Factors Affecting Mortality in Elderly Hypertensive Hospitalized Patients with COVID-19: A Retrospective Study
et al., Clinical Interventions in Aging, doi:10.2147/cia.s431271, Nov 2023
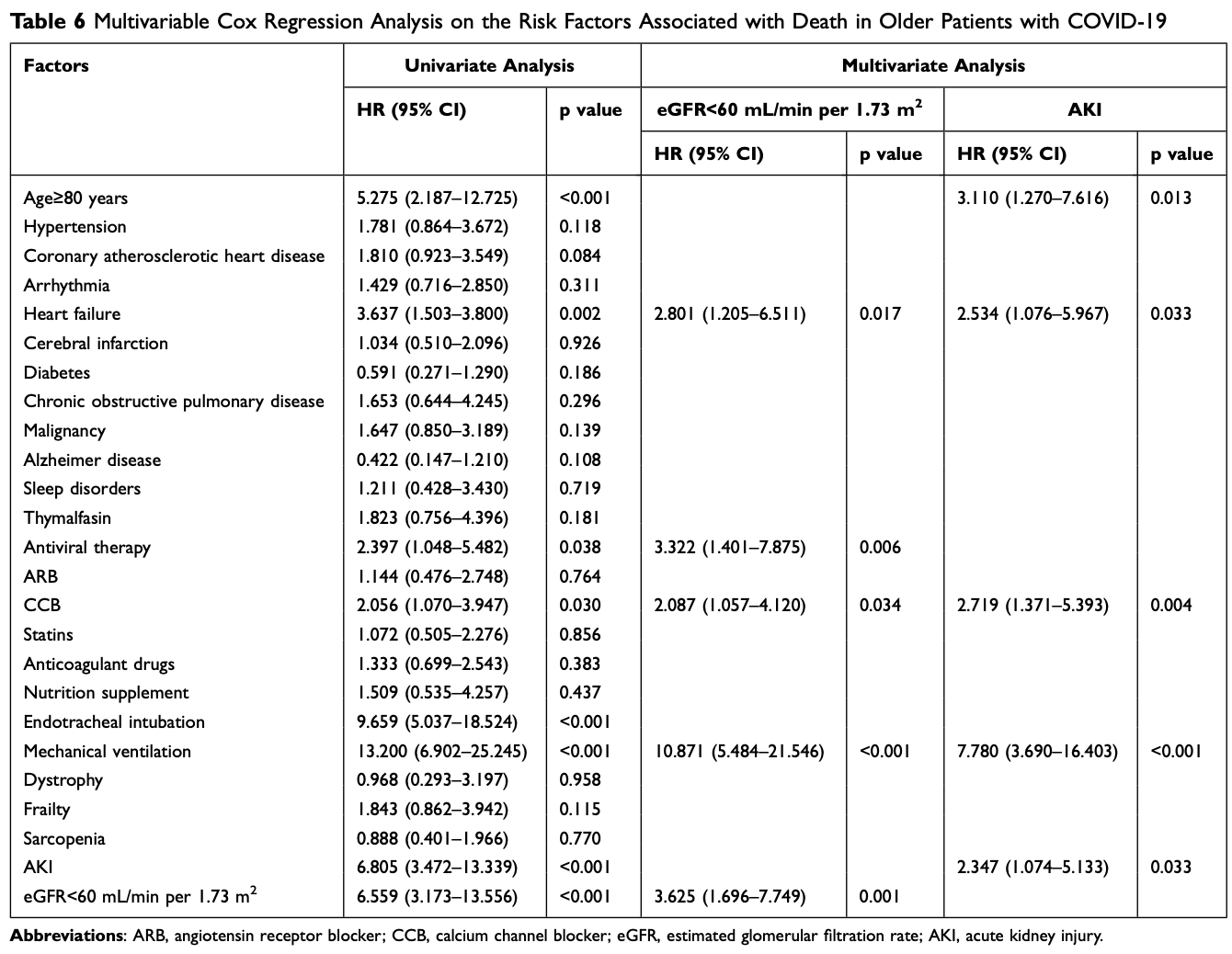
Retrospective 748 elderly hospitalized COVID-19 patients in China showing increased risk of death with paxlovid/molnupiravir. Multivariate analysis showed that paxlovid/molnupiravir was independently associated with higher in-hospital mortality (HR 3.3, p=0.006). Authors do not provide results for paxlovid and molnupiravir separately.
Potential risks of molnupiravir include the creation of dangerous variants, and mutagenicity, carcinogenicity, teratogenicity, and embryotoxicity1-15. Multiple analyses have identified variants potentially created by molnupiravir16-20. Studies show significantly increased risk of acute kidney injury21, cardiovascular toxocity22, and neurological symptoms21. Treatment may increase viral rebound23,24.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments25.
Study covers paxlovid and molnupiravir.
|
risk of death, 232.2% higher, HR 3.32, p = 0.006, treatment 68, control 680, adjusted per study, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Swanstrom et al., Lethal mutagenesis as an antiviral strategy, Science, doi:10.1126/science.abn0048.
2.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
3.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
4.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
5.
Huntsman, M., An assessment of the reproductive toxicity of the anti-COVID-19 drug molnupiravir using stem cell-based embryo models, Master's Thesis, scholarspace.manoa.hawaii.edu/items/cd11342c-b4dc-44c0-8b44-ce6e3369c40b.
6.
Huntsman (B) et al., Detection of developmental toxicity of the anti-COVID-19 drug molnupiravir using gastruloid-based in vitro assays, Toxicological Sciences, doi:10.1093/toxsci/kfaf093.
7.
Zibat et al., N4-hydroxycytidine, the active compound of Molnupiravir, promotes SARS-CoV-2 mutagenesis and escape from a neutralizing nanobody, iScience, doi:10.1016/j.isci.2023.107786.
8.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
9.
Gruber et al., Molnupiravir increases SARS‐CoV‐2 genome diversity and complexity: A case‐control cohort study, Journal of Medical Virology, doi:10.1002/jmv.29642.
10.
Marikawa et al., An active metabolite of the anti-COVID-19 drug molnupiravir impairs mouse preimplantation embryos at clinically relevant concentrations, Reproductive Toxicology, doi:10.1016/j.reprotox.2023.108475.
11.
Rahman, M., Elucidation of the DNA repair mechanisms involved in the repair of DNA damage caused by the Arabinosides and Anti-COVID-19 drugs, tokyo-metro-u.repo.nii.ac.jp/records/2000972.
12.
Zhou et al., β-D-N4-hydroxycytidine Inhibits SARS-CoV-2 Through Lethal Mutagenesis But Is Also Mutagenic To Mammalian Cells, The Journal of Infectious Diseases, doi:10.1093/infdis/jiab247.
13.
Chamod et al., Molnupiravir Metabolite--N4-hydroxycytidine Causes Cytotoxicity and DNA Damage in Mammalian Cells in vitro: N4-hydroxycytidine Induced Cytotoxicity DNA Damage, Asian Medical Journal and Alternative Medicine, 23:3, asianmedjam.com/index.php/amjam/article/view/1448.
14.
Standing et al., Randomized controlled trial of molnupiravir SARS-CoV-2 viral and antibody response in at-risk adult outpatients, Nature Communications, doi:10.1038/s41467-024-45641-0.
15.
Mori et al., Reactive oxygen species-mediated cytotoxic and DNA-damaging mechanism of N4-hydroxycytidine, a metabolite of the COVID-19 therapeutic drug molnupiravir, Free Radical Research, doi:10.1080/10715762.2025.2469738.
16.
Focosi et al., The fitness of molnupiravir-signed SARS-CoV-2 variants: imputation analysis based on prescription counts and GISAID analyses by country, Intervirology, doi:10.1159/000540282.
17.
Sanderson et al., A molnupiravir-associated mutational signature in global SARS-CoV-2 genomes, Nature, doi:10.1038/s41586-023-06649-6.
18.
Fountain-Jones et al., Effect of molnupiravir on SARS-CoV-2 evolution in immunocompromised patients: a retrospective observational study, The Lancet Microbe, doi:10.1016/S2666-5247(23)00393-2.
19.
Kosakovsky Pond et al., Anti-COVID drug accelerates viral evolution, Nature, doi:10.1038/d41586-023-03248-3.
21.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
22.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
23.
Shah et al., SARS-CoV-2 infectious shedding and rebound among adults with and without oral antiviral use: two case-ascertained prospective household studies, The Lancet Microbe, doi:10.1016/j.lanmic.2025.101227.
Xu et al., 30 Nov 2023, retrospective, China, peer-reviewed, median age 76.0, 3 authors, study period 8 December, 2022 - 7 January, 2023.
Contact: lily197459@163.com.
Factors Affecting Mortality in Elderly Hypertensive Hospitalized Patients with COVID-19: A Retrospective Study
Clinical Interventions in Aging, doi:10.2147/cia.s431271
Purpose: Corona Virus Disease 2019 (COVID-19) endangers the health and survival of the elderly. We tried to explore factors especially kidney function which affected mortality in elderly hypertensive patients with COVID-19. Methods: We conducted a retrospective research of 748 COVID-19 elderly patients (≥65 years old) at Zhejiang Hospital. This study compared demographic data, laboratory values, comorbidities, treatments, and clinical outcomes of hypertension and non-hypertension participants, and subgroup analysis of age and frailty was conducted in the hypertension population. Survival analysis was used to determine risk factors for death in elderly patients with COVID-19. Results: Our study revealed that the elderly hypertensive patients with COVID-19 had higher blood urea nitrogen (BUN), serum uric acid (UA), serum creatinine (Scr), lower estimated glomerular filtration rate (eGFR), higher incidence of severity, admission to intensive care unit (ICU) and death, and longer in-hospital stay than non-hypertensive patients, which also occurred in the very elderly hypertensive patients compared with younger hypertensive patients and frail hypertensive patients compared with no-frail hypertensive patients. In addition, the prevalence of acute kidney injury (AKI) was higher in the oldest old hypertensive patients and frail hypertensive patients. Multivariate survival analysis indicated that the independent risk factors for death from COVID-19 were age ≥80 years, heart failure, antiviral therapy, calcium channel blocker (CCB) therapy, mechanical ventilation, AKI, and eGFR<60 mL/min per 1.73 m 2 .
Conclusion: The results of the present study suggested that the elderly hypertensive patients with COVID-19 would have more serious kidney injury, more serious disease progression and higher mortality, which also occurred in very elderly and frailty subgroup. Kidney dysfunction was closely related to mortality in elderly patients with COVID-19.
Abbreviations BUN, blood urea nitrogen; UA, serum uric acid; Scr, serum creatinine; eGFR, estimated glomerular filtration rate; ICU, intensive care unit; AKI, acute kidney injury; CCB, calcium channel blocker; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; COPD, chronic obstructive pulmonary disease; AD, Alzheimer disease; ARB, angiotensin receptor blocker; IQR, interquartile range; ACE, angiotensin-converting enzyme; ACEI, angiotensin-converting enzyme inhibitor; cat L, cathepsin L; TMPRSS2, transmembrane protease serine 2.
Ethical Approval The Ethics Committee of Zhejiang Hospital approved this study (2022-31J). Participants who took part in screening for geriatric syndrome were given written informed consent before participating in the study. All methods were carried out in accordance with relevant guidelines and regulations.
Disclosure The authors have no conflicts of interest to declare that are relevant to the content of this article.
References
Abdalla, Arabey, Gai, Hypertension is still a moving target in the context of COVID-19 and post-acute COVID-19 syndrome, J Med Virol, doi:10.1002/jmv.28128
Anderson, Eldadah, Halter, Acute kidney injury in older adults, J Am Soc Nephrol, doi:10.1681/ASN.2010090934
Bepouka, Situakibanza, Sangare, Mortality associated with COVID-19 and hypertension in sub-Saharan Africa. A systematic review and meta-analysis, Jl Clin Hypertens, doi:10.1111/jch.14417
Chen, Dai, Mo, Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: a single-centered, retrospective study, J Gerontol: Series A, doi:10.1093/gerona/glaa089
Cheng, Luo, Wang, Kidney disease is associated with in-hospital death of patients with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.03.005
Chronopoulos, Cruz, Ronco, Hospital-acquired acute kidney injury in the elderly, Nat Rev Nephrol, doi:10.1038/nrneph.2009.234
Chu, Chan, Yuen, Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study, Lancet Microbe, doi:10.1016/S2666-5247(20)30004-5
Dent, Martin, Bergman, Woo, Romero-Ortuno et al., Management of frailty: opportunities, challenges, and future directions, Lancet, doi:10.1016/S0140-6736(19)31785-4
Diao, Wang, Wang, Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 infection, Nat Commun, doi:10.1038/s41467-021-22781-1
Docherty, Harrison, Green, Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study, BMJ, doi:10.1136/bmj.m1985
Farkash, Wilson, Jentzen, Ultrastructural evidence for direct renal infection with SARS-CoV-2, J Am Soc Nephrol, doi:10.1681/ASN.2020040432
Gallo, Calvez, Savoia, Hypertension and COVID-19: current evidence and perspectives, High Blood Press Cardiovasc Prev, doi:10.1007/s40292-022-00506-9
Gorbalenya, Baker, Baric, The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2, Nat Microbiol, doi:10.1038/s41564-020-0695-z
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy, JAMA, doi:10.1001/jama.2020.5394
Gu, Huang, Cui, Association of acute kidney injury with 1-year outcome of kidney function in hospital survivors with COVID-19: a cohort study, Ebiomedicine, doi:10.1016/j.ebiom.2022.103817
Guan, Liang, Zhao, Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J, doi:10.1183/13993003.00547-2020
Hirsch, Ng, Ross, Acute kidney injury in patients hospitalized with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.05.006
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat Rev Microbiol, doi:10.1038/s41579-020-00459-7
Iaccarino, Grassi, Borghi, Ferri, Salvetti et al., Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian society of hypertension, Hypertens, doi:10.1161/HYPERTENSIONAHA.120.15324
Jiang, Eales, Scannali, Hypertension and renin-angiotensin system blockers are not associated with expression of angiotensin-converting enzyme 2 (ACE2) in the kidney, journal Clinical Interventions in Aging, doi:10.1093/eurheartj/ehaa794
Kellum, Romagnani, Ashuntantang, Ronco, Zarbock et al., Acute kidney injury, Nat Rev Dis Primers, doi:10.1038/s41572-021-00284-z
Küçük, Ergün, Yakar, The effect of frailty on the development of acute kidney injury in critically-ill geriatric patients with COVID-19, Turk J Med Sci, doi:10.55730/1300-0144.5488
Li, Xu, Yu, Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.04.006
Majumder, Minko, Recent developments on therapeutic and diagnostic approaches for COVID-19, Aaps J, doi:10.1208/s12248-020-00532-2
Mancusi, Grassi, Borghi, Determinants of healing among patients with coronavirus disease 2019: the results of the SARS-RAS study of the Italian Society of Hypertension, J Hypertens, doi:10.1097/HJH.0000000000002666
Martin, Sheaff, Renal ageing, J Pathol, doi:10.1002/path.2111
Mennuni, Rubattu, Pierelli, Tocci, Fofi et al., Hypertension and kidneys: unraveling complex molecular mechanisms underlying hypertensive renal damage, J Hum Hypertens, doi:10.1038/jhh.2013.55
Monteil, Kwon, Prado, Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2, Cell, doi:10.1016/j.cell.2020.04.004
Naicker, Yang, Hwang, Liu, Chen et al., The Novel Coronavirus 2019 epidemic and kidneys, Kidney Int, doi:10.1016/j.kint.2020.03.001
Nashiry, Sumi, Islam, Quinn, Moni, Bioinformatics and system biology approach to identify the influences of COVID-19 on cardiovascular and hypertensive comorbidities, Brief Bioinform, doi:10.1093/bib/bbaa426
Ng, Hirsch, Hazzan, Outcomes among patients hospitalized with COVID-19 and acute kidney injury, Am J Kidney Dis, doi:10.1053/j.ajkd.2020.09.002
Oussalah, Gleye, Urmes, Long-term ACE Inhibitor/ARB use is associated with severe renal dysfunction and acute kidney injury in patients with severe COVID-19: results from a referral center cohort in the Northeast of France, Clin Infect Dis, doi:10.1093/cid/ciaa677
Patel, Verma, COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence?, JAMA, doi:10.1001/jama.2020.4812
Peng, He, Xue, Yang, Liu et al., Role of hypertension on the severity of COVID-19: a review, J Cardiovasc Pharmacol, doi:10.1097/FJC.0000000000001116
Pranata, Henrina, Lim, Clinical frailty scale and mortality in COVID-19: a systematic review and dose-response meta-analysis, Arch Gerontol Geriatr, doi:10.1016/j.archger.2020.104324
Puelles, Lutgehetmann, Lindenmeyer, Multiorgan and renal tropism of SARS-CoV-2, N Engl J Med, doi:10.1056/NEJMc2011400
Qian, Li, Peng, Gao, Cai et al., Association between hypertension and prognosis of patients with COVID-19: a systematic review and meta-analysis, Clin Exp Hypertens, doi:10.1080/10641963.2022.2071914
Rostami, Mastrangelo, Einollahi, A prospective study on risk factors for acute kidney injury and all-cause mortality in hospitalized COVID-19 patients from Tehran (Iran), Front Immunol, doi:10.3389/fimmu.2022.874426
Schiffrin, Flack, Ito, Muntner, Webb, Hypertension and COVID-19, Am J Hypertens, doi:10.1093/ajh/hpaa057
Shah, Khan, Dhurandhar, Hegde, The triumvirate: why hypertension, obesity, and diabetes are risk factors for adverse effects in patients with COVID-19, Acta Diabetol, doi:10.1007/s00592-020-01636-z
Shalaeva, Shadmanov, Azizova, Is lone hypertension a risk factor for more severe COVID-19 outcomes?, Glob Heart, doi:10.5334/gh.1099
Shi, Yu, Zhao, Wang, Zhao et al., Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan, Crit Care, doi:10.1186/s13054-020-2833-7
Shibata, Arima, Asayama, Hypertension and related diseases in the era of COVID-19: a report from the Japanese Society of Hypertension Task Force on COVID-19, Hypertens Res, doi:10.1038/s41440-020-0515-0
Simon, Jauslin, Rueegg, Association of frailty with adverse outcomes in patients with suspected COVID-19 infection, J Clin Med, doi:10.3390/jcm10112472
Simonnet, Chetboun, Poissy, High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obes, doi:10.1002/oby.22831
Synowiec, Szczepanski, Barreto-Duran, Lie, Pyrc, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): a Systemic Infection, Clin Microbiol Rev, doi:10.1128/CMR.00133-20
Tehrani, Killander, Astrand, Jakobsson, Gille-Johnson, Risk factors for death in adult COVID-19 patients: frailty predicts fatal outcome in older patients, Int J Infect Dis, doi:10.1016/j.ijid.2020.10.071
Wang, Hu, Hu, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, Clinical Interventions in Aging, doi:10.1001/jama.2020.1585
Wu, Chen, Cai, Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 Pneumonia in Wuhan, China, JAMA Intern Med, doi:10.1001/jamainternmed.2020.0994
Yan, Zuo, Cheng, Acute kidney injury is associated with in-hospital mortality in older patients with COVID-19, J Gerontol: Series A, doi:10.1093/gerona/glaa181
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.2147/cia.s431271",
"ISSN": [
"1178-1998"
],
"URL": "http://dx.doi.org/10.2147/cia.s431271",
"author": [
{
"affiliation": [],
"family": "Xu",
"given": "Qun",
"sequence": "first"
},
{
"affiliation": [],
"family": "Li",
"given": "Fangzhou",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Xujiao",
"sequence": "additional"
}
],
"container-title": "Clinical Interventions in Aging",
"container-title-short": "CIA",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
11,
20
]
],
"date-time": "2023-11-20T04:55:11Z",
"timestamp": 1700456111000
},
"deposited": {
"date-parts": [
[
2023,
11,
20
]
],
"date-time": "2023-11-20T04:55:13Z",
"timestamp": 1700456113000
},
"indexed": {
"date-parts": [
[
2023,
11,
21
]
],
"date-time": "2023-11-21T00:10:10Z",
"timestamp": 1700525410535
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
11
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
11,
1
]
],
"date-time": "2023-11-01T00:00:00Z",
"timestamp": 1698796800000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=94479",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=94479",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "1905-1921",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2023,
11
]
]
},
"published-online": {
"date-parts": [
[
2023,
11
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1038/s41564-020-0695-z",
"author": "Gorbalenya",
"doi-asserted-by": "publisher",
"first-page": "536",
"journal-title": "Nat Microbiol",
"key": "ref1",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "141",
"journal-title": "Nat Rev Microbiol",
"key": "ref2",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2022.874426",
"author": "Rostami",
"doi-asserted-by": "publisher",
"first-page": "874426",
"journal-title": "Front Immunol",
"key": "ref3",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"author": "Cheng",
"doi-asserted-by": "publisher",
"first-page": "829",
"journal-title": "Kidney Int",
"key": "ref4",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Lancet",
"key": "ref5",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.5394",
"author": "Grasselli",
"doi-asserted-by": "publisher",
"first-page": "1574",
"journal-title": "JAMA",
"key": "ref6",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.4812",
"author": "Patel",
"doi-asserted-by": "publisher",
"first-page": "1769",
"journal-title": "JAMA",
"key": "ref7",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1093/bib/bbaa426",
"author": "Nashiry",
"doi-asserted-by": "publisher",
"first-page": "1387",
"journal-title": "Brief Bioinform",
"key": "ref8",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1183/13993003.00547-2020",
"author": "Guan",
"doi-asserted-by": "publisher",
"first-page": "2000547",
"journal-title": "Eur Respir J",
"key": "ref9",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1097/FJC.0000000000001116",
"author": "Peng",
"doi-asserted-by": "publisher",
"first-page": "e648",
"journal-title": "J Cardiovasc Pharmacol",
"key": "ref10",
"volume": "78",
"year": "2021"
},
{
"DOI": "10.1007/s40292-022-00506-9",
"author": "Gallo",
"doi-asserted-by": "publisher",
"first-page": "115",
"journal-title": "High Blood Press Cardiovasc Prev",
"key": "ref11",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1111/jch.14417",
"author": "Bepouka",
"doi-asserted-by": "publisher",
"first-page": "99",
"journal-title": "Jl Clin Hypertens",
"key": "ref12",
"volume": "24",
"year": "2022"
},
{
"DOI": "10.1093/ajh/hpaa057",
"author": "Schiffrin",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "Am J Hypertens",
"key": "ref13",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1002/oby.22831",
"author": "Simonnet",
"doi-asserted-by": "publisher",
"first-page": "1195",
"journal-title": "Obes",
"key": "ref14",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "934",
"journal-title": "JAMA Intern Med",
"key": "ref15",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(19)31785-4",
"author": "Dent",
"doi-asserted-by": "publisher",
"first-page": "1376",
"journal-title": "Lancet",
"key": "ref16",
"volume": "394",
"year": "2019"
},
{
"DOI": "10.1016/j.archger.2020.104324",
"author": "Pranata",
"doi-asserted-by": "publisher",
"first-page": "104324",
"journal-title": "Arch Gerontol Geriatr",
"key": "ref17",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1038/s41440-020-0515-0",
"author": "Shibata",
"doi-asserted-by": "publisher",
"first-page": "1028",
"journal-title": "Hypertens Res",
"key": "ref18",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1007/s00592-020-01636-z",
"author": "Shah",
"doi-asserted-by": "publisher",
"first-page": "831",
"journal-title": "Acta Diabetol",
"key": "ref19",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1038/jhh.2013.55",
"author": "Mennuni",
"doi-asserted-by": "publisher",
"first-page": "74",
"journal-title": "J Hum Hypertens",
"key": "ref20",
"volume": "28",
"year": "2014"
},
{
"DOI": "10.1038/nrneph.2009.234",
"author": "Chronopoulos",
"doi-asserted-by": "publisher",
"first-page": "141",
"journal-title": "Nat Rev Nephrol",
"key": "ref21",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.1681/ASN.2010090934",
"author": "Anderson",
"doi-asserted-by": "publisher",
"first-page": "28",
"journal-title": "J Am Soc Nephrol",
"key": "ref22",
"volume": "22",
"year": "2011"
},
{
"DOI": "10.1002/path.2111",
"author": "Martin",
"doi-asserted-by": "publisher",
"first-page": "198",
"journal-title": "J Pathol",
"key": "ref23",
"volume": "211",
"year": "2007"
},
{
"DOI": "10.1016/j.kint.2020.05.006",
"author": "Hirsch",
"doi-asserted-by": "publisher",
"first-page": "209",
"journal-title": "Kidney Int",
"key": "ref24",
"volume": "98",
"year": "2020"
},
{
"DOI": "10.1016/j.ebiom.2022.103817",
"author": "Gu",
"doi-asserted-by": "publisher",
"first-page": "103817",
"journal-title": "Ebiomedicine",
"key": "ref25",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.1053/j.ajkd.2020.09.002",
"author": "Ng",
"doi-asserted-by": "publisher",
"first-page": "204",
"journal-title": "Am J Kidney Dis",
"key": "ref26",
"volume": "77",
"year": "2021"
},
{
"DOI": "10.55730/1300-0144.5488",
"author": "Küçük",
"doi-asserted-by": "publisher",
"first-page": "1495",
"journal-title": "Turk J Med Sci",
"key": "ref27",
"volume": "52",
"year": "2022"
},
{
"DOI": "10.1038/s41572-021-00284-z",
"author": "Kellum",
"doi-asserted-by": "publisher",
"first-page": "52",
"journal-title": "Nat Rev Dis Primers",
"key": "ref28",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/j.jaci.2020.04.006",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "110",
"journal-title": "J Allergy Clin Immunol",
"key": "ref29",
"volume": "146",
"year": "2020"
},
{
"DOI": "10.1186/s13054-020-2833-7",
"author": "Shi",
"doi-asserted-by": "publisher",
"first-page": "108",
"journal-title": "Crit Care",
"key": "ref30",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1061",
"journal-title": "JAMA",
"key": "ref31",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1002/jmv.28128",
"author": "Abdalla",
"doi-asserted-by": "publisher",
"journal-title": "J Med Virol",
"key": "ref32",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.5334/gh.1099",
"author": "Shalaeva",
"doi-asserted-by": "publisher",
"first-page": "17",
"journal-title": "Glob Heart",
"key": "ref33",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1080/10641963.2022.2071914",
"author": "Qian",
"doi-asserted-by": "publisher",
"first-page": "451",
"journal-title": "Clin Exp Hypertens",
"key": "ref34",
"volume": "44",
"year": "2022"
},
{
"DOI": "10.1136/bmj.m1985",
"author": "Docherty",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "ref35",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.10.071",
"author": "Tehrani",
"doi-asserted-by": "publisher",
"first-page": "415",
"journal-title": "Int J Infect Dis",
"key": "ref36",
"volume": "102",
"year": "2021"
},
{
"DOI": "10.1208/s12248-020-00532-2",
"author": "Majumder",
"doi-asserted-by": "publisher",
"first-page": "14",
"journal-title": "Aaps J",
"key": "ref37",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.3390/jcm10112472",
"author": "Simon",
"doi-asserted-by": "publisher",
"first-page": "2472",
"journal-title": "J Clin Med",
"key": "ref38",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1097/HJH.0000000000002666",
"author": "Mancusi",
"doi-asserted-by": "publisher",
"first-page": "376",
"journal-title": "J Hypertens",
"key": "ref39",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.120.15324",
"author": "Iaccarino",
"doi-asserted-by": "publisher",
"first-page": "366",
"journal-title": "Hypertens",
"key": "ref40",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1128/CMR.00133-20",
"author": "Synowiec",
"doi-asserted-by": "publisher",
"journal-title": "Clin Microbiol Rev",
"key": "ref41",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1016/S2666-5247(20)30004-5",
"author": "Chu",
"doi-asserted-by": "publisher",
"first-page": "e14",
"journal-title": "Lancet Microbe",
"key": "ref42",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.04.004",
"author": "Monteil",
"doi-asserted-by": "publisher",
"first-page": "905",
"journal-title": "Cell",
"key": "ref43",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2020040432",
"author": "Farkash",
"doi-asserted-by": "publisher",
"first-page": "1683",
"journal-title": "J Am Soc Nephrol",
"key": "ref44",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1038/s41467-021-22781-1",
"author": "Diao",
"doi-asserted-by": "publisher",
"journal-title": "Nat Commun",
"key": "ref45",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.kint.2020.03.001",
"author": "Naicker",
"doi-asserted-by": "publisher",
"first-page": "824",
"journal-title": "Kidney Int",
"key": "ref46",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.1093/gerona/glaa089",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "1788",
"journal-title": "J Gerontol: Series A",
"key": "ref47",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1093/gerona/glaa181",
"author": "Yan",
"doi-asserted-by": "publisher",
"first-page": "456",
"journal-title": "J Gerontol: Series A",
"key": "ref48",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1093/cid/ciaa677",
"author": "Oussalah",
"doi-asserted-by": "publisher",
"journal-title": "Clin Infect Dis",
"key": "ref49",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2011400",
"author": "Puelles",
"doi-asserted-by": "publisher",
"first-page": "590",
"journal-title": "N Engl J Med",
"key": "ref50",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehaa794",
"author": "Jiang",
"doi-asserted-by": "publisher",
"first-page": "4580",
"journal-title": "Eur Heart J",
"key": "ref51",
"volume": "41",
"year": "2020"
}
],
"reference-count": 51,
"references-count": 51,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/factors-affecting-mortality-in-elderly-hypertensive-hospitalized-patie-peer-reviewed-fulltext-article-CIA"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Geriatrics and Gerontology",
"General Medicine"
],
"subtitle": [],
"title": "Factors Affecting Mortality in Elderly Hypertensive Hospitalized Patients with COVID-19: A Retrospective Study",
"type": "journal-article",
"volume": "Volume 18"
}
xu9