Effectiveness of molnupiravir and nirmatrelvir–ritonavir in CKD patients with COVID-19
et al., Kidney International Reports, doi:10.1016/j.ekir.2024.02.009, Feb 2024
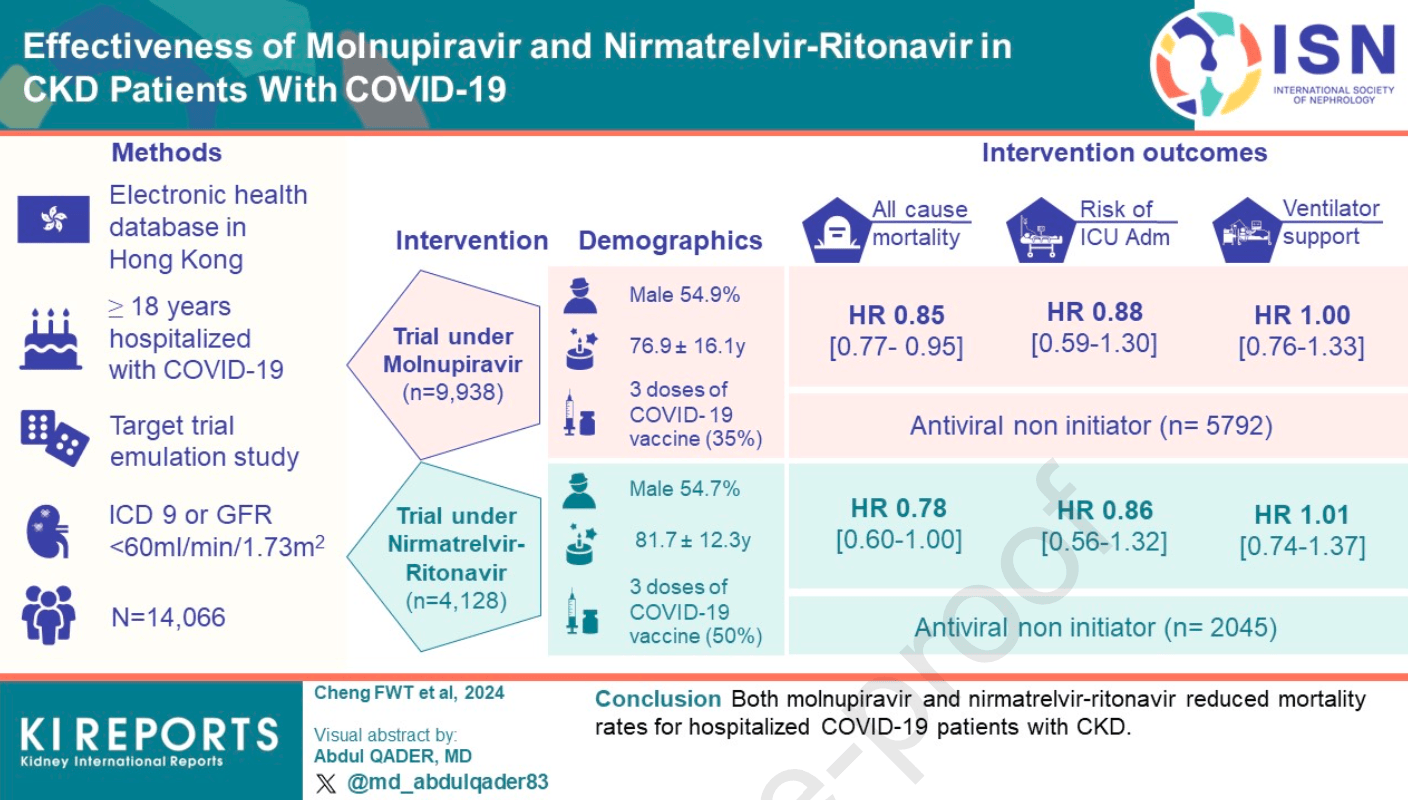
Retrospective emulated target trial of hospitalized COVID-19 patients with chronic kidney disease in Hong Kong showing lower mortality with molnupiravir and paxlovid treatment. No significant reduction was found in ICU admission or ventilatory support.
Notably, there is no estimated benefit for ventilatory support, the outcome most directly related to severe COVID-19.
The very large difference in vaccine uptake suggests major confounding issues, for example treatment decisions based on vaccine uptake, or confounding by time where control patients are more likely from earlier periods with lower vaccine uptake, which may also correspond to more dangerous variants.
Potential risks of molnupiravir include the creation of dangerous variants, and mutagenicity, carcinogenicity, teratogenicity, and embryotoxicity1-15. Multiple analyses have identified variants potentially created by molnupiravir16-20. Studies show significantly increased risk of acute kidney injury21, cardiovascular toxocity22, and neurological symptoms21. Treatment may increase viral rebound23,24.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments25.
Study covers molnupiravir and paxlovid.
|
risk of death, 14.6% lower, HR 0.85, p = 0.003, treatment 4,146, control 5,792.
|
|
ventilatory support, 0.1% higher, HR 1.00, p = 1.00, treatment 4,146, control 5,792.
|
|
risk of ICU admission, 12.5% lower, HR 0.88, p = 0.52, treatment 4,146, control 5,792.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Swanstrom et al., Lethal mutagenesis as an antiviral strategy, Science, doi:10.1126/science.abn0048.
2.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
3.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
4.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
5.
Huntsman, M., An assessment of the reproductive toxicity of the anti-COVID-19 drug molnupiravir using stem cell-based embryo models, Master's Thesis, scholarspace.manoa.hawaii.edu/items/cd11342c-b4dc-44c0-8b44-ce6e3369c40b.
6.
Huntsman (B) et al., Detection of developmental toxicity of the anti-COVID-19 drug molnupiravir using gastruloid-based in vitro assays, Toxicological Sciences, doi:10.1093/toxsci/kfaf093.
7.
Zibat et al., N4-hydroxycytidine, the active compound of Molnupiravir, promotes SARS-CoV-2 mutagenesis and escape from a neutralizing nanobody, iScience, doi:10.1016/j.isci.2023.107786.
8.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
9.
Gruber et al., Molnupiravir increases SARS‐CoV‐2 genome diversity and complexity: A case‐control cohort study, Journal of Medical Virology, doi:10.1002/jmv.29642.
10.
Marikawa et al., An active metabolite of the anti-COVID-19 drug molnupiravir impairs mouse preimplantation embryos at clinically relevant concentrations, Reproductive Toxicology, doi:10.1016/j.reprotox.2023.108475.
11.
Rahman, M., Elucidation of the DNA repair mechanisms involved in the repair of DNA damage caused by the Arabinosides and Anti-COVID-19 drugs, tokyo-metro-u.repo.nii.ac.jp/records/2000972.
12.
Zhou et al., β-D-N4-hydroxycytidine Inhibits SARS-CoV-2 Through Lethal Mutagenesis But Is Also Mutagenic To Mammalian Cells, The Journal of Infectious Diseases, doi:10.1093/infdis/jiab247.
13.
Chamod et al., Molnupiravir Metabolite--N4-hydroxycytidine Causes Cytotoxicity and DNA Damage in Mammalian Cells in vitro: N4-hydroxycytidine Induced Cytotoxicity DNA Damage, Asian Medical Journal and Alternative Medicine, 23:3, asianmedjam.com/index.php/amjam/article/view/1448.
14.
Standing et al., Randomized controlled trial of molnupiravir SARS-CoV-2 viral and antibody response in at-risk adult outpatients, Nature Communications, doi:10.1038/s41467-024-45641-0.
15.
Mori et al., Reactive oxygen species-mediated cytotoxic and DNA-damaging mechanism of N4-hydroxycytidine, a metabolite of the COVID-19 therapeutic drug molnupiravir, Free Radical Research, doi:10.1080/10715762.2025.2469738.
16.
Focosi et al., The fitness of molnupiravir-signed SARS-CoV-2 variants: imputation analysis based on prescription counts and GISAID analyses by country, Intervirology, doi:10.1159/000540282.
17.
Sanderson et al., A molnupiravir-associated mutational signature in global SARS-CoV-2 genomes, Nature, doi:10.1038/s41586-023-06649-6.
18.
Fountain-Jones et al., Effect of molnupiravir on SARS-CoV-2 evolution in immunocompromised patients: a retrospective observational study, The Lancet Microbe, doi:10.1016/S2666-5247(23)00393-2.
19.
Kosakovsky Pond et al., Anti-COVID drug accelerates viral evolution, Nature, doi:10.1038/d41586-023-03248-3.
21.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
22.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
23.
Shah et al., SARS-CoV-2 infectious shedding and rebound among adults with and without oral antiviral use: two case-ascertained prospective household studies, The Lancet Microbe, doi:10.1016/j.lanmic.2025.101227.
Cheng et al., 9 Feb 2024, retrospective, China, peer-reviewed, 11 authors.
Contact: ewchan@hku.hk, wongick@hku.hk.
Effectiveness of molnupiravir and nirmatrelvir–ritonavir in CKD patients with COVID-19.
Kidney International Reports, doi:10.1016/j.ekir.2024.02.009
Introduction Even with effective vaccines, patients with CKD have a higher risk of hospitalization and death subsequent to COVID-19 infection compared with those without CKD. Molnupiravir and nirmatrelvir-ritonavir have been approved for emergency use, but their effectiveness for the CKD population is still unknown. This study was conducted to determine the effectiveness of these drugs in reducing mortality and severe COVID-19 in the CKD population. Methods This was a target trial emulation study using electronic health databases in Hong Kong. Patients with CKD aged 18 years or older who were hospitalized with COVID-19 were included. The per-protocol average treatment effect among COVID-19 oral antiviral initiators, including all-cause mortality, ICU admission, and ventilatory support within 28 days, were compared to non-initiators.
Results Antivirals have been found to lower the risk of all-cause mortality, with molnupiravir at a hazard ratio (HR) of 0.85 [95% CI, 0.77 to 0.95] and nirmatrelvir-ritonavir at an HR of 0.78 [CI, 0.60 to 1.00]. However, they do not significantly reduce the risk of ICU admission (molnupiravir: HR, 0.88 [CI, 0.59 to 1.30]; nirmatrelvir-ritonavir: HR, 0.86 [CI, 0.56 to 1.32]) or ventilatory support (molnupiravir: HR, 1.00 [CI, 0.76 to 1.33]; nirmatrelvir-ritonavir: HR, 1.01 [CI, 0.74 to 1.37]). There was a greater risk reduction in males and those with higher Charlson Comorbidity Index. The nirmatrelvir-ritonavir trial also showed reduced risk for those who had antiviral treatment and received three or more vaccine doses.
Conclusion Both molnupiravir and nirmatrelvir-ritonavir reduced mortality rates for hospitalized COVID-19 patients with CKD.
Supplementary Material STROBE statement (PDF) Supplementary Table S1 Target trial specification and emulation using observational data (PDF) Supplementary Table S2 . Baseline and post-assignment covariates for the construction of inverse probability weights (PDF) Supplementary Table S3 . Survival Probability for Outcomes in COVID-19 Oral Antiviral Initiators Compared With Non-initiators (PDF) Supplementary information is available at KI Report's website. J o u r n a l P r e -p r o o f
References
Agostino, Lee, Belanger, Cupples, Anderson et al., Relation of pooled logistic regression to time dependent Cox regression analysis: the Framingham Heart Study, Stat Med
Arribas, Bhagani, Lobo, Randomized Trial of Molnupiravir or Placebo in Patients Hospitalized with Covid-19, NEJM Evidence
Bernal, Da Silva, Musungaie, Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients, N Engl J Med
Carr, Kronbichler, Graham-Brown, Review of Early Immune Response to SARS-CoV-2 Vaccination Among Patients With CKD, Kidney Int Rep
Cheng, Fan, Wong, The effectiveness and safety of mRNA (BNT162b2) and inactivated (CoronaVac) COVID-19 vaccines among individuals with chronic kidney diseases, Kidney Int
Cheng, Wong, Qin, Risk of glomerular diseases, proteinuria and hematuria following mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines, Nephrol Dial Transplant
Cho, Harden, Moreno, Oral antiviral therapies for COVID-19 in patients with advanced chronic kidney disease or kidney failure, Nephrol Dial Transplant
Chua, Kwan, Chui, Epidemiology of Acute Myocarditis/Pericarditis in Hong Kong Adolescents Following Comirnaty Vaccination, Clin Infect Dis
Chui, Wan, Thromboembolic events and hemorrhagic stroke after mRNA (BNT162b2) and inactivated (CoronaVac) covid-19 vaccination: a self-controlled case series study
Flythe, Assimon, Tugman, Characteristics and Outcomes of Individuals With Pre-existing Kidney Disease and COVID-19 Admitted to Intensive Care Units in the United States, Am J Kidney Dis
Hammond, Leister-Tebbe, Gardner, Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19, N Engl J Med
Harrison, Fazio-Eynullayeva, Lane, Underhill, Lip, Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: A federated electronic medical record analysis, PLoS medicine
Hernán, Brumback, Robins, Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men, Epidemiology
Hernán, Methods of Public Health Research -Strengthening Causal Inference from Observational Data, New England Journal of Medicine
Hernán, Robins, Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available, Am J Epidemiol
J O U R N A L P R E, None
Kale, Shelke, Dagar, Anders, Gaikwad, How to use COVID-19 antiviral drugs in patients with chronic kidney disease, Front Pharmacol
Khan, Khan, Mustagir, Rana, Islam et al., Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: A systematic review and meta-analysis, J Glob Health
Kragholm, Andersen, Gerds, Association Between Male Sex and Outcomes of Coronavirus Disease 2019 (COVID-19)-A Danish Nationwide, Registerbased Study, Clin Infect Dis
Lai, Li, Peng, Carditis After COVID-19 Vaccination With a Messenger RNA Vaccine and an Inactivated Virus Vaccine : A Case-Control Study, Ann Intern Med
Lawrence, Mirchandani, Hill, Evaluation of publication bias for 12 clinical trials of molnupiravir to treat SARS-CoV-2 infection in 13,694 patients
Peckham, De Gruijter, Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission, Nat Commun
Petrilli, Jones, Yang, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Planas, Saunders, Maes, Considerable escape of SARS-CoV-2 Omicron to antibody neutralization, Nature
Taji, Thomas, Oliver, COVID-19 in patients undergoing long-term dialysis in Ontario, CMAJ
Toussi, Neutel, Navarro, Pharmacokinetics of Oral Nirmatrelvir/Ritonavir, a Protease Inhibitor for Treatment of COVID-19, in Subjects With Renal Impairment, Clin Pharmacol Ther
Wan, Chui, Lai, Bell's palsy following vaccination with mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines: a case series and nested case-control study, Lancet Infect Dis
Wan, Chui, Wang, Herpes zoster related hospitalization after inactivated (CoronaVac) and mRNA (BNT162b2) SARS-CoV-2 vaccination: A self-controlled case series and nested case-control study, Lancet Reg Health West Pac
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature
Wong, Lau, Xiong, Adverse events of special interest and mortality following vaccination with mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines in Hong Kong: A retrospective study, PLoS Med
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, The lancet
DOI record:
{
"DOI": "10.1016/j.ekir.2024.02.009",
"ISSN": [
"2468-0249"
],
"URL": "http://dx.doi.org/10.1016/j.ekir.2024.02.009",
"alternative-id": [
"S2468024924000986"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Effectiveness of molnupiravir and nirmatrelvir–ritonavir in CKD patients with COVID-19."
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Kidney International Reports"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.ekir.2024.02.009"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2024 Published by Elsevier Inc. on behalf of the International Society of Nephrology."
}
],
"author": [
{
"affiliation": [],
"family": "Cheng",
"given": "Franco Wing Tak",
"sequence": "first"
},
{
"affiliation": [],
"family": "Yan",
"given": "Vincent Ka Chun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wan",
"given": "Eric Yuk Fai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chui",
"given": "Celine Sze Ling",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lai",
"given": "Francisco Tsz Tsun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wong",
"given": "Carlos King Ho",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Xue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Irene Ran",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tang",
"given": "Sydney Chi Wai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wong",
"given": "Ian Chi Kei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chan",
"given": "Esther Wai Yin",
"sequence": "additional"
}
],
"container-title": "Kidney International Reports",
"container-title-short": "Kidney International Reports",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"kireports.org",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2024,
2,
9
]
],
"date-time": "2024-02-09T17:40:16Z",
"timestamp": 1707500416000
},
"deposited": {
"date-parts": [
[
2024,
2,
9
]
],
"date-time": "2024-02-09T17:40:32Z",
"timestamp": 1707500432000
},
"indexed": {
"date-parts": [
[
2024,
2,
11
]
],
"date-time": "2024-02-11T12:16:36Z",
"timestamp": 1707653796441
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
2
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
1
]
],
"date-time": "2024-02-01T00:00:00Z",
"timestamp": 1706745600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 5,
"start": {
"date-parts": [
[
2024,
2,
6
]
],
"date-time": "2024-02-06T00:00:00Z",
"timestamp": 1707177600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2468024924000986?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2468024924000986?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"prefix": "10.1016",
"published": {
"date-parts": [
[
2024,
2
]
]
},
"published-print": {
"date-parts": [
[
2024,
2
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "Williamson",
"doi-asserted-by": "crossref",
"first-page": "430",
"journal-title": "Nature",
"key": "10.1016/j.ekir.2024.02.009_bib1",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.7189/jogh.10.020503",
"article-title": "Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: A systematic review and meta-analysis",
"author": "Khan",
"doi-asserted-by": "crossref",
"journal-title": "J Glob Health",
"key": "10.1016/j.ekir.2024.02.009_bib2",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1053/j.ajkd.2020.09.003",
"article-title": "Characteristics and Outcomes of Individuals With Pre-existing Kidney Disease and COVID-19 Admitted to Intensive Care Units in the United States",
"author": "Flythe",
"doi-asserted-by": "crossref",
"first-page": "190",
"journal-title": "Am J Kidney Dis",
"key": "10.1016/j.ekir.2024.02.009_bib3",
"volume": "77",
"year": "2021"
},
{
"article-title": "The effectiveness and safety of mRNA (BNT162b2) and inactivated (CoronaVac) COVID-19 vaccines among individuals with chronic kidney diseases",
"author": "Cheng",
"issue": "22",
"journal-title": "Kidney Int",
"key": "10.1016/j.ekir.2024.02.009_bib4",
"volume": "S0085-2538",
"year": "2022"
},
{
"DOI": "10.1503/cmaj.202601",
"article-title": "COVID-19 in patients undergoing long-term dialysis in Ontario",
"author": "Taji",
"doi-asserted-by": "crossref",
"first-page": "E278",
"journal-title": "CMAJ",
"key": "10.1016/j.ekir.2024.02.009_bib5",
"volume": "193",
"year": "2021"
},
{
"DOI": "10.1016/j.ekir.2021.06.027",
"article-title": "Review of Early Immune Response to SARS-CoV-2 Vaccination Among Patients With CKD",
"author": "Carr",
"doi-asserted-by": "crossref",
"first-page": "2292",
"journal-title": "Kidney Int Rep",
"key": "10.1016/j.ekir.2024.02.009_bib6",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1038/s41586-021-04389-z",
"article-title": "Considerable escape of SARS-CoV-2 Omicron to antibody neutralization",
"author": "Planas",
"doi-asserted-by": "crossref",
"first-page": "671",
"journal-title": "Nature",
"key": "10.1016/j.ekir.2024.02.009_bib7",
"volume": "602",
"year": "2022"
},
{
"key": "10.1016/j.ekir.2024.02.009_bib8",
"unstructured": "Update: FDA Authorizes Additional Oral Antiviral Treatment of COVID-19 in Certain Adults. 2021;"
},
{
"key": "10.1016/j.ekir.2024.02.009_bib9",
"unstructured": "Update: FDA authorizes first oral antiviral for treatment of COVID-19. 2021;"
},
{
"DOI": "10.1056/NEJMoa2116044",
"article-title": "Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients",
"author": "Jayk Bernal",
"doi-asserted-by": "crossref",
"first-page": "509",
"journal-title": "N Engl J Med",
"key": "10.1016/j.ekir.2024.02.009_bib10",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2118542",
"article-title": "Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19",
"author": "Hammond",
"doi-asserted-by": "crossref",
"first-page": "1397",
"journal-title": "N Engl J Med",
"key": "10.1016/j.ekir.2024.02.009_bib11",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.3389/fphar.2023.1053814",
"article-title": "How to use COVID-19 antiviral drugs in patients with chronic kidney disease",
"author": "Kale",
"doi-asserted-by": "crossref",
"journal-title": "Front Pharmacol",
"key": "10.1016/j.ekir.2024.02.009_bib12",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1002/cpt.2688",
"article-title": "Pharmacokinetics of Oral Nirmatrelvir/Ritonavir, a Protease Inhibitor for Treatment of COVID-19, in Subjects With Renal Impairment",
"author": "Toussi",
"doi-asserted-by": "crossref",
"first-page": "892",
"journal-title": "Clin Pharmacol Ther",
"key": "10.1016/j.ekir.2024.02.009_bib13",
"volume": "112",
"year": "2022"
},
{
"key": "10.1016/j.ekir.2024.02.009_bib14",
"unstructured": "Free COVID-19 oral drugs plan set. 2022;"
},
{
"key": "10.1016/j.ekir.2024.02.009_bib15",
"unstructured": "LCQ7: Introduction of new drugs for treating Coronavirus Disease 2019. 2022;"
},
{
"key": "10.1016/j.ekir.2024.02.009_bib16",
"unstructured": "First shipment of COVID-19 oral drug Paxlovid distributed to HA for application (with photos). 2022;"
},
{
"article-title": "Risk of glomerular diseases, proteinuria and hematuria following mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines",
"author": "Cheng",
"journal-title": "Nephrol Dial Transplant",
"key": "10.1016/j.ekir.2024.02.009_bib17",
"year": "2022"
},
{
"article-title": "Epidemiology of Acute Myocarditis/Pericarditis in Hong Kong Adolescents Following Comirnaty Vaccination",
"author": "Chua",
"journal-title": "Clin Infect Dis",
"key": "10.1016/j.ekir.2024.02.009_bib18",
"year": "2021"
},
{
"DOI": "10.1016/j.eclinm.2022.101504",
"article-title": "Thromboembolic events and hemorrhagic stroke after mRNA (BNT162b2) and inactivated (CoronaVac) covid-19 vaccination: a self-controlled case series study",
"author": "Chui",
"doi-asserted-by": "crossref",
"journal-title": "eClinicalMedicine",
"key": "10.1016/j.ekir.2024.02.009_bib19",
"year": "2022"
},
{
"DOI": "10.7326/M21-3700",
"article-title": "Carditis After COVID-19 Vaccination With a Messenger RNA Vaccine and an Inactivated Virus Vaccine : A Case-Control Study",
"author": "Lai",
"doi-asserted-by": "crossref",
"journal-title": "Ann Intern Med",
"key": "10.1016/j.ekir.2024.02.009_bib20",
"year": "2022"
},
{
"DOI": "10.1016/S1473-3099(21)00451-5",
"article-title": "Bell’s palsy following vaccination with mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines: a case series and nested case-control study",
"author": "Wan",
"doi-asserted-by": "crossref",
"first-page": "64",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.ekir.2024.02.009_bib21",
"volume": "22",
"year": "2022"
},
{
"article-title": "Herpes zoster related hospitalization after inactivated (CoronaVac) and mRNA (BNT162b2) SARS-CoV-2 vaccination: A self-controlled case series and nested case-control study",
"author": "Wan",
"journal-title": "Lancet Reg Health West Pac",
"key": "10.1016/j.ekir.2024.02.009_bib22",
"volume": "21",
"year": "2022"
},
{
"DOI": "10.1371/journal.pmed.1004018",
"article-title": "Adverse events of special interest and mortality following vaccination with mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines in Hong Kong: A retrospective study",
"author": "Wong",
"doi-asserted-by": "crossref",
"journal-title": "PLoS Med",
"key": "10.1016/j.ekir.2024.02.009_bib23",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1056/NEJMp2113319",
"article-title": "Methods of Public Health Research — Strengthening Causal Inference from Observational Data",
"author": "Hernán",
"doi-asserted-by": "crossref",
"first-page": "1345",
"journal-title": "New England Journal of Medicine",
"key": "10.1016/j.ekir.2024.02.009_bib24",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1093/aje/kwv254",
"article-title": "Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available",
"author": "Hernán",
"doi-asserted-by": "crossref",
"first-page": "758",
"journal-title": "Am J Epidemiol",
"key": "10.1016/j.ekir.2024.02.009_bib25",
"volume": "183",
"year": "2016"
},
{
"key": "10.1016/j.ekir.2024.02.009_bib26",
"unstructured": "Fact Sheet for Health Care Providers Emergency Use Authorization (EUA) For Paxlovid. 2022;"
},
{
"DOI": "10.1002/sim.4780091214",
"article-title": "Relation of pooled logistic regression to time dependent Cox regression analysis: the Framingham Heart Study",
"author": "D’Agostino",
"doi-asserted-by": "crossref",
"first-page": "1501",
"journal-title": "Stat Med",
"key": "10.1016/j.ekir.2024.02.009_bib27",
"volume": "9",
"year": "1990"
},
{
"DOI": "10.1097/00001648-200009000-00012",
"article-title": "Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men",
"author": "Hernán",
"doi-asserted-by": "crossref",
"first-page": "561",
"journal-title": "Epidemiology",
"key": "10.1016/j.ekir.2024.02.009_bib28",
"volume": "11",
"year": "2000"
},
{
"DOI": "10.1056/EVIDoa2100044",
"article-title": "Randomized Trial of Molnupiravir or Placebo in Patients Hospitalized with Covid-19",
"author": "Arribas",
"doi-asserted-by": "crossref",
"journal-title": "NEJM Evidence",
"key": "10.1016/j.ekir.2024.02.009_bib29",
"volume": "1",
"year": "2022"
},
{
"article-title": "Evaluation of publication bias for 12 clinical trials of molnupiravir to treat SARS-CoV-2 infection in 13,694 patients",
"author": "Lawrence",
"journal-title": "Research Square",
"key": "10.1016/j.ekir.2024.02.009_bib30",
"year": "2022"
},
{
"article-title": "Oral antiviral therapies for COVID-19 in patients with advanced chronic kidney disease or kidney failure",
"author": "Cho",
"journal-title": "Nephrol Dial Transplant",
"key": "10.1016/j.ekir.2024.02.009_bib31",
"year": "2023"
},
{
"DOI": "10.1371/journal.pmed.1003321",
"article-title": "Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: A federated electronic medical record analysis",
"author": "Harrison",
"doi-asserted-by": "crossref",
"journal-title": "PLoS medicine",
"key": "10.1016/j.ekir.2024.02.009_bib32",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"journal-title": "The lancet",
"key": "10.1016/j.ekir.2024.02.009_bib33",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1966",
"article-title": "Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study",
"author": "Petrilli",
"doi-asserted-by": "crossref",
"first-page": "m1966",
"journal-title": "BMJ",
"key": "10.1016/j.ekir.2024.02.009_bib34",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa924",
"article-title": "Association Between Male Sex and Outcomes of Coronavirus Disease 2019 (COVID-19)-A Danish Nationwide, Register-based Study",
"author": "Kragholm",
"doi-asserted-by": "crossref",
"first-page": "e4025",
"journal-title": "Clin Infect Dis",
"key": "10.1016/j.ekir.2024.02.009_bib35",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1038/s41467-020-19741-6",
"article-title": "Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission",
"author": "Peckham",
"doi-asserted-by": "crossref",
"first-page": "6317",
"journal-title": "Nat Commun",
"key": "10.1016/j.ekir.2024.02.009_bib36",
"volume": "11",
"year": "2020"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2468024924000986"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nephrology"
],
"subtitle": [],
"title": "Effectiveness of molnupiravir and nirmatrelvir–ritonavir in CKD patients with COVID-19.",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}