Vitamin C Deficiency in Blood Samples of COVID-19 Patients
et al., Antioxidants, doi:10.3390/antiox11081580, Aug 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
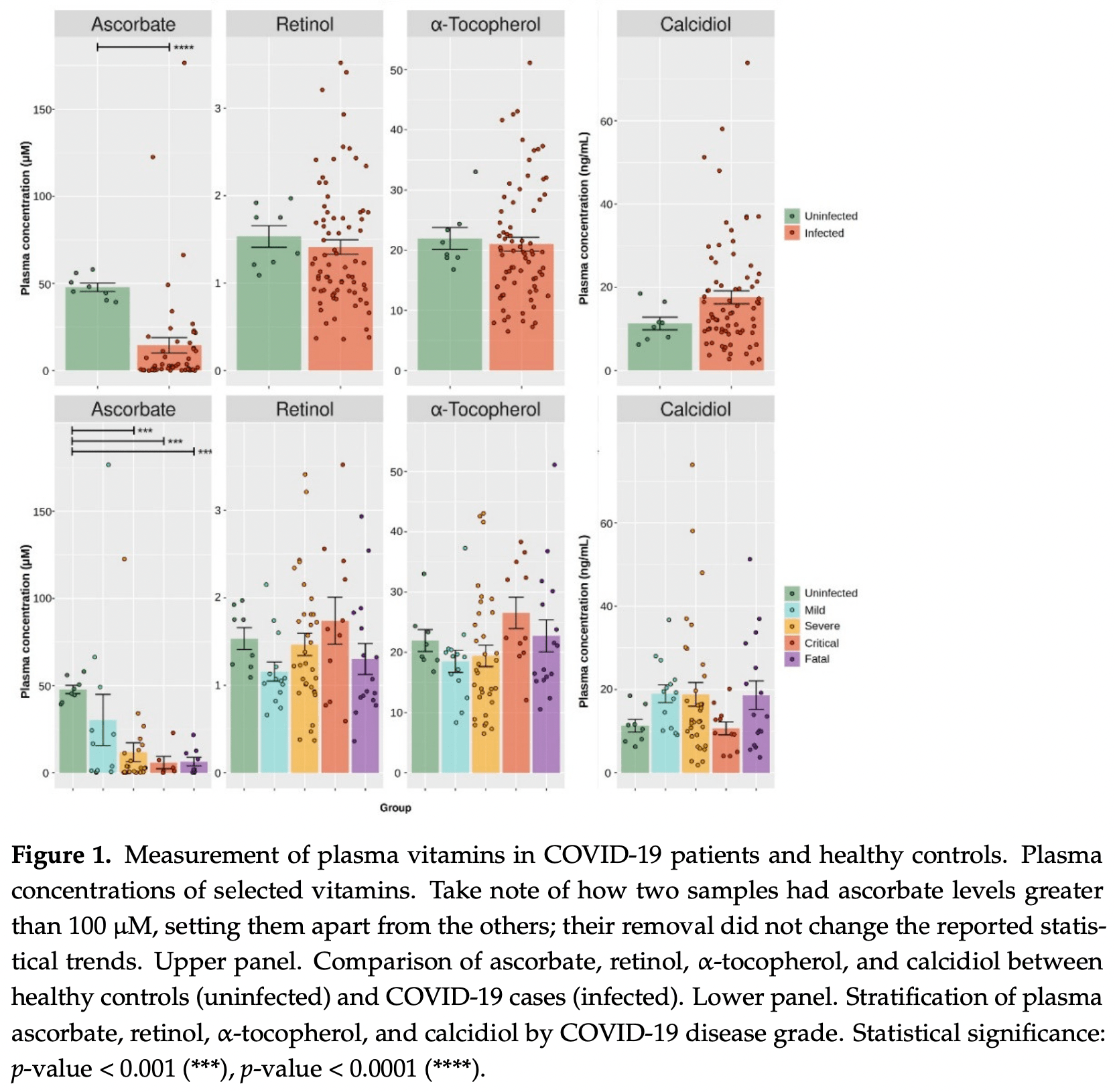
Analysis of 74 COVID-19 patients and 8 controls in Germany, showing low vitamin C levels associated with mortality. There was no significant difference for vitamin A, D, or E levels. Very few group details are provided, for example the age of patients in the control group and each severity group is not provided.
Sinnberg et al., 15 Aug 2022, retrospective, Germany, peer-reviewed, 15 authors, study period February 2020 - November 2020.
Contact: luigi.marongiu@uni-tuebingen.de (corresponding author), sascha.venturelli@uni-hohenheim.de.
Vitamin C Deficiency in Blood Samples of COVID-19 Patients
Antioxidants, doi:10.3390/antiox11081580
Coronavirus disease 2019 (COVID-19) is the most notable pandemic of the modern era. A relationship between ascorbate (vitamin C) and COVID-19 severity is well known, whereas the role of other vitamins is less understood. The present study compared the blood levels of four vitamins in a cohort of COVID-19 patients with different severities and uninfected individuals. Serum concentrations of ascorbate, calcidiol, retinol, and α-tocopherol were measured in a cohort of 74 COVID-19 patients and 8 uninfected volunteers. The blood levels were statistically compared and additional co-morbidity factors were considered. COVID-19 patients had significantly lower plasma ascorbate levels than the controls (p-value < 0.001), and further stratification revealed that the controls had higher levels than fatal, critical, and severe COVID-19 cases (p-values < 0.001). However, no such trend was observed for calcidiol, retinol, or α-tocopherol (p-value ≥ 0.093). Survival analysis showed that plasma ascorbate below 11.4 µM was associated with a lengthy hospitalization and a high risk of death. The results indicated that COVID-19 cases had depleted blood ascorbate associated with poor medical conditions, confirming the role of this vitamin in the outcome of COVID-19 infection.
Conflicts of Interest: The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
Ahammed, Anjum, Rahman, Haider, Kock et al., Estimation of novel coronavirus (COVID-19) reproduction number and case fatality rate: A systematic review and meta-analysis, Health Sci. Rep, doi:10.1002/hsr2.274
Alimohamadi, Tola, Abbasi-Ghahramanloo, Janani, Sepandi, Case fatality rate of COVID-19: A systematic review and meta-analysis, J. Prev. Med. Hyg, doi:10.15167/2421-4248/jpmh2021.62.2.1627
Arvinte, Singh, Marik, Serum Levels of Vitamin C and Vitamin D in a Cohort of Critically Ill COVID-19 Patients of a North American Community Hospital Intensive Care Unit in May 2020: A Pilot Study, Med. Drug Discov
Bowie, O'neill, Vitamin C Inhibits NF-κB Activation by TNF via the Activation of p38 Mitogen-Activated Protein Kinase, J. Immunol, doi:10.4049/jimmunol.165.12.7180
Braiman, Latitude Dependence of the COVID-19 Mortality Rate-A Possible Relationship to Vitamin D Deficiency?, SSRN, doi:10.2139/ssrn.3561958
Brant, Tian, Majerciak, Yang, Zheng, SARS-CoV-2: From its discovery to genome structure, transcription, and replication, Cell Biosci, doi:10.1186/s13578-021-00643-z
Busse, Chow, Mccurdy, Khanna, COVID-19 and the RAAS-a potential role for angiotensin II?, Crit. Care, doi:10.1186/s13054-020-02862-1
Caballero-García, Pérez-Valdecantos, Guallar, Caballero-Castillo, Roche et al., Effect of Vitamin D Supplementation on Muscle Status in Old Patients Recovering from COVID-19 Infection, Medicina
Calder, Nutrition, immunity and COVID-19, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000085
Carr, Rosengrave, Bayer, Chambers, Mehrtens et al., Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes, Crit. Care, doi:10.1186/s13054-017-1891-y
Carr, Spencer, Dixon, Chambers, Patients with Community Acquired Pneumonia Exhibit Depleted Vitamin C Status and Elevated Oxidative Stress, Nutrients, doi:10.3390/nu12051318
Carstensen, Plummer, Laara, Hills, Epi, A Package for Statistical Analysis in Epidemiology
Casadevall, Pirofski, In fatal COVID-19, the immune response can control the virus but kill the patient, doi:10.1073/pnas.2021128117
Cecchini, Cecchini, SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression, Med. Hypotheses, doi:10.1016/j.mehy.2020.110102
Chen, Luo, Yuan, Wang, Yang et al., Vitamin C Mitigates Oxidative Stress and Tumor Necrosis Factor-Alpha in Severe Community-Acquired Pneumonia and LPS-Induced Macrophages, Mediat. Inflamm, doi:10.1155/2014/426740
Chiscano-Camón, Ruiz-Rodriguez, Ruiz-Sanmartin, Roca, Ferrer, Vitamin C levels in patients with SARS-CoV-2-associated acute respiratory distress syndrome, Crit. Care, doi:10.1186/s13054-020-03249-y
Crook, Horgas, Yoon, Grundmann, Johnson-Mallard, Insufficient Vitamin C Levels among Adults in the United States: Results from the NHANES Surveys, 2003-2006, Nutrients, doi:10.3390/nu13113910
Cucinotta, Vanelli, WHO Declares COVID-19 a Pandemic, Acta Bio-Med. Atenei Parm, doi:10.23750/abm.v91i1.9397
Erol, Saglam, Saglam, Erol, Altun et al., The Protection Potential of Antioxidant Vitamins Against Acute Respiratory Distress Syndrome: A Rat Trial, Inflammation, doi:10.1007/s10753-019-01020-2
Fisher, Kraskauskas, Martin, Farkas, Wegelin et al., None
Frese, Schmerer, Wortmann, Schürmann, König et al., Imaging of SARS-CoV-2 infected Vero E6 cells by helium ion microscopy, Beilstein J. Nanotechnol, doi:10.3762/bjnano.12.13
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hati, Bhattacharyya, Impact of Thiol-Disulfide Balance on the Binding of COVID-19 Spike Protein with Angiotensin-Converting Enzyme 2 Receptor, ACS Omega, doi:10.1021/acsomega.0c02125
Hemilä, Carr, Chalker, Vitamin C May Increase the Recovery Rate of Outpatient Cases of SARS-CoV-2 Infection by 70%: Reanalysis of the COVID A to Z Randomized Clinical Trial, Front. Immunol, doi:10.3389/fimmu.2021.674681
Hemilä, Chalker, Vitamin C Can Shorten the Length of Stay in the ICU: A Meta-Analysis, Nutrients, doi:10.3390/nu11040708
Hiedra, Lo, Elbashabsheh, Gul, Wright et al., The use of IV vitamin C for patients with COVID-19: A case series, Expert Rev. Anti-Infect. Ther, doi:10.1080/14787210.2020.1794819
Hodges, What's new about scurvy?, Am. J. Clin. Nutr, doi:10.1093/ajcn/24.4.383
Holford, Carr, Jovic, Ali, Whitaker et al., Vitamin C-An Adjunctive Therapy for Respiratory Infection, Sepsis and COVID-19, Nutrients, doi:10.3390/nu12123760
Holford, Carr, Zawari, Vizcaychipi, Vitamin C Intervention for Critical COVID-19: A Pragmatic Review of the Current Level of Evidence, Life, doi:10.3390/life11111166
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat. Rev. Microbiol
Jackson, Farzan, Chen, Choe, Mechanisms of SARS-CoV-2 entry into cells, Nat. Rev. Mol. Cell Biol, doi:10.1038/s41580-021-00418-x
Jacob, Skala, Omaye, Biochemical indices of human vitamin C status, Am. J. Clin. Nutr
Jamalimoghadamsiahkali, Zarezade, Koolaji, Seyedalinaghi, Zendehdel et al., Safety and effectiveness of high-dose vitamin C in patients with COVID-19: A randomized open-label clinical trial, Eur. J. Med. Res, doi:10.1186/s40001-021-00490-1
Jovic, Ali, Ibrahim, Jessop, Tarassoli et al., Could Vitamins Help in the Fight against COVID-19?, Nutrients, doi:10.3390/nu12092550
Kumari, Dembra, Dembra, Bhawna, Gul et al., The Role of Vitamin C as Adjuvant Therapy in COVID-19, Cureus, doi:10.7759/cureus.11779
Lauer, Burkard, Niessner, Leischner, Renner et al., Ex Vivo Evaluation of the Sepsis Triple Therapy High-Dose Vitamin C in Combination with Vitamin B1 and Hydrocortisone in a Human Peripheral Blood Mononuclear Cells (PBMCs) Model, Nutrients, doi:10.3390/nu13072366
Li, Fan, Lai, Han, Li et al., Coronavirus infections and immune responses, J. Med. Virol, doi:10.1002/jmv.25685
Li, Tong, Bare, Devlin, Assessment of the Association of Vitamin D Level with SARS-CoV-2 Seropositivity among Working-Age Adults, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.11634
Mccartney, Byrne, Optimisation of Vitamin D Status for Enhanced Immuno-protection against COVID-19, Ir. Med. J
Meyerowitz-Katz, Merone, A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates, Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis, doi:10.1016/j.ijid.2020.09.1464
Milani, Macchi, Guz-Mark, Vitamin C in the Treatment of COVID-19, Nutrients, doi:10.3390/nu13041172
Muhammad, Kani, Iliya, Muhammad, Binji et al., Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: A cross-sectional comparative study in Jigawa, Northwestern Nigeria, SAGE Open Med, doi:10.1177/2050312121991246
Natarajan, Mechanisms of attenuation of abdominal sepsis induced acute lung injury by ascorbic acid, Am. J. Physiol.-Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00300.2011
Pauling, Vitamin C and common cold, JAMA, doi:10.1001/jama.1971.03180280086025
Pinnawala, Thrastardottir, Constantinou, Keeping a Balance during the Pandemic: A Narrative Review on the Important Role of Micronutrients in Preventing Infection and Reducing Complications of COVID-19, Curr. Nutr. Rep, doi:10.1007/s13668-021-00356-2
Quek, Ooi, Teng, Chan, Ng et al., Zinc and vitamin C intake increases spike and neutralising antibody production following SARS-CoV-2 infection, Clin. Transl. Med, doi:10.1002/ctm2.731
Ranieri, Rubenfeld, Thompson, Ferguson, Caldwell et al., Acute respiratory distress syndrome: The Berlin Definition, JAMA, doi:10.1001/jama.2012.5669
Reider, Chung, Devarshi, Grant, Hazels Mitmesser, Inadequacy of Immune Health Nutrients: Intakes in US Adults, the 2005-2016 NHANES, Nutrients, doi:10.3390/nu12061735
Rothan, Byrareddy, The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak, J. Autoimmun, doi:10.1016/j.jaut.2020.102433
Sarohan, Kızıl, ˙inkaya, Mahmud, Akram et al., A novel hypothesis for COVID-19 pathogenesis: Retinol depletion and retinoid signaling disorder, Cell. Signal, doi:10.1016/j.cellsig.2021.110121
Suhail, Zajac, Fossum, Lowater, Mccracken et al., Role of Oxidative Stress on SARS-CoV (SARS) and SARS-CoV-2 (COVID-19) Infection: A Review, Protein J, doi:10.1007/s10930-020-09935-8
Tehrani, Yadegarynia, Abrishami, Moradi, Gharaei et al., An investigation into the Effects of Intravenous Vitamin C on Pulmonary CT Findings and Clinical Outcomes of Patients with COVID 19 Pneumonia A Randomized Clinical Trial, Urol. J, doi:10.22037/uj.v18i.6863
Tepasse, Vollenberg, Fobker, Kabar, Schmidt et al., Vitamin A Plasma Levels in COVID-19 Patients: A Prospective Multicenter Study and Hypothesis, Nutrients, doi:10.3390/nu13072173
Tomasa-Irriguible, Bielsa-Berrocal, COVID-19: Up to 82% critically ill patients had low Vitamin C values, Nutr. J, doi:10.1186/s12937-021-00727-z
Traber, Stevens, Vitamins, Beneficial effects from a mechanistic perspective, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2011.05.017
Tyml, Vitamin C and Microvascular Dysfunction in Systemic Inflammation, Antioxidants, doi:10.3390/antiox6030049
Vankadari, Wilce, Emerging WuHan (COVID-19) coronavirus: Glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1739565
Venturelli, Leischner, Helling, Burkard, Marongiu, Vitamins as Possible Cancer Biomarkers: Significance and Limitations, Nutrients, doi:10.3390/nu13113914
Venturelli, Sinnberg, Berger, Noor, Levesque et al., Epigenetic Impacts of Ascorbate on Human Metastatic Melanoma Cells, Front. Oncol, doi:10.3389/fonc.2014.00227
Venturelli, Sinnberg, Niessner, Busch, Molecular mechanisms of pharmacological doses of ascorbate on cancer cells, Wien. Med. Wochenschr, doi:10.1007/s10354-015-0356-7
Vollbracht, Kraft, Feasibility of Vitamin C in the Treatment of Post Viral Fatigue with Focus on Long COVID, Based on a Systematic Review of IV Vitamin C on Fatigue, Nutrients, doi:10.3390/nu13041154
Yamada, Shimojima, Narita, Tsukamoto, Kato et al., RIG-I-Like Receptor and Toll-Like Receptor Signaling Pathways Cause Aberrant Production of Inflammatory Cytokines/Chemokines in a Severe Fever with Thrombocytopenia Syndrome Virus Infection Mouse Model, J. Virol, doi:10.1128/JVI.02246-17
Yang, Wang, Liu, Shang, Cheng et al., Traditional Chinese medicine together with high-dose vitamin C improves the therapeutic effect of western medicine against COVID-19, Am. J. Transl. Res
Zabet, Mohammadi, Ramezani, Khalili, Effect of high-dose Ascorbic acid on vasopressor's requirement in septic shock, J. Res. Pharm. Pract, doi:10.4103/2279-042X.179569
Zhang, Rao, Li, Zhu, Liu et al., Pilot trial of high-dose vitamin C in critically ill COVID-19 patients, Ann. Intensive Care, doi:10.1186/s13613-020-00792-3
Zhang, Xiao, Cai, Chen, Structure of SARS-CoV-2 spike protein, Curr. Opin. Virol, doi:10.1016/j.coviro.2021.08.010
Zhao, Ling, Li, Peng, Huang et al., Beneficial aspects of high dose intravenous vitamin C on patients with COVID-19 pneumonia in severe condition: A retrospective case series study, Ann. Palliat. Med, doi:10.21037/apm-20-1387
Zhao, Liu, Liu, Peng, Huang et al., High Dose Intravenous Vitamin C for Preventing the Disease Aggravation of Moderate COVID-19 Pneumonia. A Retrospective Propensity Matched before-after Study, Front. Pharmacol, doi:10.3389/fphar.2021.638556
Zhou, Yang, Wang, Hu, Zhang et al., A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:10.1038/s41586-020-2012-7
DOI record:
{
"DOI": "10.3390/antiox11081580",
"ISSN": [
"2076-3921"
],
"URL": "http://dx.doi.org/10.3390/antiox11081580",
"abstract": "<jats:p>Coronavirus disease 2019 (COVID-19) is the most notable pandemic of the modern era. A relationship between ascorbate (vitamin C) and COVID-19 severity is well known, whereas the role of other vitamins is less understood. The present study compared the blood levels of four vitamins in a cohort of COVID-19 patients with different severities and uninfected individuals. Serum concentrations of ascorbate, calcidiol, retinol, and α-tocopherol were measured in a cohort of 74 COVID-19 patients and 8 uninfected volunteers. The blood levels were statistically compared and additional co-morbidity factors were considered. COVID-19 patients had significantly lower plasma ascorbate levels than the controls (p-value < 0.001), and further stratification revealed that the controls had higher levels than fatal, critical, and severe COVID-19 cases (p-values < 0.001). However, no such trend was observed for calcidiol, retinol, or α-tocopherol (p-value ≥ 0.093). Survival analysis showed that plasma ascorbate below 11.4 µM was associated with a lengthy hospitalization and a high risk of death. The results indicated that COVID-19 cases had depleted blood ascorbate associated with poor medical conditions, confirming the role of this vitamin in the outcome of COVID-19 infection.</jats:p>",
"alternative-id": [
"antiox11081580"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3922-3327",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sinnberg",
"given": "Tobias",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lichtensteiger",
"given": "Christa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hill-Mündel",
"given": "Katharina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leischner",
"given": "Christian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2542-7022",
"affiliation": [],
"authenticated-orcid": false,
"family": "Niessner",
"given": "Heike",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Busch",
"given": "Christian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Renner",
"given": "Olga",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wyss",
"given": "Nina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Flatz",
"given": "Lukas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4557-7730",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lauer",
"given": "Ulrich M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3759-2439",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hoelzle",
"given": "Ludwig E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nohr",
"given": "Donatus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burkard",
"given": "Markus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marongiu",
"given": "Luigi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Venturelli",
"given": "Sascha",
"sequence": "additional"
}
],
"container-title": "Antioxidants",
"container-title-short": "Antioxidants",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
16
]
],
"date-time": "2022-08-16T00:58:08Z",
"timestamp": 1660611488000
},
"deposited": {
"date-parts": [
[
2022,
8,
16
]
],
"date-time": "2022-08-16T08:06:31Z",
"timestamp": 1660637191000
},
"funder": [
{
"award": [
"D.30.21947, reference: GzV 1.14"
],
"name": "Else-Uebelmesser-Stiftung"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
16
]
],
"date-time": "2022-08-16T08:43:31Z",
"timestamp": 1660639411202
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2022,
8,
15
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2022,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
15
]
],
"date-time": "2022-08-15T00:00:00Z",
"timestamp": 1660521600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-3921/11/8/1580/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1580",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
8,
15
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
15
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/s41586-020-2012-7",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.23750/abm.v91i1.9397",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"key": "ref3",
"unstructured": "Coronavirus Research Center, Center for Systems Science and Engineering (CSSE) Baltimore, MD, USAhttps://coronavirus.jhu.edu/map.html"
},
{
"DOI": "10.1002/hsr2.274",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.15167/2421-4248/jpmh2021.62.2.1627",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.ijid.2020.09.1464",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1038/s41580-021-00418-x",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1186/s13578-021-00643-z",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3762/bjnano.12.13",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1016/j.coviro.2021.08.010",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1002/jmv.25685",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.jaut.2020.102433",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3390/nu11040708",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1007/s13668-021-00356-2",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.3390/medicina57101079",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1001/jama.1971.03180280086025",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.3390/nu13072366",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1007/s10753-019-01020-2",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1007/s10354-015-0356-7",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.3389/fonc.2014.00227",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1152/ajplung.00300.2011",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.3390/nu13041154",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.3389/fimmu.2021.674681",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.3390/nu13041172",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1128/JVI.02246-17",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.cellsig.2021.110121",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1073/pnas.2021128117",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.3390/nu13072173",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.3390/nu12092550",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"article-title": "Optimisation of Vitamin D Status for Enhanced Immuno-protection against COVID-19",
"author": "McCartney",
"first-page": "58",
"journal-title": "Ir. Med. J.",
"key": "ref33",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1080/22221751.2020.1739565",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.2139/ssrn.3561958",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1001/jama.2012.5669",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"key": "ref38",
"unstructured": "Epi: A Package for Statistical Analysis in Epidemiology; 2021https://CRAN.R-project.org/package=Epi"
},
{
"key": "ref39",
"series-title": "Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids",
"year": "2000"
},
{
"DOI": "10.3390/nu13113910",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1093/ajcn/46.5.818",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1093/ajcn/24.4.383",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.3390/nu13113914",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1016/j.medidd.2020.100064",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1186/s12937-021-00727-z",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1186/s13054-020-03249-y",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.3390/life11111166",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11634",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1186/s13054-017-1891-y",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.3390/nu12061735",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.4103/2279-042X.179569",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.21037/apm-20-1387",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.3389/fphar.2021.638556",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1186/s40001-021-00490-1",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1002/ctm2.731",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.4049/jimmunol.165.12.7180",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1155/2014/426740",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1186/s13613-020-00792-3",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1016/j.mehy.2020.110102",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1177/2050312121991246",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1016/j.freeradbiomed.2011.05.017",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1021/acsomega.0c02125",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1186/s13054-020-02862-1",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1007/s10930-020-09935-8",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.3390/nu12123760",
"doi-asserted-by": "publisher",
"key": "ref65"
},
{
"DOI": "10.3390/nu12051318",
"doi-asserted-by": "publisher",
"key": "ref66"
},
{
"DOI": "10.7759/cureus.11779",
"doi-asserted-by": "publisher",
"key": "ref67"
},
{
"article-title": "Traditional Chinese medicine together with high-dose vitamin C improves the therapeutic effect of western medicine against COVID-19",
"author": "Yang",
"first-page": "501",
"journal-title": "Am. J. Transl. Res.",
"key": "ref68",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.22037/uj.v18i.6863",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.3390/antiox6030049",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"DOI": "10.1080/14787210.2020.1794819",
"doi-asserted-by": "publisher",
"key": "ref71"
}
],
"reference-count": 71,
"references-count": 71,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-3921/11/8/1580"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cell Biology",
"Clinical Biochemistry",
"Molecular Biology",
"Biochemistry",
"Physiology"
],
"subtitle": [],
"title": "Vitamin C Deficiency in Blood Samples of COVID-19 Patients",
"type": "journal-article",
"volume": "11"
}
sinnberg
