.90, I 2 = 0%, p-value: 0.41, τ 2 = 0%) when compared with COVID-19 patients without aspirin use. The present review found administration of a low dose of aspirin in COVID-19 patients significantly reduced mortality risk.
Conflict of interest The authors declare that there is no conflict of interest regarding the publication of this article.
Funding None.
Consent to participate Not applicable.
Ethical approval Not applicable.
Author details Manal Banaser 1 , Mutaman Jarrar
References
Akbar, Pranata, Wibowo, Lim, Sihite et al., The prognostic value of elevated creatine kinase to predict poor outcome in patients with COVID-19 -a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.02.012
Alamdari, Afaghi, Rahimi, Tarki, Tavana et al., Mortality risk factors among hospitalized COVID-19 patients in a major referral center in Iran, Tohoku J Exp Med, doi:10.1620/tjem.252.73
Aly, Ibrahim, Should aspirin be used for prophylaxis of COVID-19-induced coagulopathy?, Med Hypotheses, doi:10.1016/j.mehy.2020.109975
Borenstein, Hedges, Higgins, Rothstein, Comprehensive meta-analysis
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019, Anesth Analg, doi:10.1213/ANE.0000000000005292
Du, Jiang, He, Song, Xu, Antiplatelet therapy for critically Ill patients: a pairwise and bayesian network meta-analysis, Shock, doi:10.1097/SHK.0000000000001057
Egger, Smith, Schneider, Minder, Bias in meta-analysis detected by a simple, graphical test, BMJ, doi:10.1136/bmj.315.7109.629
Han, Yang, Liu, Liu, Wu et al., Prominent changes in blood coagulation of patients with SARS-CoV-2 infection, Clin Chem Lab Med, doi:10.1515/cclm-2020-0188
Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study, Intensive Care Med, doi:10.1007/s00134-020-06062-x
Ho, Dusendang, Schmittdiel, Kavecansky, Tavakoli et al., Association of chronic anticoagulant and antiplatelet use on disease severity in SARS-COV-2 infected patients, J Thromb Thrombolysis, doi:10.1007/s11239-021-02383-w
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res, doi:10.1016/j.thromres.2020.04.013
Liu, Huang, Li, Zhou, Liang et al., Effect of low-dose aspirin on mortality and viral duration of the hospitalized adults with COVID-19, Medicine, doi:10.1097/MD.0000000000024544
Meizlish, Goshua, Liu, Fine, Amin et al., Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity scorematched analysis, Am J Hematol, doi:10.1002/ajh.26102
Merzon, Green, Vinker, Golan-Cohen, Gorohovski et al., The use of aspirin for primary prevention of cardiovascular disease is associated with a lower likelihood of COVID-19 infection, FEBS J, doi:10.1111/febs.15784
Minno, Ambrosino, Calcaterra, Minno, COVID-19 and venous thromboembolism: a meta-analysis of literature studies, Semin Thromb Hemost, doi:10.1055/s-0040-1715456
Moher, Liberati, Tetzlaff, Altman, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, BMJ, doi:10.1136/bmj.b2535
Moher, Liberati, Tetzlaff, Altman, Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement, Int J Surg, doi:10.1016/j.ijsu.2010.02.007
Osborne, Veigulis, Arreola, Mahajan, Röösli et al., Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration, PLoS One, doi:10.1371/journal.pone.0246825
Pranata, Lim, Yonas, Huang, Nasution et al., Thrombocytopenia as a prognostic marker in COVID-19 patients: diagnostic test accuracy meta-analysis, Epidemiol Infect, doi:10.1017/S0950268821000236
Russell, Moss, Rigg, Van Hemelrijck, COVID-19 and treatment with NSAIDs and corticosteroids: should we be limiting their use in the clinical setting? Ecancermedicalscience, doi:10.3332/ecancer.2020.1023
Sahai, Bhandari, Koupenova, Freedman, Godwin et al., SARS-CoV-2 receptors are expressed on human platelets and the effect of aspirin on clinical outcomes in COVID-19 patients, Res Sq, doi:10.21203/rs.3.rs-119031/v1
Salah, Mehta, Meta-analysis of the effect of aspirin on mortality in COVID-19, Am J Cardiol, doi:10.1016/j.amjcard.2020.12.073
Trujillo-Murillo, Rincón-Sánchez, Martínez-Rodríguez, Bosques-Padilla, Ramos-Jiménez et al., Acetylsalicylic acid inhibits hepatitis C virus RNA and protein expression through cyclooxygenase 2 signaling pathways, Hepatology, doi:10.1002/hep.22215
Wang, Li, Gu, Wang, Liu et al., Effect of antiplatelet therapy on acute respiratory distress syndrome and mortality in critically Ill patients: a meta-analysis, PLoS One, doi:10.1371/journal.pone.0154754
Yang, Han, Nilsson-Payant, Gupta, Wang et al., A human pluripotent stem cell-based platform to study SARS-CoV-2 tropism and model virus infection in human cells and organoids, Cell Stem Cell, doi:10.1016/j.stem.2020.06.015
Yuan, Chen, Li, Chen, Wang et al., Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease, J Cell Mol Med, doi:10.1111/jcmm.16198
Zhou, Li, Yang, Antiplatelet therapy after percutaneous coronary intervention in patients with COVID-19, Circulation, doi:10.1161/CIRCULATIONAHA.120.046988
DOI record:
{
"DOI": "10.24911/ijmdc.51-1640383699",
"ISSN": [
"1658-7820"
],
"URL": "http://dx.doi.org/10.24911/ijmdc.51-1640383699",
"author": [
{
"affiliation": [],
"family": "Banaser",
"given": "Manal",
"sequence": "first"
},
{
"affiliation": [],
"family": "Jarrar",
"given": "Mutaman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alqahtani",
"given": "Ayed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Banaser",
"given": "Abdulelah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Albaker",
"given": "Waleed",
"sequence": "additional"
}
],
"container-title": [
"International Journal of Medicine in Developing Countries"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
20
]
],
"date-time": "2022-01-20T21:35:55Z",
"timestamp": 1642714555000
},
"deposited": {
"date-parts": [
[
2022,
1,
31
]
],
"date-time": "2022-01-31T17:56:29Z",
"timestamp": 1643651789000
},
"indexed": {
"date-parts": [
[
2022,
1,
31
]
],
"date-time": "2022-01-31T18:14:26Z",
"timestamp": 1643652866051
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "1658-7820"
}
],
"issued": {
"date-parts": [
[
2022
]
]
},
"license": [
{
"URL": "http://https://www.ijmdc.com/?sec=licenseinfo",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
1
]
],
"date-time": "2022-01-01T00:00:00Z",
"timestamp": 1640995200000
}
}
],
"link": [
{
"URL": "https://www.ejmanager.com/fulltextpdf.php?mno=117130",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10538",
"original-title": [],
"page": "526-534",
"prefix": "10.24911",
"published": {
"date-parts": [
[
2022
]
]
},
"published-online": {
"date-parts": [
[
2022
]
]
},
"publisher": "Discover STM Publishing Ltd.",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [
"IJMDC"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Earth and Planetary Sciences",
"General Environmental Science"
],
"subtitle": [],
"title": [
"A systematic review and meta-analysis on efficacy of low dose aspirin on the management of COVID-19"
],
"type": "journal-article"
}