The effect of favipiravir versus hydroxychloroquine on clinical and laboratory findings in COVID-19 in healthcare workers
et al., The Brazilian Journal of Infectious Diseases, doi:10.1016/j.bjid.2022.102328, Feb 2022
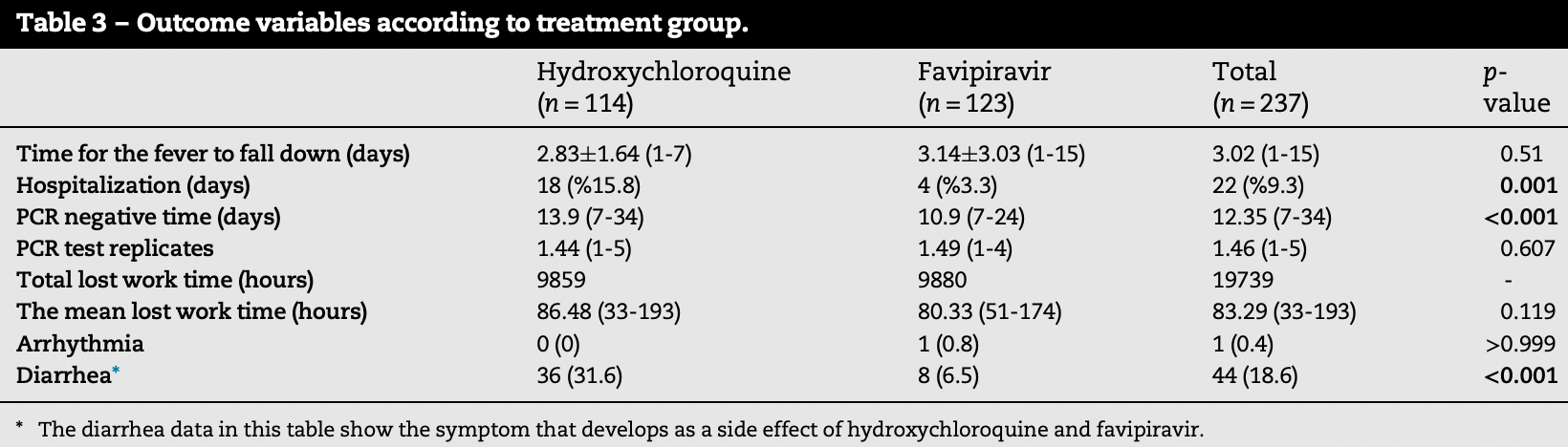
Retrospective 237 low-risk healthcare workers in Turkey, 123 treated with favipiravir and 114 treated with HCQ, showing lower hospitalization and faster viral clearance with favipiravir, and similar improvement. This study is subject to substantial confounding by time because the patients in each group are from different time periods with an overall period of 10 months including the beginning of the pandemic, resulting in significant differences in variants encountered and SOC. Propensity for hospital admission may also have changed significantly.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
This study is excluded in meta-analysis:
substantial confounding by time likely due to separation of groups in different time periods over an extended period of time.
|
risk of hospitalization, 79.4% lower, RR 0.21, p = 0.001, treatment 4 of 123 (3.3%), control 18 of 114 (15.8%), NNT 8.0.
|
|
recovery time, 11.0% higher, relative time 1.11, p = 0.51, treatment 123, control 114.
|
|
time to viral-, 21.6% lower, relative time 0.78, p < 0.001, treatment 123, control 114.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Turan et al., 1 Feb 2022, retrospective, Turkey, peer-reviewed, mean age 33.4, 10 authors, study period 11 March, 2020 - 1 January, 2021, this trial compares with another treatment - results may be better when compared to placebo.
The effect of favipiravir versus hydroxychloroquine on clinical and laboratory findings in COVID-19 in healthcare workers
The Brazilian Journal of Infectious Diseases, doi:10.1016/j.bjid.2022.102328
Objectives: Comparative data on hydroxychloroquine and favipiravir, commonly used agents in the treatment of Coronavirus Disease-2019 (COVID-19), are still limited. In this study, it was aimed to compare treatment outcomes in healthcare workers with COVID-19 who were prospectively followed by the occupational health and safety unit. Methods: A total of 237 healthcare-workers, diagnosed as mild or moderate COVID-19 between March 11, 2020 and January 1, 2021, were given hydroxychloroquine (n = 114) or favipiravir (n = 123). Clinical and laboratory findings were evaluated.
Results: The mean age of the patients was 33.4 §11.5 years. The mean time to negative PCR was found to be significantly shorter in patients receiving favipiravir compared to the hydroxychloroquine group (10.9 vs. 13.9 days; p < 0.001). The rate of hospitalization in the hydroxychloroquine group was significantly higher than favipiravir group (15.8% vs. 3.3%). In terms of side effects; the frequency of diarrhea in patients receiving hydroxychloroquine was significantly higher than that in the favipiravir group (31.6% vs. 6.5%; p < 0.001). Conclusions: Favipiravir and hydroxychloroquine were similar in terms of improvement of clinical symptoms of healthcare workers with mild or moderate COVID-19 infection, but favipiravir was significantly more effective in reducing viral load and hospitalization rates. Furthermore, favipiravir caused significantly less side-effects than hydroxychloroquine.
References
Agrawal, Raju, Udwadia, Favipiravir: a new and emerging antiviral option in COVID-19, Med J Armed Forces India, doi:10.1016/j.mjafi.2020.08.004
Cai, Yang, Liu, Experimental treatment with favipiravir for COVID-19: an open-label control study, Engineering, doi:10.1016/j.eng.2020.03.007
Cap, Bilge, Isik, The effect of favipiravir on QTcinterval in patients hospitalized with coronavirus disease
Coomes, Haghbayan, Favipiravir, an antiviralfor COVID-19?, J Antimicrob Chemother, doi:10.1093/jac/dkaa171
Costanzo, Giglio, Roviello, SARS-CoV-2: recent reports on antiviral therapies based on lopinavir/ritonavir, darunavir/umifenovir, hydroxychloroquine, remdesivir, favipiravir and other drugs for the treatment of the new coronavirus, Curr Med Chem, doi:10.2174/0929867327666200416131117
Covid-, This finding indicates that if SARS-CoV-2 PCR neg-284 ativity is expected, lost work time can be reduced. 285 The present study had some limitations. In order to make 286 a direct comparison of hydroxychloroquine and favipiravir 287 and to avoid bias, patients who received these agents in com-288 bination with other drugs
Doi, Hibino, Hase, A prospective, randomized, open-label trial of early versus late favipiravir therapy in hospitalized patients with COVID-19, Antimicrob Agents Chemother, doi:10.1128/AAC.01897-20
Elavarasi, Prasad, Seth, Chloroquine and hydroxychloroquine for the treatment of COVID-19: a systematic review and meta-analysis, J Gen Intern Med, doi:10.1007/s11606-020-06146-w
Furuta, Komeno, Nakamura, Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase, Proc Jpn Acad Ser B, doi:10.2183/pjab.93.027
Ghasemnejad-Berenji, Pashapour, Favipiravir and COVID-19: a simplified summary, Drug Res, doi:10.1055/a-1296-7935
Hernandez, Roman, Pasupuleti, Barboza, White, Hydroxychloroquine or chloroquine for treatment or prophylaxis of COVID-19: a living systematic review, Ann Intern Med, doi:10.7326/M20-2496
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 315 and COVID-19, Nat Rev Microbiol, doi:10.1038/s41579-020-00459-7
Ib Añez, Martínez, Valenzuela, Silva, Valenzuela, Hydroxychloroquineand chloroquine in COVID-19: should they be used as standard therapy?, Clin Rheumatol, doi:10.1007/s10067-020-05202-4
Izci-Cetinkaya, Karag€ Oz, Yildiz, Comparison of liver safety of favipiravir and hydroxychloroquine in COVID-19 treatment, Klimik Derg, doi:10.5152/kd.2020.49
Joshi, Parkar, Ansari, Role of favipiravir in the treatment of COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.10.069
Kaptein, Jacobs, Langendries, Favipiravir at highdoses has potent antiviral activity in SARS-CoV-2-infected hamsters, whereas hydroxychloroquine lacks activity, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2014441117
Mehta, Mazer-Amirshahi, Alkindi, Pourmand, Pharmacotherapy in COVID-19; A narrative review for 319 emergency providers, Am J Emerg Med, doi:10.1016/j.ajem.2020.04.035
Shrestha, Budhathoki, Khadka, Shah, Pokharel et al., Favipiravir versus other antiviral or standard of care for COVID-19 treatment: a rapid systematic review and metaanalysis, Virol J, doi:10.1186/s12985-020-01412-z
Sinha, Balayla, Hydroxychloroquine and COVID-19, Postgrad Med J, doi:10.1136/postgradmedj-2020-137785
Therefore, favipiravir is thought to be a useful agent in the 305 treatment of mild or moderate COVID-19 infection
Therefore, lost work time was 276 similar in patients who received hydroxychloroquine or favi-277 piravir
Yousefi, Valizadeh, Ghaffari, Vahedi, Karbalaei et al., A global treatments for coronaviruses including COVID-19, J Cell Physiol, doi:10.1002/jcp.29785
DOI record:
{
"DOI": "10.1016/j.bjid.2022.102328",
"ISSN": [
"1413-8670"
],
"URL": "http://dx.doi.org/10.1016/j.bjid.2022.102328",
"alternative-id": [
"S1413867022000174"
],
"article-number": "102328",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-7505-341X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Turan",
"given": "Derya Bayırlı",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-1193-2079",
"affiliation": [],
"authenticated-orcid": false,
"family": "Menteş",
"given": "Mehtap",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2621-1511",
"affiliation": [],
"authenticated-orcid": false,
"family": "Özel",
"given": "Yıldıran",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0585-8797",
"affiliation": [],
"authenticated-orcid": false,
"family": "Şerefhanoğlu",
"given": "Kıvanç",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7652-6880",
"affiliation": [],
"authenticated-orcid": false,
"family": "Aydoğan",
"given": "Burcu",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7838-7290",
"affiliation": [],
"authenticated-orcid": false,
"family": "İbil",
"given": "Neşe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5870-6426",
"affiliation": [],
"authenticated-orcid": false,
"family": "Güneşdoğdu",
"given": "Füsun",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2494-0083",
"affiliation": [],
"authenticated-orcid": false,
"family": "Orucova",
"given": "Hijran Mammadova",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7459-9210",
"affiliation": [],
"authenticated-orcid": false,
"family": "Saltürk",
"given": "Cüneyt",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0059-1667",
"affiliation": [],
"authenticated-orcid": false,
"family": "Çelik",
"given": "Hakan",
"sequence": "additional"
}
],
"container-title": [
"The Brazilian Journal of Infectious Diseases"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
2,
1
]
],
"date-time": "2022-02-01T23:11:37Z",
"timestamp": 1643757097000
},
"deposited": {
"date-parts": [
[
2022,
2,
6
]
],
"date-time": "2022-02-06T12:43:59Z",
"timestamp": 1644151439000
},
"indexed": {
"date-parts": [
[
2022,
2,
6
]
],
"date-time": "2022-02-06T13:11:16Z",
"timestamp": 1644153076304
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "1413-8670"
}
],
"issued": {
"date-parts": [
[
2022,
2
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
1
]
],
"date-time": "2022-02-01T00:00:00Z",
"timestamp": 1643673600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
28
]
],
"date-time": "2022-01-28T00:00:00Z",
"timestamp": 1643328000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1413867022000174?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1413867022000174?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "102328",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
2
]
]
},
"published-print": {
"date-parts": [
[
2022,
2
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1038/s41579-020-00459-7",
"article-title": "Characteristics of SARS-CoV-2 and COVID-19",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "141",
"journal-title": "Nat Rev Microbiol",
"key": "10.1016/j.bjid.2022.102328_bib0001",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1016/j.ajem.2020.04.035",
"article-title": "Pharmacotherapy in COVID-19; A narrative review for emergency providers",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "1488",
"journal-title": "Am J Emerg Med",
"key": "10.1016/j.bjid.2022.102328_bib0002",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1002/jcp.29785",
"article-title": "A global treatments for coronaviruses including COVID-19",
"author": "Yousefi",
"doi-asserted-by": "crossref",
"first-page": "9133",
"journal-title": "J Cell Physiol",
"key": "10.1016/j.bjid.2022.102328_bib0003",
"volume": "235",
"year": "2020"
},
{
"DOI": "10.1136/postgradmedj-2020-137785",
"article-title": "Hydroxychloroquine and COVID-19",
"author": "Sinha",
"doi-asserted-by": "crossref",
"first-page": "550",
"journal-title": "Postgrad Med J",
"key": "10.1016/j.bjid.2022.102328_bib0004",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.1093/jac/dkaa171",
"article-title": "Favipiravir, an antiviralfor COVID-19?",
"author": "Coomes",
"doi-asserted-by": "crossref",
"first-page": "2013",
"journal-title": "J Antimicrob Chemother",
"key": "10.1016/j.bjid.2022.102328_bib0005",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1007/s11606-020-06146-w",
"article-title": "Chloroquine and hydroxychloroquine for the treatment of COVID-19: a systematic review and meta-analysis",
"author": "Elavarasi",
"doi-asserted-by": "crossref",
"first-page": "3308",
"journal-title": "J Gen Intern Med",
"key": "10.1016/j.bjid.2022.102328_bib0006",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1016/j.mjafi.2020.08.004",
"article-title": "Favipiravir: a new and emerging antiviral option in COVID-19",
"author": "Agrawal",
"doi-asserted-by": "crossref",
"first-page": "370",
"journal-title": "Med J Armed Forces India",
"key": "10.1016/j.bjid.2022.102328_bib0007",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.2174/0929867327666200416131117",
"article-title": "SARS-CoV-2: recent reports on antiviral therapies based on lopinavir/ritonavir, darunavir/umifenovir, hydroxychloroquine, remdesivir, favipiravir and other drugs for the treatment of the new coronavirus",
"author": "Costanzo",
"doi-asserted-by": "crossref",
"first-page": "4536",
"journal-title": "Curr Med Chem",
"key": "10.1016/j.bjid.2022.102328_bib0008",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.2183/pjab.93.027",
"article-title": "Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase",
"author": "Furuta",
"doi-asserted-by": "crossref",
"first-page": "449",
"journal-title": "Proc Jpn Acad Ser B",
"key": "10.1016/j.bjid.2022.102328_bib0009",
"volume": "93",
"year": "2017"
},
{
"DOI": "10.1007/s10067-020-05202-4",
"article-title": "Hydroxychloroquineand chloroquine in COVID-19: should they be used as standard therapy?",
"author": "Ibáñez",
"doi-asserted-by": "crossref",
"first-page": "2461",
"journal-title": "Clin Rheumatol",
"key": "10.1016/j.bjid.2022.102328_bib0010",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.7326/M20-2496",
"article-title": "Hydroxychloroquine or chloroquine for treatment or prophylaxis of COVID-19: a living systematic review",
"author": "Hernandez",
"doi-asserted-by": "crossref",
"first-page": "287",
"journal-title": "Ann Intern Med",
"key": "10.1016/j.bjid.2022.102328_bib0011",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.1016/j.eng.2020.03.007",
"article-title": "Experimental treatment with favipiravir for COVID-19: an open-label control study",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "1192",
"journal-title": "Engineering",
"key": "10.1016/j.bjid.2022.102328_bib0012",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2014441117",
"article-title": "Favipiravir at highdoses has potent antiviral activity in SARS-CoV-2-infected hamsters, whereas hydroxychloroquine lacks activity",
"author": "Kaptein",
"doi-asserted-by": "crossref",
"first-page": "26955",
"journal-title": "Proc Natl Acad Sci U S A",
"key": "10.1016/j.bjid.2022.102328_bib0013",
"volume": "117",
"year": "2020"
},
{
"DOI": "10.1128/AAC.01897-20",
"article-title": "A prospective, randomized, open-label trial of early versus late favipiravir therapy in hospitalized patients with COVID-19",
"author": "Doi",
"doi-asserted-by": "crossref",
"journal-title": "Antimicrob Agents Chemother",
"key": "10.1016/j.bjid.2022.102328_bib0014",
"volume": "64",
"year": "2020"
},
{
"DOI": "10.1055/a-1296-7935",
"article-title": "Favipiravir and COVID-19: a simplified summary",
"author": "Ghasemnejad-Berenji",
"doi-asserted-by": "crossref",
"first-page": "166",
"journal-title": "Drug Res",
"key": "10.1016/j.bjid.2022.102328_bib0015",
"volume": "71",
"year": "2021"
},
{
"DOI": "10.1186/s12985-020-01412-z",
"article-title": "Favipiravir versus other antiviral or standard of care for COVID-19 treatment: a rapid systematic review and meta-analysis",
"author": "Shrestha",
"doi-asserted-by": "crossref",
"first-page": "141",
"journal-title": "Virol J",
"key": "10.1016/j.bjid.2022.102328_bib0016",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.10.069",
"article-title": "Role of favipiravir in the treatment of COVID-19",
"author": "Joshi",
"doi-asserted-by": "crossref",
"first-page": "501",
"journal-title": "Int J Infect Dis",
"key": "10.1016/j.bjid.2022.102328_bib0017",
"volume": "102",
"year": "2021"
},
{
"DOI": "10.5152/kd.2020.49",
"article-title": "Comparison of liver safety of favipiravir and hydroxychloroquine in COVID-19 treatment",
"author": "Izci-Cetinkaya",
"doi-asserted-by": "crossref",
"first-page": "235",
"journal-title": "Klimik Derg",
"key": "10.1016/j.bjid.2022.102328_bib0018",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1016/j.jelectrocard.2020.10.015",
"article-title": "The effect of favipiravir on QTcinterval in patients hospitalized with coronavirus disease 2019",
"author": "Cap",
"doi-asserted-by": "crossref",
"first-page": "115",
"journal-title": "J Electrocardiol",
"key": "10.1016/j.bjid.2022.102328_bib0019",
"volume": "63",
"year": "2020"
}
],
"reference-count": 19,
"references-count": 19,
"relation": {},
"score": 1,
"short-container-title": [
"The Brazilian Journal of Infectious Diseases"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Microbiology (medical)"
],
"subtitle": [],
"title": [
"The effect of favipiravir versus hydroxychloroquine on clinical and laboratory findings in COVID-19 in healthcare workers"
],
"type": "journal-article"
}