Vitamin C Deficiency in Blood Samples of COVID-19 Patients
et al., Antioxidants, doi:10.3390/antiox11081580, Aug 2022
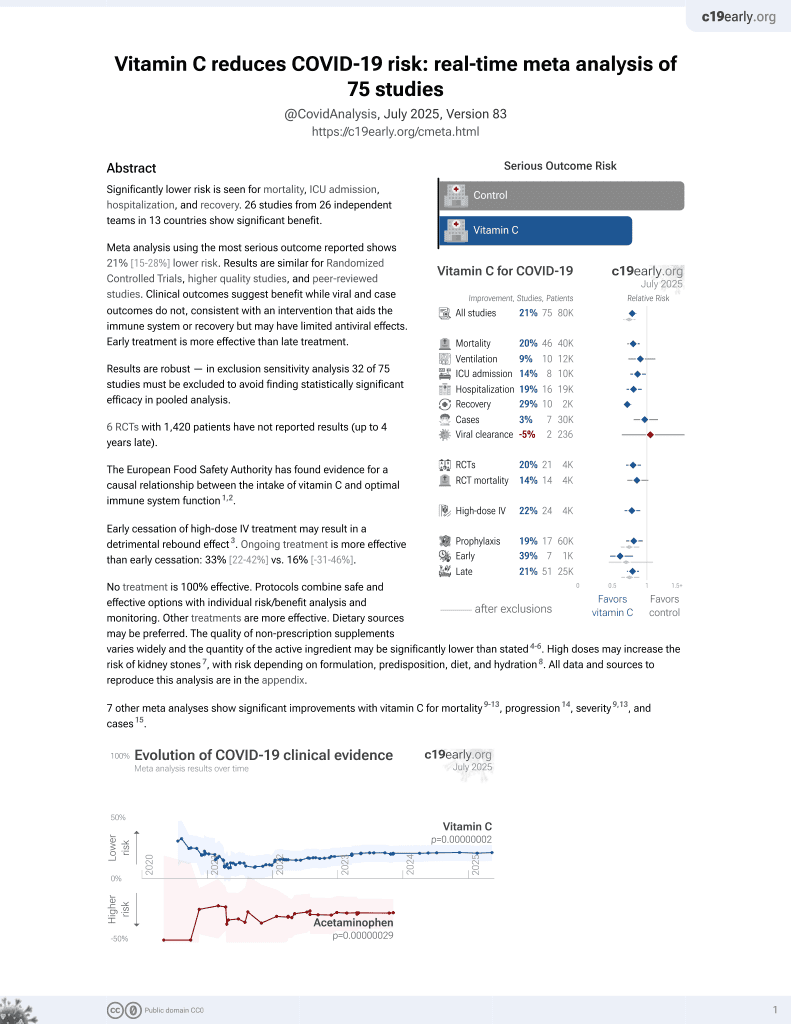
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000076 from 73 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 74 COVID-19 patients and 8 controls in Germany, showing low vitamin C levels associated with mortality. There was no significant difference for vitamin A, D, or E levels. Very few group details are provided, for example the age of patients in the control group and each severity group is not provided.
|
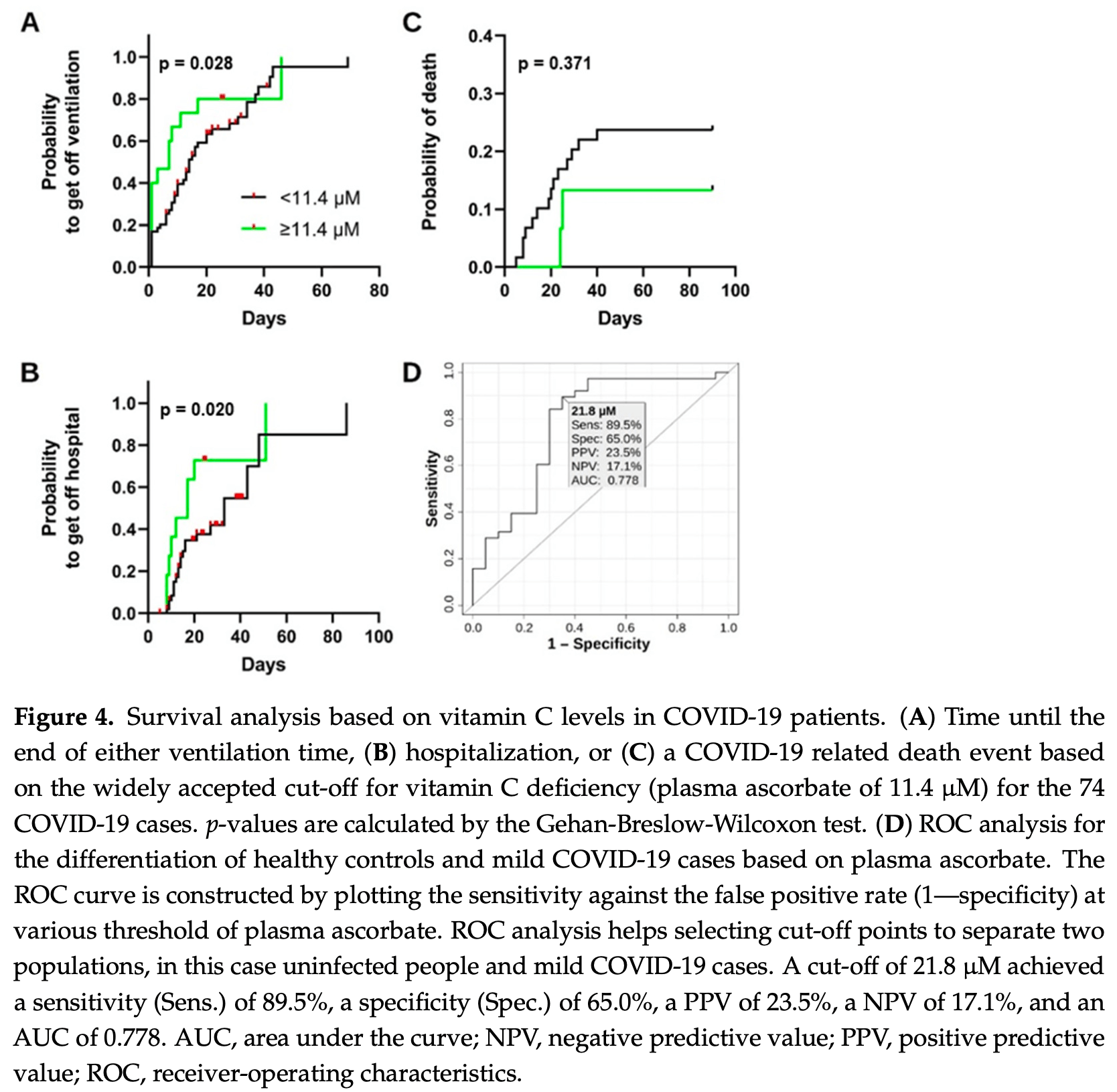
risk of death, 41.9% lower, HR 0.58, p = 0.38, high vitamin C levels (≥11.4μM) 0 of 15 (0.0%), low vitamin C levels (<11.4μM) 9 of 59 (15.3%), NNT 6.6, adjusted per study, inverted to make HR<1 favor high vitamin C levels (≥11.4μM), survival analysis.
|
|
risk of mechanical ventilation, 40.9% lower, HR 0.59, p = 0.17, high vitamin C levels (≥11.4μM) 15, low vitamin C levels (<11.4μM) 59, adjusted per study, ventilation time survival analysis.
|
|
risk of hospitalization, 60.7% lower, HR 0.39, p = 0.0498, high vitamin C levels (≥11.4μM) 15, low vitamin C levels (<11.4μM) 59, adjusted per study, hospitalization time survival analysis.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sinnberg et al., 15 Aug 2022, retrospective, Germany, peer-reviewed, 15 authors, study period February 2020 - November 2020.
Contact: luigi.marongiu@uni-tuebingen.de (corresponding author), sascha.venturelli@uni-hohenheim.de.
Vitamin C Deficiency in Blood Samples of COVID-19 Patients
Antioxidants, doi:10.3390/antiox11081580
Coronavirus disease 2019 (COVID-19) is the most notable pandemic of the modern era. A relationship between ascorbate (vitamin C) and COVID-19 severity is well known, whereas the role of other vitamins is less understood. The present study compared the blood levels of four vitamins in a cohort of COVID-19 patients with different severities and uninfected individuals. Serum concentrations of ascorbate, calcidiol, retinol, and α-tocopherol were measured in a cohort of 74 COVID-19 patients and 8 uninfected volunteers. The blood levels were statistically compared and additional co-morbidity factors were considered. COVID-19 patients had significantly lower plasma ascorbate levels than the controls (p-value < 0.001), and further stratification revealed that the controls had higher levels than fatal, critical, and severe COVID-19 cases (p-values < 0.001). However, no such trend was observed for calcidiol, retinol, or α-tocopherol (p-value ≥ 0.093). Survival analysis showed that plasma ascorbate below 11.4 µM was associated with a lengthy hospitalization and a high risk of death. The results indicated that COVID-19 cases had depleted blood ascorbate associated with poor medical conditions, confirming the role of this vitamin in the outcome of COVID-19 infection.
Conflicts of Interest: The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
Ahammed, Anjum, Rahman, Haider, Kock et al., Estimation of novel coronavirus (COVID-19) reproduction number and case fatality rate: A systematic review and meta-analysis, Health Sci. Rep, doi:10.1002/hsr2.274
Alimohamadi, Tola, Abbasi-Ghahramanloo, Janani, Sepandi, Case fatality rate of COVID-19: A systematic review and meta-analysis, J. Prev. Med. Hyg, doi:10.15167/2421-4248/jpmh2021.62.2.1627
Arvinte, Singh, Marik, Serum Levels of Vitamin C and Vitamin D in a Cohort of Critically Ill COVID-19 Patients of a North American Community Hospital Intensive Care Unit in May 2020: A Pilot Study, Med. Drug Discov
Bowie, O'neill, Vitamin C Inhibits NF-κB Activation by TNF via the Activation of p38 Mitogen-Activated Protein Kinase, J. Immunol, doi:10.4049/jimmunol.165.12.7180
Braiman, Latitude Dependence of the COVID-19 Mortality Rate-A Possible Relationship to Vitamin D Deficiency?, SSRN, doi:10.2139/ssrn.3561958
Brant, Tian, Majerciak, Yang, Zheng, SARS-CoV-2: From its discovery to genome structure, transcription, and replication, Cell Biosci, doi:10.1186/s13578-021-00643-z
Busse, Chow, Mccurdy, Khanna, COVID-19 and the RAAS-a potential role for angiotensin II?, Crit. Care, doi:10.1186/s13054-020-02862-1
Caballero-García, Pérez-Valdecantos, Guallar, Caballero-Castillo, Roche et al., Effect of Vitamin D Supplementation on Muscle Status in Old Patients Recovering from COVID-19 Infection, Medicina
Calder, Nutrition, immunity and COVID-19, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000085
Carr, Rosengrave, Bayer, Chambers, Mehrtens et al., Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes, Crit. Care, doi:10.1186/s13054-017-1891-y
Carr, Spencer, Dixon, Chambers, Patients with Community Acquired Pneumonia Exhibit Depleted Vitamin C Status and Elevated Oxidative Stress, Nutrients, doi:10.3390/nu12051318
Carstensen, Plummer, Laara, Hills, Epi, A Package for Statistical Analysis in Epidemiology
Casadevall, Pirofski, In fatal COVID-19, the immune response can control the virus but kill the patient, doi:10.1073/pnas.2021128117
Cecchini, Cecchini, SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression, Med. Hypotheses, doi:10.1016/j.mehy.2020.110102
Chen, Luo, Yuan, Wang, Yang et al., Vitamin C Mitigates Oxidative Stress and Tumor Necrosis Factor-Alpha in Severe Community-Acquired Pneumonia and LPS-Induced Macrophages, Mediat. Inflamm, doi:10.1155/2014/426740
Chiscano-Camón, Ruiz-Rodriguez, Ruiz-Sanmartin, Roca, Ferrer, Vitamin C levels in patients with SARS-CoV-2-associated acute respiratory distress syndrome, Crit. Care, doi:10.1186/s13054-020-03249-y
Crook, Horgas, Yoon, Grundmann, Johnson-Mallard, Insufficient Vitamin C Levels among Adults in the United States: Results from the NHANES Surveys, 2003-2006, Nutrients, doi:10.3390/nu13113910
Cucinotta, Vanelli, WHO Declares COVID-19 a Pandemic, Acta Bio-Med. Atenei Parm, doi:10.23750/abm.v91i1.9397
Erol, Saglam, Saglam, Erol, Altun et al., The Protection Potential of Antioxidant Vitamins Against Acute Respiratory Distress Syndrome: A Rat Trial, Inflammation, doi:10.1007/s10753-019-01020-2
Fisher, Kraskauskas, Martin, Farkas, Wegelin et al., None
Frese, Schmerer, Wortmann, Schürmann, König et al., Imaging of SARS-CoV-2 infected Vero E6 cells by helium ion microscopy, Beilstein J. Nanotechnol, doi:10.3762/bjnano.12.13
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hati, Bhattacharyya, Impact of Thiol-Disulfide Balance on the Binding of COVID-19 Spike Protein with Angiotensin-Converting Enzyme 2 Receptor, ACS Omega, doi:10.1021/acsomega.0c02125
Hemilä, Carr, Chalker, Vitamin C May Increase the Recovery Rate of Outpatient Cases of SARS-CoV-2 Infection by 70%: Reanalysis of the COVID A to Z Randomized Clinical Trial, Front. Immunol, doi:10.3389/fimmu.2021.674681
Hemilä, Chalker, Vitamin C Can Shorten the Length of Stay in the ICU: A Meta-Analysis, Nutrients, doi:10.3390/nu11040708
Hiedra, Lo, Elbashabsheh, Gul, Wright et al., The use of IV vitamin C for patients with COVID-19: A case series, Expert Rev. Anti-Infect. Ther, doi:10.1080/14787210.2020.1794819
Hodges, What's new about scurvy?, Am. J. Clin. Nutr, doi:10.1093/ajcn/24.4.383
Holford, Carr, Jovic, Ali, Whitaker et al., Vitamin C-An Adjunctive Therapy for Respiratory Infection, Sepsis and COVID-19, Nutrients, doi:10.3390/nu12123760
Holford, Carr, Zawari, Vizcaychipi, Vitamin C Intervention for Critical COVID-19: A Pragmatic Review of the Current Level of Evidence, Life, doi:10.3390/life11111166
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat. Rev. Microbiol
Jackson, Farzan, Chen, Choe, Mechanisms of SARS-CoV-2 entry into cells, Nat. Rev. Mol. Cell Biol, doi:10.1038/s41580-021-00418-x
Jacob, Skala, Omaye, Biochemical indices of human vitamin C status, Am. J. Clin. Nutr
Jamalimoghadamsiahkali, Zarezade, Koolaji, Seyedalinaghi, Zendehdel et al., Safety and effectiveness of high-dose vitamin C in patients with COVID-19: A randomized open-label clinical trial, Eur. J. Med. Res, doi:10.1186/s40001-021-00490-1
Jovic, Ali, Ibrahim, Jessop, Tarassoli et al., Could Vitamins Help in the Fight against COVID-19?, Nutrients, doi:10.3390/nu12092550
Kumari, Dembra, Dembra, Bhawna, Gul et al., The Role of Vitamin C as Adjuvant Therapy in COVID-19, Cureus, doi:10.7759/cureus.11779
Lauer, Burkard, Niessner, Leischner, Renner et al., Ex Vivo Evaluation of the Sepsis Triple Therapy High-Dose Vitamin C in Combination with Vitamin B1 and Hydrocortisone in a Human Peripheral Blood Mononuclear Cells (PBMCs) Model, Nutrients, doi:10.3390/nu13072366
Li, Fan, Lai, Han, Li et al., Coronavirus infections and immune responses, J. Med. Virol, doi:10.1002/jmv.25685
Li, Tong, Bare, Devlin, Assessment of the Association of Vitamin D Level with SARS-CoV-2 Seropositivity among Working-Age Adults, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.11634
Mccartney, Byrne, Optimisation of Vitamin D Status for Enhanced Immuno-protection against COVID-19, Ir. Med. J
Meyerowitz-Katz, Merone, A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates, Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis, doi:10.1016/j.ijid.2020.09.1464
Milani, Macchi, Guz-Mark, Vitamin C in the Treatment of COVID-19, Nutrients, doi:10.3390/nu13041172
Muhammad, Kani, Iliya, Muhammad, Binji et al., Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: A cross-sectional comparative study in Jigawa, Northwestern Nigeria, SAGE Open Med, doi:10.1177/2050312121991246
Natarajan, Mechanisms of attenuation of abdominal sepsis induced acute lung injury by ascorbic acid, Am. J. Physiol.-Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00300.2011
Pauling, Vitamin C and common cold, JAMA, doi:10.1001/jama.1971.03180280086025
Pinnawala, Thrastardottir, Constantinou, Keeping a Balance during the Pandemic: A Narrative Review on the Important Role of Micronutrients in Preventing Infection and Reducing Complications of COVID-19, Curr. Nutr. Rep, doi:10.1007/s13668-021-00356-2
Quek, Ooi, Teng, Chan, Ng et al., Zinc and vitamin C intake increases spike and neutralising antibody production following SARS-CoV-2 infection, Clin. Transl. Med, doi:10.1002/ctm2.731
Ranieri, Rubenfeld, Thompson, Ferguson, Caldwell et al., Acute respiratory distress syndrome: The Berlin Definition, JAMA, doi:10.1001/jama.2012.5669
Reider, Chung, Devarshi, Grant, Hazels Mitmesser, Inadequacy of Immune Health Nutrients: Intakes in US Adults, the 2005-2016 NHANES, Nutrients, doi:10.3390/nu12061735
Rothan, Byrareddy, The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak, J. Autoimmun, doi:10.1016/j.jaut.2020.102433
Sarohan, Kızıl, ˙inkaya, Mahmud, Akram et al., A novel hypothesis for COVID-19 pathogenesis: Retinol depletion and retinoid signaling disorder, Cell. Signal, doi:10.1016/j.cellsig.2021.110121
Suhail, Zajac, Fossum, Lowater, Mccracken et al., Role of Oxidative Stress on SARS-CoV (SARS) and SARS-CoV-2 (COVID-19) Infection: A Review, Protein J, doi:10.1007/s10930-020-09935-8
Tehrani, Yadegarynia, Abrishami, Moradi, Gharaei et al., An investigation into the Effects of Intravenous Vitamin C on Pulmonary CT Findings and Clinical Outcomes of Patients with COVID 19 Pneumonia A Randomized Clinical Trial, Urol. J, doi:10.22037/uj.v18i.6863
Tepasse, Vollenberg, Fobker, Kabar, Schmidt et al., Vitamin A Plasma Levels in COVID-19 Patients: A Prospective Multicenter Study and Hypothesis, Nutrients, doi:10.3390/nu13072173
Tomasa-Irriguible, Bielsa-Berrocal, COVID-19: Up to 82% critically ill patients had low Vitamin C values, Nutr. J, doi:10.1186/s12937-021-00727-z
Traber, Stevens, Vitamins, Beneficial effects from a mechanistic perspective, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2011.05.017
Tyml, Vitamin C and Microvascular Dysfunction in Systemic Inflammation, Antioxidants, doi:10.3390/antiox6030049
Vankadari, Wilce, Emerging WuHan (COVID-19) coronavirus: Glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1739565
Venturelli, Leischner, Helling, Burkard, Marongiu, Vitamins as Possible Cancer Biomarkers: Significance and Limitations, Nutrients, doi:10.3390/nu13113914
Venturelli, Sinnberg, Berger, Noor, Levesque et al., Epigenetic Impacts of Ascorbate on Human Metastatic Melanoma Cells, Front. Oncol, doi:10.3389/fonc.2014.00227
Venturelli, Sinnberg, Niessner, Busch, Molecular mechanisms of pharmacological doses of ascorbate on cancer cells, Wien. Med. Wochenschr, doi:10.1007/s10354-015-0356-7
Vollbracht, Kraft, Feasibility of Vitamin C in the Treatment of Post Viral Fatigue with Focus on Long COVID, Based on a Systematic Review of IV Vitamin C on Fatigue, Nutrients, doi:10.3390/nu13041154
Yamada, Shimojima, Narita, Tsukamoto, Kato et al., RIG-I-Like Receptor and Toll-Like Receptor Signaling Pathways Cause Aberrant Production of Inflammatory Cytokines/Chemokines in a Severe Fever with Thrombocytopenia Syndrome Virus Infection Mouse Model, J. Virol, doi:10.1128/JVI.02246-17
Yang, Wang, Liu, Shang, Cheng et al., Traditional Chinese medicine together with high-dose vitamin C improves the therapeutic effect of western medicine against COVID-19, Am. J. Transl. Res
Zabet, Mohammadi, Ramezani, Khalili, Effect of high-dose Ascorbic acid on vasopressor's requirement in septic shock, J. Res. Pharm. Pract, doi:10.4103/2279-042X.179569
Zhang, Rao, Li, Zhu, Liu et al., Pilot trial of high-dose vitamin C in critically ill COVID-19 patients, Ann. Intensive Care, doi:10.1186/s13613-020-00792-3
Zhang, Xiao, Cai, Chen, Structure of SARS-CoV-2 spike protein, Curr. Opin. Virol, doi:10.1016/j.coviro.2021.08.010
Zhao, Ling, Li, Peng, Huang et al., Beneficial aspects of high dose intravenous vitamin C on patients with COVID-19 pneumonia in severe condition: A retrospective case series study, Ann. Palliat. Med, doi:10.21037/apm-20-1387
Zhao, Liu, Liu, Peng, Huang et al., High Dose Intravenous Vitamin C for Preventing the Disease Aggravation of Moderate COVID-19 Pneumonia. A Retrospective Propensity Matched before-after Study, Front. Pharmacol, doi:10.3389/fphar.2021.638556
Zhou, Yang, Wang, Hu, Zhang et al., A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:10.1038/s41586-020-2012-7
DOI record:
{
"DOI": "10.3390/antiox11081580",
"ISSN": [
"2076-3921"
],
"URL": "http://dx.doi.org/10.3390/antiox11081580",
"abstract": "<jats:p>Coronavirus disease 2019 (COVID-19) is the most notable pandemic of the modern era. A relationship between ascorbate (vitamin C) and COVID-19 severity is well known, whereas the role of other vitamins is less understood. The present study compared the blood levels of four vitamins in a cohort of COVID-19 patients with different severities and uninfected individuals. Serum concentrations of ascorbate, calcidiol, retinol, and α-tocopherol were measured in a cohort of 74 COVID-19 patients and 8 uninfected volunteers. The blood levels were statistically compared and additional co-morbidity factors were considered. COVID-19 patients had significantly lower plasma ascorbate levels than the controls (p-value < 0.001), and further stratification revealed that the controls had higher levels than fatal, critical, and severe COVID-19 cases (p-values < 0.001). However, no such trend was observed for calcidiol, retinol, or α-tocopherol (p-value ≥ 0.093). Survival analysis showed that plasma ascorbate below 11.4 µM was associated with a lengthy hospitalization and a high risk of death. The results indicated that COVID-19 cases had depleted blood ascorbate associated with poor medical conditions, confirming the role of this vitamin in the outcome of COVID-19 infection.</jats:p>",
"alternative-id": [
"antiox11081580"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3922-3327",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sinnberg",
"given": "Tobias",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lichtensteiger",
"given": "Christa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hill-Mündel",
"given": "Katharina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leischner",
"given": "Christian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2542-7022",
"affiliation": [],
"authenticated-orcid": false,
"family": "Niessner",
"given": "Heike",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Busch",
"given": "Christian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Renner",
"given": "Olga",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wyss",
"given": "Nina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Flatz",
"given": "Lukas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4557-7730",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lauer",
"given": "Ulrich M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3759-2439",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hoelzle",
"given": "Ludwig E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nohr",
"given": "Donatus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burkard",
"given": "Markus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marongiu",
"given": "Luigi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Venturelli",
"given": "Sascha",
"sequence": "additional"
}
],
"container-title": "Antioxidants",
"container-title-short": "Antioxidants",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
16
]
],
"date-time": "2022-08-16T00:58:08Z",
"timestamp": 1660611488000
},
"deposited": {
"date-parts": [
[
2022,
8,
16
]
],
"date-time": "2022-08-16T08:06:31Z",
"timestamp": 1660637191000
},
"funder": [
{
"award": [
"D.30.21947, reference: GzV 1.14"
],
"name": "Else-Uebelmesser-Stiftung"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
16
]
],
"date-time": "2022-08-16T08:43:31Z",
"timestamp": 1660639411202
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2022,
8,
15
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2022,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
15
]
],
"date-time": "2022-08-15T00:00:00Z",
"timestamp": 1660521600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-3921/11/8/1580/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1580",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
8,
15
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
15
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/s41586-020-2012-7",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.23750/abm.v91i1.9397",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"key": "ref3",
"unstructured": "Coronavirus Research Center, Center for Systems Science and Engineering (CSSE) Baltimore, MD, USAhttps://coronavirus.jhu.edu/map.html"
},
{
"DOI": "10.1002/hsr2.274",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.15167/2421-4248/jpmh2021.62.2.1627",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.ijid.2020.09.1464",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1038/s41580-021-00418-x",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1186/s13578-021-00643-z",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3762/bjnano.12.13",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1016/j.coviro.2021.08.010",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1002/jmv.25685",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.jaut.2020.102433",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3390/nu11040708",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1007/s13668-021-00356-2",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.3390/medicina57101079",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1001/jama.1971.03180280086025",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.3390/nu13072366",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1007/s10753-019-01020-2",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1007/s10354-015-0356-7",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.3389/fonc.2014.00227",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1152/ajplung.00300.2011",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.3390/nu13041154",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.3389/fimmu.2021.674681",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.3390/nu13041172",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1128/JVI.02246-17",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.cellsig.2021.110121",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1073/pnas.2021128117",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.3390/nu13072173",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.3390/nu12092550",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"article-title": "Optimisation of Vitamin D Status for Enhanced Immuno-protection against COVID-19",
"author": "McCartney",
"first-page": "58",
"journal-title": "Ir. Med. J.",
"key": "ref33",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1080/22221751.2020.1739565",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.2139/ssrn.3561958",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1001/jama.2012.5669",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"key": "ref38",
"unstructured": "Epi: A Package for Statistical Analysis in Epidemiology; 2021https://CRAN.R-project.org/package=Epi"
},
{
"key": "ref39",
"series-title": "Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids",
"year": "2000"
},
{
"DOI": "10.3390/nu13113910",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1093/ajcn/46.5.818",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1093/ajcn/24.4.383",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.3390/nu13113914",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1016/j.medidd.2020.100064",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1186/s12937-021-00727-z",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1186/s13054-020-03249-y",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.3390/life11111166",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11634",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1186/s13054-017-1891-y",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.3390/nu12061735",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.4103/2279-042X.179569",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.21037/apm-20-1387",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.3389/fphar.2021.638556",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1186/s40001-021-00490-1",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1002/ctm2.731",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.4049/jimmunol.165.12.7180",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1155/2014/426740",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1186/s13613-020-00792-3",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1016/j.mehy.2020.110102",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1177/2050312121991246",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1016/j.freeradbiomed.2011.05.017",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1021/acsomega.0c02125",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1186/s13054-020-02862-1",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1007/s10930-020-09935-8",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.3390/nu12123760",
"doi-asserted-by": "publisher",
"key": "ref65"
},
{
"DOI": "10.3390/nu12051318",
"doi-asserted-by": "publisher",
"key": "ref66"
},
{
"DOI": "10.7759/cureus.11779",
"doi-asserted-by": "publisher",
"key": "ref67"
},
{
"article-title": "Traditional Chinese medicine together with high-dose vitamin C improves the therapeutic effect of western medicine against COVID-19",
"author": "Yang",
"first-page": "501",
"journal-title": "Am. J. Transl. Res.",
"key": "ref68",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.22037/uj.v18i.6863",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.3390/antiox6030049",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"DOI": "10.1080/14787210.2020.1794819",
"doi-asserted-by": "publisher",
"key": "ref71"
}
],
"reference-count": 71,
"references-count": 71,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-3921/11/8/1580"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cell Biology",
"Clinical Biochemistry",
"Molecular Biology",
"Biochemistry",
"Physiology"
],
"subtitle": [],
"title": "Vitamin C Deficiency in Blood Samples of COVID-19 Patients",
"type": "journal-article",
"volume": "11"
}
sinnberg