Inhibition of SARS-CoV-2 Infection in Vero Cells by Bovine Lactoferrin under Different Iron-Saturation States
et al., Pharmaceuticals, doi:10.3390/ph16101352 , Sep 2023
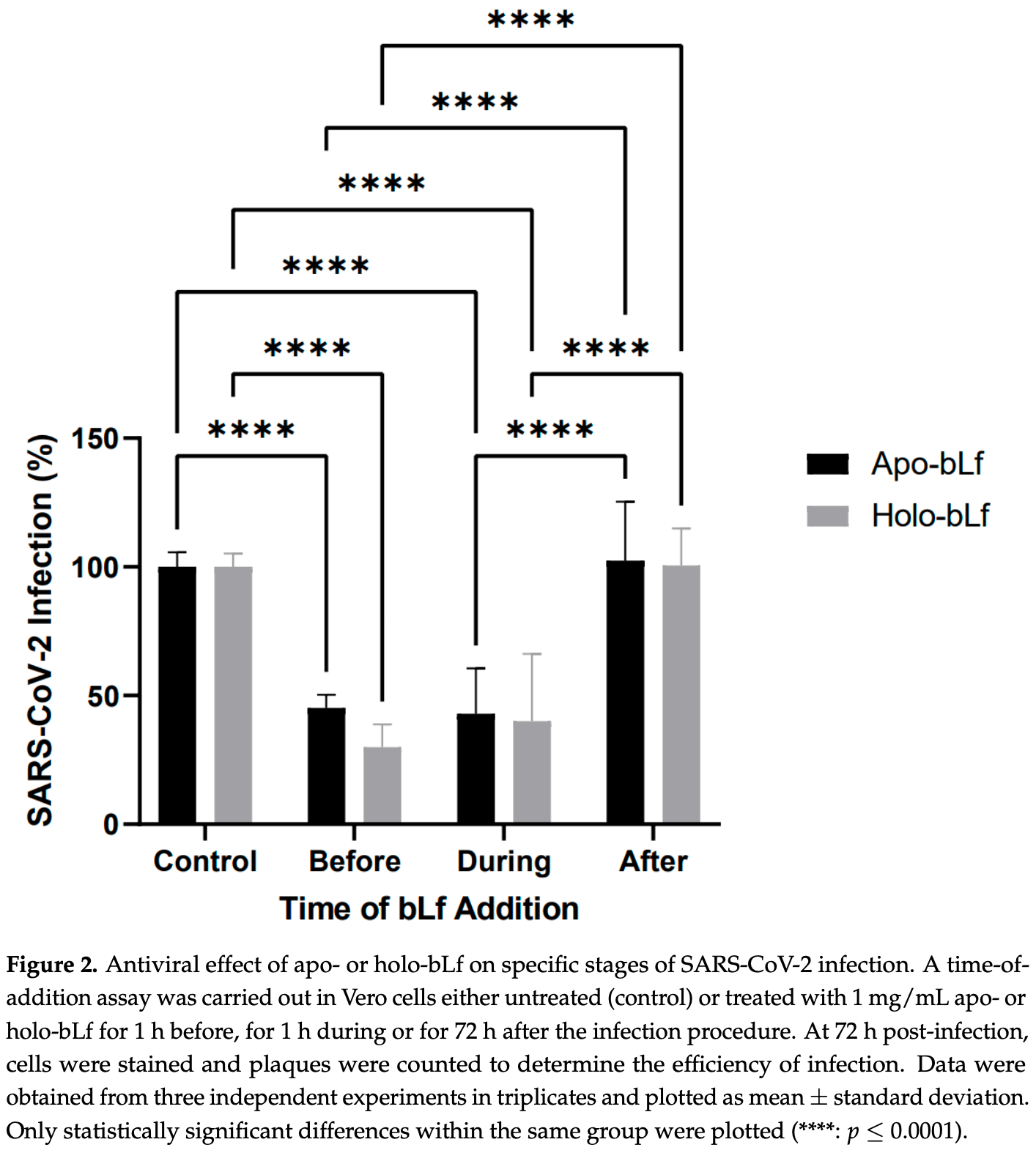
In vitro study showing that iron-free and iron-saturated bovine lactoferrin inhibited SARS-CoV-2 ancestral and omicron Vero cell infection. Treatment before or during infection was effective, while treatment after infection showed no significant effect. Saturated lactoferrin showed improved efficacy, with 70% vs. 55% reduction for treatment before infection. Electron microscopy confirmed improved efficacy with saturated lactoferrin.
The results suggest that lactoferrin treatment may be most effective if given prophylactically or immediately at the onset of COVID-19 symptoms. While both iron-free and iron-saturated lactoferrin inhibited infection, the saturated form appeared more effective, suggesting that iron supplementation may improve lactoferrin's efficacy against COVID-19.
18 preclinical studies support the efficacy of lactoferrin for COVID-19:
1.
da Silva et al., Immunomodulatory effect of bovine lactoferrin during SARS-CoV-2 infection, Frontiers in Immunology, doi:10.3389/fimmu.2024.1456634.
2.
Cutone et al., Lactoferrin binding to Sars-CoV-2 Spike glycoprotein protects host from infection, inflammation and iron dysregulation., Research Square, doi:10.21203/rs.3.rs-1605740/v1.
3.
Miotto et al., Molecular Mechanisms Behind Anti SARS-CoV-2 Action of Lactoferrin, Frontiers in Molecular Biosciences, doi:10.3389/fmolb.2021.607443.
4.
Babulic et al., Lactoferrin Binds through Its N-Terminus to the Receptor-Binding Domain of the SARS-CoV-2 Spike Protein, Pharmaceuticals, doi:10.3390/ph17081021.
5.
Yathindranath et al., Lipid Nanoparticle-Based Inhibitors for SARS-CoV-2 Host Cell Infection, International Journal of Nanomedicine, doi:10.2147/IJN.S448005.
6.
Alves et al., Inhibition of SARS-CoV-2 Infection in Vero Cells by Bovine Lactoferrin under Different Iron-Saturation States, Pharmaceuticals, doi:10.3390/ph16101352.
7.
Kobayashi-Sakamoto et al., Bovine lactoferrin suppresses the cathepsin-dependent pathway of SARS-CoV-2 entry in vitro, International Dairy Journal, doi:10.1016/j.idairyj.2023.105805.
8.
Andreu et al., Liposomal Lactoferrin Exerts Antiviral Activity against HCoV-229E and SARS-CoV-2 Pseudoviruses In Vitro, Viruses, doi:10.3390/v15040972.
9.
Yazawa et al., Evaluation of SARS-CoV-2 isolation in cell culture from nasal/nasopharyngeal swabs or saliva specimens of patients with COVID-19, Research Square, doi:10.21203/rs.3.rs-2676422/v1.
10.
Piacentini et al., Lactoferrin Inhibition of the Complex Formation between ACE2 Receptor and SARS CoV-2 Recognition Binding Domain, International Journal of Molecular Sciences, doi:10.3390/ijms23105436.
11.
Ostrov et al., Highly Specific Sigma Receptor Ligands Exhibit Anti-Viral Properties in SARS-CoV-2 Infected Cells, Pathogens, doi:10.3390/pathogens10111514.
12.
Mirabelli et al., Morphological cell profiling of SARS-CoV-2 infection identifies drug repurposing candidates for COVID-19, Proceedings of the National Academy of Sciences, doi:10.1073/pnas.2105815118.
13.
Salaris et al., Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro, Nutrients, doi:10.3390/nu13020328.
Alves et al., 25 Sep 2023, peer-reviewed, 16 authors.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Inhibition of SARS-CoV-2 Infection in Vero Cells by Bovine Lactoferrin under Different Iron-Saturation States
doi:10.3390/ph16101352
Despite the rapid mass vaccination against COVID-19, the emergence of new SARS-CoV-2 variants of concern, such as omicron, is still a great distress, and new therapeutic options are needed. Bovine lactoferrin (bLf), a multifunctional iron-binding glycoprotein available in unsaturated (apo-bLf) and saturated (holo-bLf) forms, has been shown to exert broad-spectrum antiviral activity against many viruses. In this study, we evaluated the efficacy of both forms of bLf at 1 mg/mL against infection of Vero cells by SARS-CoV-2. As assessed with antiviral assays, an equivalent significant reduction in virus infection by about 70% was observed when either form of bLf was present throughout the infection procedure with the SARS-CoV-2 ancestral or omicron strain. This inhibitory effect seemed to be concentrated during the early steps of virus infection, since a significant reduction in its efficiency by about 60% was observed when apo-or holo-bLf were incubated with the cells before or during virus addition, with no significant difference between the antiviral effects of the distinct iron-saturation states of the protein. However, an ultrastructural analysis of bLf treatment during the early steps of virus infection revealed that holo-bLf was somewhat more effective than apo-bLf in inhibiting virus entry. Together, these data suggest that bLf mainly acts in the early events of SARS-CoV-2 infection and is effective against the ancestral virus as well as its omicron variant. Considering that there are no effective treatments to COVID-19 with tolerable toxicity yet, bLf shows up as a promising candidate.
Conflicts of Interest: The authors declare no conflict of interest. The funders had no role in the design of this study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
Baker, Baker, Lactoferrin and iron: Structural and dynamic aspects of binding and release, Biometals, doi:10.1023/B:BIOM.0000027694.40260.70
Barros, Sanches, Marques De Carvalho, Santos, Ferraz De Souza et al., Influence of iron binding in the structural stability and cellular internalization of bovine lactoferrin, Heliyon, doi:10.1016/j.heliyon.2021.e08087
Campione, Lanna, Cosio, Rosa, Conte et al., Lactoferrin Against SARS-CoV-2: In Vitro and In Silico Evidences, Front. Pharmacol, doi:10.3389/fphar.2021.666600
Carvalho, Casseb, Gonçalves, Silva, Gomes et al., Bovine lactoferrin activity against Chikungunya and Zika viruses, J. Gen. Virol, doi:10.1099/jgv.0.000849
Carvalho, Matos, Caetano, Sousa Junior, Campos et al., In Vitro Inhibition of SARS-CoV-2 Infection by Bovine Lactoferrin, bioRxiv, doi:10.1101/2020.05.13.093781
Carvalho, Sousa, Jr, Silva, Oliveira et al., Inhibition of Mayaro virus infection by bovine lactoferrin, Virology, doi:10.1016/j.virol.2014.01.022
Chen, Fan, Lin, Chen, Hsu et al., Bovine Lactoferrin Inhibits Dengue Virus Infectivity by Interacting with Heparan Sulfate, Low-Density Lipoprotein Receptor, and DC-SIGN, Int. J. Mol. Sci, doi:10.3390/ijms18091957
Chen, Wang, Gilby, Wei, Omicron Variant (B.1.1.529): Infectivity, Vaccine Breakthrough, and Antibody Resistance, J. Chem. Inf. Model, doi:10.1021/acs.jcim.1c01451
Chia, Young, Chia, The Omicron-transformer: Rise of the subvariants in the age of vaccines, Ann. Acad. Med. Singap, doi:10.47102/annals-acadmedsg.2022294
Cui, Li, Shi, Origin and evolution of pathogenic coronaviruses, Nat. Rev. Microbiol, doi:10.1038/s41579-018-0118-9
Denani, Real-Hohn, De Carvalho, Gomes, Gonçalves, Lactoferrin affects rhinovirus B-14 entry into H1-HeLa cells, Arch. Virol, doi:10.1007/s00705-021-04993-4
Di Biase, Pietrantoni, Tinari, Siciliano, Valenti et al., Heparin-interacting sites of bovine lactoferrin are involved in anti-adenovirus activity, J. Med. Virol, doi:10.1002/jmv.10337
Fehr, Perlman, Coronaviruses: An overview of their replication and pathogenesis, Methods Mol. Biol, doi:10.1007/978-1-4939-2438-7_1
González-Chávez, Arévalo-Gallegos, Rascón-Cruz, Lactoferrin: Structure, function and applications, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2008.07.020
Hao, Shan, Wei, Ma, Sun, Lactoferrin: Major Physiological Functions and Applications, Curr. Protein Pept. Sci, doi:10.2174/1389203719666180514150921
Hasöksüz, Kiliç, Saraç, Coronaviruses and SARS-CoV-2, Turk. J. Med. Sci, doi:10.3906/sag-2004-127
Hu, Meng, Zhang, Xiang, Wang, The in vitro antiviral activity of lactoferrin against common human coronaviruses and SARS-CoV-2 is mediated by targeting the heparan sulfate co-receptor, Emerg. Microbes Infect, doi:10.1080/22221751.2021.1888660
Koch, Uckeley, Doldan, Stanifer, Boulant et al., TMPRSS2 expression dictates the entry route used by SARS-CoV-2 to infect host cells, EMBO J, doi:10.15252/embj.2021107821
Kumar, Prasoon, Kumari, Pareek, Faiq et al., SARS-CoV-2-specific virulence factors in COVID-19, J. Med. Virol, doi:10.1002/jmv.26615
Lang, Yang, Deng, Liu, Yang et al., Inhibition of SARS pseudovirus cell entry by lactoferrin binding to heparan sulfate proteoglycans, PLoS ONE, doi:10.1371/journal.pone.0023710
Marchetti, Trybala, Superti, Johansson, Bergström, Inhibition of herpes simplex virus infection by lactoferrin is dependent on interference with the virus binding to glycosaminoglycans, Virology, doi:10.1016/j.virol.2003.09.029
Ren, Wang, Gao, Zhou, Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity, transmission, and vaccine resistance, World J. Clin. Cases, doi:10.12998/wjcc.v10.i1.1
Rosa, Tripepi, Naldi, Aimati, Santangeli et al., Ambulatory COVID-19 Patients Treated with Lactoferrin as a Supplementary Antiviral Agent: A Preliminary Study, J. Clin. Med, doi:10.3390/jcm10184276
Salaris, Scarpa, Elli, Bertolini, Guglielmetti et al., Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro, Nutrients, doi:10.3390/nu13020328
Sokolov, Isakova-Sivak, Mezhenskaya, Kostevich, Gorbunov et al., Molecular mimicry of the receptor-binding domain of the SARS-CoV-2 spike protein: From the interaction of spike-specific antibodies with transferrin and lactoferrin to the antiviral effects of human recombinant lactoferrin, Biometals, doi:10.1007/s10534-022-00458-6
Van Der Strate, Beljaars, Molema, Harmsen, Meijer, Antiviral activities of lactoferrin, Antiviral Res, doi:10.1016/S0166-3542(01)00195-4
Viana, Moyo, Amoako, Tegally, Scheepers et al., Rapid epidemic expansion of the SARS-CoV-2 Omicron variant in southern Africa, Nature, doi:10.1038/s41586-022-04411-y
Wang, Grunewald, Perlman, Coronaviruses: An Updated Overview of Their Replication and Pathogenesis, Methods Mol. Biol, doi:10.1007/978-1-0716-0900-2_1
Wang, Timilsena, Blanch, Adhikari, Lactoferrin: Structure, function, denaturation and digestion, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2017.1381583
Wotring, Fursmidt, Ward, Sexton, Evaluating the in vitro efficacy of bovine lactoferrin products against SARS-CoV-2 variants of concern, J. Dairy Sci, doi:10.3168/jds.2021-21247
Wu, Chen, Chan, The outbreak of COVID-19: An overview, J. Chin. Med. Assoc, doi:10.1097/JCMA.0000000000000270
Xu, Zhong, Deng, Peng, Dan et al., High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa, Int. J. Oral Sci, doi:10.1038/s41368-020-0074-x
Zimecki, Actor, Kruzel, The potential for Lactoferrin to reduce SARS-CoV-2 induced cytokine storm, Int. Immunopharmacol, doi:10.1016/j.intimp.2021.107571