The wide spectrum anti-inflammatory activity of andrographolide in comparison to NSAIDs: a promising therapeutic compound against the cytokine storm
et al., bioRxiv, doi:10.1101/2024.02.21.581396, Feb 2024
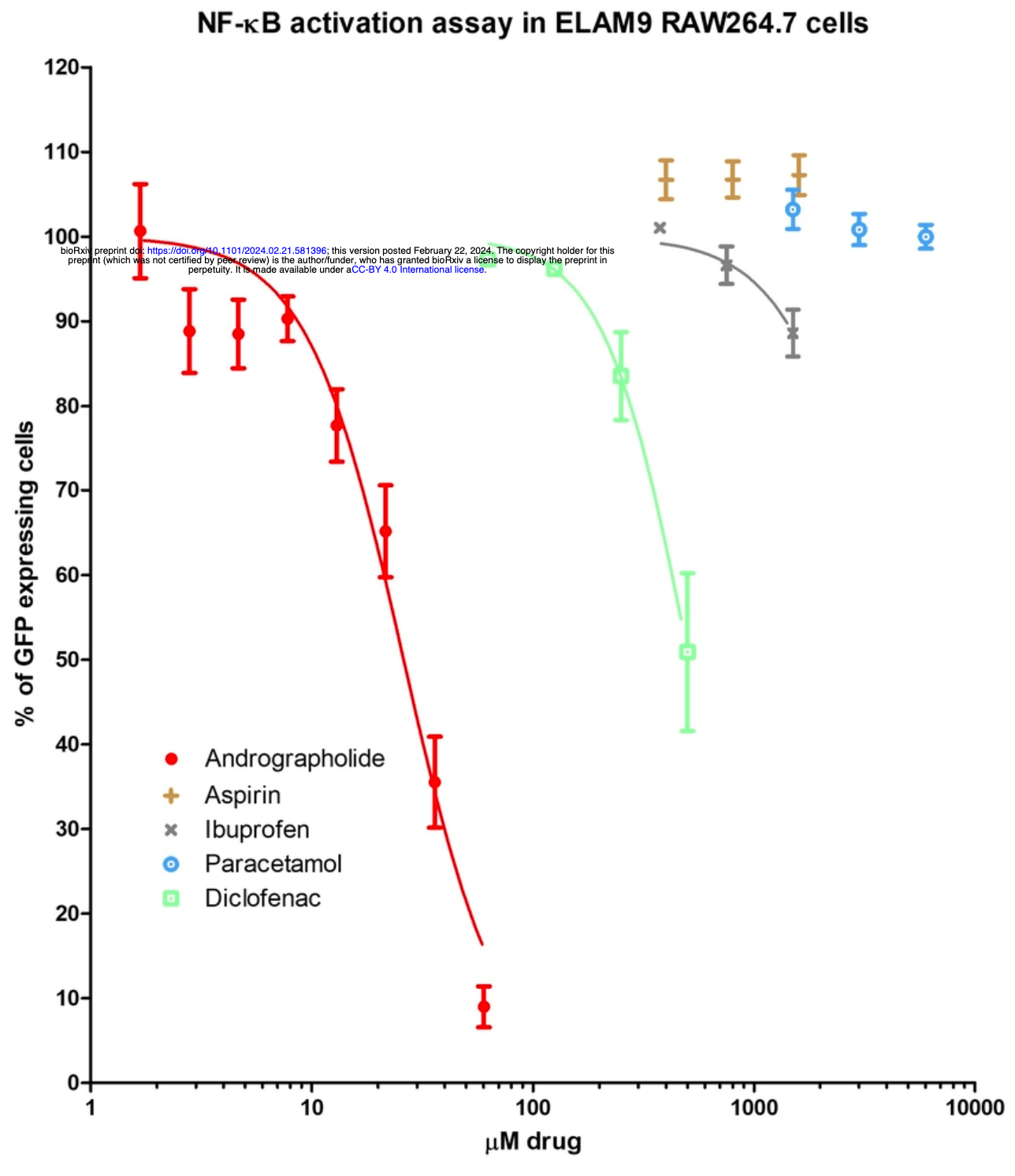
In vitro study showing that andrographolide exhibits broad anti-inflammatory and cytokine inhibiting activity against lipopolysaccharide (LPS) and interferon-γ induced inflammation in murine RAW264.7 and human THP-1 macrophage cell lines. Andrographolide significantly inhibited the release of key proinflammatory mediators involved in cytokine storm including nitric oxide (NO), prostaglandin E2 (PGE2), tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), IL-1β, and interferon-γ (IFN-γ). The cytokine-inhibiting activity of andrographolide was more potent than common nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and diclofenac. Authors suggest the anti-inflammatory mechanism of andrographolide is linked to inhibition of NFκB activation. Results indicate andrographolide may have therapeutic potential for regulating inflammation and cytokine release associated with COVID-19 infection.
25 preclinical studies support the efficacy of andrographolide for COVID-19:
In vitro studies demonstrate inhibition of the MproA,18 protein.
In vitro studies demonstrate efficacy in Calu-3B,18, A549C,14, and HUVECD,18 cells.
Animal studies demonstrate efficacy in Sprague Dawley miceE,18 and Golden Syrian hamstersF,14.
Andrographolide inhibits Mpro in a dose-dependent manner18, reduces ACE2 levels in the lung tissue of mice in combination with baicalein18, inhibits binding between the SARS-CoV-2 spike protein and ACE218, alleviates lung inflammation and cytokine storm in mice18, and improves survival and reduces lung inflammation via anti-inflammatory effects in Syrian hamsters14.
1.
Zhang et al., Effects and Mechanisms of Andrographolide for COVID-19: A Network Pharmacology-Based and Experimentally Validated Study, Natural Product Communications, doi:10.1177/1934578X241288428.
2.
Thomas et al., Cheminformatics approach to identify andrographolide derivatives as dual inhibitors of methyltransferases (nsp14 and nsp16) of SARS-CoV-2, Scientific Reports, doi:10.1038/s41598-024-58532-7.
3.
Arifin et al., Computational exploration of Andrographis paniculata herb compounds as potential antiviral agents targeting NSP3 (6W02) and NSP5 (7AR6) of SARS-COV-2, GSC Biological and Pharmaceutical Sciences, doi:10.30574/gscbps.2023.25.2.0292.
4.
Bhattarai et al., Investigating the binding affinity of andrographolide against human SARS-CoV-2 spike receptor-binding domain through docking and molecular dynamics simulations, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2023.2174596.
5.
Nguyen et al., The Potential of Ameliorating COVID-19 and Sequelae From Andrographis paniculata via Bioinformatics, Bioinformatics and Biology Insights, doi:10.1177/11779322221149622.
6.
Dassanayake et al., Molecular Docking and In-Silico Analysis of Natural Biomolecules against Dengue, Ebola, Zika, SARS-CoV-2 Variants of Concern and Monkeypox Virus, International Journal of Molecular Sciences, doi:10.3390/ijms231911131.
7.
Ningrum et al., Potency Of Andrographolide, L-Mimosine And Asiaticoside Compound As Antiviral For Covid-19 Based On In Silico Method, Proceedings Universitas Muhammadiyah Yogyakarta Undergraduate Conference, doi:10.18196/umygrace.v2i2.418.
8.
Ravichandran et al., Identification of Potential Semisynthetic Andrographolide Derivatives to Combat COVID-19 by Targeting the SARS-COV-2 Spike Protein and Human ACE2 Receptor– An In-silico Approach, Biointerface Research in Applied Chemistry, doi:10.33263/BRIAC132.155.
9.
Saeheng et al., In Silico Prediction of Andrographolide Dosage Regimens for COVID-19 Treatment, The American Journal of Chinese Medicine, doi:10.1142/S0192415X22500732.
10.
Khanal et al., Combination of system biology to probe the anti-viral activity of andrographolide and its derivative against COVID-19, RSC Advances, doi:10.1039/D0RA10529E.
11.
Rehan et al., A Computational Approach Identified Andrographolide as a Potential Drug for Suppressing COVID-19-Induced Cytokine Storm, Frontiers in Immunology, doi:10.3389/fimmu.2021.648250.
12.
Rajagopal et al., Activity of phytochemical constituents of Curcuma longa (turmeric) and Andrographis paniculata against coronavirus (COVID-19): an in silico approach, Future Journal of Pharmaceutical Sciences, doi:10.1186/s43094-020-00126-x.
13.
Dey et al., The role of andrographolide and its derivative in COVID-19 associated proteins and immune system, Research Square, doi:10.21203/rs.3.rs-35800/v1.
14.
Kongsomros et al., In vivo evaluation of Andrographis paniculata and Boesenbergia rotunda extract activity against SARS-CoV-2 Delta variant in Golden Syrian hamsters: Potential herbal alternative for COVID-19 treatment, Journal of Traditional and Complementary Medicine, doi:10.1016/j.jtcme.2024.05.004.
15.
Chaopreecha et al., Andrographolide attenuates SARS-CoV-2 infection via an up-regulation of glutamate-cysteine ligase catalytic subunit (GCLC), Phytomedicine, doi:10.1016/j.phymed.2024.156279.
16.
Li et al., Andrographolide suppresses SARS-CoV-2 infection by downregulating ACE2 expression: A mechanistic study, Antiviral Therapy, doi:10.1177/13596535241259952.
17.
Low et al., The wide spectrum anti-inflammatory activity of andrographolide in comparison to NSAIDs: a promising therapeutic compound against the cytokine storm, bioRxiv, doi:10.1101/2024.02.21.581396.
18.
Wan et al., Synergistic inhibition effects of andrographolide and baicalin on coronavirus mechanisms by downregulation of ACE2 protein level, Scientific Reports, doi:10.1038/s41598-024-54722-5.
19.
Siridechakorn et al., Inhibitory efficiency of Andrographis paniculata extract on viral multiplication and nitric oxide production, Scientific Reports, doi:10.1038/s41598-023-46249-y.
a.
The main protease or Mpro, also known as 3CLpro or nsp5, is a cysteine protease that cleaves viral polyproteins into functional units needed for replication. Inhibiting Mpro disrupts the SARS-CoV-2 lifecycle within the host cell, preventing the creation of new copies.
b.
Calu-3 is a human lung adenocarcinoma cell line with moderate ACE2 and TMPRSS2 expression and SARS-CoV-2 susceptibility. It provides a model of the human respiratory epithelium, but many not be ideal for modeling early stages of infection due to the moderate expression levels of ACE2 and TMPRSS2.
c.
A549 is a human lung carcinoma cell line with low ACE2 expression and SARS-CoV-2 susceptibility. Viral entry/replication can be studied but the cells may not replicate all aspects of lung infection.
d.
HUVEC (Human Umbilical Vein Endothelial Cells) are primary endothelial cells derived from the vein of the umbilical cord. They are used to study vascular biology, including inflammation, angiogenesis, and viral interactions with endothelial cells.
e.
An outbred multipurpose breed of albino mouse used extensively in medical research.
f.
A rodent model widely used in infectious disease research due to their susceptibility to viral infections and similar disease progression to humans.
Low et al., 22 Feb 2024, preprint, 8 authors.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
The wide spectrum anti-inflammatory activity of andrographolide in comparison to NSAIDs: a promising therapeutic compound against the cytokine storm
doi:10.1101/2024.02.21.581396
The challenges of the COVID-19 pandemic have highlighted an increasing clinical demand for safe and effective treatment options against an overzealous immune defence response, also known as the "cytokine storm". Andrographolide is a naturally derived bioactive compound with promising anti-inflammatory activity in many clinical studies. However, its cytokine-inhibiting activity, in direct comparison to commonly used nonsteroidal anti-inflammatory drugs (NSAIDs), has not been extensively investigated in existing literature. The anti-inflammatory activities of andrographolide and common NSAIDs, such as diclofenac, aspirin, paracetamol and ibuprofen were measured on lipopolysaccharide (LPS) and interferon-γ induced RAW264.7 cells. The levels of PGE2, nitric oxide (NO), TNF-α & LPS-induced release of pro-inflammatory cytokines on differentiated human macrophage THP-1 cells were measured against increasing concentrations of andrographolide and aforementioned NSAIDs. The associated mechanistic pathway was examined on NFκB using flow cytometry on the human endothelial-leukocyte adhesion molecule (ELAM9) (E-selectin) transfected RAW264.7 cells with green fluorescent protein (GFP). Andrographolide exhibited broad and potent anti-inflammatory and cytokineinhibiting activity in both cell lines by inhibiting the release of IL-6, TNF-α and IFN-γ, which are known to play a key role in the etiology of cytokine storm and the pathogenesis of inflammation. In comparison, the tested NSAIDs demonstrated weak or no activity against proinflammatory mediators except for PGE2, where the activity of andrographolide (IC 50 = 8.8 µM, 95% CI= 7.4 to 10.4 µM) was comparable to that of paracetamol (IC 50 = 7.73 µM, 95% CI = 6.14 to 9.73 µM). The anti-inflammatory action of andrographolide was associated with its potent downregulation of NFκB. The wide-spectrum anti-inflammatory activity of andrographolide demonstrates its therapeutic potential against cytokine storms as an alternative to NSAIDs.
Conflicts of Interest: The authors declare no conflict of interest.
References
Abc, Do I have the flu, COVID-19 or RSV? Let's unpack the difference in symptoms of these viruses
Abc, Respiratory syncytial virus cases are rising in Australia -how is testing done? Available online
Akbar, Andrographis paniculata: a review of pharmacological activities and clinical effects, Alternative medicine review : a journal of clinical therapeutic
Bachmann, Oxenius, Interleukin 2: from immunostimulation to immunoregulation and back again, EMBO reports
Bhuyan, Alsherbiny, Low, Zhou, Kaur et al., Broad-spectrum pharmacological activity of Australian propolis and metabolomic-driven identification of marker metabolites of propolis samples from three continents, Food Funct, doi:10.1039/d1fo00127b
Bogdan, Röllinghoff, Diefenbach, The role of nitric oxide in innate immunity, Immunological reviews
Canvin, El-Gabalawy, Anti-inflammatory therapy, Phys Med Rehabil Clin N Am
Chao, Lin, Isolation and identification of bioactive compounds in Andrographis paniculata (Chuanxinlian), Chinese medicine
Chiou, Lin, Chen, Andrographolide suppresses the expression of inducible nitric oxide synthase in macrophage and restores the vasoconstriction in rat aorta treated with lipopolysaccharide, British journal of pharmacology
Dediego, Nieto-Torres, Regla-Nava, Jimenez-Guardeño, Fernandez-Delgado et al., Inhibition of NF-κB-mediated inflammation in severe acute respiratory syndrome coronavirus-infected mice increases survival, Journal of virology
Ding, Chen, Wu, Yang, Yang et al., Andrographolide inhibits influenza a virus-induced inflammation in a murine model through NF-κB and JAK-STAT signaling pathway, Microbes and infection
Favalli, Ingegnoli, De Lucia, Cincinelli, Cimaz et al., COVID-19 infection and rheumatoid arthritis: Faraway, so close!, Autoimmunity reviews
Giavridis, Van Der Stegen, Eyquem, Hamieh, Piersigilli et al., CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade, Nature medicine
Giollo, Adami, Gatti, Idolazzi, Rossini, Coronavirus disease 19 (Covid-19) and non-steroidal antiinflammatory drugs (NSAID), Annals of the Rheumatic Diseases
Guan, Tee, Ng, Chan, Peh et al., Andrographolide protects against cigarette smoke-induced oxidative lung injury via augmentation of Nrf2 activity, British journal of pharmacology
Guo, Cao, Hong, Tan, Chen et al., The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-an update on the status, Military Medical Research
Handa, Sharma, Hepatoprotective Activity of Andrographolide from Andrographis-Paniculata against Carbontetrachloride, Indian J Med Res-B
Hawboldt, Adverse Events Associated with NSAIDs, GASTROENTEROLOGY
Hossain, Urbi, Sule, Hafizur Rahman, Andrographis Paniculata (burm, f.) Wall. ex Nees: a review of ethnobotany, phytochemistry, and pharmacology, ScientificWorldJournal, doi:10.1155/2014/274905
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, The Lancet
Hurdayal, Brombacher, Interleukin-4 receptor alpha: from innate to adaptive immunity in murine models of cutaneous leishmaniasis, Frontiers in immunology
Hussell, Pennycook, Openshaw, Inhibition of tumor necrosis factor reduces the severity of virus-specific lung immunopathology, European journal of immunology
Jarukamjorn, Nemoto, Pharmacological aspects of Andrographis paniculata on health and its major diterpenoid constituent andrographolide, J Health Sci, doi:10.1248/Jhs.54.370
Karunaweera, Raju, Gyengesi, Münch, Plant polyphenols as inhibitors of NF-κB induced cytokine productiona potential anti-inflammatory treatment for Alzheimer's disease?, Frontiers in molecular neuroscience, doi:10.3389/fnmol.2015.00024
Kaur, Dufour, Cell lines: Valuable tools or useless artifacts, Spermatogenesis, doi:`10.4161/spmg.19885
Kim, Lertnimitphun, Jiang, Tan, Zhou et al., Andrographolide inhibits inflammatory responses in LPS-stimulated macrophages and murine acute colitis through activating AMPK, Biochemical pharmacology
Koehn, Carter, The evolving role of natural products in drug discovery, Nat Rev Drug Discov
Koffeman, Valkhoff, Celik, Jong, Sturkenboom et al., High-risk use of over-the-counter non-steroidal anti-inflammatory drugs: a populationbased cross-sectional study, Brit J Gen Pract, doi:10.3399/bjgp14X677815
Kulesza, Zielniok, Hawryluk, Paczek, Burdzinska, Ibuprofen in Therapeutic Concentrations Affects the Secretion of Human Bone Marrow Mesenchymal Stromal Cells, but Not Their Proliferative and Migratory Capacity, Biomolecules, doi:10.3390/biom12020287
Kushner, Mccarberg, Grange, The use of non-steroidal anti-inflammatory drugs (NSAIDs) in COVID-19, Prim Care Respir Med, doi:10.1038/s41533-022-00300-z
Laughey, Lodhi, Pennick, Ibuprofen, other NSAIDs and COVID-19: a narrative review, Inflammopharmacol, doi:10.1007/s10787-023-01309-7
Levita, Nawawi, Mutholib, Ibrahim, Andrographolide inhibits COX-2 expression in human fibroblast cells due to its interaction with arginine and histidine in cyclooxygenase site, J Appl Sci
Li, -Z.; Tan, Wang, Li, Andrographolide benefits rheumatoid arthritis via inhibiting MAPK pathways, Inflammation
Li, Zhang, Zhu, Wang, Jin, Liposomal andrographolide dry powder inhalers for treatment of bacterial pneumonia via anti-inflammatory pathway, International journal of pharmaceutics
Little, Non-steroidal anti-inflammatory drugs and covid-19
Liu, Zhang, Zheng, Chen, Yu et al., Gastroprotective effect of andrographolide sodium bisulfite against indomethacin-induced gastric ulceration in rats, International immunopharmacology
Marinella, Indomethacin and resveratrol as potential treatment adjuncts for SARS-CoV-2/COVID-19, International journal of clinical practice, doi:10.1111/ijcp.13535
Mehra, Ruschitzka, COVID-19 Illness and Heart Failure A Missing Link?, JACC: HEART FAILURE, doi:10.1016/j.jchf.2020.03.004
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: consider cytokine storm syndromes and immunosuppression, The Lancet
Mohammed, Fighting cytokine storm and immunomodulatory deficiency: By using natural products therapy up to now, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1111329
Moore, Coronary Risks Associated with Diclofenac and Other NSAIDs: An Update, Drug Safety
Moore, June, Cytokine release syndrome in severe COVID-19, Science
Mukherjee, Wahile, Integrated approaches towards drug development from Ayurveda and other Indian system of medicines, J Ethnopharmacol, doi:10.1016/j.jep.2005.09.024
Needleman, Manning, Interactions between the inducible cyclooxygenase (COX-2) and nitric oxide synthase (iNOS) pathways: implications for therapeutic intervention in osteoarthritis, Osteoarthritis and cartilage
Newman, Cragg, Natural products as sources of new drugs over the last 25 years, Journal of natural products
Patwardhan, Warude, Pushpangadan, Bhatt, Ayurveda and traditional Chinese medicine: A comparative overview, Evid-Based Compl Alt, doi:10.1093/Ecam/Neh140
Peprotech, ELISA: Sandwich TMB
Ragab, Eldin, Taeimah, Khattab, Salem, The COVID-19 Cytokine Storm; What We Know So Far, Frontiers in Immunology, doi:10.3389/fimmu.2020.01446
Ramana, Deberge, Kumar, Alia, Durbin et al., Inflammatory impact of IFN-γ in CD8+ T cellmediated lung injury is mediated by both Stat1-dependent and-independent pathways, American Journal of Physiology-Lung Cellular and Molecular Physiology
Ramatillah, Gan, Pratiwy, Sulaiman, Jaber et al., Impact of cytokine storm on severity of COVID-19 disease in a private hospital in West Jakarta prior to vaccination, Plos One, doi:10.1371/journal.pone.0262438
Ritchie, Singanayagam, Immunosuppression for hyperinflammation in COVID-19: a double-edged sword?, The Lancet
Roberts, Dunn, Terry, Jennings, Hume et al., Differences in macrophage activation by bacterial DNA and CpG-containing oligonucleotides, The Journal of Immunology
Rouhi, Rediscovering natural products, Chemical & Engineering News
Russell, Moss, George, Santaolalla, Cope et al., Associations between immunesuppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence, ecancermedicalscience
Ryabkova, Churilov, Shoenfeld, Influenza infection, SARS, MERS and COVID-19: Cytokine storm -The common denominator and the lessons to be learned, Clin Immunol, doi:10.1016/j.clim.2020.108652
Santos, Holloway, Custer, Alves, Simon, Encephalitis and cytokine storm secondary to respiratory viruses in children: Two case reports, Front Pediatr, doi:10.3389/fped.2022.1049724
Saranya, Geetha, Selvamathy, A biochemical study on the gastroprotective effect of andrographolide in rats induced with gastric ulcer, Indian journal of pharmaceutical sciences, doi:10.4103/0250-474X.99012
Shang, -X.; Shen, Stub, Zhu, -J.; Qiao et al., Adverse Effects of Andrographolide Derivative Medications Compared to the Safe use of Herbal Preparations of Andrographis paniculata: Results of a Systematic Review and Meta-Analysis of Clinical Studies, Front Pharmacol, doi:10.3389/fphar.2022.773282
Shirey, Pletneva, Puche, Keegan, Prince et al., Control of RSV-induced lung injury by alternatively activated macrophages is IL-4R alpha-, TLR4-, and IFN-beta-dependent, Mucosal Immunol, doi:10.1038/mi.2010.6
Stacey, Young, Clark, Sester, Roberts et al., The molecular basis for the lack of immunostimulatory activity of vertebrate DNA, The Journal of Immunology, doi:10.4049/jimmunol.170.7.3614
Suryavanshi, Zaiachuk, Pryimak, Kovalchuk, Kovalchuk, Cannabinoids Alleviate the LPS-Induced Cytokine Storm via Attenuating NLRP3 Inflammasome Signaling and TYK2-Mediated STAT3 Signaling Pathways In Vitro, Cells, doi:10.3390/cells11091391
Taciak, Białasek, Braniewska, Sas, Sawicka et al., Evaluation of phenotypic and functional stability of RAW 264.7 cell line through serial passages, PloS One, doi:10.1371/journal.pone.0198943
Trivedi, Abbas, Lehmann, Rupasinghe, Antiviral and Anti-Inflammatory Plant-Derived Bioactive Compounds and Their Potential Use in the Treatment of COVID-19-Related Pathologies, J Xenobiot, doi:10.3390/jox12040020
Worakunphanich, Thavorncharoensap, Youngkong, Thadanipon, Thakkinstian, Safety of Andrographis paniculata: A systematic review and metaanalysis, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.5190
Wu, Yang, TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib, Journal of Microbiology, Immunology and Infection
Xi-Zhi, Thomas, New fronts emerge in the influenza cytokine storm
Xu, Han, Li, Sun, Wang et al., Effective treatment of severe COVID-19 patients with tocilizumab, Proceedings of the National Academy of Sciences
Zeng, Wei, Zhou, Yuan, Lei et al., Andrographolide: A review of its pharmacology, pharmacokinetics, toxicity and clinical trials and pharmaceutical researches, Phytotherapy Research, doi:10.1002/ptr.7324
Zhang, An, Cytokines, inflammation and pain, International anesthesiology clinics
Zhou, Zhao, Gan, Wang, Peng et al., Use of non-steroidal antiinflammatory drugs and adverse outcomes during the COVID-19 pandemic: A systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2022.101373