Lactoferrin binding to Sars-CoV-2 Spike glycoprotein protects host from infection, inflammation and iron dysregulation.
et al., Research Square, doi:10.21203/rs.3.rs-1605740/v1, May 2022
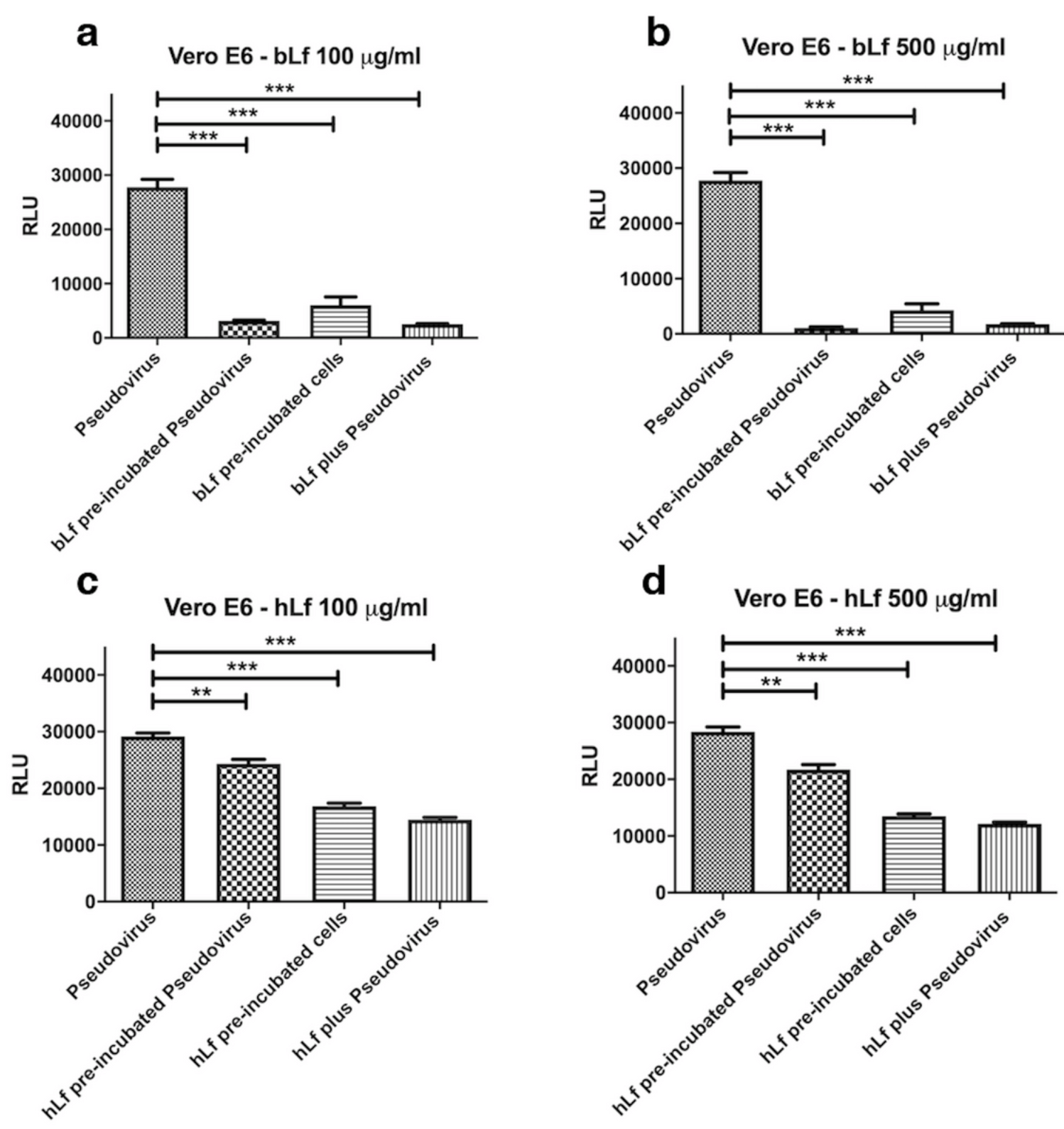
Vero E6, Caco-2, and THP-1 in vitro study showing lactoferrin inhibited SARS-CoV-2 spike pseudovirus. Nutraceutically available bovine lactoferrin was more effective than human lactoferrin.
18 preclinical studies support the efficacy of lactoferrin for COVID-19:
1.
da Silva et al., Immunomodulatory effect of bovine lactoferrin during SARS-CoV-2 infection, Frontiers in Immunology, doi:10.3389/fimmu.2024.1456634.
2.
Cutone et al., Lactoferrin binding to Sars-CoV-2 Spike glycoprotein protects host from infection, inflammation and iron dysregulation., Research Square, doi:10.21203/rs.3.rs-1605740/v1.
3.
Miotto et al., Molecular Mechanisms Behind Anti SARS-CoV-2 Action of Lactoferrin, Frontiers in Molecular Biosciences, doi:10.3389/fmolb.2021.607443.
4.
Babulic et al., Lactoferrin Binds through Its N-Terminus to the Receptor-Binding Domain of the SARS-CoV-2 Spike Protein, Pharmaceuticals, doi:10.3390/ph17081021.
5.
Yathindranath et al., Lipid Nanoparticle-Based Inhibitors for SARS-CoV-2 Host Cell Infection, International Journal of Nanomedicine, doi:10.2147/IJN.S448005.
6.
Alves et al., Inhibition of SARS-CoV-2 Infection in Vero Cells by Bovine Lactoferrin under Different Iron-Saturation States, Pharmaceuticals, doi:10.3390/ph16101352.
7.
Kobayashi-Sakamoto et al., Bovine lactoferrin suppresses the cathepsin-dependent pathway of SARS-CoV-2 entry in vitro, International Dairy Journal, doi:10.1016/j.idairyj.2023.105805.
8.
Andreu et al., Liposomal Lactoferrin Exerts Antiviral Activity against HCoV-229E and SARS-CoV-2 Pseudoviruses In Vitro, Viruses, doi:10.3390/v15040972.
9.
Yazawa et al., Evaluation of SARS-CoV-2 isolation in cell culture from nasal/nasopharyngeal swabs or saliva specimens of patients with COVID-19, Research Square, doi:10.21203/rs.3.rs-2676422/v1.
10.
Piacentini et al., Lactoferrin Inhibition of the Complex Formation between ACE2 Receptor and SARS CoV-2 Recognition Binding Domain, International Journal of Molecular Sciences, doi:10.3390/ijms23105436.
11.
Ostrov et al., Highly Specific Sigma Receptor Ligands Exhibit Anti-Viral Properties in SARS-CoV-2 Infected Cells, Pathogens, doi:10.3390/pathogens10111514.
12.
Mirabelli et al., Morphological cell profiling of SARS-CoV-2 infection identifies drug repurposing candidates for COVID-19, Proceedings of the National Academy of Sciences, doi:10.1073/pnas.2105815118.
13.
Salaris et al., Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro, Nutrients, doi:10.3390/nu13020328.
Cutone et al., 17 May 2022, Italy, preprint, 12 authors.
Contact: musci@unimol.it.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Lactoferrin binding to Sars-CoV-2 Spike glycoprotein protects host from infection, inflammation and iron dysregulation.
doi:10.21203/rs.3.rs-1605740/v1
The anti-SARS-Cov-2 activity of the iron-binding protein Lactoferrrin has been investigated in epithelial and macrophagic cell models using a Pseudovirus decorated with the SARS-CoV-2 Spike glycoprotein. The human and, even more, the nutraceutically available bovine Lactoferrin inhibit pseudoviral infection in all cellular models tested. The bovine protein efficiently counteracts the deleterious effects of purified Spike on iron and inflammatory homeostasis, as shown by restored levels of the main proteins of the iron-handling system and, in the case of macrophagic THP-1 cells, of the proinflammatory cytokines IL-1β and IL-6. A direct interaction between Lactoferrin and Spike is likely at the basis of the observed effects, as demonstrated by an in vitro pull-down assay. Finally, in silico approaches have been applied to analyze the interactions of human and bovine Lactoferrins with Transferrin Receptor 1, a potential gate for SARS-CoV-2 entry into cells, as well as the binding of the bovine protein to different variants of concern of the SARS-Cov-2 Spike glycoprotein. Our results give hope for the employment of bovine Lactoferrin as an adjuvant of the standard of care therapies in COVID-19 treatment.
Statements and Declarations
Competing Interests No competing interests do declare.
Author Contributions All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by Antimo Cutone, Luigi Rosa and Mattia Falconi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data Availability The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Abraham, Corbett, Farzan, Choe, Harrison, Structural basis for receptor recognition by New World hemorrhagic fever arenaviruses, Nat Struct Mol Biol, doi:10.1038/nsmb.1772
Abraham, Murtola, Schulz, Páll, Smith et al., GROMACS: High Performance Molecular Simulations through Multi-Level Parallelism from Laptops to Supercomputers, SoftwareX, doi:10.1016/j.softx.2015.06.001
Bergamaschi, Sabatino, Pasini, Ubezio, Costanzo et al., Intestinal expression of genes implicated in iron absorption and their regulation by hepcidin, Clin Nutr, doi:10.1016/j.clnu.2016.09.021
Campione, Lanna, Cosio, Rosa, Conte et al., Lactoferrin against SARS-CoV-2: In vitro and in silico evidences, Front Pharmacol, doi:10.3389/fphar.2021.666600
Campione, Lanna, Cosio, Rosa, Conte et al., Lactoferrin as Antiviral Treatment in COVID-19 Management: Preliminary Evidence, Int J Environ Res Public Health, doi:10.3390/ijerph182010985
Case, Betz, Cerutti, Cheatham, Darden et al., Amber 2016
Crook, Girard, Sevilla, Merrill, Friend et al., A TfR-Binding Cystine-Dense Peptide Promotes Blood-Brain Barrier Penetration of Bioactive Molecules, J Mol Biol, doi:10.1016/j.jmb.2020.04.002
Cutone, Lepanto, Rosa, Scotti, Rossi et al., Aerosolized Bovine Lactoferrin Counteracts Infection, Inflammation and Iron Dysbalance in A Cystic Fibrosis Mouse Model of Pseudomonas aeruginosa Chronic Lung Infection, Int J Mol Sci, doi:10.3390/ijms20092128
Cutone, Rosa, Lepanto, Scotti, Berlutti et al., Lactoferrin Efficiently Counteracts the Inflammation-Induced Changes of the Iron Homeostasis System in Macrophages, Front Immunol, doi:10.3389/fimmu.2017.00705
Di, Cutone, Polticelli, Rosa, Lepanto et al., The ferroportin-ceruloplasmin system and the mammalian iron homeostasis machine: Regulatory pathways and the role of lactoferrin, Biometals, doi:10.1007/s10534-018-0087-5
Donovan, Lima, Pinkus, Pinkus, Zon et al., The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis, Cell Metab, doi:10.1016/j.cmet.2005.01.003
Eckenroth, Steere, Chasteen, Everse, Mason, How the binding of human transferrin primes the transferrin receptor potentiating iron release at endosomal pH, Proc Natl Acad Sci U S A, doi:10.1073/pnas.1105786108
Frazer, Anderson, The orchestration of body iron intake: how and where do enterocytes receive their cues?, Blood Cells Mol Dis, doi:10.1016/S1079-9796(03)00039-1
Frioni, Conte, Cutone, Longhi, Musci et al., Lactoferrin differently modulates the inflammatory response in epithelial models mimicking human inflammatory and infectious diseases, Biometals, doi:10.1007/s10534-014-9740-9
Ganz, Nemeth, Iron homeostasis in host defence and inflammation, Nat Rev, doi:10.1038/nri3863
Garzon, Lopéz-Blanco, Pons, Kovacs, Abagyan et al., FRODOCK: a New Approach for Fast Rotational Protein-Protein Docking, Bioinformatics, doi:10.1093/bioinformatics/btp447
Hoffmann, Kleine-Weber, Schroeder, Kruger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Hu, Meng, Zhang, Xiang, Wang, The in vitro antiviral activity of lactoferrin against common human coronaviruses and SARS-CoV-2 is mediated by targeting the heparan sulfate co-receptor, Emerg Microbes Infect, doi:10.1080/22221751.2021.1888660
Iannone, Ambrosino, Bracco, Rosa, Funel et al., CRESCO ENEA HPC Clusters: a Working Example of a Multifabric GPFS Spectrum Scale Layout, doi:10.1109/HPCS48598.2019.9188135
Kawabata, Tong, Kawanami, Wano, Hirose et al., Analyses for binding of the transferrin family of proteins to the transferrin receptor 2, Br J Haematol, doi:10.1111/j.1365-2141.2004.05224
Kozakov, Hall, Xia, Porter, Padhorny et al., The ClusPro web server for protein-protein docking, Nat Protoc, doi:10.1038/nprot.2016.169
Lepanto, Rosa, Cutone, Conte, Paesano et al., Efficacy of Lactoferrin Oral Administration in the Treatment of Anemia and Anemia of Inflammation in Pregnant and Non-pregnant Women: An Interventional Study, Front Immunol, doi:10.3389/fimmu.2018.02123
Liu, Li, Xu, Wu, Luo et al., Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19, J Clin Virol, doi:10.1016/j.jcv.2020.104370
Liu, Nguyen, Marquess, Yang, Haile, Regulation of hepcidin and ferroportin expression by lipopolysaccharide in splenic macrophages, Blood Cells Mol Dis, doi:10.1016/j.bcmd.2005.04.006
Lu, Zhao, Li, Niu, Yang et al., Genomic Characterisation and Epidemiology of 2019 Novel Coronavirus: Implications for Virus Origins and Receptor Binding, The Lancet, doi:10.1016/S0140-6736(20)30251-8
Mackenzie, Garrick, Iron imports: II. Iron uptake at the apical membrane in the intestine, Am J Physiol Gastrointest Liver Physiol, doi:10.1152/ajpgi.00363.2005
Malik, Naz, Sheikh, Khan, Moriconi et al., Comparison of changes in gene expression of transferrin receptor-1 and other iron-regulatory proteins in rat liver and brain during acute-phase response, Cell Tissue Res, doi:10.1007/s00441-011-1152-3
Mancinelli, Rosa, Cutone, Lepanto, Franchitto et al., Viral Hepatitis and Iron Dysregulation: Molecular Pathways and the Role of Lactoferrin, Molecules, doi:10.3390/molecules25081997
Marques, Auriac, Willemetz, Banha, Silva et al., Immune cells and hepatocytes express glycosylphosphatidylinositol-anchored ceruloplasmin at their cell surface, Blood Cells Mol Dis, doi:10.1016/j.bcmd.2011.11.005
Mazumder, Mukhopadhyay, Prok, Cathcart, Fox, Induction of ceruloplasmin synthesis by IFN-gamma in human monocytic cells, J Immunol
Mazumder, Sampath, Fox, Translational control of ceruloplasmin gene expression: beyond the IRE, Biol Res, doi:10.4067/s0716-97602006000100007
Mcgibbon, Beauchamp, Harrigan, Klein, Swails et al., MDTraj: A Modern Open Library for the Analysis of Molecular Dynamics Trajectories, Biophys J, doi:10.1016/j.bpj.2015.08.015
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: Consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/S0140-6736(20)30628-0
Mirabelli, Wotring, Zhang, Mccarty, Fursmidt et al., Morphological cell profiling of SARS-CoV-2 infection identifies drug repurposing candidates for COVID-19, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2105815118
Moore, Anderson, Groom, Haridas, Baker, Three-dimensional Structure of Diferric Bovine Lactoferrin at 2.8 Å Resolution, J Mol Biol, doi:10.1006/jmbi.1997.1386
Patra, Meyer, Geerling, Isbell, Hoft et al., SARS-CoV-2 Spike protein promotes IL-6 trans-signaling by activation of angiotensin II receptor signaling in epithelial cells, PLoS Pathog, doi:10.1371/journal.ppat.1009128
Persichini, Maio, Di Patti, Rizzo, Toscano et al., Interleukin-1β induces ceruloplasmin and ferroportin-1 gene expression via MAP kinases and C/EBPβ, AP-1, and NF-κB activation, Neurosci Lett, doi:10.1016/j.neulet.2010.08.034
Pettersen, Goddard, Huang, Couch, Greenblatt et al., UCSF Chimera--A Visualization System for Exploratory Research and Analysis, J Comput Chem, doi:10.1002/jcc.20084
Phillips, Braun, Wang, Gumbart, Tajkhorshid et al., Scalable Molecular Dynamics with NAMD, J Comput Chem, doi:10.1002/jcc.20289
Phua, Weng, Ling, Egi, Lim et al., Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations, Lancet Respir Med, doi:10.1016/S2213-2600(20)30161-2
Ramírez-Aportela, Blanco, Chacón, FRODOCK 2.0: Fast Protein-Protein Docking Server, Bioinformatics, doi:10.1093/bioinformatics/btw141
Recalcati, Locati, Marini, Santambrogio, Zaninotto et al., Differential regulation of iron homeostasis during human macrophage polarized activation, Eur J Immunol, doi:10.1002/eji.200939889
Romeo, Christen, Niles, Kosman, Intracellular chelation of iron by bipyridyl inhibits DNA virus replication: ribonucleotide reductase maturation as a probe of intracellular iron pools, J Biol Chem, doi:10.1074/jbc.M010806200
Romeo, Iacovelli, Falconi, Targeting the SARS-CoV-2 Spike Glycoprotein Prefusion Conformation: Virtual Screening and Molecular Dynamics Simulations Applied to the Identification of Potential Fusion Inhibitors, Virus Res, doi:10.1016/j.virusres.2020.198068
Rosa, Cutone, Lepanto, Paesano, Valenti, Lactoferrin: A Natural Glycoprotein Involved in Iron and Inflammatory Homeostasis, Int J Mol Sci, doi:10.3390/ijms18091985
Rosa, Tripepi, Naldi, Aimati, Santangeli et al., Ambulatory COVID-19 Patients Treated with Lactoferrin as a Supplementary Antiviral Agent: A Preliminary Study, J Clin Med, doi:10.3390/jcm10184276
Ryckaert, Ciccotti, Berendsen, Numerical Integration of the Cartesian Equations of Motion of a System with Constraints: Molecular Dynamics of N-Alkanes, J Comput Phys, doi:10.1016/0021-9991(77)90098-5
Saadi, Pal, Sarma, Spike Glycoprotein Is Central to Coronavirus Pathogenesis-Parallel Between m-CoV and SARS-CoV-2, Ann Neurosci, doi:10.1177/09727531211023755
Salomon-Ferrer, Walker, An Overview of the Amber Biomolecular Simulation Package, WIREs Comput Mol Sci, doi:10.1002/wcms.1121
Schmidt, The role of iron in viral infections, Front Biosci (Landmark Ed), doi:10.2741/4839
Sheikh, Dudas, Ramadori, Changes of gene expression of iron regulatory proteins during turpentine oil-induced acute-phase response in the rat, Lab Invest, doi:10.1038/labinvest.3700553
Sienkiewicz, Jaśkiewicz, Tarasiuk, Fichna, Lactoferrin: an overview of its main functions, immunomodulatory and antimicrobial role, and clinical significance, Crit Rev Food Sci Nutr, doi:10.1080/10408398.2021.1895063
Tacchini, Gammella, Ponti, Recalcati, Cairo, Role of HIF-1 and NF-kappaB transcription factors in the modulation of transferrin receptor by inflammatory and anti-inflammatory signals, J Biol Chem, doi:10.1074/jbc.M800365200
Tang, Yang, Duan, Liao, Liu et al., Transferrin receptor is another receptor for SARS-CoV-2 entry, bioRxiv, doi:10.1101/2020.10.23.350348
Tian, Li, Huang, Xia, Lu et al., Potent Binding of 2019 Novel Coronavirus Spike Protein by a SARS Coronavirus-specific Human Monoclonal Antibody, Emerg Microbes Infect, doi:10.1080/22221751.2020.1729069
Tisato, Gallo, Melloni, Celeghini, Passaro et al., TRAIL and Ceruloplasmin Inverse Correlation as a Representative Crosstalk between Inflammation and Oxidative Stress, Mediators Inflamm, doi:10.1155/2018/9629537
Tran, Eubanks, Schaffer, Zhou, Linder, Secretion of ferritin by rat hepatoma cells and its regulation by inflammatory cytokines and iron, Blood, doi:10.1182/blood.V90.12.4979
Valenti, Antonini, Lactoferrin: an important host defence against microbial and viral attack, Cell Mol Life Sci, doi:10.1007/s00018-005-5372-0
Walls, Park, Tortorici, Wall, Mcguire et al., Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein, Cell, doi:10.1016/j.cell.2020.02.058
Wesselius, Nelson, Skikne, Increased release of ferritin and iron by ironloaded alveolar macrophages in cigarette smokers, Am J Respir Crit Care Med, doi:10.1164/ajrccm.150.3.8087339
Willemetz, Beatty, Richer, Rubio, Auriac et al., Iron-and Hepcidin-Independent Downregulation of the Iron Exporter Ferroportin in Macrophages during Salmonella Infection, Front Immunol, doi:10.3389/fimmu.2017.00498
Xiong, She, Takeuchi, Han, Engelhardt et al., Signaling role of intracellular iron in NF-kappaB activation, J Biol Chem, doi:10.1074/jbc.M210905200
DOI record:
{
"DOI": "10.21203/rs.3.rs-1605740/v1",
"URL": "http://dx.doi.org/10.21203/rs.3.rs-1605740/v1",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>The anti-SARS-Cov-2 activity of the iron-binding protein Lactoferrrin has been investigated in epithelial and macrophagic cell models using a Pseudovirus decorated with the SARS-CoV-2 Spike glycoprotein. The human and, even more, the nutraceutically available bovine Lactoferrin inhibit pseudoviral infection in all cellular models tested. The bovine protein efficiently counteracts the deleterious effects of purified Spike on iron and inflammatory homeostasis, as shown by restored levels of the main proteins of the iron-handling system and, in the case of macrophagic THP-1 cells, of the proinflammatory cytokines IL-1β and IL-6. A direct interaction between Lactoferrin and Spike is likely at the basis of the observed effects, as demonstrated by an in vitro pull-down assay. Finally, in silico approaches have been applied to analyze the interactions of human and bovine Lactoferrins with Transferrin Receptor 1, a potential gate for SARS-CoV-2 entry into cells, as well as the binding of the bovine protein to different variants of concern of the SARS-Cov-2 Spike glycoprotein. Our results give hope for the employment of bovine Lactoferrin as an adjuvant of the standard of care therapies in COVID-19 treatment.</jats:p>",
"accepted": {
"date-parts": [
[
2022,
4,
28
]
]
},
"author": [
{
"affiliation": [
{
"name": "University of Molise Department of Bioscience and Environment: Universita degli Studi del Molise Dipartimento di Bioscienze e Territorio"
}
],
"family": "Cutone",
"given": "Antimo",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Sapienza University of Rome Department of Public Health and Infectious Diseases"
}
],
"family": "Rosa",
"given": "Luigi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Sapienza University of Rome Department of Biochemical Sciences"
}
],
"family": "Patti",
"given": "Maria Carmela Bonaccorsi di",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Univ of Rome Tor Vergata Department of Biologyersity"
}
],
"family": "Iacovelli",
"given": "Federico",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Sapienza University of Rome Department of Public Health and Infectious Diseases"
}
],
"family": "Conte",
"given": "Maria Pia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "University of Molise Department of Bioscience and Territory: Universita degli Studi del Molise Dipartimento di Bioscienze e Territorio"
}
],
"family": "Ianiro",
"given": "Giusi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "University of Rome Tor Vergata Department of Biology"
}
],
"family": "Romeo",
"given": "Alice",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "University of Rome Tor Vergata Dermatology Unit"
}
],
"family": "Campione",
"given": "Elena",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "University of Rome Tor Vergata Dermatology Unit"
}
],
"family": "Bianchi",
"given": "Luca",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Sapienza University of Rome Department of Public Health and Infectious Diseases"
}
],
"family": "Valenti",
"given": "Piera",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "University of Rome Tor Vergata Department of Biology"
}
],
"family": "Falconi",
"given": "Mattia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5196-709X",
"affiliation": [
{
"name": "University of Molise Department of Bioscience and Territory: Universita degli Studi del Molise Dipartimento di Bioscienze e Territorio"
}
],
"authenticated-orcid": false,
"family": "Musci",
"given": "Giovanni",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
5,
17
]
],
"date-time": "2022-05-17T19:19:22Z",
"timestamp": 1652815162000
},
"deposited": {
"date-parts": [
[
2022,
5,
17
]
],
"date-time": "2022-05-17T19:19:24Z",
"timestamp": 1652815164000
},
"group-title": "In Review",
"indexed": {
"date-parts": [
[
2022,
5,
17
]
],
"date-time": "2022-05-17T19:42:01Z",
"timestamp": 1652816521679
},
"institution": [
{
"name": "Research Square"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
5,
17
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
17
]
],
"date-time": "2022-05-17T00:00:00Z",
"timestamp": 1652745600000
}
}
],
"link": [
{
"URL": "https://www.researchsquare.com/article/rs-1605740/v1",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.researchsquare.com/article/rs-1605740/v1.html",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "8761",
"original-title": [],
"posted": {
"date-parts": [
[
2022,
5,
17
]
]
},
"prefix": "10.21203",
"published": {
"date-parts": [
[
2022,
5,
17
]
]
},
"publisher": "Research Square Platform LLC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.researchsquare.com/article/rs-1605740/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Lactoferrin binding to Sars-CoV-2 Spike glycoprotein protects host from infection, inflammation and iron dysregulation.",
"type": "posted-content"
}