Effectiveness of probiotics on COVID-19 prevention and treatment against mild COVID-19 in outpatient care: A systematic review
et al., Nutrition and Health, doi:10.1177/02601060251378200, PROSPERO CRD42024611230, Sep 2025
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Systematic review of 8 randomized controlled trials and 1 pre-post study examining probiotics for COVID-19 prevention and treatment in outpatients with mild symptoms, showing lower COVID-19 cases and improved recovery with treatment.
1.
Chau et al., Effectiveness of probiotics on COVID-19 prevention and treatment against mild COVID-19 in outpatient care: A systematic review, Nutrition and Health, doi:10.1177/02601060251378200.
2.
Bajić et al., Immunity's core reset: Synbiotics and gut microbiota in the COVID-19 era, Innate Immunity, doi:10.1177/17534259251362023.
3.
Bigman et al., A Comprehensive Scoping Review on Diet and Nutrition in Relation to Long COVID-19 Symptoms and Recovery, Nutrients, doi:10.3390/nu17111802.
4.
Fazli et al., Possible Link between Gut Microbiota, Diet, and COVID-19 Infection, Journal of Medical Bacteriology, 12:4, jmb.tums.ac.ir/index.php/jmb/article/view/525.
5.
Santa et al., Comparative analysis of COVID-19 responses in Japan and Africa: diet, phytochemicals, vitamin D, and gut microbiota in reducing mortality—A systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1465324.
6.
Kaushal, A., Nutraceuticals and pharmacological to balance the transitional microbiome to extend immunity during COVID-19 and other viral infections, Journal of Translational Medicine, doi:10.1186/s12967-024-05587-9.
7.
Mu et al., Anti-inflammatory and Nutritional Interventions Against SARS-CoV-2: A Comprehensive Review, Journal of Agriculture and Food Research, doi:10.1016/j.jafr.2024.101422.
8.
Taufer et al., Lactobacilli in COVID-19: A Systematic Review Based on Next-Generation Sequencing Studies, Microorganisms, doi:10.3390/microorganisms12020284.
9.
Righi et al., Gut Microbiome Disruption Following SARS-CoV-2: A Review, Microorganisms, doi:10.3390/microorganisms12010131.
10.
Petrariu et al., Role of probiotics in managing various human diseases, from oral pathology to cancer and gastrointestinal diseases, Frontiers in Microbiology, doi:10.3389/fmicb.2023.1296447.
11.
Taufer (B) et al., The Role of Bifidobacterium in COVID-19: A Systematic Review, Life, doi:10.3390/life13091847.
12.
Di Pierro, F., A possible probiotic (S. salivarius K12) approach to improve oral and lung microbiotas and raise defenses against SARS-CoV-2, Minerva Medica, doi:10.23736/S0026-4806.20.06570-2.
13.
Kurian et al., Probiotics in Prevention and Treatment of COVID-19: Current Perspective and Future Prospects, Archives of Medical Research, doi:10.1016/j.arcmed.2021.03.002.
14.
Singh et al., Probiotics: A potential immunomodulator in COVID-19 infection management, Nutrition Research, doi:10.1016/j.nutres.2020.12.014.
15.
Stavropoulou et al., Probiotics as a Weapon in the Fight Against COVID-19, Frontiers in Nutrition, doi:10.3389/fnut.2020.614986.
Chau et al., 26 Sep 2025, peer-reviewed, 3 authors, trial PROSPERO CRD42024611230.
Contact: chung.chau.23@ucl.ac.uk.
Effectiveness of probiotics on COVID-19 prevention and treatment against mild COVID-19 in outpatient care: A systematic review
Nutrition and Health, doi:10.1177/02601060251378200
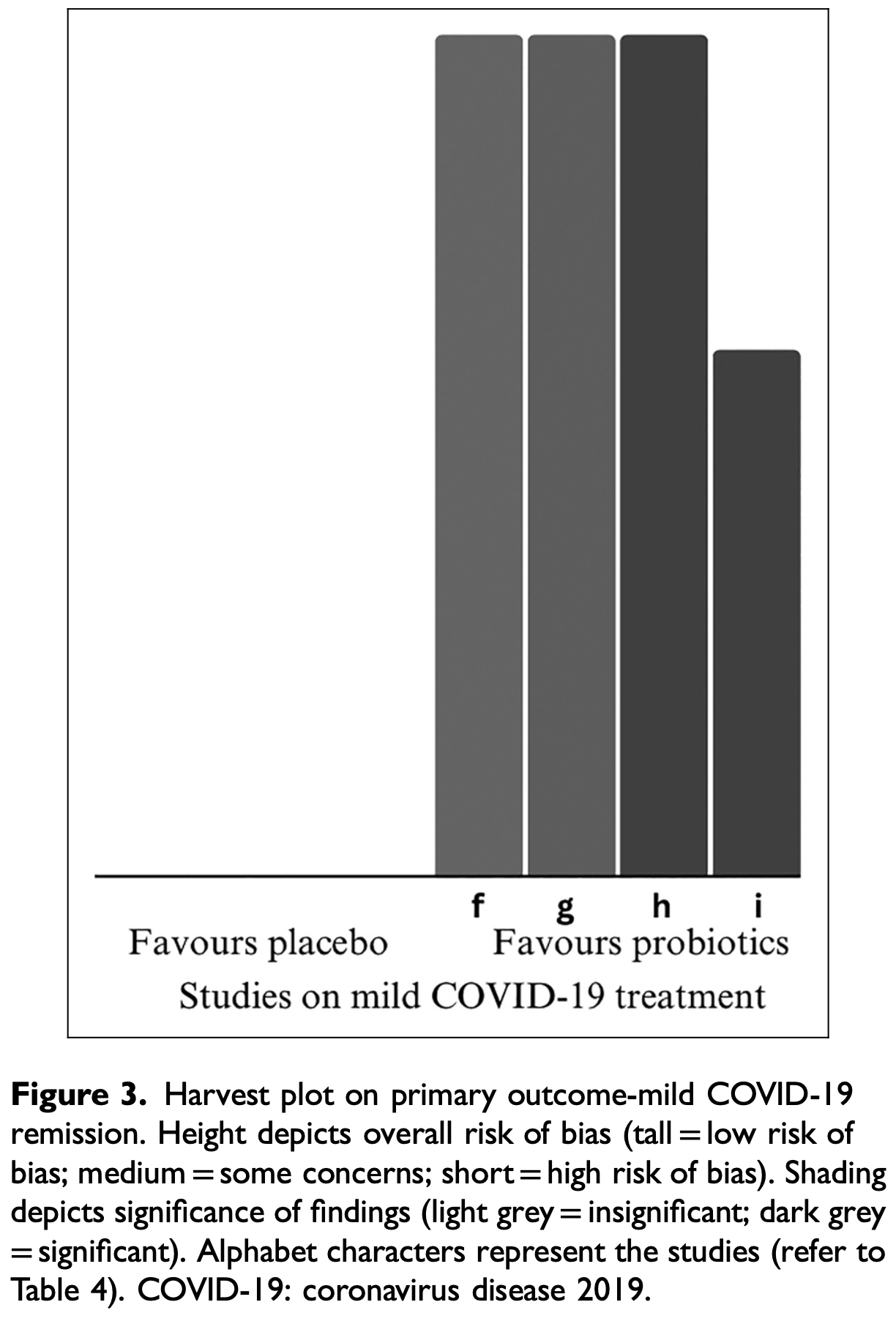
Background: In previous research, probiotics have shown to be beneficial in preventing and limiting the progress of upper respiratory infections. Their effectiveness in relation to coronavirus disease 2019 (COVID-19) has been investigated mainly in hospitalized patients, and less so among outpatients who constitute majority of COVID-19 cases. Aim: This systematic review evaluates the available evidence regarding the effectiveness of probiotic use on prevention and treatment of COVID-19 among patients with mild symptoms in outpatient settings. Methods: PubMed, Embase and Cochrane Library were searched for studies from their inception to May 2024, restricting to randomized controlled trials and before-and-after studies. The primary outcomes were infection incidence and complete remission rate. Cochrane risk-of-bias tool (RoB 2.0) and risk of bias in non-randomized studies of interventions tool (ROBINS-I) were used to assess the risk of bias. The Grading of Recommendations, Assessment, Development, and Evaluations approach was performed to assess the certainty of the evidence. Results: Eight randomized controlled trials and one pre-post study on 1235 participants were included. Four studies had low risk of bias. Probiotics were effective in reducing the incidence of COVID-19 upon exposure and accelerating the symptomatic remission of mild COVID-19 with less systemic symptoms. Overall, the certainty of evidence on both primary outcomes was moderate. Comorbidities and old ages were found to be significant confounders. Probiotics demonstrated significant immunomodulatory and humoral effects in the nasopharyngeal cavity. Conclusion: These results suggest that probiotics are effective at preventing COVID-19 and support faster recovery from mild COVID-19 among individuals seeking for outpatient care. People with comorbidities, that is, metabolic disorder and elderly benefit the most from probiotics supplements.
Declaration of conflicting interests The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical statement Ethical approval is not applicable to this article as no new data was collected.
Supplemental material Supplemental material for this article is available online.
References
Acosta-Navarro, Dias, De Gouveia, Vegetarian and plant-based diets associated with lower incidence of COVID-19, BMJ Nutrition, Prevention & Health
Ahanchian, Ranjbar, Reihani, Synbiotic for prevention of SARS-Cov2 infection in high risk hospital staffs: A randomized controlled trial, Open Journal of Nursing
Akatsu, Iwabuchi, Xiao, Clinical effects of probiotic Bifidobacterium longum BB536 on immune function and intestinal microbiota in elderly patients receiving enteral tube feeding, Journal of Parenteral and Enteral Nutrition
Berg, Nielsen, Nygaard, Long COVID symptoms in SARS-CoV-2-positive adolescents and matched controls (LongCOVIDKidsDK): A national, cross-sectional study, The Lancet Child & Adolescent Health
Bilin ́ski, Winter, ́ski, Rapid resolution of COVID-19 after faecal microbiota transplantation, Gut
Boeck, Cauwenberghs, Spacova, Randomized, double-blind, placebo-controlled trial of a throat spray with selected lactobacilli in COVID-19 outpatients, Microbiology Spectrum
Butler, Dorward, Yu, Azithromycin for community treatment of suspected COVID-19 in people at increased risk of an adverse clinical course in the UK (PRINCIPLE): A randomised, controlled, open-label, adaptive platform trial, The Lancet
Ceccarelli, Borrazzo, Pinacchio, Oral bacteriotherapy in patients with COVID-19: A retrospective cohort study, Frontiers in Nutrition
Chen, Liang, Liang, Probiotics: Functional food ingredients with the potential to reduce hypertension Frontiers in Cellular and Infection, Microbiology
Daneshkhah, Agrawal, Eshein, Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clinical and Experimental Research
Dang, Marsland, Microbes, metabolites, and the gut-lung axis, Mucosal Immunology
Das, Heredia, De, Pereira, Korean traditional foods as antiviral and respiratory disease prevention and treatments: A detailed review, Trends in Food Science & Technology
Davis, Assaf, Mccorkell, Characterizing long COVID in an international cohort: 7 months of symptoms and their impact, EClinicalMedicine
Dennis, Wamil, Alberts, Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: A prospective, community-based study, BMJ Open
Dugas, Grote-Westrick, Vollenberg, Less severe course of COVID-19 is associated with elevated levels of antibodies against seasonal human coronaviruses OC43 and HKU1 (HCoV OC43, HCoV HKU1), IJID
El-Warrak, Nunes, Luna, Towards the future of public health: Roadmapping trends and scenarios in the post-COVID healthcare era, Healthcare
Enaud, Prevel, Ciarlo, The gut-lung axis in health and respiratory diseases: A place for inter-organ and interkingdom crosstalks Frontiers in Cellular and Infection, Microbiology
Endam, Alromaih, Gonzalez, Intranasal application of Lactococcus lactis W136 is safe in chronic rhinosinusitis patients with previous sinus surgery, Frontiers in Cellular and Infection Microbiology
Fanos, Pintus, Pintus, Lung microbiota in the acute respiratory disease: From coronavirus to metabolomics, JPNIM
Forsgård, Rode, Lobenius-Palmér, Limosilactobacillus reuteri DSM 17938 supplementation and SARS-CoV-2 specific antibody response in healthy adults: A randomized, triple-blinded, placebo-controlled trial, Gut Microbes
Gohil, Samson, Dastager, Probiotics in the prophylaxis of COVID-19: Something is better than nothing, 3 Biotech
Gou, Fu, Yue, Gut microbiota, inflammation, and molecular signatures of host response to infection, JGG
Grand, Research, Probiotics market size, share & trends analysis report by product (food & beverages, dietary supplements), by ingredient (bacteria, yeast), by distribution channel, by end-use, by region, and segment forecasts
Gutiérrez-Castrellón, Gandara-Martí, Abreu, Probiotic improves symptomatic and viral clearance in Covid19 outpatients: A randomized, quadruple-blinded, placebo-controlled trial, Gut Microbes
Higgins, Thomas, Chandler, Cochrane Handbook for Systematic Reviews of Interventions
Infusino, Marazzato, Mancone, Diet supplementation, probiotics, and nutraceuticals in SARS-CoV-2 infection: A scoping review, Nutrients
Jeon, Kim, Kim, Effects of yogurt containing probiotics on respiratory virus infections: Influenza H1N1 and SARS-CoV-2, Journal of Dairy Science
Jiang, Hou, Tang, A phase trial of the oral Lactobacillus casei vaccine polarizes Th2 cell immunity against transmissible gastroenteritis coronavirus infection, Applied Microbiology and Biotechnology
Jones, Martoni, Prakash, Oral supplementation with probiotic L. reuteri NCIMB 30242 increases mean circulating 25-hydroxyvitamin D: A post hoc analysis of a randomized controlled trial, The Journal of Clinical Endocrinology & Metabolism
Kageyama, Nishizaki, Aida, Lactobacillus plantarum induces innate cytokine responses that potentially provide a protective benefit against COVID-19: A single-arm, double-blind, prospective trial combined with an in vitro cytokine response assay, Experimental and Therapeutic Medicine
King, Glanville, Sanders, Effectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: A systematic review and meta-analysis, British Journal of Nutrition
Kolesnyk, Paliy, Sydorchuk, The role of nutritional support with probiotics in outpatients with symptomatic acute respiratory tract infections: A multicenter, randomized, double-blind, placebo-controlled dietary study, BMC Nutrition
Kurian, Unnikrishnan, Miraj, Probiotics in prevention and treatment of COVID-19: Current perspective and future prospects, AMS
Lau, Su, Lau, A synbiotic preparation (SIM01) for post-acute COVID-19 syndrome in Hong Kong (RECOVERY): A randomised, double-blind, placebo-controlled trial, The Lancet Infectious Diseases
Lee, Lin, Lei, Does vitamin D deficiency affect the immunogenic responses to influenza vaccination? A systematic review and meta-analysis, Nutrients
Ley, Turnbaugh, Klein, Human gut microbes associated with obesity, Nature
Li, Cheng, Xu, The role of probiotics in coronavirus disease-19 infection in Wuhan: A retrospective study of 311 severe patients, International Immunopharmacology
Li, Hilgenfeld, Whitley, Therapeutic strategies for COVID-19: Progress and lessons learned, Nature Reviews Drug Discovery
Mckee, Britton, Black, Methods in health services research. Interpreting the evidence: Choosing between randomised and non-randomised studies, Bmj
Morais, Passos, Maciel, Can probiotics and diet promote beneficial immune modulation and purine control in coronavirus infection?, Nutrients
Mozota, Castro, Gómez-Torres, Administration of Ligilactobacillus salivarius MP101 in an elderly nursing home during the COVID-19 pandemic: Immunological and nutritional impact Foods
Murad, Mustafa, Schünemann, Rating the certainty in evidence in the absence of a single estimate of effect, Evidence Based Medicine
Nguyen, Chong, Hor, Role of probiotics in the management of COVID-19: A computational perspective, Nutrients
Park, Gonsalves, Tan, Comparing frequency of booster vaccination to prevent severe COVID-19 by risk group in the United States, Nature Communications
Pierro, Iqtadar, Mumtaz, Clinical effects of Streptococcus salivarius K12 in hospitalized COVID-19 patients: Results of a preliminary study, Microorganisms
Prashar, Long Covid: Conceptualizing the challenges for public health, Journal of Public Health
Rajput, Paliwal, Naithani, COVID-19 and gut microbiota: A potential connection, Indian Journal of Clinical Biochemistry
Rodriguez-Blanque, Sánchez-García, Vargas, Evaluation of the effect of Loigolactobacillus coryniformis K8 CECT 5711 consumption in health care workers exposed to COVID-19, Frontiers in Nutrition
Roessler, Tesch, Batram, Post-COVID-19-associated morbidity in children, adolescents, and adults: A matched cohort study including more than 157,000 individuals with COVID-19 in Germany, PLoS Medicine
Sankova, Kytko, Dydykina, Fermented milk and probiotic foods are an important part of population diet during SARS-CoV-2 pandemic, Voprosy Pitaniya
Seethaler, Nguyen, Basrai, Short-chain fatty acids are key mediators of the favorable effects of the Mediterranean diet on intestinal barrier integrity: Data from the randomized controlled LIBRE trial, AJCN
Sengupta, Brooks, Grant, Accounting for time: Circadian rhythms in the time of COVID-19, Journal of Biological Rhythms
Sheikh Mohamed, Isho, Chao, Systemic and mucosal IgA responses are variably induced in response to SARS-CoV-2 mRNA vaccination and are associated with protection against subsequent infection, Mucosal Immunology
Shimizu, Yamada, Ogura, Synbiotics modulate gut microbiota and reduce enteritis and ventilator-associated pneumonia in patients with sepsis: A randomized controlled trial, Critical Care
Sugimura, Takahashi, Jounai, Effects of oral intake of plasmacytoid dendritic cells-stimulative lactic acid bacterial strain on pathogenesis of influenza-like illness and immunological response to influenza virus, British Journal of Nutrition
Tao, Gu, Mao, Effects of probiotics on type II diabetes mellitus: A meta-analysis, Journal of Translational Medicine
Tian, Ran, Wen, Probiotics improve symptoms of patients with COVID-19 through gut-lung axis: A systematic review and meta-analysis, Frontiers in Nutrition
Wang, Lin, Xiang, Oropharyngeal probiotic ENT-K12 prevents respiratory tract infections among frontline medical staff fighting against COVID-19: A pilot study, Frontiers in Bioengineering and Biotechnology
Who, int/dashboards
Wischmeyer, Tang, Ren, Efficacy of probiotic treatment as post-exposure prophylaxis for COVID-19: A double-blind, placebo-controlled randomized trial, Clinical Nutrition
Wu, Huang, Liu, Clinical efficacy of probiotics in the treatment of patients with COVID-19: A systematic review and meta-analysis of randomized controlled trials, Expert Review of Anti-Infective Therapy
Xu, Cai, Shen, Management of COVID-19: The Zhejiang experience. Zhejiang da Xue Xue Bao, Yi Xue Ban
Yang, Chakraborty, Saha, Gnotobiotic rats reveal that gut microbiota regulates colonic mRNA of ACE2, the receptor for SARS-CoV-2 infectivity, Hypertension
Zhao, Dong, Hao, Probiotics for preventing acute upper respiratory tract infections, Cochrane Database of Systematic Reviews
Zhu, Pitre, Ching, Safety and efficacy of probiotic supplements as adjunctive therapies in patients with COVID-19: A systematic review and meta-analysis, PLoS One
DOI record:
{
"DOI": "10.1177/02601060251378200",
"ISSN": [
"0260-1060",
"2047-945X"
],
"URL": "http://dx.doi.org/10.1177/02601060251378200",
"abstract": "<jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>In previous research, probiotics have shown to be beneficial in preventing and limiting the progress of upper respiratory infections. Their effectiveness in relation to coronavirus disease 2019 (COVID-19) has been investigated mainly in hospitalized patients, and less so among outpatients who constitute majority of COVID-19 cases.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Aim</jats:title>\n <jats:p>This systematic review evaluates the available evidence regarding the effectiveness of probiotic use on prevention and treatment of COVID-19 among patients with mild symptoms in outpatient settings.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>PubMed, Embase and Cochrane Library were searched for studies from their inception to May 2024, restricting to randomized controlled trials and before-and-after studies. The primary outcomes were infection incidence and complete remission rate. Cochrane risk-of-bias tool (RoB 2.0) and risk of bias in non-randomized studies of interventions tool (ROBINS-I) were used to assess the risk of bias. The Grading of Recommendations, Assessment, Development, and Evaluations approach was performed to assess the certainty of the evidence.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Eight randomized controlled trials and one pre-post study on 1235 participants were included. Four studies had low risk of bias. Probiotics were effective in reducing the incidence of COVID-19 upon exposure and accelerating the symptomatic remission of mild COVID-19 with less systemic symptoms. Overall, the certainty of evidence on both primary outcomes was moderate. Comorbidities and old ages were found to be significant confounders. Probiotics demonstrated significant immunomodulatory and humoral effects in the nasopharyngeal cavity.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>These results suggest that probiotics are effective at preventing COVID-19 and support faster recovery from mild COVID-19 among individuals seeking for outpatient care. People with comorbidities, that is, metabolic disorder and elderly benefit the most from probiotics supplements.</jats:p>\n </jats:sec>",
"alternative-id": [
"10.1177/02601060251378200"
],
"article-number": "02601060251378200",
"author": [
{
"ORCID": "https://orcid.org/0009-0006-7440-9089",
"affiliation": [
{
"name": "Institute of Epidemiology and Health Care, University College London, London, UK"
}
],
"authenticated-orcid": false,
"family": "Chau",
"given": "Chung Hang Hannah",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0002-4482-148X",
"affiliation": [
{
"name": "Institute of Epidemiology and Health Care, University College London, London, UK"
}
],
"authenticated-orcid": false,
"family": "Stefler",
"given": "Denes",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0009-0000-3928-9807",
"affiliation": [
{
"name": "Nuffield Department of Population Health, University of Oxford, Oxford, UK"
}
],
"authenticated-orcid": false,
"family": "Szeto",
"given": "Michelle Man Sum",
"sequence": "additional"
}
],
"container-title": "Nutrition and Health",
"container-title-short": "Nutr Health",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.sagepub.com"
]
},
"created": {
"date-parts": [
[
2025,
9,
26
]
],
"date-time": "2025-09-26T16:52:22Z",
"timestamp": 1758905542000
},
"deposited": {
"date-parts": [
[
2025,
9,
29
]
],
"date-time": "2025-09-29T13:48:00Z",
"timestamp": 1759153680000
},
"indexed": {
"date-parts": [
[
2025,
9,
29
]
],
"date-time": "2025-09-29T14:10:12Z",
"timestamp": 1759155012372,
"version": "3.44.0"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
9,
26
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
9,
26
]
],
"date-time": "2025-09-26T00:00:00Z",
"timestamp": 1758844800000
}
},
{
"URL": "https://journals.sagepub.com/page/policies/text-and-data-mining-license",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
9,
26
]
],
"date-time": "2025-09-26T00:00:00Z",
"timestamp": 1758844800000
}
}
],
"link": [
{
"URL": "https://journals.sagepub.com/doi/pdf/10.1177/02601060251378200",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://journals.sagepub.com/doi/full-xml/10.1177/02601060251378200",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://journals.sagepub.com/doi/pdf/10.1177/02601060251378200",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "179",
"original-title": [],
"prefix": "10.1177",
"published": {
"date-parts": [
[
2025,
9,
26
]
]
},
"published-online": {
"date-parts": [
[
2025,
9,
26
]
]
},
"publisher": "SAGE Publications",
"reference": [
{
"DOI": "10.1136/bmjnph-2023-000629",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_2_1"
},
{
"DOI": "10.4236/ojn.2021.115025",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_3_1"
},
{
"DOI": "10.1177/0148607112467819",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_4_1"
},
{
"DOI": "10.1136/gutjnl-2021-325010",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_5_1"
},
{
"DOI": "10.1016/S0140-6736(21)00461-X",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_6_1"
},
{
"DOI": "10.3389/fnut.2020.613928",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_7_1"
},
{
"DOI": "10.3389/fcimb.2023.1220877",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_8_1"
},
{
"DOI": "10.1007/s40520-020-01677-y",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_9_1"
},
{
"DOI": "10.1038/s41385-019-0160-6",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_10_1"
},
{
"DOI": "10.1016/j.tifs.2021.07.037",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_11_1"
},
{
"DOI": "10.1016/j.eclinm.2021.101019",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_12_1"
},
{
"DOI": "10.1128/spectrum.01682-22",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_13_1"
},
{
"DOI": "10.1136/bmjopen-2020-048391",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_14_1"
},
{
"DOI": "10.3390/microorganisms10101926",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_15_1"
},
{
"article-title": "Less severe course of COVID-19 is associated with elevated levels of antibodies against seasonal human coronaviruses OC43 and HKU1 (HCoV OC43, HCoV HKU1)",
"author": "Dugas M",
"first-page": "304",
"journal-title": "IJID",
"key": "e_1_3_3_16_1",
"unstructured": "Dugas M, Grote-Westrick T, Vollenberg R, et al. (2021) Less severe course of COVID-19 is associated with elevated levels of antibodies against seasonal human coronaviruses OC43 and HKU1 (HCoV OC43, HCoV HKU1). IJID 105: 304–306.",
"volume": "105",
"year": "2021"
},
{
"DOI": "10.3390/healthcare11243118",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_17_1"
},
{
"DOI": "10.3389/fcimb.2020.00009",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_18_1"
},
{
"DOI": "10.3389/fcimb.2020.00440",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_19_1"
},
{
"article-title": "Lung microbiota in the acute respiratory disease: From coronavirus to metabolomics",
"author": "Fanos V",
"issue": "1",
"journal-title": "JPNIM",
"key": "e_1_3_3_20_1",
"unstructured": "Fanos V, Pintus MC, Pintus R, et al. (2020) Lung microbiota in the acute respiratory disease: From coronavirus to metabolomics. JPNIM 9(1): e090139.",
"volume": "9",
"year": "2020"
},
{
"key": "e_1_3_3_21_1",
"unstructured": "Food and Agriculture Organization. (2001) Health and nutritional properties of probiotics in food including powder milk with live lactic acid bacteria. Available at: https://www.iqb.es/digestivo/pdfs/probioticos.pdf (accessed 14 July 2024)."
},
{
"DOI": "10.1080/19490976.2023.2229938",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_22_1"
},
{
"DOI": "10.1007/s13205-020-02554-1",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_23_1"
},
{
"article-title": "Gut microbiota, inflammation, and molecular signatures of host response to infection",
"author": "Gou W",
"first-page": "792",
"issue": "9",
"journal-title": "JGG",
"key": "e_1_3_3_24_1",
"unstructured": "Gou W, Fu Y, Yue L, et al. (2021) Gut microbiota, inflammation, and molecular signatures of host response to infection. JGG 48(9): 792–802.",
"volume": "48",
"year": "2021"
},
{
"key": "e_1_3_3_25_1",
"unstructured": "Grand view research. (2023) Probiotics market size share & trends analysis report by product (food & beverages dietary supplements) by ingredient (bacteria yeast) by distribution channel by end-use by region and segment forecasts 2023–2030. Available at: https://www.grandviewresearch.com/industry-analysis/probiotics-market (accessed 14 July 2024)."
},
{
"DOI": "10.1080/19490976.2021.2018899",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_26_1"
},
{
"DOI": "10.1002/9781119536604",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_27_1"
},
{
"DOI": "10.3390/nu12061718",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_28_1"
},
{
"DOI": "10.3168/jds.2022-22198",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_29_1"
},
{
"DOI": "10.1007/s00253-016-7424-9",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_30_1"
},
{
"DOI": "10.1210/jc.2012-4262",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_31_1"
},
{
"DOI": "10.3892/etm.2021.10942",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_32_1"
},
{
"DOI": "10.1016/S2352-4642(22)00004-9",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_33_1"
},
{
"DOI": "10.1017/S0007114514000075",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_34_1"
},
{
"DOI": "10.1186/s40795-023-00816-8",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_35_1"
},
{
"article-title": "Probiotics in prevention and treatment of COVID-19: Current perspective and future prospects",
"author": "Kurian SJ",
"first-page": "582",
"issue": "6",
"journal-title": "AMS",
"key": "e_1_3_3_36_1",
"unstructured": "Kurian SJ, Unnikrishnan MK, Miraj SS, et al. (2021) Probiotics in prevention and treatment of COVID-19: Current perspective and future prospects. AMS 52(6): 582–594.",
"volume": "52",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(23)00685-0",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_37_1"
},
{
"DOI": "10.3390/nu10040409",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_38_1"
},
{
"DOI": "10.1038/4441022a",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_39_1"
},
{
"DOI": "10.1038/s41573-023-00672-y",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_40_1"
},
{
"DOI": "10.1016/j.intimp.2021.107531",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_41_1"
},
{
"DOI": "10.1136/bmj.319.7205.312",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_42_1"
},
{
"DOI": "10.3390/nu12061737",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_43_1"
},
{
"article-title": "Administration of Ligilactobacillus salivarius MP101 in an elderly nursing home during the COVID-19 pandemic: Immunological and nutritional impact",
"author": "Mozota M",
"first-page": "2149",
"issue": "9",
"journal-title": "Foods (Basel, Switzerland)",
"key": "e_1_3_3_44_1",
"unstructured": "Mozota M, Castro I, Gómez-Torres N, et al. (2021) Administration of Ligilactobacillus salivarius MP101 in an elderly nursing home during the COVID-19 pandemic: Immunological and nutritional impact Foods (Basel, Switzerland) 10(9): 2149",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1136/ebmed-2017-110668",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_45_1"
},
{
"DOI": "10.3390/nu14020274",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_46_1"
},
{
"DOI": "10.1038/s41467-024-45549-9",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_47_1"
},
{
"DOI": "10.1093/pubmed/fdac153",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_48_1"
},
{
"DOI": "10.1007/s12291-020-00948-9",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_49_1"
},
{
"DOI": "10.3389/fnut.2022.962566",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_50_1"
},
{
"DOI": "10.1371/journal.pmed.1004122",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_51_1"
},
{
"article-title": "Fermented milk and probiotic foods are an important part of population diet during SARS-CoV-2 pandemic",
"author": "Sankova MV",
"first-page": "86",
"issue": "1",
"journal-title": "Voprosy Pitaniya",
"key": "e_1_3_3_52_1",
"unstructured": "Sankova MV, Kytko OV, Dydykina IS, et al. (2022) Fermented milk and probiotic foods are an important part of population diet during SARS-CoV-2 pandemic. Voprosy Pitaniya 91(1): 86–97.",
"volume": "91",
"year": "2022"
},
{
"article-title": "Short-chain fatty acids are key mediators of the favorable effects of the Mediterranean diet on intestinal barrier integrity: Data from the randomized controlled LIBRE trial",
"author": "Seethaler B",
"first-page": "928",
"issue": "4",
"journal-title": "AJCN",
"key": "e_1_3_3_53_1",
"unstructured": "Seethaler B, Nguyen NK, Basrai M, et al. (2022) Short-chain fatty acids are key mediators of the favorable effects of the Mediterranean diet on intestinal barrier integrity: Data from the randomized controlled LIBRE trial. AJCN 116(4): 928–942.",
"volume": "116",
"year": "2022"
},
{
"DOI": "10.1177/0748730420953335",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_54_1"
},
{
"DOI": "10.1038/s41385-022-00511-0",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_55_1"
},
{
"DOI": "10.1186/s13054-018-2167-x",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_56_1"
},
{
"DOI": "10.1017/S0007114515002408",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_57_1"
},
{
"DOI": "10.1186/s12967-020-02213-2",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_58_1"
},
{
"DOI": "10.3389/fnut.2023.1179432",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_59_1"
},
{
"DOI": "10.3389/fbioe.2021.646184",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_60_1"
},
{
"DOI": "10.1016/j.clnu.2023.11.043",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_61_1"
},
{
"key": "e_1_3_3_62_1",
"unstructured": "World Health Organization. (2023) Clinical management of COVID-19: Living guideline. Available at: https://app.magicapp.org/#/guideline/j1WBYn (accessed 20 July 2024)."
},
{
"key": "e_1_3_3_63_1",
"unstructured": "World Health Organization. (2024a) COVID-19 vaccination world data. Available at: https://data.who.int/dashboards/covid19/vaccines (accessed 14 July 2024)."
},
{
"key": "e_1_3_3_64_1",
"unstructured": "World Health Organization. (2024b) Number of COVID-19 cases reported to WHO (cumulative total). Available at: https://data.who.int/dashboards/covid19/cases?n=o (accessed 14 July 2024)."
},
{
"key": "e_1_3_3_65_1",
"unstructured": "World Health Organization. (2024c) Number of COVID-19 deaths reported to WHO (cumulative total). Available at: https://data.who.int/dashboards/covid19/deaths?n=o (accessed 14 July 2024)."
},
{
"DOI": "10.1080/14787210.2023.2189100",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_66_1"
},
{
"article-title": "Management of COVID-19: The Zhejiang experience",
"author": "Xu K",
"first-page": "147",
"issue": "2",
"journal-title": "Zhejiang da Xue Xue Bao. Yi Xue Ban",
"key": "e_1_3_3_67_1",
"unstructured": "Xu K, Cai H, Shen Y, et al. (2020) Management of COVID-19: The Zhejiang experience. Zhejiang da Xue Xue Bao. Yi Xue Ban 49(2): 147–157.",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.120.15360",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_68_1"
},
{
"article-title": "Probiotics for preventing acute upper respiratory tract infections",
"author": "Zhao Y",
"issue": "8",
"journal-title": "Cochrane Database of Systematic Reviews",
"key": "e_1_3_3_69_1",
"unstructured": "Zhao Y, Dong BR, Hao Q (2022) Probiotics for preventing acute upper respiratory tract infections. Cochrane Database of Systematic Reviews 8(8): Cd006895.",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0278356",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_70_1"
}
],
"reference-count": 69,
"references-count": 69,
"relation": {},
"resource": {
"primary": {
"URL": "https://journals.sagepub.com/doi/10.1177/02601060251378200"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Effectiveness of probiotics on COVID-19 prevention and treatment against mild COVID-19 in outpatient care: A systematic review",
"type": "journal-article",
"update-policy": "https://doi.org/10.1177/sage-journals-update-policy"
}
