Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro
et al., Nutrients, doi:10.3390/nu13020328, Jan 2021
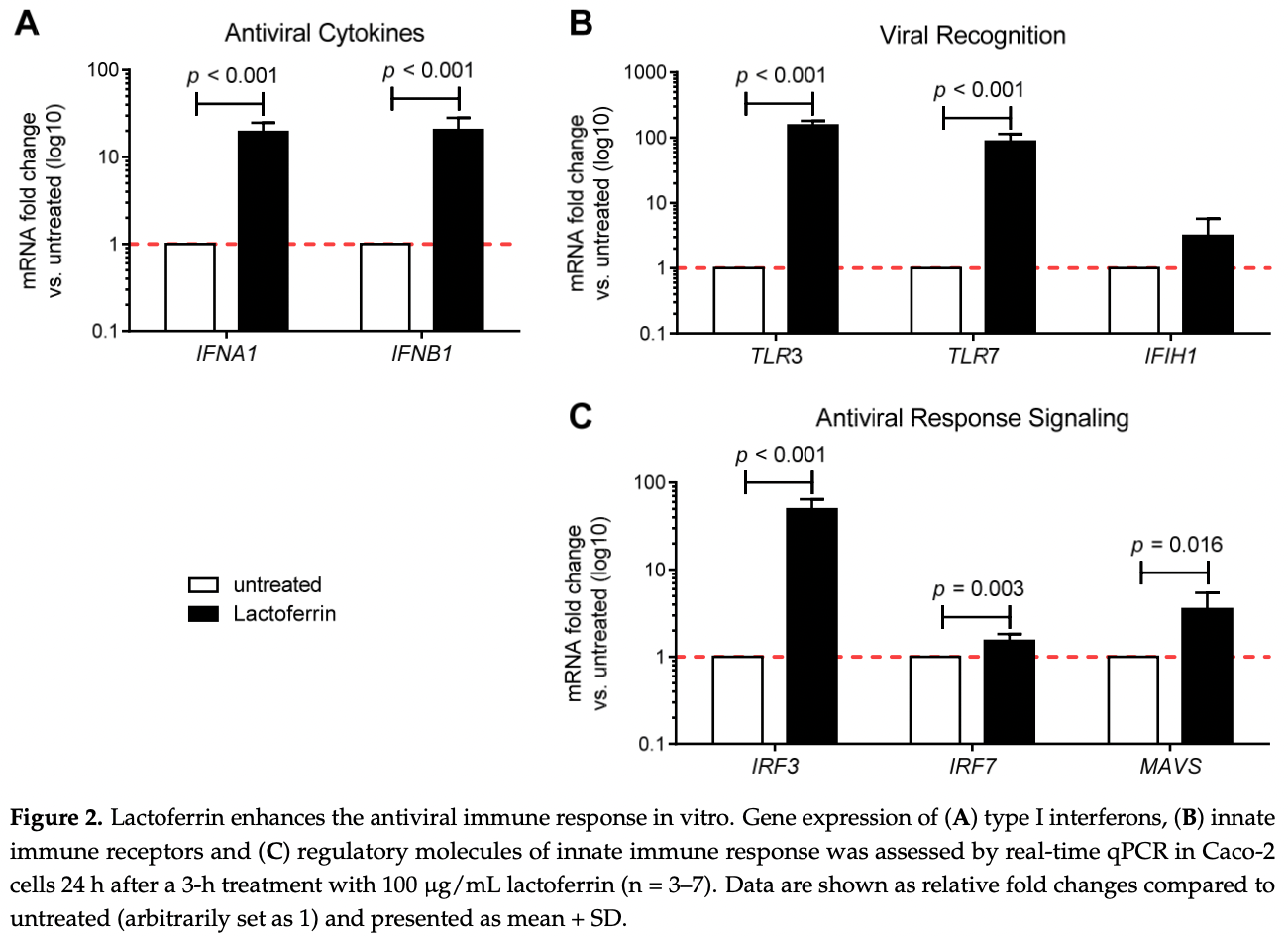
Caco-2 and Vero E6 in vitro study showing lactoferrin enhances the antiviral immune response, partially inhibits SARS-CoV-2 infection in Caco-2 intestinal epithelial cells, and modulates cytokine production.
18 preclinical studies support the efficacy of lactoferrin for COVID-19:
1.
da Silva et al., Immunomodulatory effect of bovine lactoferrin during SARS-CoV-2 infection, Frontiers in Immunology, doi:10.3389/fimmu.2024.1456634.
2.
Cutone et al., Lactoferrin binding to Sars-CoV-2 Spike glycoprotein protects host from infection, inflammation and iron dysregulation., Research Square, doi:10.21203/rs.3.rs-1605740/v1.
3.
Miotto et al., Molecular Mechanisms Behind Anti SARS-CoV-2 Action of Lactoferrin, Frontiers in Molecular Biosciences, doi:10.3389/fmolb.2021.607443.
4.
Babulic et al., Lactoferrin Binds through Its N-Terminus to the Receptor-Binding Domain of the SARS-CoV-2 Spike Protein, Pharmaceuticals, doi:10.3390/ph17081021.
5.
Yathindranath et al., Lipid Nanoparticle-Based Inhibitors for SARS-CoV-2 Host Cell Infection, International Journal of Nanomedicine, doi:10.2147/IJN.S448005.
6.
Alves et al., Inhibition of SARS-CoV-2 Infection in Vero Cells by Bovine Lactoferrin under Different Iron-Saturation States, Pharmaceuticals, doi:10.3390/ph16101352.
7.
Kobayashi-Sakamoto et al., Bovine lactoferrin suppresses the cathepsin-dependent pathway of SARS-CoV-2 entry in vitro, International Dairy Journal, doi:10.1016/j.idairyj.2023.105805.
8.
Andreu et al., Liposomal Lactoferrin Exerts Antiviral Activity against HCoV-229E and SARS-CoV-2 Pseudoviruses In Vitro, Viruses, doi:10.3390/v15040972.
9.
Yazawa et al., Evaluation of SARS-CoV-2 isolation in cell culture from nasal/nasopharyngeal swabs or saliva specimens of patients with COVID-19, Research Square, doi:10.21203/rs.3.rs-2676422/v1.
10.
Piacentini et al., Lactoferrin Inhibition of the Complex Formation between ACE2 Receptor and SARS CoV-2 Recognition Binding Domain, International Journal of Molecular Sciences, doi:10.3390/ijms23105436.
11.
Ostrov et al., Highly Specific Sigma Receptor Ligands Exhibit Anti-Viral Properties in SARS-CoV-2 Infected Cells, Pathogens, doi:10.3390/pathogens10111514.
12.
Mirabelli et al., Morphological cell profiling of SARS-CoV-2 infection identifies drug repurposing candidates for COVID-19, Proceedings of the National Academy of Sciences, doi:10.1073/pnas.2105815118.
13.
Salaris et al., Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro, Nutrients, doi:10.3390/nu13020328.
Salaris et al., 23 Jan 2021, peer-reviewed, 9 authors.
Contact: paola.brun.1@unipd.it (corresponding author), claudio.salaris@studenti.unipd.it, alice.bertolini@studenti.unipd.it, ignazio.castagliuolo@unipd.it, melania.scarpa@iov.veneto.it, marina.elli@aat-taa.eu, simone.guglielmetti@unimi.it, fabrizio.pregliasco@unimi.it, corrado.blandizzi@med.unipi.it.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro
Nutrients, doi:10.3390/nu13020328
SARS-CoV-2 is a newly emerging virus that currently lacks curative treatments. Lactoferrin (LF) is a naturally occurring non-toxic glycoprotein with broad-spectrum antiviral, immunomodulatory and anti-inflammatory effects. In this study, we assessed the potential of LF in the prevention of SARS-CoV-2 infection in vitro. Antiviral immune response gene expression was analyzed by qRT-PCR in uninfected Caco-2 intestinal epithelial cells treated with LF. An infection assay for SARS-CoV-2 was performed in Caco-2 cells treated or not with LF. SARS-CoV-2 titer was determined by qRT-PCR, plaque assay and immunostaining. Inflammatory and anti-inflammatory cytokine production was determined by qRT-PCR. LF significantly induced the expression of IFNA1, IFNB1, TLR3, TLR7, IRF3, IRF7 and MAVS genes. Furthermore, LF partially inhibited SARS-CoV-2 infection and replication in Caco-2 intestinal epithelial cells. Our in vitro data support LF as an immune modulator of the antiviral immune response with moderate effects against SARS-CoV-2 infection.
Conflicts of Interest: The authors declare no conflict of interest.
References
Actor, Hwang, Kruzel, Lactoferrin as a Natural Immune Modulator, Curr. Pharm. Des, doi:10.2174/138161209788453202
Andersen, Rambaut, Lipkin, Holmes, Garry, The Proximal Origin of SARS-CoV-2, Nat. Med, doi:10.1038/s41591-020-0820-9
Baveye, Elass, Mazurier, Spik, Legrand, Lactoferrin: A Multifunctional Glycoprotein Involved in the Modulation of the Inflammatory Process, Clin. Chem. Lab. Med, doi:10.1515/CCLM.1999.049
Buscarini, Manfredi, Brambilla, Menozzi, Londoni et al., GI Symptoms as Early Signs of COVID-19 in Hospitalised Italian Patients, Gut, doi:10.1136/gutjnl-2020-321434
Campione, Cosio, Rosa, Lanna, Di Girolamo et al., Lactoferrin as Protective Natural Barrier of Respiratory and Intestinal Mucosa against Coronavirus Infection and Inflammation, Int. J. Mol. Sci
Caprio, Infante, Calanchini, Mammi, Fabbri et al., Not Just the Bone. Evidence for Beneficial Pleiotropic Extraskeletal Effects, Eat Weight Disord, doi:10.1007/s40519-016-0312-6
Castillo, Entrenas Costa, Vaquero Barrios, Alcalá Díaz, López Miranda et al., Effect of Calcifediol Treatment and Best Available Therapy versus Best Available Therapy on Intensive Care Unit Admission and Mortality among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical Study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Chang, Ng, Sun, Lactoferrin as Potential Preventative and Adjunct Treatment for COVID-19, Int. J. Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.106118
Channappanavar, Fehr, Zheng, Wohlford-Lenane, Abrahante et al., IFN-I Response Timing Relative to Virus Replication Determines MERS Coronavirus Infection Outcomes, J. Clin. Investig, doi:10.1172/JCI126363
Clausen, Sandoval, Spliid, Pihl, Perrett et al., SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2, Cell, doi:10.1016/j.cell.2020.09.033
Convertino, Tuccori, Ferraro, Valdiserra, Cappello et al., Exploring Pharmacological Approaches for Managing Cytokine Storm Associated with Pneumonia and Acute Respiratory Distress Syndrome in COVID-19 Patients, Crit. Care, doi:10.1186/s13054-020-03020-3
Curran, Demick, Mansfield, Lactoferrin Activates Macrophages via TLR4-Dependent and -Independent Signaling Pathways, Cell Immunol, doi:10.1016/j.cellimm.2006.08.006
De Haan, Li, Te Lintelo, Bosch, Haijema et al., Murine Coronavirus with an Extended Host Range Uses Heparan Sulfate as an Entry Receptor, J. Virol, doi:10.1128/JVI.79.22.14451-14456.2005
Elnagdy, Alkhazindar, The Potential of Antimicrobial Peptides as an Antiviral Therapy against COVID-19, ACS Pharm. Transl. Sci, doi:10.1021/acsptsci.0c00059
Fabbri, Infante, Ricordi, Editorial-Vitamin D Status: A Key Modulator of Innate Immunity and Natural Defense from Acute Viral Respiratory Infections, Eur. Rev. Med. Pharm. Sci, doi:10.26355/eurrev_202004_20876
Fornasa, Tsilingiri, Caprioli, Botti, Mapelli et al., Dichotomy of Short and Long Thymic Stromal Lymphopoietin Isoforms in Inflammatory Disorders of the Bowel and Skin, J. Allergy Clin. Immunol, doi:10.1016/j.jaci.2015.04.011
Ghio, Carter, Dailey, Devlin, Samet, Respiratory Epithelial Cells Demonstrate Lactoferrin Receptors That Increase after Metal Exposure, Am. J. Physiol. Lung Cell. Mol. Physiol, doi:10.1152/ajplung.1999.276.6.L933
Glanville, Treatments and Vaccines for COVID-19: Authorised Medicines
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Honda, Taniguchi, IRFs: Master Regulators of Signalling by Toll-like Receptors and Cytosolic Pattern-Recognition Receptors, Nat. Rev. Immunol, doi:10.1038/nri1900
Ikeda, Nozaki, Sugiyama, Tanaka, Naganuma et al., Characterization of Antiviral Activity of Lactoferrin against Hepatitis C Virus Infection in Human Cultured Cells, Virus Res, doi:10.1016/S0168-1702(99)00121-5
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of Vitamin D Level among Asymptomatic and Critically Ill COVID-19 Patients and Its Correlation with Inflammatory Markers, Sci. Rep, doi:10.1038/s41598-020-77093-z
Jenssen, Hancock, Antimicrobial Properties of Lactoferrin, Biochimie, doi:10.1016/j.biochi.2008.05.015
Jiang, Lopez, Kelleher, Lönnerdal, Apo-and Holo-Lactoferrin Are Both Internalized by Lactoferrin Receptor via Clathrin-Mediated Endocytosis but Differentially Affect ERK-Signaling and Cell Proliferation in Caco-2 Cells, J. Cell Physiol, doi:10.1002/jcp.22650
Kawasaki, Kawai, Toll-Like Receptor Signaling Pathways, Front. Immunol, doi:10.3389/fimmu.2014.00461
Kell, Heyden, Pretorius, The Biology of Lactoferrin, an Iron-Binding Protein That Can Help Defend Against Viruses and Bacteria, Front. Immunol, doi:10.3389/fimmu.2020.01221
Lamers, Beumer, Van Der Vaart, Knoops, Puschhof et al., SARS-CoV-2 Productively Infects Human Gut Enterocytes, Science, doi:10.1126/science.abc1669
Lang, Yang, Deng, Liu, Yang et al., Inhibition of SARS Pseudovirus Cell Entry by Lactoferrin Binding to Heparan Sulfate Proteoglycans, PLoS ONE, doi:10.1371/journal.pone.0023710
Leung, Clinical Features of Deaths in the Novel Coronavirus Epidemic in China, Rev. Med Virol, doi:10.1002/rmv.2103
Lim, Ng, Tam, Liu, Human Coronaviruses: A Review of Virus-Host Interactions, Diseases, doi:10.3390/diseases4030026
Lopez, Nonnecke, Lönnerdal, The Lactoferrin Receptor Is Differentially Expressed across Several Human Epithelial Cell Types, FASEB J, doi:10.1096/fasebj.26.1_supplement.644.5
Machnicki, Zimecki, Zagulski, Lactoferrin Regulates the Release of Tumour Necrosis Factor Alpha and Interleukin 6 in Vivo, Int. J. Exp. Pathol
Martinez, Compounds with Therapeutic Potential against Novel Respiratory 2019 Coronavirus, Antimicrob. Agents Chemother, doi:10.1128/AAC.00399-20
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., HLH Across Speciality Collaboration, UK. COVID-19: Consider Cytokine Storm Syndromes and Immunosuppression, Lancet, doi:10.1016/S0140-6736(20)30628-0
Milewska, Zarebski, Nowak, Stozek, Potempa et al., Human Coronavirus NL63 Utilizes Heparan Sulfate Proteoglycans for Attachment to Target Cells, J. Virol, doi:10.1128/JVI.02078-14
Mrityunjaya, Pavithra, Neelam, Janhavi, Halami et al., Immune-Boosting, Antioxidant and Anti-Inflammatory Food Supplements Targeting Pathogenesis of COVID-19, Front. Immunol, doi:10.3389/fimmu.2020.570122
Ou, Liu, Lei, Li, Mi et al., Characterization of Spike Glycoprotein of SARS-CoV-2 on Virus Entry and Its Immune Cross-Reactivity with SARS-CoV, Nat. Commun, doi:10.1038/s41467-020-15562-9
Pereira, Dantas Damascena, Galvão Azevedo, De Almeida Oliveira, Da Mota Santana et al., Deficiency Aggravates COVID-19: Systematic Review and Meta-Analysis, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1841090
Pišlar, Mitrović, Sabotič, Fonović, Nanut et al., The Role of Cysteine Peptidases in Coronavirus Cell Entry and Replication: The Therapeutic Potential of Cathepsin Inhibitors, PLoS Pathog, doi:10.1371/journal.ppat.1009013
Redhu, Gounni, Function and Mechanisms of TSLP/TSLPR Complex in Asthma and COPD, Clin. Exp. Allergy, doi:10.1111/j.1365-2222.2011.03919.x
Sano, Miyauchi, Takakura, Yamauchi, Murata et al., Cysteine Protease Inhibitors in Various Milk Preparations and Its Importance as a Food, Food Res. Int, doi:10.1016/j.foodres.2004.10.011
Scaldaferri, Ianiro, Privitera, Lopetuso, Vetrone et al., The Thrilling Journey of SARS-CoV-2 into the Intestine: From Pathogenesis to Future Clinical Implications, Inflamm. Bowel Dis, doi:10.1093/ibd/izaa181
Serrano, Kochergina, Albors, Diaz, Oroval et al., Liposomal Lactoferrin as Potential Preventative and Cure for COVID-19, IJRHS, doi:10.5530/ijrhs.8.1.3
Shin, Wakabayashi, Yamauchi, Yaeshima, Iwatsuki, Recombinant Human Intelectin Binds Bovine Lactoferrin and Its Peptides, Biol. Pharm Bull, doi:10.1248/bpb.31.1605
Siqueiros-Cendón, Arévalo-Gallegos, Iglesias-Figueroa, García-Montoya, Salazar-Martínez et al., Immunomodulatory Effects of Lactoferrin, Acta Pharm. Sin, doi:10.1038/aps.2013.200
Sun, Louie, Vannella, Wilke, Levine et al., New Concepts of IL-10-Induced Lung Fibrosis: Fibrocyte Recruitment and M2 Activation in a CCL2/CCR2 Axis, Am. J. Physiol. Lung Cell Mol. Physiol, doi:10.1152/ajplung.00122.2010
Superti, Ammendolia, Valenti, Seganti, Antirotaviral Activity of Milk Proteins: Lactoferrin Prevents Rotavirus Infection in the Enterocyte-like Cell Line HT-29, Med. Microbiol. Immunol, doi:10.1007/s004300050049
Takayama, In vitro and Animal Models for SARS-CoV-2 Research, Trends Pharmacol. Sci, doi:10.1016/j.tips.2020.05.005
Van Der Strate, Beljaars, Molema, Harmsen, Meijer, Antiviral Activities of Lactoferrin, Antivir. Res, doi:10.1016/S0166-3542(01)00195-4
Van Doorn, Meijer, Frampton, Barclay, De Boer, Systematic Review with Meta-analysis: SARS-CoV-2 Stool Testing and the Potential for Faecal-oral Transmission, Aliment Pharm, doi:10.1111/apt.16036
Van Splunter, Perdijk, Fick-Brinkhof, Feitsma, Floris-Vollenbroek et al., Bovine Lactoferrin Enhances TLR7-Mediated Responses in Plasmacytoid Dendritic Cells in Elderly Women: Results From a Nutritional Intervention Study With Bovine Lactoferrin, GOS and Vitamin D, Front. Immunol, doi:10.3389/fimmu.2018.02677
Wakabayashi, Oda, Yamauchi, Abe, Lactoferrin for Prevention of Common Viral Infections, J. Infect. Chemother, doi:10.1016/j.jiac.2014.08.003
Wang, Li, Zhao, Ren, Guo, Lactoferrin Stimulates the Expression of Vitamin D Receptor in Vitamin D Deficient Mice, J. Funct. Foods, doi:10.1016/j.jff.2019.02.012
Wang, Timilsena, Blanch, Adhikari, Lactoferrin: Structure, Function, Denaturation and Digestion, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2017.1381583
Wang, Wang, Wang, Luo, Wan et al., Lactoferrin for the Treatment of COVID-19, Exp. Med, doi:10.3892/etm.2020.9402
DOI record:
{
"DOI": "10.3390/nu13020328",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu13020328",
"abstract": "<jats:p>SARS-CoV-2 is a newly emerging virus that currently lacks curative treatments. Lactoferrin (LF) is a naturally occurring non-toxic glycoprotein with broad-spectrum antiviral, immunomodulatory and anti-inflammatory effects. In this study, we assessed the potential of LF in the prevention of SARS-CoV-2 infection in vitro. Antiviral immune response gene expression was analyzed by qRT-PCR in uninfected Caco-2 intestinal epithelial cells treated with LF. An infection assay for SARS-CoV-2 was performed in Caco-2 cells treated or not with LF. SARS-CoV-2 titer was determined by qRT-PCR, plaque assay and immunostaining. Inflammatory and anti-inflammatory cytokine production was determined by qRT-PCR. LF significantly induced the expression of IFNA1, IFNB1, TLR3, TLR7, IRF3, IRF7 and MAVS genes. Furthermore, LF partially inhibited SARS-CoV-2 infection and replication in Caco-2 intestinal epithelial cells. Our in vitro data support LF as an immune modulator of the antiviral immune response with moderate effects against SARS-CoV-2 infection.</jats:p>",
"alternative-id": [
"nu13020328"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6998-8550",
"affiliation": [],
"authenticated-orcid": false,
"family": "Salaris",
"given": "Claudio",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-7055-635X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Scarpa",
"given": "Melania",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elli",
"given": "Marina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bertolini",
"given": "Alice",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8673-8190",
"affiliation": [],
"authenticated-orcid": false,
"family": "Guglielmetti",
"given": "Simone",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3919-0679",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pregliasco",
"given": "Fabrizio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Blandizzi",
"given": "Corrado",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3279-9000",
"affiliation": [],
"authenticated-orcid": false,
"family": "Brun",
"given": "Paola",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Castagliuolo",
"given": "Ignazio",
"sequence": "additional"
}
],
"container-title": [
"Nutrients"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
1,
25
]
],
"date-time": "2021-01-25T14:59:40Z",
"timestamp": 1611586780000
},
"deposited": {
"date-parts": [
[
2021,
1,
25
]
],
"date-time": "2021-01-25T16:18:56Z",
"timestamp": 1611591536000
},
"indexed": {
"date-parts": [
[
2021,
12,
19
]
],
"date-time": "2021-12-19T01:09:33Z",
"timestamp": 1639876173713
},
"is-referenced-by-count": 20,
"issn-type": [
{
"type": "electronic",
"value": "2072-6643"
}
],
"issue": "2",
"issued": {
"date-parts": [
[
2021,
1,
23
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2021,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
23
]
],
"date-time": "2021-01-23T00:00:00Z",
"timestamp": 1611360000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/13/2/328/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "328",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
1,
23
]
]
},
"published-online": {
"date-parts": [
[
2021,
1,
23
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1002/rmv.2103",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1038/s41591-020-0820-9",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.3390/diseases4030026",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.cell.2020.09.033",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"key": "ref6",
"unstructured": "World Health Organization: Modes of Transmissionhttps://scholar.google.com/scholar_lookup?journal=Sci+Br&title=Modes+of+transmission+of+virus+causing+COVID%E2%80%9019:+implications+for+IPC+precaution+recommendations&publication_year=2020&"
},
{
"DOI": "10.1126/science.abc1669",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1111/apt.16036",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1128/AAC.00399-20",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"key": "ref10",
"unstructured": "Treatments and Vaccines for COVID-19: Authorised Medicineshttps://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/treatments-vaccines-covid-19-authorised-medicines"
},
{
"DOI": "10.1186/s13054-020-03020-3",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3390/ijms21144903",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1371/journal.pone.0023710",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1007/s004300050049",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1016/S0168-1702(99)00121-5",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1016/S0166-3542(01)00195-4",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.jiac.2014.08.003",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1021/acsptsci.0c00059",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/j.biochi.2008.05.015",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1128/JVI.79.22.14451-14456.2005",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1128/JVI.02078-14",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1016/j.foodres.2004.10.011",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1038/s41467-020-15562-9",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1371/journal.ppat.1009013",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.2174/138161209788453202",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"article-title": "Lactoferrin Regulates the Release of Tumour Necrosis Factor Alpha and Interleukin 6 in Vivo",
"author": "Machnicki",
"first-page": "433",
"journal-title": "Int. J. Exp. Pathol.",
"key": "ref26",
"volume": "74",
"year": "1993"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106118",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.tips.2020.05.005",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"key": "ref30",
"unstructured": "Molecular Assays to Diagnose COVID-19: Summary Table of Available Protocolshttps://www.who.int/publications/m/item/molecular-assays-to-diagnose-covid-19-summary-table-of-available-protocols"
},
{
"DOI": "10.1038/aps.2013.200",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1515/CCLM.1999.049",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.3892/etm.2020.9402",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.3389/fimmu.2020.570122",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.5530/ijrhs.8.1.3",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1096/fasebj.26.1_supplement.644.5",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1152/ajplung.1999.276.6.L933",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1002/jcp.22650",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1248/bpb.31.1605",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1016/j.cellimm.2006.08.006",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.3389/fimmu.2020.01221",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1038/nri1900",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.3389/fimmu.2014.00461",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1172/JCI126363",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.3389/fimmu.2018.02677",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1136/gutjnl-2020-321434",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1093/ibd/izaa181",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1080/10408398.2017.1381583",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1016/j.jff.2019.02.012",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.26355/eurrev_202004_20876",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1007/s40519-016-0312-6",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1111/j.1365-2222.2011.03919.x",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.1016/j.jaci.2015.04.011",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1152/ajplung.00122.2010",
"doi-asserted-by": "publisher",
"key": "ref57"
}
],
"reference-count": 57,
"references-count": 57,
"relation": {},
"score": 1,
"short-container-title": [
"Nutrients"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": [
"Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro"
],
"type": "journal-article",
"volume": "13"
}