Zinc against COVID-19? Symptom surveillance and deficiency risk groups
et al., PLOS Neglected Tropical Diseases, doi:10.1371/journal.pntd.0008895, Jan 2021
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
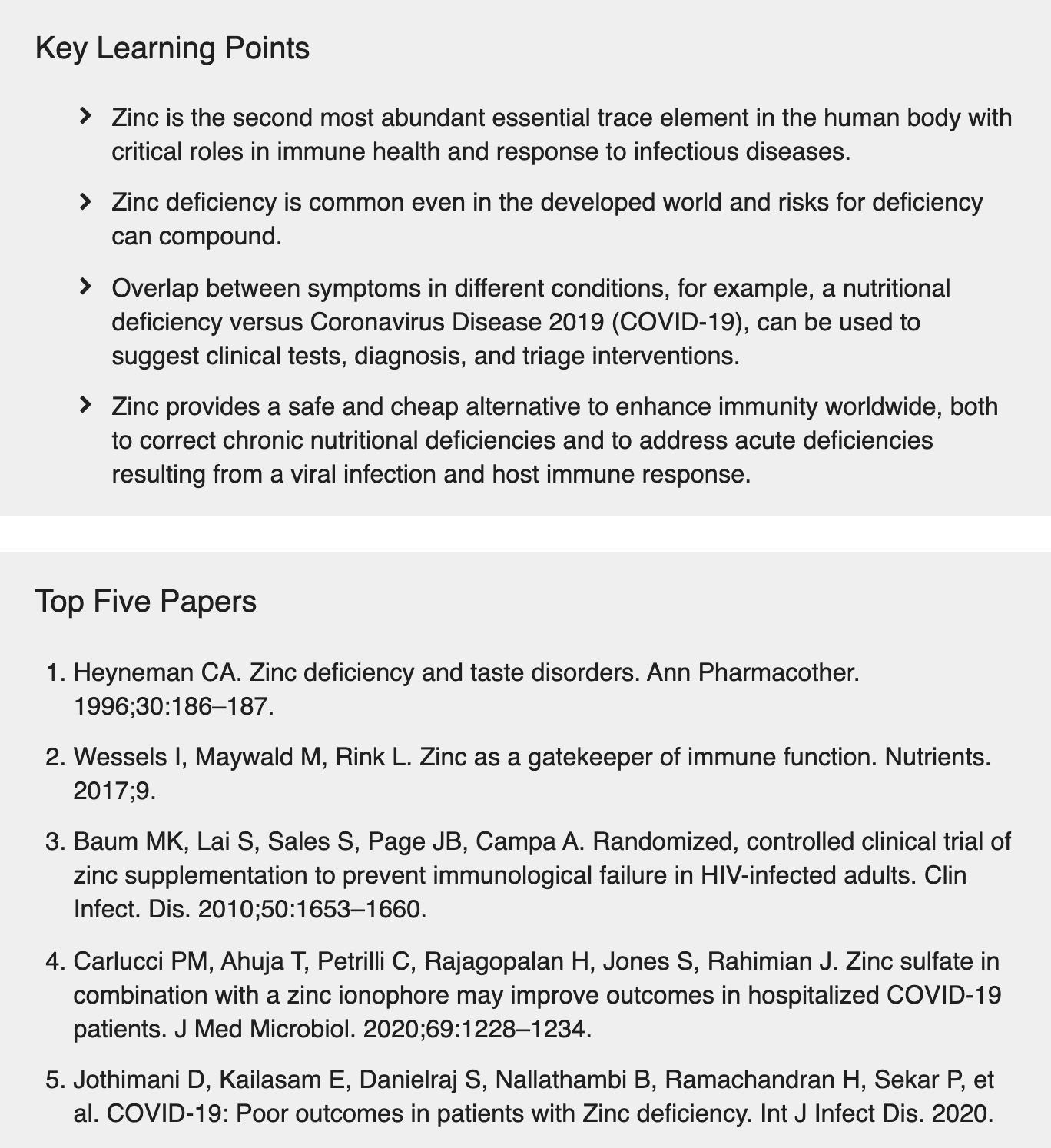
Literature review concluding that zinc should be included as part of preventative supplementation for COVID-19, in general for support of immune health, and should also be considered in the context of zinc deficiency acquired during a viral infection and host immune response.
1.
Smail et al., Antioxidant and oxidative enzymes, genetic variants, and cofactors as prognostic biomarkers of COVID-19 severity and mortality: a systematic review, Frontiers in Molecular Biosciences, doi:10.3389/fmolb.2025.1700263.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Fazli et al., Possible Link between Gut Microbiota, Diet, and COVID-19 Infection, Journal of Medical Bacteriology, 12:4, jmb.tums.ac.ir/index.php/jmb/article/view/525.
4.
Mu et al., Anti-inflammatory and Nutritional Interventions Against SARS-CoV-2: A Comprehensive Review, Journal of Agriculture and Food Research, doi:10.1016/j.jafr.2024.101422.
5.
Jin et al., The nutritional roles of zinc for immune system and COVID-19 patients, Frontiers in Nutrition, doi:10.3389/fnut.2024.1385591.
6.
Briassoulis et al., The Anti-Oxidative, Anti-Inflammatory, Anti-Apoptotic, and Anti-Necroptotic Role of Zinc in COVID-19 and Sepsis, Antioxidants, doi:10.3390/antiox12111942.
7.
Winn et al., Effect of any form of steroids in comparison with that of other medications on the duration of olfactory dysfunction in patients with COVID-19: A systematic review of randomized trials and quasi-experimental studies, PLOS ONE, doi:10.1371/journal.pone.0288285.
8.
Schloss et al., Nutritional deficiencies that may predispose to long COVID, Inflammopharmacology, doi:10.1007/s10787-023-01183-3.
9.
Arora et al., Global Dietary and Herbal Supplement Use during COVID-19—A Scoping Review, Nutrients, doi:10.3390/nu15030771.
10.
Wang et al., Zinc and COVID-19: Immunity, Susceptibility, Severity and Intervention, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2022.2119932.
11.
Foshati et al., Antioxidants and clinical outcomes of patients with coronavirus disease 2019: A systematic review of observational and interventional studies, Food Science & Nutrition, doi:10.1002/fsn3.3034.
12.
DiGuilio et al., Micronutrient Improvement of Epithelial Barrier Function in Various Disease States: A Case for Adjuvant Therapy, International Journal of Molecular Sciences, doi:10.3390/ijms23062995.
13.
Wessels et al., Zinc deficiency as a possible risk factor for increased susceptibility and severe progression of Corona Virus Disease 19, British Journal of Nutrition, doi:10.1017/S0007114521000738.
14.
Sethuram et al., Potential Role of Zinc in the COVID-19 Disease Process and its Probable Impact on Reproduction, Reproductive Sciences, doi:10.1007/s43032-020-00400-6.
15.
Joachimiak et al., Zinc against COVID-19? Symptom surveillance and deficiency risk groups, PLOS Neglected Tropical Diseases, doi:10.1371/journal.pntd.0008895.
Joachimiak et al., 4 Jan 2021, peer-reviewed, 1 author.
Zinc against COVID-19? Symptom surveillance and deficiency risk groups
PLOS Neglected Tropical Diseases, doi:10.1371/journal.pntd.0008895
A wide variety of symptoms is associated with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, and these symptoms can overlap with other conditions and diseases. Knowing the distribution of symptoms across diseases and individuals can support clinical actions on timelines shorter than those for drug and vaccine development. Here, we focus on zinc deficiency symptoms, symptom overlap with other conditions, as well as zinc effects on immune health and mechanistic zinc deficiency risk groups. There are wellstudied beneficial effects of zinc on the immune system including a decreased susceptibility to and improved clinical outcomes for infectious pathogens including multiple viruses. Zinc is also an anti-inflammatory and anti-oxidative stress agent, relevant to some severe Coronavirus Disease 2019 (COVID-19) symptoms. Unfortunately, zinc deficiency is common worldwide and not exclusive to the developing world. Lifestyle choices and preexisting conditions alone can result in zinc deficiency, and we compile zinc risk groups based on a review of the literature. It is also important to distinguish chronic zinc deficiency from deficiency acquired upon viral infection and immune response and their different supplementation strategies. Zinc is being considered as prophylactic or adjunct therapy for COVID-19, with 12 clinical trials underway, highlighting the relevance of this trace element for global pandemics. Using the example of zinc, we show that there is a critical need for a deeper understanding of essential trace elements in human health, and the resulting deficiency symptoms and their overlap with other conditions. This knowledge will directly support human immune health for decreasing susceptibility, shortening illness duration, and preventing progression to severe cases in the current and future pandemics.
References
Adams, Baker, Sobieraj, Myth Busters: Dietary Supplements and COVID-19, Ann Pharmacother, doi:10.1177/1060028020928052
Ahangar, Naderi, Noroozi, Ghasemi, Zamani et al., Zinc Deficiency and Oxidative Stress Involved in Valproic Acid Induced Hepatotoxicity: Protection by Zinc and Selenium Supplementation, Biol Trace Elem Res, doi:10.1007/s12011-017-0944-z
Alexander, Davidson, Intranasal Zinc and Anosmia: The Zinc-Induced Anosmia Syndrome, Laryngoscope, doi:10.1097/01.mlg.0000191549.17796.13
Alschuler, Weil, Horwitz, Stamets, Chiasson et al., Integrative considerations during the COVID-19 pandemic, Explore, doi:10.1016/j.explore.2020.03.007
Amin, Fs, Toxicological and safety assessment of tartrazine as a synthetic food additive on health biomarkers: A review, Afr J Biotechnol
Andersen, Rambaut, Lipkin, Holmes, Garry, The proximal origin of SARS-CoV-2, Nat Med, doi:10.1038/s41591-020-0820-9
Anderson, Heesterbeek, Klinkenberg, Hollingsworth, How will country-based mitigation measures influence the course of the COVID-19 epidemic?, Lancet, doi:10.1016/S0140-6736%2820%2930567-5
Andreini, Banci, Bertini, Rosato, Counting the zinc-proteins encoded in the human genome, J Proteome Res, doi:10.1021/pr050361j
Arunachalam, Wimmers, Mok, Perera, Scott et al., Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans, Science, doi:10.1126/science.abc6261
Atkin-Thor, Goddard, 'nion, Stephen, Kolff, Hypogeusia and zinc depletion in chronic dialysis patients, Am J Clin Nutr, doi:10.1093/ajcn/31.10.1948
Bar-On, Flamholz, Phillips, SARS-CoV-2 (COVID-19) by the numbers, doi:10.7554/eLife.57309
Barnett, Hamer, Meydani, Low zinc status: a new risk factor for pneumonia in the elderly?, Nutr Rev, doi:10.1111/j.1753-4887.2009.00253.x
Barve, Chen, Kirpich, Watson, Mcclain, Development, Prevention, and Treatment of Alcohol-Induced Organ Injury: The Role of Nutrition, Alcohol Res
Basnet, Shrestha, Sharma, Mathisen, Prasai et al., A randomized controlled trial of zinc as adjuvant therapy for severe pneumonia in young children, Pediatrics, doi:10.1542/peds.2010-3091
Baum, Lai, Sales, Page, Campa, Randomized, controlled clinical trial of zinc supplementation to prevent immunological failure in HIV-infected adults, Clin Infect Dis, doi:10.1086/652864
Bhandari, Bahl, Taneja, Strand, Mølbak et al., Effect of routine zinc supplementation on pneumonia in children aged 6 months to 3 years: randomised controlled trial in an urban slum, BMJ, doi:10.1136/bmj.324.7350.1358
Bo, Lezo, Menato, Gallo, Bardelli et al., Gestational hyperglycemia, zinc, selenium, and antioxidant vitamins, Nutrition, doi:10.1016/j.nut.2004.05.022
Bose, Coles, Gunavathi, John, Moses et al., Efficacy of zinc in the treatment of severe pneumonia in hospitalized children <2 y old, Am J Clin Nutr, doi:10.1093/ajcn/83.5.1089
Brann, Tsukahara, Weinreb, Lipovsek, Van Den Berge et al., Non-neuronal expression of SARS-CoV-2 entry genes in the olfaory system suggests mechanisms underlying COVID-19-associated anosmia, Sci Adv, doi:10.1126/sciadv.abc5801
Braun, Rosenfeldt, Pharmaco-nutrient interactions-a systematic review of zinc and antihypertensive therapy, Int J Clin Pract, doi:10.1111/ijcp.12040
Brooks, Yunus, Santosham, Wahed, Nahar et al., Zinc for severe pneumonia in very young children: double-blind placebo-controlled trial, Lancet, doi:10.1016/S0140-6736%2804%2916252-1
Brown, Hess, Vosti, Baker, Comparison of the Estimated Cost-Effectiveness of Preventive and Therapeutic Zinc Supplementation Strategies for Reducing Child Morbidity and Mortality in Sub-Saharan Africa, Food Nutr Bull, doi:10.1177/156482651303400209
Butowt, Bilinska, SARS-CoV-2: Olfaction, Brain Infection, and the Urgent Need for Clinical Samples Allowing Earlier Virus Detection, ACS Chem Neurosci, doi:10.1021/acschemneuro.0c00172
Ca ´rcamo, Hooton, Weiss, Gilman, Wener et al., Brief Report: Randomized Controlled Trial of Zinc Supplementation for Persistent Diarrhea in Adults With HIV-1 Infection, JAIDS Journal of Acquired Immune Deficiency Syndromes, doi:10.1097/01.qai.0000242446.44285.b5
Calder, Carr, Gombart, Eggersdorfer, Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections, Nutrients, doi:10.3390/nu12041181
Carlucci, Ahuja, Petrilli, Rajagopalan, Jones et al., Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients, J Med Microbiol, doi:10.1099/jmm.0.001250
Cascella, Rajnik, Cuomo, Dulebohn, Napoli, Features, Evaluation and Treatment Coronavirus (COVID-19)
Caulfield, Zavaleta, Shankar, Merialdi, Potential contribution of maternal zinc supplementation during pregnancy to maternal and child survival, Am J Clin Nutr, doi:10.1093/ajcn/68.2.499S
Chasapis, Loutsidou, Spiliopoulou, Stefanidou, Zinc and human health: an update, Arch Toxicol, doi:10.1007/s00204-011-0775-1
Chen, Lee, Yan, Kim, Wei et al., BioConceptVec: Creating and evaluating literaturebased biomedical concept embeddings on a large scale, PLoS Comput Biol, doi:10.1371/journal.pcbi.1007617
Chen, Qi, Liu, Ling, Qian et al., Clinical progression of patients with COVID-19 in Shanghai, China J Infect, doi:10.1016/j.jinf.2020.03.004
Cheng, Lau, Woo, Yuen, Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection, Clin Microbiol Rev, doi:10.1128/CMR.00023-07
Costarelli, Muti, Malavolta, Cipriano, Giacconi et al., Distinctive modulation of inflammatory and metabolic parameters in relation to zinc nutritional status in adult overweight/obese subjects, J Nutr Biochem, doi:10.1016/j.jnutbio.2009.02.001
Craddock, Neale, Peoples, Probst, Vegetarian-Based Dietary Patterns and their Relation with Inflammatory and Immune Biomarkers: A Systematic Review and Meta-Analysis, Adv Nutr, doi:10.1093/advances/nmy103
D'arienzo, Conigliob, Assessment of the SARS-CoV-2 basic reproduction number, R 0 , based on the early phase of COVID-19 outbreak in Italy, Biosafety and Health, doi:10.1016/j.bsheal.2020.03.004
Da Silva, Hiller, Gai, Kullak-Ublick, Vitamin D3 transactivates the zinc and manganese transporter SLC30A10 via the Vitamin D receptor, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2016.04.006
Damianaki, Lourenco, Braconnier, Ghobril, Devuyst et al., Renal handling of zinc in chronic kidney disease patients and the role of circulating zinc levels in renal function decline, Nephrol Dial Transplant, doi:10.1093/ndt/gfz065
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients, doi:10.1101/2020.04.08.20058578
Davidson, Smith, The Bradford Hill criteria and zinc-induced anosmia: a causality analysis, Arch Otolaryngol Head Neck Surg, doi:10.1001/archoto.2010.111
Day, Covid-19: four fifths of cases are asymptomatic. China figures indicate, BMJ, doi:10.1136/bmj.m1375
Day, Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village, BMJ, doi:10.1136/bmj.m1165
De Faria, Corgosinho, Sanches, Prado, Laviano et al., Dietary recommendations during the COVID-19 pandemic, Nutr Rev, doi:10.1093/nutrit/nuaa067
Decook, Hirsch, Anosmia due to inhalational zinc: a case report, Chem Senses
Derwand, Scholz, Does zinc supplementation enhance the clinical efficacy of chloroquine/hydroxychloroquine to win todays battle against COVID-19?, Med Hypotheses
Du, Liang, Yang, Cao, Li, Predictors of Mortality for Patients with COVID-19 Pneumonia Caused by SARS-CoV-2: A Prospective Cohort Study, Eur Respir J, doi:10.1183/13993003.00524-2020
Dutta, Procaccino, Aamodt, Zinc Metabolism in Patients with Exocrine Pancreatic Insufficiency, J Am Coll Nutr, doi:10.1080/07315724.1998.10718803
Ekholm, Virkki, Ylinen, Johansson, The effect of phytic acid and some natural chelating agents on the solubility of mineral elements in oat bran, Food Chem
Elbaz, Zahra, Hanafy, Magnesium, zinc and copper estimation in children with attention deficit hyperactivity disorder (ADHD), Egyptian Journal of Medical Human Genetics
Eliezer, Hautefort, Hamel, Verillaud, Herman et al., Sudden and Complete Olfactory Loss Function as a Possible Symptom of COVID-19, JAMA Otolaryngol Head Neck Surg, doi:10.1001/jamaoto.2020.0832
Emami, Javanmardi, Pirbonyeh, Akbari, Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis, Arch Acad Emerg Med
Fairweather-Tait, Harvey, Ford, Does ageing affect zinc homeostasis and dietary requirements?, Exp Gerontol, doi:10.1016/j.exger.2007.10.015
Farooq, Alamri, Alwhahabi, Metwally, Kareem, The status of zinc in type 2 diabetic patients and its association with glycemic control, J Family Community Med, doi:10.4103/jfcm.JFCM%5F113%5F19
Finzi, Treatment of SARS-CoV-2 with high dose oral zinc salts: A report on four patients, Int J Infect Dis, doi:10.1016/j.ijid.2020.06.006
Fischer, Giroux, 'abbe, The effect of dietary zinc on intestinal copper absorption, Am J Clin Nutr, doi:10.1093/ajcn/34.9.1670
Furrer, Jancso, Colic, Rinaldi, OGER++: hybrid multi-type entity recognition, J Cheminform, doi:10.1186/s13321-018-0326-3
Gammoh, Rink, Zinc and the Immune System, Nutrition and Immunity, doi:10.1007/978-3-030-16073-9%5F8
Giacomelli, Pezzati, Conti, Bernacchia, Siano et al., Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study, Clin Infect Dis, doi:10.1093/cid/ciaa330
Gray, Dhana, Stein, Khumalo, Zinc and atopic dermatitis: a systematic review and metaanalysis, J Eur Acad Dermatol Venereol, doi:10.1111/jdv.15524
Green, Lewin, Wightman, Lee, Ravindran et al., A randomised controlled trial of oral zinc on the immune response to tuberculosis in HIV-infected patients, Int J Tuberc Lung Dis
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Haase, An Element of Life: Competition for Zinc in Host-Pathogen Interaction, Immunity, doi:10.1016/j.immuni.2013.09.009
Haase, Mocchegiani, Rink, Correlation between zinc status and immune function in the elderly, Biogerontology, doi:10.1007/s10522-006-9057-3
Haase, Rink, Zinc and Immunity. Encyclopedia of Metalloproteins, doi:10.1007/978-1-4614-1533-6
Hartman, Hess, Connor, Prolonged viral RNA shedding after COVID-19 symptom resolution in older convalescent plasma donors, doi:10.1101/2020.05.07.20090621
Hendricks, Walker, Zinc deficiency in inflammatory bowel disease, Nutr Rev, doi:10.1111/j.1753-4887.1988.tb05381.x
Henkin, Schecter, Friedewald, Demets, Raff, A double blind study of the effects of zinc sulfate on taste and smell dysfunction, Am J Med Sci, doi:10.1097/00000441-197611000-00006
Herna ´ndez-Camacho, ´a, Parsons, Navas-Enamorado, Zinc at the crossroads of exercise and proteostasis, Redox Biol, doi:10.1016/j.redox.2020.101529
Heyneman, Zinc deficiency and taste disorders, Ann Pharmacother, doi:10.1177/106002809603000215
Himoto, Masaki, Associations between Zinc Deficiency and Metabolic Abnormalities in Patients with Chronic Liver Disease, Nutrients, doi:10.3390/nu10010088
Hirano, Murakami, Fukada, Nishida, Yamasaki et al., Roles of Zinc and Zinc Signaling in Immunity: Zinc as an Intracellular Signaling Molecule, Adv Immunol, doi:10.1016/S0065-2776%2808%2900003-5
Howie, Bottomley, Chimah, Ideh, Ebruke et al., Zinc as an adjunct therapy in the management of severe pneumonia among Gambian children: randomized controlled trial, J Glob Health, doi:10.7189/jogh.08.010418
Ibs, Rink, Zinc-altered immune function, J Nutr, doi:10.1093/jn/133.5.1452S
Jafek, Linschoten, Murrow, Anosmia after intranasal zinc gluconate use, Am J Rhinol
Jayawardena, Sooriyaarachchi, Chourdakis, Jeewandara, Ranasinghe, Enhancing immunity in viral infections, with special emphasis on COVID-19: A review, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.015
Jeejeebhoy, Zinc: an essential trace element for parenteral nutrition, Gastroenterology, doi:10.1053/j.gastro.2009.08.014
Jordan, Adab, Cheng, Covid-19: risk factors for severe disease and death, BMJ, doi:10.1136/bmj.m1198
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with Zinc deficiency, Int J Infect Dis, doi:10.1016/j.ijid.2020.09.014
Kambhampati, Vaishya, Vaish, Unprecedented surge in publications related to COVID-19 in the first three months of pandemic: A bibliometric analytic report, J Clin Orthop Trauma, doi:10.1016/j.jcot.2020.04.030
Katz, Keen, Litt, Hurley, Kellams-Harrison et al., Zinc deficiency in anorexia nervosa, J Adolesc Health Care, doi:10.1016/0197-0070%2887%2990227-0
King, Brown, Gibson, Krebs, Lowe et al., Biomarkers of Nutrition for Development (BOND)-Zinc Review, J Nutr, doi:10.3945/jn.115.220079
Kloubert, Rink, Zinc Regulation of the Immune Response, Nutrition, Immunity, and Infection, doi:10.1201/9781315118901-15
Kolenko, Uzzo, Dulin, Hauzman, Bukowski et al., Mechanism of apoptosis induced by zinc deficiency in peripheral blood T lymphocytes, Apoptosis, doi:10.1023/a%3A1012497926537
Krebs, Update on zinc deficiency and excess in clinical pediatric practice, Ann Nutr Metab, doi:10.1159/000348261
Kumssa, Joy, Ander, Watts, Young et al., Dietary calcium and zinc deficiency risks are decreasing but remain prevalent, Sci Rep, doi:10.1038/srep10974
Kwong, Aubrey, Godoy, Is Loss Of Smell And Taste A Symptom Of COVID-19? Doctors Want To Find Out
Lao, Imam, Nguyen, Anosmia, hyposmia, and dysgeusia as indicators for positive SARS-CoV-2 infection, World J Otorhinolaryngol Head Neck Surg, doi:10.1016/j.wjorl.2020.04.001
Lauer, Grantz, Bi, Jones, Zheng et al., The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application, Ann Intern Med, doi:10.7326/M20-0504
Lechien, Chiesa-Estomba, Hans, Barillari, Jouffe et al., Loss of Smell and Taste in 2013 European Patients With Mild to Moderate COVID-19, Ann Intern Med, doi:10.7326/M20-2428
Lee, Choi, Hong, Kim, Lee et al., The cancer chemotherapeutic agent paclitaxel (Taxol) reduces hippocampal neurogenesis via down-regulation of vesicular zinc, Sci Rep, doi:10.1038/s41598-017-12054-7
Liu, Ga ´lvez-Peralta, Pyle, Rudawsky, Pavlovicz, ZIP8 regulates host defense through zinc-mediated inhibition of NF-κB, Cell Rep, doi:10.1016/j.celrep.2013.01.009
Lo, Dietary factors influencing zinc absorption, J Nutr, doi:10.1093/jn/130.5.1378S
Lyckholm, Heddinger, Parker, Coyne, Ramakrishnan et al., A randomized, placebo controlled trial of oral zinc for chemotherapy-related taste and smell disorders, J Pain Palliat Care Pharmacother, doi:10.3109/15360288.2012.676618
Maares, Haase, Zinc and immunity: An essential interrelation, Arch Biochem Biophys, doi:10.1016/j.abb.2016.03.022
Machado, Gutierrez, Anosmia and Ageusia as Initial or Unique Symptoms after SARS-COV-2 Virus Infection, Medicine & Pharmacology, doi:10.20944/preprints202004.0272.v1
Maheswaran, Abikshyeet, Sitra, Gokulanathan, Vaithiyanadane et al., Gustatory dysfunction, J Pharm Bioallied Sci, doi:10.4103/0975-7406.137257
Malaty, Malaty, Smell and taste disorders in primary care, Am Fam Physician
Mao, Liang, Shen, Ghosh, Zhu et al., Implications of COVID-19 for patients with pre-existing digestive diseases, Lancet Gastroenterol Hepatol, doi:10.1016/S2468-1253%2820%2930076-5
Marreiro D Do, Cruz, Morais, Beserra, Severo et al., Zinc and Oxidative Stress: Current Mechanisms, Antioxidants, doi:10.3390/antiox6020024
Maverakis, Fung, Lynch, Draznin, Michael et al., Acrodermatitis enteropathica and an overview of zinc metabolism, J Am Acad Dermatol, doi:10.1016/j.jaad.2006.08.015
Melissa, Christopher, Kenneth, The National COVID Cohort Collaborative (N3C): Rationale, Design, Infrastructure, and Deployment, J Am Med Inform Assoc, doi:10.1093/jamia/ocaa196
Menni, Valdes, Freydin, Ganesh, Moustafa et al., Loss of smell and taste in combination with other symptoms is a strong predictor of COVID-19 infection, Epidemiology medRxiv, doi:10.1101/2020.04.05.20048421
Meydani, Barnett, Dallal, Fine, Jacques et al., Serum zinc and pneumonia in nursing home elderly, Am J Clin Nutr, doi:10.1093/ajcn/86.4.1167
Mocchegiani, Romeo, Malavolta, Costarelli, Giacconi et al., Zinc: dietary intake and impact of supplementation on immune function in elderly, Age, doi:10.1007/s11357-011-9377-3
Neubauerova, Tulinska, Kuricova, Liskova, Volkovova et al., The Effect of Vegetarian Diet on Immune Response, Epidemiology, doi:10.1097/01.ede.0000289012.66211.45
Nishiura, Kobayashi, Suzuki, Jung, Hayashi et al., Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19), Int J Infect Dis, doi:10.1016/j.jebdp.2020.101499
Offit, The Vitamin Myth: Why We Think We Need Supplements
Olechnowicz, Tinkov, Skalny, Suliburska, Zinc status is associated with inflammation, oxidative stress, lipid, and glucose metabolism, J Physiol Sci, doi:10.1007/s12576-017-0571-7
Pisano, Hilas, Zinc and Taste Disturbances in Older Adults: A Review of the Literature, Consult Pharm, doi:10.4140/TCP.n.2016.267
Prasad, Impact of the discovery of human zinc deficiency on health, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2014.09.002
Prasad, Zinc and Immunity, Biochemistry of Zinc, doi:10.1007/978-1-4757-9444-1
Prasad, Zinc deficiency in patients with sickle cell disease, Am J Clin Nutr, doi:10.1093/ajcn/75.2.181
Prasad, Zinc is an Antioxidant and Anti-Inflammatory Agent: Its Role in Human Health, Front Nutr, doi:10.3389/fnut.2014.00014
Prates, Garvin, Pavicic, Jones, Shah et al., Confronting the COVID-19 Pandemic with Systems Biology, doi:10.1101/2020.04.06.028712
Qasemzadeh, Fathi, Tashvighi, Gharehbeglou, Yadollah-Damavandi et al., The effect of adjuvant zinc therapy on recovery from pneumonia in hospitalized children: a double-blind randomized controlled trial, Scientifica, doi:10.1155/2014/694193
Rahman, Idid, Can Zn Be a Critical Element in COVID-19 Treatment?, Biol Trace Elem Res, doi:10.1007/s12011-020-02194-9
Rahman, Potential benefits of combination of Nigella sativa and Zn supplements to treat COVID-19, Journal of Herbal Medicine, doi:10.1016/j.hermed.2020.100382
Remy, Mazer, Striker, Ellebedy, Walton et al., Severe immunosuppression and not a cytokine storm characterize COVID-19 infections, JCI Insight, doi:10.1172/jci.insight.140329
Ripamonti, Zecca, Brunelli, Fulfaro, Villa et al., A randomized, controlled clinical trial to evaluate the effects of zinc sulfate on cancer patients with taste alterations caused by head and neck irradiation, Cancer, doi:10.1002/%28sici%291097-0142%2819980515%2982%3A10%26lt%3B1938%3A%3Aaid-cncr18%26gt%3B3.0.co%3B2-u
Rodriguez, Cao, Rickenbacher, Benz, Magdamo et al., Innate immune signaling in the olfactory epithelium reduces odorant receptor levels: modeling transient smell loss in COVID-19 patients, medRxiv, doi:10.1101/2020.06.14.20131128
Russell, Moss, George, Santaolalla, Cope et al., Associations between immunesuppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence, doi:10.3332/ecancer.2020.1022
Sanche, Lin, Xu, Romero-Severson, Hengartner et al., High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2, Emerg Infect Dis, doi:10.3201/eid2607.200282
Sandstead, Freeland-Graves, Dietary phytate, zinc and hidden zinc deficiency, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2014.08.011
Shah, Dutta, Shah, Mishra, Role of zinc in severe pneumonia: a randomized double bind placebo controlled study, Ital J Pediatr, doi:10.1186/1824-7288-38-36
Shankar, Prasad, Zinc and immune function: the biological basis of altered resistance to infection, Am J Clin Nutr, doi:10.1093/ajcn/68.2.447S
Sharafi, Allami, Efficacy of zinc sulphate on in-hospital outcome of community-acquired pneumonia in people aged 50 years and over, Int J Tuberc Lung Dis, doi:10.5588/ijtld.15.0653
Shetty, Zinc deficiency and infections, Nutrition, immunity and infection, doi:10.1079/9780851995311.0101
Shi, Qin, Shen, Cai, Liu et al., Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China JAMA Cardiol, doi:10.1001/jamacardio.2020.0950
Singh, Das, Zinc for the common cold, Cochrane Database Syst Rev, doi:10.1002/14651858.CD001364.pub4
Skalny, Rink, Ajsuvakova, Aschner, Gritsenko et al., Zinc and respiratory tract infections: Perspectives for COVID-19 (Review), Int J Mol Med, doi:10.3892/ijmm.2020.4575
Sudre, Lee, Lochlainn, Varsavsky, Murray et al., Symptom clusters in Covid19: A potential clinical prediction tool from the COVID Symptom study app, doi:10.1101/2020.06.12.20129056v1?rss=1%22
Takagi, Nagamine, Abe, Takayama, Sato et al., Zinc supplementation enhances the response to interferon therapy in patients with chronic hepatitis C, J Viral Hepat, doi:10.1046/j.1365-2893.2001.00311.x
Tan, Ho, Kalimuddin, Cherng, Teh et al., A cohort study to evaluate the effect of combination Vitamin D, Magnesium and Vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients, doi:10.1016/j.nut.2020.111017
Tisdall, Brown, Defries, Persistent anosmia following zinc sulfate nasal spraying, J Pediatr
Van Biervliet, Ku ¨ry, Bruyne, Vanakker, Schmitt et al., Clinical zinc deficiency as early presentation of Wilson disease, J Pediatr Gastroenterol Nutr, doi:10.1097/MPG.0000000000000628
Velthuis, Van Den Worm, She, Sims, Baric et al., Zn2 Inhibits Coronavirus and Arterivirus RNA Polymerase Activity In Vitro and Zinc Ionophores Block the Replication of These Viruses in Cell Culture, PLoS Pathog, doi:10.1371/journal.ppat.1001176
Ward, Soulsbury, Zettel, Colquhoun, Bunday et al., The Influence of the Chemical Additive Tartrazine on the Zinc Status of Hyperactive Children-a Double-blind Placebo-controlled Study, Journal of Nutritional Medicine, doi:10.3109/13590849009003134
Wessells, Brown, Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting, PLoS One, doi:10.1371/journal.pone.0050568
Wessels, Maywald, Rink, Zinc as a Gatekeeper of Immune Function, Nutrients, doi:10.3390/nu9121286
Wieringa, Dijkhuizen, Fiorentino, Laillou, Berger, Determination of zinc status in humans: which indicator should we use?, Nutrients, doi:10.3390/nu7053252
Wilder, The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States, Clin Infect Dis, doi:10.1093/cid/ciaa959
Wong, Rinaldi, Ho, Zinc deficiency enhanced inflammatory response by increasing immune cell activation and inducing IL6 promoter demethylation, Mol Nutr Food Res, doi:10.1002/mnfr.201400761
Wu, Chen, Cai, Jia'an, Zhou et al., Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China, JAMA Intern Med, doi:10.1001/jamainternmed.2020.0994
Xue, Moyer, Peng, Wu, Hannafon et al., Chloroquine Is a Zinc Ionophore, PLoS One
Yagi, Asakawa, Ueda, Ikeda, Miyawaki et al., The role of zinc in the treatment of taste disorders, Recent Pat Food Nutr Agric, doi:10.2174/2212798411305010007
Yang, Lawless, Descriptive analysis of divalent salts, J Sens Stud, doi:10.1111/j.1745-459X.2005.00005.x
Ye, Yuan, Yuen, Fung, Chan, Zoonotic origins of human coronaviruses, Int J Biol Sci, doi:10.7150/ijbs.45472
Zeng, Zhang, Efficacy and safety of zinc supplementation for adults, children and pregnant women with HIV infection: systematic review, Tropical Med Int Health, doi:10.1111/j.1365-3156.2011.02871.x
Zhang, Liu, Potential interventions for novel coronavirus in China: A systematic review, J Med Virol, doi:10.1002/jmv.25707
Zhang, Xie, Hashimoto, Current status of potential therapeutic candidates for the COVID-19 crisis, Brain Behav Immun, doi:10.1016/j.bbi.2020.04.046
Zinc, Health, and Immunity, Metabolic Medicine and Surgery, doi:10.1201/b17616-37
Zumla, Hui, Azhar, Memish, Maeurer, Reducing mortality from 2019-nCoV: hostdirected therapies should be an option, Lancet, doi:10.1016/S0140-6736%2820%2930305-6
DOI record:
{
"DOI": "10.1371/journal.pntd.0008895",
"ISSN": [
"1935-2735"
],
"URL": "http://dx.doi.org/10.1371/journal.pntd.0008895",
"abstract": "<jats:p>A wide variety of symptoms is associated with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, and these symptoms can overlap with other conditions and diseases. Knowing the distribution of symptoms across diseases and individuals can support clinical actions on timelines shorter than those for drug and vaccine development. Here, we focus on zinc deficiency symptoms, symptom overlap with other conditions, as well as zinc effects on immune health and mechanistic zinc deficiency risk groups. There are well-studied beneficial effects of zinc on the immune system including a decreased susceptibility to and improved clinical outcomes for infectious pathogens including multiple viruses. Zinc is also an anti-inflammatory and anti-oxidative stress agent, relevant to some severe Coronavirus Disease 2019 (COVID-19) symptoms. Unfortunately, zinc deficiency is common worldwide and not exclusive to the developing world. Lifestyle choices and preexisting conditions alone can result in zinc deficiency, and we compile zinc risk groups based on a review of the literature. It is also important to distinguish chronic zinc deficiency from deficiency acquired upon viral infection and immune response and their different supplementation strategies. Zinc is being considered as prophylactic or adjunct therapy for COVID-19, with 12 clinical trials underway, highlighting the relevance of this trace element for global pandemics. Using the example of zinc, we show that there is a critical need for a deeper understanding of essential trace elements in human health, and the resulting deficiency symptoms and their overlap with other conditions. This knowledge will directly support human immune health for decreasing susceptibility, shortening illness duration, and preventing progression to severe cases in the current and future pandemics.</jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-8175-045X",
"affiliation": [],
"authenticated-orcid": true,
"family": "Joachimiak",
"given": "Marcin P.",
"sequence": "first"
}
],
"container-title": "PLOS Neglected Tropical Diseases",
"container-title-short": "PLoS Negl Trop Dis",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosntds.org"
]
},
"created": {
"date-parts": [
[
2021,
1,
4
]
],
"date-time": "2021-01-04T18:28:15Z",
"timestamp": 1609784895000
},
"deposited": {
"date-parts": [
[
2023,
10,
16
]
],
"date-time": "2023-10-16T20:44:41Z",
"timestamp": 1697489081000
},
"editor": [
{
"affiliation": [],
"family": "Lau",
"given": "Susanna Kar Pui",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
27
]
],
"date-time": "2024-04-27T15:12:48Z",
"timestamp": 1714230768036
},
"is-referenced-by-count": 49,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
1,
4
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2021,
1,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
4
]
],
"date-time": "2021-01-04T00:00:00Z",
"timestamp": 1609718400000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pntd.0008895",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0008895",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2021,
1,
4
]
]
},
"published-online": {
"date-parts": [
[
2021,
1,
4
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"DOI": "10.7150/ijbs.45472",
"article-title": "Zoonotic origins of human coronaviruses",
"author": "Z-W Ye",
"doi-asserted-by": "crossref",
"first-page": "1686",
"journal-title": "Int J Biol Sci",
"key": "pntd.0008895.ref001",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-0820-9",
"article-title": "The proximal origin of SARS-CoV-2",
"author": "KG Andersen",
"doi-asserted-by": "crossref",
"first-page": "450",
"journal-title": "Nat Med",
"key": "pntd.0008895.ref002",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1128/CMR.00023-07",
"article-title": "Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection",
"author": "VCC Cheng",
"doi-asserted-by": "crossref",
"first-page": "660",
"journal-title": "Clin Microbiol Rev",
"key": "pntd.0008895.ref003",
"volume": "20",
"year": "2007"
},
{
"article-title": "Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China",
"author": "C Wu",
"journal-title": "JAMA Intern Med",
"key": "pntd.0008895.ref004",
"year": "2020"
},
{
"article-title": "Implications of COVID-19 for patients with pre-existing digestive diseases",
"author": "R Mao",
"first-page": "426",
"journal-title": "Lancet Gastroenterol Hepatol.",
"key": "pntd.0008895.ref005",
"volume": "5",
"year": "2020"
},
{
"article-title": "Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan",
"author": "S Shi",
"journal-title": "China JAMA Cardiol",
"key": "pntd.0008895.ref006",
"year": "2020"
},
{
"article-title": "Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis",
"author": "A Emami",
"first-page": "e35",
"journal-title": "Arch Acad Emerg Med",
"key": "pntd.0008895.ref007",
"volume": "8",
"year": "2020"
},
{
"article-title": "Predictors of Mortality for Patients with COVID-19 Pneumonia Caused by SARS-CoV-2: A Prospective Cohort Study",
"author": "R-H Du",
"journal-title": "Eur Respir J",
"key": "pntd.0008895.ref008",
"year": "2020"
},
{
"article-title": "Covid-19: risk factors for severe disease and death",
"author": "RE Jordan",
"first-page": "m1198",
"journal-title": "BMJ",
"key": "pntd.0008895.ref009",
"volume": "2020"
},
{
"article-title": "Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19)",
"author": "H Nishiura",
"journal-title": "Int J Infect Dis",
"key": "pntd.0008895.ref010",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1165",
"article-title": "Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village",
"author": "M. Day",
"doi-asserted-by": "crossref",
"first-page": "m1165",
"journal-title": "BMJ",
"key": "pntd.0008895.ref011",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1375",
"article-title": "Covid-19: four fifths of cases are asymptomatic. China figures indicate",
"author": "M. Day",
"doi-asserted-by": "crossref",
"first-page": "m1375",
"journal-title": "BMJ",
"key": "pntd.0008895.ref012",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.3201/eid2607.200282",
"article-title": "High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2",
"author": "S Sanche",
"doi-asserted-by": "crossref",
"journal-title": "Emerg Infect Dis",
"key": "pntd.0008895.ref013",
"volume": "26",
"year": "2020"
},
{
"article-title": "Assessment of the SARS-CoV-2 basic reproduction number, R0, based on the early phase of COVID-19 outbreak in Italy",
"author": "M D'Arienzo",
"journal-title": "Biosafety and Health",
"key": "pntd.0008895.ref014",
"year": "2020"
},
{
"article-title": "Symptom clusters in Covid19: A potential clinical prediction tool from the COVID Symptom study app",
"author": "CH Sudre",
"journal-title": "MedRxiv",
"key": "pntd.0008895.ref015",
"year": "2020"
},
{
"DOI": "10.1101/2020.05.07.20090621",
"article-title": "Prolonged viral RNA shedding after COVID-19 symptom resolution in older convalescent plasma donors",
"author": "WR Hartman",
"doi-asserted-by": "crossref",
"key": "pntd.0008895.ref016"
},
{
"key": "pntd.0008895.ref017",
"unstructured": "Website. [cited 18 Jun 2020]. Available from: “Coronavirus Disease 2019 (COVID-19) CDC—Symptoms of Coronavirus.” n.d. Accessed June 18, 2020. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html."
},
{
"author": "M Cascella",
"key": "pntd.0008895.ref018",
"volume-title": "Features, Evaluation and Treatment Coronavirus (COVID-19). StatPearls.",
"year": "2020"
},
{
"article-title": "Clinical Characteristics of Coronavirus Disease 2019 in China",
"author": "W-J Guan",
"journal-title": "N Engl J Med",
"key": "pntd.0008895.ref019",
"year": "2020"
},
{
"article-title": "Is Loss Of Smell And Taste A Symptom Of COVID-19? Doctors Want To Find Out",
"author": "E Kwong",
"journal-title": "NPR",
"key": "pntd.0008895.ref020",
"year": "2020"
},
{
"article-title": "Loss of smell and taste in combination with other symptoms is a strong predictor of COVID-19 infection",
"author": "C Menni",
"journal-title": "Epidemiology medRxiv.",
"key": "pntd.0008895.ref021",
"year": "2020"
},
{
"article-title": "Anosmia and Ageusia as Initial or Unique Symptoms after SARS-COV-2 Virus Infection",
"author": "C Machado",
"journal-title": "Medicine & Pharmacology",
"key": "pntd.0008895.ref022",
"year": "2020"
},
{
"article-title": "Sudden and Complete Olfactory Loss Function as a Possible Symptom of COVID-19",
"author": "M Eliezer",
"journal-title": "JAMA Otolaryngol Head Neck Surg",
"key": "pntd.0008895.ref023",
"year": "2020"
},
{
"article-title": "Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study",
"author": "A Giacomelli",
"journal-title": "Clin Infect Dis",
"key": "pntd.0008895.ref024",
"year": "2020"
},
{
"article-title": "Anosmia, hyposmia, and dysgeusia as indicators for positive SARS-CoV-2 infection",
"author": "WP Lao",
"journal-title": "World J Otorhinolaryngol Head Neck Surg.",
"key": "pntd.0008895.ref025",
"year": "2020"
},
{
"article-title": "Loss of Smell and Taste in 2013 European Patients With Mild to Moderate COVID-19",
"author": "JR Lechien",
"journal-title": "Ann Intern Med",
"key": "pntd.0008895.ref026",
"year": "2020"
},
{
"key": "pntd.0008895.ref027",
"unstructured": "JHU CSSE COVID-19 Dashboard. [cited 28 Apr 2020]. Available from: https://coronavirus.jhu.edu/map.html"
},
{
"key": "pntd.0008895.ref028",
"unstructured": "CDC COVID-19 symptoms. [cited 28 Apr 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html"
},
{
"DOI": "10.1126/sciadv.abc5801",
"article-title": "Non-neuronal expression of SARS-CoV-2 entry genes in the olfaory system suggests mechanisms underlying COVID-19-associated anosmia",
"author": "DH Brann",
"doi-asserted-by": "crossref",
"first-page": "eabc5801",
"journal-title": "Sci Adv",
"key": "pntd.0008895.ref029",
"year": "2020"
},
{
"article-title": "Confronting the COVID-19 Pandemic with Systems Biology",
"author": "ET Prates",
"journal-title": "bioRxiv",
"key": "pntd.0008895.ref030",
"year": "2020"
},
{
"article-title": "The National COVID Cohort Collaborative (N3C): Rationale, Design, Infrastructure, and Deployment",
"author": "H Melissa",
"journal-title": "J Am Med Inform Assoc.",
"key": "pntd.0008895.ref031",
"year": "2020"
},
{
"DOI": "10.3390/nu9121286",
"article-title": "Zinc as a Gatekeeper of Immune Function",
"author": "I Wessels",
"doi-asserted-by": "crossref",
"journal-title": "Nutrients",
"key": "pntd.0008895.ref032",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1016/j.abb.2016.03.022",
"article-title": "Zinc and immunity: An essential interrelation",
"author": "M Maares",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Arch Biochem Biophys",
"key": "pntd.0008895.ref033",
"volume": "611",
"year": "2016"
},
{
"DOI": "10.1016/j.jtemb.2014.09.002",
"article-title": "Impact of the discovery of human zinc deficiency on health",
"author": "AS Prasad",
"doi-asserted-by": "crossref",
"first-page": "357",
"journal-title": "J Trace Elem Med Biol",
"key": "pntd.0008895.ref034",
"volume": "28",
"year": "2014"
},
{
"key": "pntd.0008895.ref035",
"unstructured": "NIH Office of Dietary Supplements. NIH Office of Dietary Supplements Zinc fact sheet. [cited 2020]. Available from: https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/"
},
{
"DOI": "10.4103/0975-7406.137257",
"article-title": "Gustatory dysfunction",
"author": "T Maheswaran",
"doi-asserted-by": "crossref",
"first-page": "S30",
"journal-title": "J Pharm Bioallied Sci",
"key": "pntd.0008895.ref036",
"volume": "6",
"year": "2014"
},
{
"article-title": "Smell and taste disorders in primary care",
"author": "J Malaty",
"first-page": "852",
"journal-title": "Am Fam Physician",
"key": "pntd.0008895.ref037",
"volume": "88",
"year": "2013"
},
{
"DOI": "10.3109/15360288.2012.676618",
"article-title": "A randomized, placebo controlled trial of oral zinc for chemotherapy-related taste and smell disorders",
"author": "L Lyckholm",
"doi-asserted-by": "crossref",
"first-page": "111",
"journal-title": "J Pain Palliat Care Pharmacother",
"key": "pntd.0008895.ref038",
"volume": "26",
"year": "2012"
},
{
"DOI": "10.1097/00000441-197611000-00006",
"article-title": "A double blind study of the effects of zinc sulfate on taste and smell dysfunction",
"author": "RI Henkin",
"doi-asserted-by": "crossref",
"first-page": "285",
"journal-title": "Am J Med Sci",
"key": "pntd.0008895.ref039",
"volume": "272",
"year": "1976"
},
{
"DOI": "10.1002/(SICI)1097-0142(19980515)82:10<1938::AID-CNCR18>3.0.CO;2-U",
"article-title": "A randomized, controlled clinical trial to evaluate the effects of zinc sulfate on cancer patients with taste alterations caused by head and neck irradiation",
"author": "C Ripamonti",
"doi-asserted-by": "crossref",
"first-page": "1938",
"journal-title": "Cancer",
"key": "pntd.0008895.ref040",
"volume": "82",
"year": "1998"
},
{
"DOI": "10.4140/TCP.n.2016.267",
"article-title": "Zinc and Taste Disturbances in Older Adults: A Review of the Literature",
"author": "M Pisano",
"doi-asserted-by": "crossref",
"first-page": "267",
"journal-title": "Consult Pharm",
"key": "pntd.0008895.ref041",
"volume": "31",
"year": "2016"
},
{
"DOI": "10.1177/106002809603000215",
"article-title": "Zinc deficiency and taste disorders",
"author": "CA Heyneman",
"doi-asserted-by": "crossref",
"first-page": "186",
"journal-title": "Ann Pharmacother",
"key": "pntd.0008895.ref042",
"volume": "30",
"year": "1996"
},
{
"DOI": "10.1093/ajcn/31.10.1948",
"article-title": "Hypogeusia and zinc depletion in chronic dialysis patients",
"author": "E Atkin-Thor",
"doi-asserted-by": "crossref",
"first-page": "1948",
"journal-title": "Am J Clin Nutr",
"key": "pntd.0008895.ref043",
"volume": "31",
"year": "1978"
},
{
"article-title": "SARS-CoV-2 (COVID-19) by the numbers",
"author": "YM Bar-On",
"journal-title": "elife",
"key": "pntd.0008895.ref044",
"year": "2020"
},
{
"DOI": "10.2174/2212798411305010007",
"article-title": "The role of zinc in the treatment of taste disorders",
"author": "T Yagi",
"doi-asserted-by": "crossref",
"first-page": "44",
"journal-title": "Recent Pat Food Nutr Agric",
"key": "pntd.0008895.ref045",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.1016/j.jnutbio.2009.02.001",
"article-title": "Distinctive modulation of inflammatory and metabolic parameters in relation to zinc nutritional status in adult overweight/obese subjects",
"author": "L Costarelli",
"doi-asserted-by": "crossref",
"first-page": "432",
"journal-title": "J Nutr Biochem",
"key": "pntd.0008895.ref046",
"volume": "21",
"year": "2010"
},
{
"DOI": "10.1007/s12576-017-0571-7",
"article-title": "Zinc status is associated with inflammation, oxidative stress, lipid, and glucose metabolism",
"author": "J Olechnowicz",
"doi-asserted-by": "crossref",
"first-page": "19",
"journal-title": "J Physiol Sci",
"key": "pntd.0008895.ref047",
"volume": "68",
"year": "2018"
},
{
"DOI": "10.1002/mnfr.201400761",
"article-title": "Zinc deficiency enhanced inflammatory response by increasing immune cell activation and inducing IL6 promoter demethylation",
"author": "CP Wong",
"doi-asserted-by": "crossref",
"first-page": "991",
"journal-title": "Mol Nutr Food Res",
"key": "pntd.0008895.ref048",
"volume": "59",
"year": "2015"
},
{
"article-title": "Innate immune signaling in the olfactory epithelium reduces odorant receptor levels: modeling transient smell loss in COVID-19 patients",
"author": "S Rodriguez",
"journal-title": "medRxiv",
"key": "pntd.0008895.ref049",
"year": "2020"
},
{
"article-title": "SARS-CoV-2: Olfaction, Brain Infection, and the Urgent Need for Clinical Samples Allowing Earlier Virus Detection",
"author": "R Butowt",
"first-page": "1200",
"journal-title": "ACS Chem Neurosci",
"key": "pntd.0008895.ref050",
"volume": "2020"
},
{
"DOI": "10.1007/s00204-011-0775-1",
"article-title": "Zinc and human health: an update",
"author": "CT Chasapis",
"doi-asserted-by": "crossref",
"first-page": "521",
"journal-title": "Arch Toxicol",
"key": "pntd.0008895.ref051",
"year": "2012"
},
{
"DOI": "10.5588/ijtld.15.0653",
"article-title": "Efficacy of zinc sulphate on in-hospital outcome of community-acquired pneumonia in people aged 50 years and over",
"author": "S Sharafi",
"doi-asserted-by": "crossref",
"first-page": "685",
"journal-title": "Int J Tuberc Lung Dis",
"key": "pntd.0008895.ref052",
"volume": "20",
"year": "2016"
},
{
"key": "pntd.0008895.ref053",
"unstructured": "6yt8. [cited 9 May 2020]. Available from: https://www.rcsb.org/structure/6yt8"
},
{
"key": "pntd.0008895.ref054",
"unstructured": "7btf. In: https://www.rcsb.org/structure/7btf."
},
{
"key": "pntd.0008895.ref055"
},
{
"key": "pntd.0008895.ref056",
"unstructured": "2fyg. [cited 9 May 2020]. Available from: https://www.rcsb.org/structure/2fyg"
},
{
"key": "pntd.0008895.ref057",
"unstructured": "6nur. [cited 9 May 2020]. Available from: https://www.rcsb.org/structure/6nur"
},
{
"DOI": "10.1021/pr050361j",
"article-title": "Counting the zinc-proteins encoded in the human genome",
"author": "C Andreini",
"doi-asserted-by": "crossref",
"first-page": "196",
"journal-title": "J Proteome Res",
"key": "pntd.0008895.ref058",
"volume": "5",
"year": "2006"
},
{
"DOI": "10.1093/jn/133.5.1452S",
"article-title": "Zinc-altered immune function",
"author": "K-H Ibs",
"doi-asserted-by": "crossref",
"first-page": "1452S",
"journal-title": "J Nutr",
"key": "pntd.0008895.ref059",
"volume": "133",
"year": "2003"
},
{
"DOI": "10.1093/ajcn/68.2.447S",
"article-title": "Zinc and immune function: the biological basis of altered resistance to infection",
"author": "AH Shankar",
"doi-asserted-by": "crossref",
"first-page": "447S",
"journal-title": "Am J Clin Nutr",
"key": "pntd.0008895.ref060",
"volume": "68",
"year": "1998"
},
{
"article-title": "Zinc and respiratory tract infections: Perspectives for COVID-19 (Review)",
"author": "AV Skalny",
"journal-title": "Int J Mol Med",
"key": "pntd.0008895.ref061",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.015",
"article-title": "Enhancing immunity in viral infections, with special emphasis on COVID-19: A review",
"author": "R Jayawardena",
"doi-asserted-by": "crossref",
"first-page": "367",
"journal-title": "Diabetes Metab Syndr",
"key": "pntd.0008895.ref062",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s11357-011-9377-3",
"article-title": "Zinc: dietary intake and impact of supplementation on immune function in elderly",
"author": "E Mocchegiani",
"doi-asserted-by": "crossref",
"first-page": "839",
"journal-title": "Age",
"key": "pntd.0008895.ref063",
"volume": "35",
"year": "2013"
},
{
"DOI": "10.1007/978-1-4757-9444-1_9",
"article-title": "Zinc and Immunity",
"author": "AS Prasad",
"doi-asserted-by": "crossref",
"first-page": "165",
"journal-title": "Biochemistry of Zinc",
"key": "pntd.0008895.ref064",
"year": "1993"
},
{
"DOI": "10.1007/978-1-4614-1533-6_213",
"article-title": "Zinc and Immunity",
"author": "H Haase",
"doi-asserted-by": "crossref",
"first-page": "2375",
"journal-title": "Encyclopedia of Metalloproteins",
"key": "pntd.0008895.ref065",
"year": "2013"
},
{
"article-title": "Zinc, Health, and Immunity",
"author": "A Prasad",
"first-page": "579",
"journal-title": "Metabolic Medicine and Surgery",
"key": "pntd.0008895.ref066",
"year": "2014"
},
{
"article-title": "Zinc deficiency and infections. Nutrition",
"author": "P. Shetty",
"first-page": "101",
"journal-title": "immunity and infection",
"key": "pntd.0008895.ref067"
},
{
"DOI": "10.1016/j.immuni.2013.09.009",
"article-title": "An Element of Life: Competition for Zinc in Host-Pathogen Interaction",
"author": "H. Haase",
"doi-asserted-by": "crossref",
"first-page": "623",
"journal-title": "Immunity",
"key": "pntd.0008895.ref068",
"year": "2013"
},
{
"DOI": "10.1016/S0065-2776(08)00003-5",
"article-title": "Roles of Zinc and Zinc Signaling in Immunity: Zinc as an Intracellular Signaling Molecule",
"author": "T Hirano",
"doi-asserted-by": "crossref",
"first-page": "149",
"journal-title": "Adv Immunol",
"key": "pntd.0008895.ref069",
"year": "2008"
},
{
"DOI": "10.1007/978-3-030-16073-9_8",
"article-title": "Zinc and the Immune System",
"author": "NZ Gammoh",
"doi-asserted-by": "crossref",
"first-page": "127",
"journal-title": "Nutrition and Immunity",
"key": "pntd.0008895.ref070",
"year": "2019"
},
{
"DOI": "10.1201/9781315118901-15",
"article-title": "Zinc Regulation of the Immune Response",
"author": "V Kloubert",
"doi-asserted-by": "crossref",
"first-page": "245",
"journal-title": "Nutrition, Immunity, and Infection",
"key": "pntd.0008895.ref071",
"year": "2017"
},
{
"DOI": "10.1023/A:1012497926537",
"article-title": "Mechanism of apoptosis induced by zinc deficiency in peripheral blood T lymphocytes",
"author": "VM Kolenko",
"doi-asserted-by": "crossref",
"first-page": "419",
"journal-title": "Apoptosis",
"key": "pntd.0008895.ref072",
"volume": "6",
"year": "2001"
},
{
"DOI": "10.3389/fnut.2014.00014",
"article-title": "Zinc is an Antioxidant and Anti-Inflammatory Agent: Its Role in Human Health",
"author": "AS Prasad",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Front Nutr",
"key": "pntd.0008895.ref073",
"volume": "1",
"year": "2014"
},
{
"DOI": "10.1016/j.celrep.2013.01.009",
"article-title": "ZIP8 regulates host defense through zinc-mediated inhibition of NF-κB",
"author": "M-J Liu",
"doi-asserted-by": "crossref",
"first-page": "386",
"journal-title": "Cell Rep",
"key": "pntd.0008895.ref074",
"volume": "3",
"year": "2013"
},
{
"article-title": "Integrative considerations during the COVID-19 pandemic",
"author": "L Alschuler",
"journal-title": "Explore",
"key": "pntd.0008895.ref075",
"year": "2020"
},
{
"DOI": "10.3332/ecancer.2020.1022",
"article-title": "Associations between immune-suppressive and stimulating drugs and novel COVID-19—a systematic review of current evidence",
"author": "B Russell",
"doi-asserted-by": "crossref",
"key": "pntd.0008895.ref076",
"year": "2020"
},
{
"article-title": "Potential interventions for novel coronavirus in China: A systematic review",
"author": "L Zhang",
"first-page": "479",
"journal-title": "J Med Virol",
"key": "pntd.0008895.ref077",
"volume": "2020"
},
{
"article-title": "Current status of potential therapeutic candidates for the COVID-19 crisis",
"author": "J Zhang",
"journal-title": "Brain Behav Immun",
"key": "pntd.0008895.ref078",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30305-6",
"article-title": "Reducing mortality from 2019-nCoV: host-directed therapies should be an option",
"author": "A Zumla",
"doi-asserted-by": "crossref",
"first-page": "e35",
"journal-title": "Lancet",
"key": "pntd.0008895.ref079",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1177/1060028020928052",
"article-title": "Myth Busters: Dietary Supplements and COVID-19",
"author": "KK Adams",
"doi-asserted-by": "crossref",
"first-page": "820",
"journal-title": "Ann Pharmacother",
"key": "pntd.0008895.ref080",
"volume": "54",
"year": "2020"
},
{
"article-title": "Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections",
"author": "PC Calder",
"journal-title": "Nutrients",
"key": "pntd.0008895.ref081",
"year": "2020"
},
{
"article-title": "Dietary recommendations during the COVID-19 pandemic",
"author": "C-RC de Faria",
"journal-title": "Nutr Rev.",
"key": "pntd.0008895.ref082",
"year": "2020"
},
{
"DOI": "10.1126/science.abc6261",
"article-title": "Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans",
"author": "PS Arunachalam",
"doi-asserted-by": "crossref",
"first-page": "1210",
"journal-title": "Science",
"key": "pntd.0008895.ref083",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.03.004",
"article-title": "Clinical progression of patients with COVID-19 in Shanghai",
"author": "J Chen",
"doi-asserted-by": "crossref",
"first-page": "e1",
"journal-title": "China J Infect",
"key": "pntd.0008895.ref084",
"volume": "80",
"year": "2020"
},
{
"article-title": "The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application",
"author": "SA Lauer",
"journal-title": "Ann Intern Med",
"key": "pntd.0008895.ref085",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0050568",
"article-title": "Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting",
"author": "KR Wessells",
"doi-asserted-by": "crossref",
"first-page": "e50568",
"journal-title": "PLoS One",
"key": "pntd.0008895.ref086",
"volume": "7",
"year": "2012"
},
{
"DOI": "10.1111/j.1753-4887.2009.00253.x",
"article-title": "Low zinc status: a new risk factor for pneumonia in the elderly?",
"author": "JB Barnett",
"doi-asserted-by": "crossref",
"first-page": "30",
"journal-title": "Nutr Rev",
"key": "pntd.0008895.ref087",
"volume": "68",
"year": "2010"
},
{
"DOI": "10.1016/S0140-6736(04)16252-1",
"article-title": "Zinc for severe pneumonia in very young children: double-blind placebo-controlled trial",
"author": "WA Brooks",
"doi-asserted-by": "crossref",
"first-page": "1683",
"journal-title": "Lancet",
"key": "pntd.0008895.ref088",
"volume": "363",
"year": "2004"
},
{
"DOI": "10.1177/194589240401800302",
"article-title": "Anosmia after intranasal zinc gluconate use",
"author": "BW Jafek",
"doi-asserted-by": "crossref",
"first-page": "137",
"journal-title": "Am J Rhinol",
"key": "pntd.0008895.ref089",
"volume": "18",
"year": "2004"
},
{
"DOI": "10.1016/S0022-3476(38)80128-1",
"article-title": "Persistent anosmia following zinc sulfate nasal spraying",
"author": "FF Tisdall",
"doi-asserted-by": "crossref",
"first-page": "60",
"journal-title": "J Pediatr",
"key": "pntd.0008895.ref090",
"volume": "13",
"year": "1938"
},
{
"article-title": "Anosmia due to inhalational zinc: a case report",
"author": "CA DeCook",
"first-page": "659",
"journal-title": "Chem Senses",
"key": "pntd.0008895.ref091",
"volume": "25",
"year": "2000"
},
{
"DOI": "10.1097/01.mlg.0000191549.17796.13",
"article-title": "Intranasal Zinc and Anosmia: The Zinc-Induced Anosmia Syndrome",
"author": "TH Alexander",
"doi-asserted-by": "crossref",
"first-page": "217",
"journal-title": "Laryngoscope",
"key": "pntd.0008895.ref092",
"year": "2006"
},
{
"DOI": "10.1001/archoto.2010.111",
"article-title": "The Bradford Hill criteria and zinc-induced anosmia: a causality analysis",
"author": "TM Davidson",
"doi-asserted-by": "crossref",
"first-page": "673",
"journal-title": "Arch Otolaryngol Head Neck Surg",
"key": "pntd.0008895.ref093",
"volume": "136",
"year": "2010"
},
{
"article-title": "The Vitamin Myth: Why We Think We Need Supplements",
"author": "P. Offit",
"journal-title": "The Atlantic",
"key": "pntd.0008895.ref094",
"year": "2013"
},
{
"article-title": "Zinc for the common cold",
"author": "M Singh",
"first-page": "CD001364",
"journal-title": "Cochrane Database Syst Rev",
"key": "pntd.0008895.ref095",
"year": "2013"
},
{
"DOI": "10.1155/2014/694193",
"article-title": "The effect of adjuvant zinc therapy on recovery from pneumonia in hospitalized children: a double-blind randomized controlled trial.",
"author": "MJ Qasemzadeh",
"doi-asserted-by": "crossref",
"first-page": "694193",
"journal-title": "Scientifica",
"key": "pntd.0008895.ref096",
"volume": "2014",
"year": "2014"
},
{
"DOI": "10.1136/bmj.324.7350.1358",
"article-title": "Effect of routine zinc supplementation on pneumonia in children aged 6 months to 3 years: randomised controlled trial in an urban slum",
"author": "N Bhandari",
"doi-asserted-by": "crossref",
"first-page": "1358",
"journal-title": "BMJ",
"key": "pntd.0008895.ref097",
"volume": "324",
"year": "2002"
},
{
"DOI": "10.1177/156482651303400209",
"article-title": "Comparison of the Estimated Cost-Effectiveness of Preventive and Therapeutic Zinc Supplementation Strategies for Reducing Child Morbidity and Mortality in Sub-Saharan Africa",
"author": "KH Brown",
"doi-asserted-by": "crossref",
"first-page": "199",
"journal-title": "Food Nutr Bull",
"key": "pntd.0008895.ref098",
"year": "2013"
},
{
"DOI": "10.1093/ajcn/83.5.1089",
"article-title": "Efficacy of zinc in the treatment of severe pneumonia in hospitalized children <2 y old",
"author": "A Bose",
"doi-asserted-by": "crossref",
"first-page": "1089",
"journal-title": "Am J Clin Nutr",
"key": "pntd.0008895.ref099",
"year": "2006"
},
{
"DOI": "10.1093/ajcn/86.4.1167",
"article-title": "Serum zinc and pneumonia in nursing home elderly",
"author": "SN Meydani",
"doi-asserted-by": "crossref",
"first-page": "1167",
"journal-title": "Am J Clin Nutr",
"key": "pntd.0008895.ref100",
"volume": "86",
"year": "2007"
},
{
"DOI": "10.1093/jn/130.5.1378S",
"article-title": "Dietary factors influencing zinc absorption",
"author": "B. Lönnerdal",
"doi-asserted-by": "crossref",
"first-page": "1378S",
"journal-title": "J Nutr",
"key": "pntd.0008895.ref101",
"volume": "130",
"year": "2000"
},
{
"DOI": "10.1016/j.jtemb.2014.08.011",
"article-title": "Dietary phytate, zinc and hidden zinc deficiency",
"author": "HH Sandstead",
"doi-asserted-by": "crossref",
"first-page": "414",
"journal-title": "J Trace Elem Med Biol",
"key": "pntd.0008895.ref102",
"volume": "28",
"year": "2014"
},
{
"author": "Institute of Medicine, Food and Nutrition Board",
"key": "pntd.0008895.ref103",
"volume-title": "Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc external link disclaimer",
"year": "2001"
},
{
"DOI": "10.1111/j.1745-459X.2005.00005.x",
"article-title": "Descriptive analysis of divalent salts",
"author": "HH-L Yang",
"doi-asserted-by": "crossref",
"first-page": "97",
"journal-title": "J Sens Stud",
"key": "pntd.0008895.ref104",
"volume": "20",
"year": "2005"
},
{
"article-title": "Dietitians of Canada. Position of the American Dietetic Association and Dietitians of Canada: Vegetarian diets",
"author": "American Dietetic Association",
"first-page": "748",
"journal-title": "J Am Diet Assoc",
"key": "pntd.0008895.ref105",
"year": "2003"
},
{
"DOI": "10.1097/01.ede.0000289012.66211.45",
"article-title": "The Effect of Vegetarian Diet on Immune Response",
"author": "E Neubauerova",
"doi-asserted-by": "crossref",
"first-page": "S196",
"journal-title": "Epidemiology",
"key": "pntd.0008895.ref106",
"year": "2007"
},
{
"DOI": "10.1093/advances/nmy103",
"article-title": "Vegetarian-Based Dietary Patterns and their Relation with Inflammatory and Immune Biomarkers: A Systematic Review and Meta-Analysis",
"author": "JC Craddock",
"doi-asserted-by": "crossref",
"first-page": "433",
"journal-title": "Adv Nutr",
"key": "pntd.0008895.ref107",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1038/srep10974",
"article-title": "Dietary calcium and zinc deficiency risks are decreasing but remain prevalent",
"author": "DB Kumssa",
"doi-asserted-by": "crossref",
"first-page": "10974",
"journal-title": "Sci Rep",
"key": "pntd.0008895.ref108",
"volume": "5",
"year": "2015"
},
{
"DOI": "10.1016/j.exger.2007.10.015",
"article-title": "Does ageing affect zinc homeostasis and dietary requirements?",
"author": "SJ Fairweather-Tait",
"doi-asserted-by": "crossref",
"first-page": "382",
"journal-title": "Exp Gerontol",
"key": "pntd.0008895.ref109",
"volume": "43",
"year": "2008"
},
{
"DOI": "10.1007/s10522-006-9057-3",
"article-title": "Correlation between zinc status and immune function in the elderly.",
"author": "H Haase",
"doi-asserted-by": "crossref",
"first-page": "421",
"journal-title": "Biogerontology",
"key": "pntd.0008895.ref110",
"volume": "7",
"year": "2006"
},
{
"DOI": "10.1016/S0308-8146(02)00249-2",
"article-title": "The effect of phytic acid and some natural chelating agents on the solubility of mineral elements in oat bran",
"author": "P Ekholm",
"doi-asserted-by": "crossref",
"first-page": "165",
"journal-title": "Food Chem",
"key": "pntd.0008895.ref111",
"volume": "80",
"year": "2003"
},
{
"article-title": "Development, Prevention, and Treatment of Alcohol-Induced Organ Injury: The Role of Nutrition",
"author": "S Barve",
"first-page": "289",
"journal-title": "Alcohol Res",
"key": "pntd.0008895.ref112",
"volume": "38",
"year": "2017"
},
{
"article-title": "Zinc and Oxidative Stress: Current Mechanisms",
"author": "N Marreiro D do",
"journal-title": "Antioxidants (Basel)",
"key": "pntd.0008895.ref113",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.5897/AJB2017.16300",
"article-title": "Toxicological and safety assessment of tartrazine as a synthetic food additive on health biomarkers: A review",
"author": "KA Amin",
"doi-asserted-by": "crossref",
"first-page": "139",
"journal-title": "Afr J Biotechnol",
"key": "pntd.0008895.ref114",
"volume": "17",
"year": "2018"
},
{
"DOI": "10.1016/j.jaad.2006.08.015",
"article-title": "Acrodermatitis enteropathica and an overview of zinc metabolism",
"author": "E Maverakis",
"doi-asserted-by": "crossref",
"first-page": "116",
"journal-title": "J Am Acad Dermatol",
"key": "pntd.0008895.ref115",
"volume": "56",
"year": "2007"
},
{
"DOI": "10.1097/MPG.0000000000000628",
"article-title": "Clinical zinc deficiency as early presentation of Wilson disease",
"author": "S Van Biervliet",
"doi-asserted-by": "crossref",
"first-page": "457",
"journal-title": "J Pediatr Gastroenterol Nutr",
"key": "pntd.0008895.ref116",
"volume": "60",
"year": "2015"
},
{
"DOI": "10.1093/ajcn/75.2.181",
"article-title": "Zinc deficiency in patients with sickle cell disease",
"author": "AS Prasad",
"doi-asserted-by": "crossref",
"first-page": "181",
"journal-title": "Am J Clin Nutr",
"key": "pntd.0008895.ref117",
"year": "2002"
},
{
"DOI": "10.1111/jdv.15524",
"article-title": "Zinc and atopic dermatitis: a systematic review and meta-analysis",
"author": "NA Gray",
"doi-asserted-by": "crossref",
"first-page": "1042",
"journal-title": "J Eur Acad Dermatol Venereol",
"key": "pntd.0008895.ref118",
"volume": "33",
"year": "2019"
},
{
"DOI": "10.1016/0197-0070(87)90227-0",
"article-title": "Zinc deficiency in anorexia nervosa",
"author": "RL Katz",
"doi-asserted-by": "crossref",
"first-page": "400",
"journal-title": "J Adolesc Health Care",
"key": "pntd.0008895.ref119",
"volume": "8",
"year": "1987"
},
{
"DOI": "10.1080/07315724.1998.10718803",
"article-title": "Zinc Metabolism in Patients with Exocrine Pancreatic Insufficiency",
"author": "SK Dutta",
"doi-asserted-by": "crossref",
"first-page": "556",
"journal-title": "J Am Coll Nutr",
"key": "pntd.0008895.ref120",
"year": "1998"
},
{
"DOI": "10.1016/j.nut.2004.05.022",
"article-title": "Gestational hyperglycemia, zinc, selenium, and antioxidant vitamins",
"author": "S Bo",
"doi-asserted-by": "crossref",
"first-page": "186",
"journal-title": "Nutrition",
"key": "pntd.0008895.ref121",
"volume": "21",
"year": "2005"
},
{
"DOI": "10.1093/ndt/gfz065",
"article-title": "Renal handling of zinc in chronic kidney disease patients and the role of circulating zinc levels in renal function decline.",
"author": "K Damianaki",
"doi-asserted-by": "crossref",
"first-page": "1163",
"journal-title": "Nephrol Dial Transplant 2020",
"key": "pntd.0008895.ref122",
"volume": "35"
},
{
"DOI": "10.3390/nu10010088",
"article-title": "Associations between Zinc Deficiency and Metabolic Abnormalities in Patients with Chronic Liver Disease",
"author": "T Himoto",
"doi-asserted-by": "crossref",
"journal-title": "Nutrients",
"key": "pntd.0008895.ref123",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.4103/jfcm.JFCM_113_19",
"article-title": "The status of zinc in type 2 diabetic patients and its association with glycemic control",
"author": "DM Farooq",
"doi-asserted-by": "crossref",
"first-page": "29",
"journal-title": "J Family Community Med 2020",
"key": "pntd.0008895.ref124",
"volume": "27"
},
{
"DOI": "10.1111/j.1753-4887.1988.tb05381.x",
"article-title": "Zinc deficiency in inflammatory bowel disease",
"author": "KM Hendricks",
"doi-asserted-by": "crossref",
"first-page": "401",
"journal-title": "Nutr Rev",
"key": "pntd.0008895.ref125",
"volume": "46",
"year": "1988"
},
{
"DOI": "10.1093/ajcn/68.2.499S",
"article-title": "Potential contribution of maternal zinc supplementation during pregnancy to maternal and child survival",
"author": "LE Caulfield",
"doi-asserted-by": "crossref",
"first-page": "499S",
"journal-title": "Am J Clin Nutr",
"key": "pntd.0008895.ref126",
"volume": "68",
"year": "1998"
},
{
"DOI": "10.1159/000348261",
"article-title": "Update on zinc deficiency and excess in clinical pediatric practice",
"author": "NF Krebs",
"doi-asserted-by": "crossref",
"first-page": "19",
"issue": "Suppl 1",
"journal-title": "Ann Nutr Metab",
"key": "pntd.0008895.ref127",
"volume": "62",
"year": "2013"
},
{
"DOI": "10.1016/j.ejmhg.2016.04.009",
"article-title": "Magnesium, zinc and copper estimation in children with attention deficit hyperactivity disorder (ADHD)",
"author": "F Elbaz",
"doi-asserted-by": "crossref",
"first-page": "153",
"journal-title": "Egyptian Journal of Medical Human Genetics",
"key": "pntd.0008895.ref128",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1016/j.redox.2020.101529",
"article-title": "Zinc at the crossroads of exercise and proteostasis",
"author": "JD Hernández-Camacho",
"doi-asserted-by": "crossref",
"first-page": "101529",
"journal-title": "Redox Biol",
"key": "pntd.0008895.ref129",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1007/s12011-017-0944-z",
"article-title": "Zinc Deficiency and Oxidative Stress Involved in Valproic Acid Induced Hepatotoxicity: Protection by Zinc and Selenium Supplementation",
"author": "N Ahangar",
"doi-asserted-by": "crossref",
"first-page": "102",
"journal-title": "Biol Trace Elem Res",
"key": "pntd.0008895.ref130",
"volume": "179",
"year": "2017"
},
{
"DOI": "10.1111/ijcp.12040",
"article-title": "Pharmaco-nutrient interactions—a systematic review of zinc and antihypertensive therapy",
"author": "LA Braun",
"doi-asserted-by": "crossref",
"first-page": "717",
"journal-title": "Int J Clin Pract",
"key": "pntd.0008895.ref131",
"volume": "67",
"year": "2013"
},
{
"DOI": "10.1053/j.gastro.2009.08.014",
"article-title": "Zinc: an essential trace element for parenteral nutrition",
"author": "K. Jeejeebhoy",
"doi-asserted-by": "crossref",
"first-page": "S7",
"journal-title": "Gastroenterology",
"key": "pntd.0008895.ref132",
"volume": "137",
"year": "2009"
},
{
"DOI": "10.1038/s41598-017-12054-7",
"article-title": "The cancer chemotherapeutic agent paclitaxel (Taxol) reduces hippocampal neurogenesis via down-regulation of vesicular zinc",
"author": "BE Lee",
"doi-asserted-by": "crossref",
"first-page": "11667",
"journal-title": "Sci Rep",
"key": "pntd.0008895.ref133",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1016/j.jsbmb.2016.04.006",
"article-title": "Vitamin D3 transactivates the zinc and manganese transporter SLC30A10 via the Vitamin D receptor",
"author": "T Claro da Silva",
"doi-asserted-by": "crossref",
"first-page": "77",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "pntd.0008895.ref134",
"volume": "163",
"year": "2016"
},
{
"DOI": "10.1101/2020.04.08.20058578",
"article-title": "The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients",
"author": "A Daneshkhah",
"doi-asserted-by": "crossref",
"key": "pntd.0008895.ref135"
},
{
"article-title": "Severe immunosuppression and not a cytokine storm characterize COVID-19 infections",
"author": "KE Remy",
"journal-title": "JCI Insight",
"key": "pntd.0008895.ref136",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/34.9.1670",
"article-title": "The effect of dietary zinc on intestinal copper absorption",
"author": "PW Fischer",
"doi-asserted-by": "crossref",
"first-page": "1670",
"journal-title": "Am J Clin Nutr",
"key": "pntd.0008895.ref137",
"volume": "34",
"year": "1981"
},
{
"key": "pntd.0008895.ref138",
"unstructured": "www.drugs.com/drug-interactions. [cited 2020]. Available from: https://www.drugs.com/drug-interactions/zinc-sulfate,zinc-index.html"
},
{
"DOI": "10.1097/01.qai.0000242446.44285.b5",
"article-title": "Brief Report: Randomized Controlled Trial of Zinc Supplementation for Persistent Diarrhea in Adults With HIV-1",
"author": "C Cárcamo",
"doi-asserted-by": "crossref",
"first-page": "197",
"journal-title": "Infection. JAIDS Journal of Acquired Immune Deficiency Syndromes",
"key": "pntd.0008895.ref139",
"volume": "43",
"year": "2006"
},
{
"DOI": "10.1086/652864",
"article-title": "Randomized, controlled clinical trial of zinc supplementation to prevent immunological failure in HIV-infected adults",
"author": "MK Baum",
"doi-asserted-by": "crossref",
"first-page": "1653",
"journal-title": "Clin Infect Dis",
"key": "pntd.0008895.ref140",
"volume": "50",
"year": "2010"
},
{
"DOI": "10.1542/peds.2010-3091",
"article-title": "A randomized controlled trial of zinc as adjuvant therapy for severe pneumonia in young children",
"author": "S Basnet",
"doi-asserted-by": "crossref",
"first-page": "701",
"journal-title": "Pediatrics",
"key": "pntd.0008895.ref141",
"volume": "129",
"year": "2012"
},
{
"DOI": "10.7189/jogh.08.010418",
"article-title": "Zinc as an adjunct therapy in the management of severe pneumonia among Gambian children: randomized controlled trial",
"author": "S Howie",
"doi-asserted-by": "crossref",
"first-page": "010418",
"journal-title": "J Glob Health",
"key": "pntd.0008895.ref142",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1186/1824-7288-38-36",
"article-title": "Role of zinc in severe pneumonia: a randomized double bind placebo controlled study",
"author": "GS Shah",
"doi-asserted-by": "crossref",
"first-page": "36",
"journal-title": "Ital J Pediatr",
"key": "pntd.0008895.ref143",
"volume": "38",
"year": "2012"
},
{
"article-title": "A randomised controlled trial of oral zinc on the immune response to tuberculosis in HIV-infected patients",
"author": "JA Green",
"first-page": "1378",
"journal-title": "Int J Tuberc Lung Dis",
"key": "pntd.0008895.ref144",
"volume": "9",
"year": "2005"
},
{
"DOI": "10.1111/j.1365-3156.2011.02871.x",
"article-title": "Efficacy and safety of zinc supplementation for adults, children and pregnant women with HIV infection: systematic review",
"author": "L Zeng",
"doi-asserted-by": "crossref",
"first-page": "1474",
"journal-title": "Tropical Med Int Health",
"key": "pntd.0008895.ref145",
"volume": "16",
"year": "2011"
},
{
"DOI": "10.1046/j.1365-2893.2001.00311.x",
"article-title": "Zinc supplementation enhances the response to interferon therapy in patients with chronic hepatitis C",
"author": "H Takagi",
"doi-asserted-by": "crossref",
"first-page": "367",
"journal-title": "J Viral Hepat",
"key": "pntd.0008895.ref146",
"volume": "8",
"year": "2001"
},
{
"DOI": "10.3945/jn.115.220079",
"article-title": "Biomarkers of Nutrition for Development (BOND)-Zinc Review",
"author": "JC King",
"doi-asserted-by": "crossref",
"first-page": "858S",
"journal-title": "J Nutr",
"key": "pntd.0008895.ref147",
"volume": "146",
"year": "2015"
},
{
"key": "pntd.0008895.ref148",
"unstructured": "National Institutes of Health. Coronavirus disease 2019 (COVID-19) treatment guidelines. [cited 3 Aug 2020]. Available from: https://www.covid19treatmentguidelines.nih.gov/"
},
{
"DOI": "10.3390/nu7053252",
"article-title": "Determination of zinc status in humans: which indicator should we use?",
"author": "FT Wieringa",
"doi-asserted-by": "crossref",
"first-page": "3252",
"journal-title": "Nutrients",
"key": "pntd.0008895.ref149",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.3109/13590849009003134",
"article-title": "The Influence of the Chemical Additive Tartrazine on the Zinc Status of Hyperactive Children—a Double-blind Placebo-controlled Study",
"author": "NI Ward",
"doi-asserted-by": "crossref",
"first-page": "51",
"journal-title": "Journal of Nutritional Medicine",
"key": "pntd.0008895.ref150",
"year": "1990"
},
{
"key": "pntd.0008895.ref151"
},
{
"author": "R Derwand",
"key": "pntd.0008895.ref152"
},
{
"article-title": "Chloroquine Is a Zinc Ionophore",
"author": "J Jing Xue",
"journal-title": "PLoS One",
"key": "pntd.0008895.ref153",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"article-title": "Zn2 Inhibits Coronavirus and Arterivirus RNA Polymerase Activity In Vitro and Zinc Ionophores Block the Replication of These Viruses in Cell Culture",
"author": "AJW te Velthuis",
"doi-asserted-by": "crossref",
"first-page": "e1001176",
"journal-title": "PLoS Pathog",
"key": "pntd.0008895.ref154",
"year": "2010"
},
{
"DOI": "10.1016/j.hermed.2020.100382",
"article-title": "Potential benefits of combination of Nigella sativa and Zn supplements to treat COVID-19",
"author": "MT Rahman",
"doi-asserted-by": "crossref",
"first-page": "100382",
"journal-title": "Journal of Herbal Medicine 2020",
"key": "pntd.0008895.ref155",
"volume": "23"
},
{
"article-title": "Can Zn Be a Critical Element in COVID-19 Treatment?",
"author": "MT Rahman",
"first-page": "1",
"journal-title": "Biol Trace Elem Res",
"key": "pntd.0008895.ref156",
"year": "2020"
},
{
"article-title": "Treatment of SARS-CoV-2 with high dose oral zinc salts: A report on four patients",
"author": "E. Finzi",
"journal-title": "Int J Infect Dis",
"key": "pntd.0008895.ref157",
"year": "2020"
},
{
"DOI": "10.1099/jmm.0.001250",
"article-title": "Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients",
"author": "PM Carlucci",
"doi-asserted-by": "crossref",
"first-page": "1228",
"journal-title": "J Med Microbiol",
"key": "pntd.0008895.ref158",
"volume": "69",
"year": "2020"
},
{
"article-title": "COVID-19: Poor outcomes in patients with Zinc deficiency",
"author": "D Jothimani",
"journal-title": "Int J Infect Dis",
"key": "pntd.0008895.ref159",
"year": "2020"
},
{
"DOI": "10.1016/j.jcot.2020.04.030",
"article-title": "Unprecedented surge in publications related to COVID-19 in the first three months of pandemic: A bibliometric analytic report",
"author": "SBS Kambhampati",
"doi-asserted-by": "crossref",
"first-page": "S304",
"journal-title": "J Clin Orthop Trauma",
"key": "pntd.0008895.ref160",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1186/s13321-018-0326-3",
"article-title": "OGER++: hybrid multi-type entity recognition",
"author": "L Furrer",
"doi-asserted-by": "crossref",
"first-page": "7",
"journal-title": "J Cheminform",
"key": "pntd.0008895.ref161",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.1371/journal.pcbi.1007617",
"article-title": "BioConceptVec: Creating and evaluating literature-based biomedical concept embeddings on a large scale",
"author": "Q Chen",
"doi-asserted-by": "crossref",
"first-page": "e1007617",
"journal-title": "PLoS Comput Biol",
"key": "pntd.0008895.ref162",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30567-5",
"article-title": "How will country-based mitigation measures influence the course of the COVID-19 epidemic?",
"author": "RM Anderson",
"doi-asserted-by": "crossref",
"first-page": "931",
"journal-title": "Lancet",
"key": "pntd.0008895.ref163",
"volume": "395",
"year": "2020"
},
{
"key": "pntd.0008895.ref164",
"unstructured": "Frontline Immune Support. In: Frontline Immune Support [Internet]. [cited 18 Jun 2020]. Available from: https://www.frontlineimmunesupport.com/."
},
{
"article-title": "A cohort study to evaluate the effect of combination Vitamin D, Magnesium and Vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients",
"author": "CW Tan",
"key": "pntd.0008895.ref165"
},
{
"article-title": "The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States",
"author": "JM Wilder",
"journal-title": "Clin Infect Dis",
"key": "pntd.0008895.ref166",
"year": "2020"
},
{
"key": "pntd.0008895.ref167",
"unstructured": "COVID-19 literature search powered by advanced NLP algorithms. In: COVIDscholar [Internet]. [cited 17 Sep 2020]. Available from: https://covidscholar.org/."
},
{
"key": "pntd.0008895.ref168",
"unstructured": "ClinicalTrials.gov Zinc Trials. In: ClinicalTrials.gov [Internet]. [cited 4 May 2020]. Available from: https://www.clinicaltrials.gov/ct2/results?cond=COVID&term=zinc&cntry=&state=&city=&dist=."
}
],
"reference-count": 168,
"references-count": 168,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pntd.0008895"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Zinc against COVID-19? Symptom surveillance and deficiency risk groups",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pntd.corrections_policy",
"volume": "15"
}
