Does the Level of Vitamin D in COVID-19 Patients Affect the Survival and Duration of Hospital Stay?
et al., Clinical Science of Nutrition, doi:10.5152/ClinSciNutr.2023.22059, Mar 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 168 hospitalized COVID-19 patients, showing no significant association between vitamin D levels and mortality. Adjusted results are only provided for vitamin D as a continuous variable.
This is the 169th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 50.9% lower, RR 0.49, p = 0.07, high D levels (≥20ng/mL) 7 of 61 (11.5%), low D levels (<20ng/mL) 25 of 107 (23.4%), NNT 8.4.
|
|
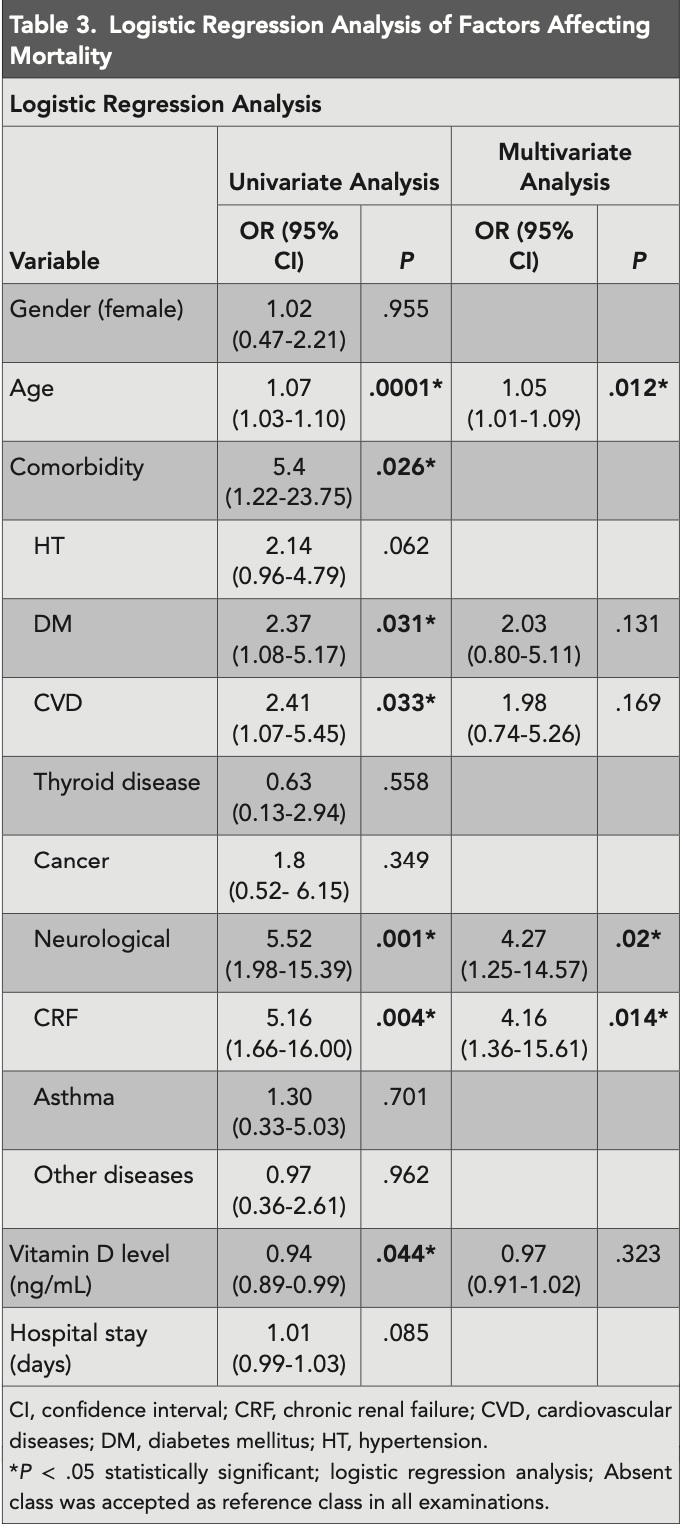
risk of death, 3.0% lower, OR 0.97, p = 0.32, adjusted per study, continuous values, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Cetin Ozbek et al., 24 Mar 2023, retrospective, Turkey, peer-reviewed, mean age 63.4, 6 authors, study period 1 August, 2021 - 31 October, 2021.
Contact: sevancetin@yiu.edu.tr.
Does the Level of Vitamin D in COVID-19 Patients Affect the Survival and Duration of Hospital Stay?
Clinical Science of Nutrition, doi:10.5152/clinscinutr.2023.22059
Objective: This study aimed to evaluate the effect of categorized and normal vitamin D levels on hospital stay and mortality in adult patients with COVID-19. Methods: One hundred sixty-eight hospitalized patients due to coronavirus disease 2019 were retrospectively evaluated. The study data were collected from medical records (age, gender, comorbidity, vitamin D level, duration of hospital stay, mortality/ survival status). Serum 25(OH) vitamin D level ≥ 30 ng/mL is defined as normal, 20-29 ng/mL is an insufficiency level, and less than 20 ng/mL is defined as a deficiency level.
Results: The mean vitamin D level of 168 patients was 18.72 ± 11.18 ng/mL, and 79.4% of patients with vitamin D deficiency had comorbidity. When vitamin D levels were categorized, there was no difference between the groups regarding hospital stay and survival (P > .05). However, when the mean vitamin D levels between the deceased and surviving patients were assessed, vitamin D levels were significantly higher in the survivors (P = .019). Vitamin D significantly affected survival compared to the univariate model (P = .044), while there was no significant effect on the multivariate model (P > .05). Even when the factors affecting the vitamin D level were adjusted, no significant results were found. Conclusion: Among hospitalized COVID-19 patients, vitamin D levels did not support an association between the duration of hospital stay and mortality.
References
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J Infect Public Health, doi:10.1016/j.jiph.2020.06.021
Alkhafaji, Argan, Albaker, The impact of vitamin D level on the severity and outcome of hospitalized patients with COVID-19 disease, Int J Gen Med, doi:10.2147/IJGM.S346169
Alpdemir, Alpdemir, Vitamin D deficiency status in Turkey: a meta-analysis, Int J Biochem
Amrein, Scherkl, Hoffmann, Vitamin D deficiency 2.0: an update on the current status worldwide, Eur J Clin Nutr, doi:10.1038/s41430-020-0558-y
Antos, Kwong, Balmorez, Villanueva, Murakami, Unusually high risks of COVID-19 mortality with age-related comorbidities: an adjusted meta-analysis method to improve the risk assessment of mortality using the comorbid mortality data, Infect Dis Rep, doi:10.3390/idr13030065
Brenner, Vitamin D supplementation to prevent COVID-19 infections and deaths-accumulating evidence from epidemiological and intervention studies calls for immediate action, Nutrients, doi:10.3390/nu13020411
Campi, Gennari, Merlotti, Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy, BMC Infect Dis, doi:10.1186/s12879-021-06281-7
Chen, Mei, Xie, Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: a meta-analysis and GRADE assessment of cohort studies and RCTs, Nutr J, doi:10.1186/s12937-021-00744-y
Crf, chronic renal failure; CVD, cardiovascular diseases; DM, diabetes mellitus
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, J Med Virol, doi:10.1002/jmv.26832
Grant, Holick, Benefits and requirements of vitamin D for optimal health: a review, Altern Med Rev
Grant, Lahore, Mcdonnell, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Holick, The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention, Rev Endocr Metab Disord, doi:10.1007/s11154-017-9424-1
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID 19 patients and its correlation with inflammatory markers, Sci Rep, doi:10.1038/s41598-020-77093-z
Karahan, Katkat, Impact of serum 25(OH) vitamin D level on mortality in patients with COVID-19 in Turkey, J Nutr Health Aging, doi:10.1007/s12603-020-1479-0
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One
Lanham-New, Webb, Cashman, Vitamin D and SARS-CoV-2 virus/COVID-19 disease, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000089
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Mitchell, Vitamin-D and COVID-19: do deficient risk a poorer outcome?, Lancet Diabetes Endocrinol
Muscogiuri, Vitamin D: past, present and future perspectives in the prevention of chronic diseases, Eur J Clin Nutr, doi:10.1038/s41430-018-0261-4
Nasiri, Khodadadi, Molaei, Does vitamin D serum level affect prognosis of COVID-19 patients?, Int J Infect Dis, doi:10.1016/j.ijid.2021.04.083
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID 19: a systematic review and meta-analysis, J Endocrinol Invest, doi:10.1007/s40618-021-01614-4
Pecina, Merry, Park, Td, Vitamin D status and severe COVID-19 disease outcomes in hospitalized patients, J Prim Care Community Health, doi:10.1177/21501327211041206
Pilz, Zittermann, Trummer, Vitamin D testing and treatment: a narrative review of current evidence, Endocr Connect, doi:10.1530/EC-18-0432
Rashedi, Poor, Asgharzadeh, Risk factors for COVID-19, Infez Med
Reis, Fernandes, Sales, Influence of vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: a multicenter prospective cohort study, Am J Clin Nutr, doi:10.1093/ajcn/nqab151
Sanyaolu, Okorie, Marinkovic, Comorbidity and its impact on patients with COVID-19, SN Compr Clin Med, doi:10.1007/s42399-020-00363-4
Serdar, Can, Kilercik, Analysis of changes in parathyroid hormone and 25 (OH) vitamin D levels with respect to age, gender and season: a data mining study, J Med Biochem, doi:10.1515/jomb-2017-0002
Siddiqui, Manansala, Abdulrahman, Immune modulatory effects of vitamin D on viral infections, Nutrients, doi:10.3390/nu12092879
Silva, Furlanetto, Does serum 25-hydroxyvitamin D decrease during acute-phase response? A systematic review, Nutr Res, doi:10.1016/j.nutres.2014.12.008
Szeto, Zucker, Lasota, Vitamin D status and COVID-19 clinical outcomes in hospitalized patients, Endocr Res, doi:10.1080/07435800.2020.1867162
Taha, Abureesh, Alghamdi, The relationship between vitamin D and infections including COVID-19: any hopes?, Int J Gen Med, doi:10.2147/IJGM.S317421
Teshome, Adane, Girma, Mekonnen, The impact of vitamin D level on COVID-19 infection: systematic review and meta-analysis, Front Public Health
Teymoori-Rad, Marashi, Vitamin D and Covid-19: from potential therapeutic effects to unanswered questions, Rev Med Virol, doi:10.1002/rmv.2159
Tsiaras, Weinstock, Factors influencing vitamin D status, Acta Derm Venereol, doi:10.2340/00015555-0980
Wang, Li, Vitamin D and chronic diseases, Aging Dis, doi:10.14336/AD.2016.1021
Yeşiltepe-Mutlu, Aksu, Bereket, Hatun, Vitamin D status across age groups in Turkey: results of 108,742 samples from a single laboratory, J Clin Res Pediatr Endocrinol, doi:10.4274/jcrpe.galenos.2019.2019.0097
DOI record:
{
"DOI": "10.5152/clinscinutr.2023.22059",
"URL": "http://dx.doi.org/10.5152/ClinSciNutr.2023.22059",
"author": [
{
"affiliation": [],
"family": "Cetin Ozbek",
"given": "Sevan",
"sequence": "first"
},
{
"affiliation": [],
"name": "Nutrition and Dietetics, Yuksek Ihtisas University, Faculty of Health Sciences, Ankara, Turkey",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ozsoy",
"given": "Selen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ozturk",
"given": "Levent",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Department of Clinical Nutrition Units, Ankara City Hospital, Ankara, Turkey",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Department of Anesthesiology and Reanimation, Ankara Yildirim Beyazit University, Faculty of Medicine, Ankara, Turkey",
"sequence": "additional"
}
],
"container-title": "Clinical Science of Nutrition",
"container-title-short": "Clin Sci Nutr",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
30
]
],
"date-time": "2023-03-30T11:53:18Z",
"timestamp": 1680177198000
},
"deposited": {
"date-parts": [
[
2023,
3,
30
]
],
"date-time": "2023-03-30T11:53:22Z",
"timestamp": 1680177202000
},
"indexed": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T05:10:29Z",
"timestamp": 1680239429118
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
3,
30
]
]
},
"member": "3111",
"original-title": [],
"prefix": "10.5152",
"published": {
"date-parts": [
[
2023,
3,
30
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
30
]
]
},
"publisher": "AVES YAYINCILIK A.Ş.",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://clinscinutr.org/en/does-the-level-of-vitamin-d-in-covid-19-patients-affect-the-survival-and-duration-of-hospital-stay-135773"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Geometry and Topology",
"Religious studies",
"General Business, Management and Accounting",
"General Business, Management and Accounting",
"History and Philosophy of Science",
"Literature and Literary Theory",
"Linguistics and Language",
"History",
"Language and Linguistics",
"Cultural Studies",
"Tourism, Leisure and Hospitality Management",
"Geography, Planning and Development",
"Tourism, Leisure and Hospitality Management",
"Tourism, Leisure and Hospitality Management",
"Tourism, Leisure and Hospitality Management",
"Geography, Planning and Development",
"Tourism, Leisure and Hospitality Management",
"Business and International Management"
],
"subtitle": [],
"title": "Does the Level of Vitamin D in COVID-19 Patients Affect the Survival and Duration of Hospital Stay?",
"type": "journal-article"
}
