Vitamin D Status and Severe COVID-19 Disease Outcomes in Hospitalized Patients
et al., Journal of Primary Care & Community Health, doi:10.1177/21501327211041206
, Aug 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 92 hospitalized patients not showing significant differences in outcomes based on vitamin D status or supplementation.
This is the 49th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 70.0% higher, OR 1.70, p = 0.52, treatment 29, control 63, supplementation, unadjusted, RR approximated with OR, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
risk of mechanical ventilation, 10.0% higher, OR 1.10, p = 0.89, treatment 29, control 63, supplementation, unadjusted, RR approximated with OR, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
risk of ICU admission, 30.0% higher, OR 1.30, p = 0.61, treatment 29, control 63, supplementation, unadjusted, RR approximated with OR, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
risk of death, 35.9% lower, RR 0.64, p = 0.74, high D levels (≥20ng/mL) 6 of 77 (7.8%), low D levels (<20ng/mL) 1 of 15 (6.7%), inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, multivariable logistic regression, outcome based on serum levels.
|
|
risk of mechanical ventilation, 56.9% lower, RR 0.43, p = 0.22, high D levels (≥20ng/mL) 8 of 15 (53.3%), low D levels (<20ng/mL) 4 of 15 (26.7%), inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, multivariable logistic regression, outcome based on serum levels.
|
|
risk of ICU admission, 13.1% higher, RR 1.13, p = 0.57, high D levels (≥20ng/mL) 54 of 77 (70.1%), low D levels (<20ng/mL) 9 of 15 (60.0%), inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, multivariable logistic regression, outcome based on serum levels.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Pecina et al., 27 Aug 2021, retrospective, USA, peer-reviewed, 4 authors, dosage not specified.
Vitamin D Status and Severe COVID-19 Disease Outcomes in Hospitalized Patients
Journal of Primary Care & Community Health, doi:10.1177/21501327211041206
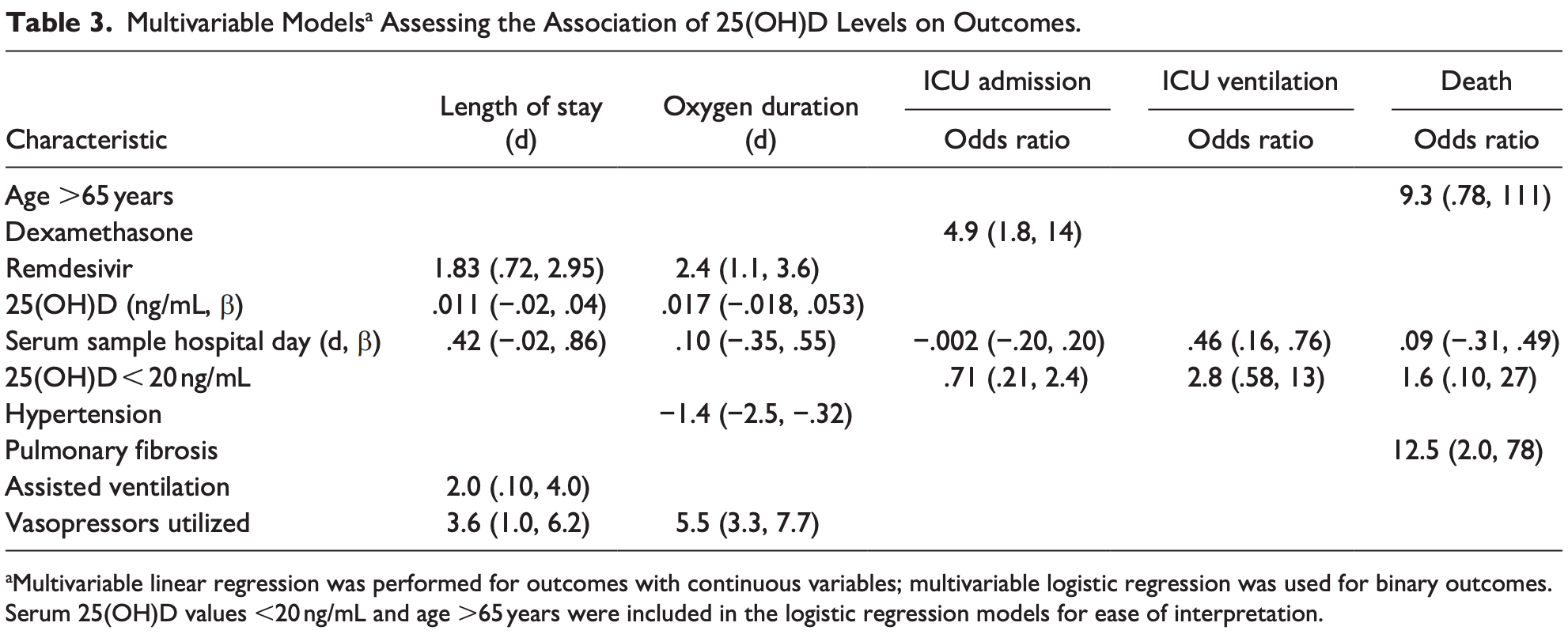
Background: Vitamin D deficiency may increase the risk of severe COVID-19 disease. Objectives: To determine if 25-hydroxyvitamin D [25(OH)D] levels in patients hospitalized for COVID-19 were associated with the clinical outcomes of days on oxygen, duration of hospitalization, ICU admission, need for assisted ventilation, or mortality. Methods: We conducted a retrospective study of 92 patients admitted to the hospital with SARS-CoV-2 infection between April 16, 2020 and October 17, 2020. Multivariable regression was performed to assess the independent relationship of 25(OH)D values on outcomes, adjusting for significant covariates and the hospitalization day the level was tested. Results: About 15 patients (16.3%) had 25(OH)D levels <20 ng/mL. Only 1 patient (3.4%) who had documented vitamin D supplementation prior to admission had 25(OH)D <20 ng/mL. Serum 25(OH)D concentrations were not significantly associated with any of our primary outcomes of days on oxygen, duration of hospitalization, intensive care unit (ICU) admission, need for mechanical ventilation, or mortality in any of the adjusted multivariable models. Adjusting for the hospital day of 25(OH) D sampling did not alter the relationship of 25(OH)D with any outcomes. Conclusion: Vitamin D status was not related to any of the primary outcomes reflecting severity of COVID-19 in hospitalized patients. However, our sample size may have lacked sufficient power to demonstrate a small effect of vitamin D status on these outcomes.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
Alsafar, Grant, Hijazi, COVID-19 disease severity and death in relation to vitamin D status among SARS-CoV-2-positive UAE residents, Nutrients
Amer, Qayyum, Relation between serum 25-hydroxyvitamin D and C-reactive protein in asymptomatic adults (from the continuous National Health and Nutrition Examination Survey 2001 to 2006), Am J Cardiol
Annweiler, Beaudenon, Gautier, COvid-19 and high-dose VITamin D supplementation TRIAL in high-risk older patients (COVIT-TRIAL): study protocol for a randomized controlled trial, Trials
Annweiler, Corvaisier, Gautier, Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study, Nutrients
Aranow, Vitamin D and the immune system, J Investig Med
Bilezikian, Bikle, Hewison, Mechanisms in endocrinology: vitamin D and COVID-19, Eur J Endocrinol
Cascella, Rajnik, Cuomo, Dulebohn, Napoli, Features, Evaluation, and Treatment of Coronavirus
D'avolio, Avataneo, Manca, 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., The possible role of vitamin D in suppressing cytokine storm and associated mortality in COVID-19 patients, medRxiv
Ginde, Mansbach, Camargo, Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey, Arch Intern Med
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK biobank, Eur J Nutr
Heart, Lung, Blood ; Ginde, Brower, Caterino, Early high-dose vitamin D3 for critically ill, vitamin D-deficient patients, New Engl J Med
Hernández, Nan, Fernandez-Ayala, Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metab
Holick, Vitamin D status: measurement, interpretation, and clinical application, Ann Epidemiol
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Ilie, Stefanescu, Smith, Va, Eshein et al., logistic regression was used for binary outcomes. Serum 25(OH)D values <20 ng/mL and age >65 years were included in the logistic regression models for ease of interpretation
Khare, Godbole, Pawar, Calcitriol [1,25[OH] 2 D3] pre-and post-treatment suppresses inflammatory response to influenza A (H1N1) infection in human lung A549 epithelial cells, Eur J Nutr
Laaksi, Ruohola, Tuohimaa, An association of serum vitamin D concentrations <40, Am J Clin Nutr
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ
Murai, Fernandes, Sales, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA
Nogués, Ovejero, Quesada-Gomez, Calcifediol treatment and COVID-19-related outcomes, SSRN Electron J. Published, doi:10.1210/clinem/dgab405
Peckham, De Gruijter, Raine, Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission, Nat Commun
Reid, Toole, Knox, The relation between acute changes in the systemic inflammatory response and plasma 25-hydroxyvitamin D concentrations after elective knee arthroplasty, Am J Clin Nutr
Ross, Manson, Abrams, The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know, J Clin Endocrinol Metab
Smet, Herroelen, Gryspeerdt, Martens, Vitamin D deficiency as risk factor for severe 1 COVID-19: a convergence of two pandemics
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review, JAMA
DOI record:
{
"DOI": "10.1177/21501327211041206",
"ISSN": [
"2150-1327",
"2150-1327"
],
"URL": "http://dx.doi.org/10.1177/21501327211041206",
"abstract": "<jats:sec><jats:title>Background:</jats:title><jats:p> Vitamin D deficiency may increase the risk of severe COVID-19 disease. </jats:p></jats:sec><jats:sec><jats:title>Objectives:</jats:title><jats:p> To determine if 25-hydroxyvitamin D [25(OH)D] levels in patients hospitalized for COVID-19 were associated with the clinical outcomes of days on oxygen, duration of hospitalization, ICU admission, need for assisted ventilation, or mortality. </jats:p></jats:sec><jats:sec><jats:title>Methods:</jats:title><jats:p> We conducted a retrospective study of 92 patients admitted to the hospital with SARS-CoV-2 infection between April 16, 2020 and October 17, 2020. Multivariable regression was performed to assess the independent relationship of 25(OH)D values on outcomes, adjusting for significant covariates and the hospitalization day the level was tested. </jats:p></jats:sec><jats:sec><jats:title>Results:</jats:title><jats:p> About 15 patients (16.3%) had 25(OH)D levels <20 ng/mL. Only 1 patient (3.4%) who had documented vitamin D supplementation prior to admission had 25(OH)D <20 ng/mL. Serum 25(OH)D concentrations were not significantly associated with any of our primary outcomes of days on oxygen, duration of hospitalization, intensive care unit (ICU) admission, need for mechanical ventilation, or mortality in any of the adjusted multivariable models. Adjusting for the hospital day of 25(OH)D sampling did not alter the relationship of 25(OH)D with any outcomes. </jats:p></jats:sec><jats:sec><jats:title>Conclusion:</jats:title><jats:p> Vitamin D status was not related to any of the primary outcomes reflecting severity of COVID-19 in hospitalized patients. However, our sample size may have lacked sufficient power to demonstrate a small effect of vitamin D status on these outcomes. </jats:p></jats:sec>",
"alternative-id": [
"10.1177/21501327211041206"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1970-1344",
"affiliation": [
{
"name": "Mayo Clinic, Rochester, MN, USA"
}
],
"authenticated-orcid": false,
"family": "Pecina",
"given": "Jennifer L.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-3816-8154",
"affiliation": [
{
"name": "Mayo Clinic, Rochester, MN, USA"
}
],
"authenticated-orcid": false,
"family": "Merry",
"given": "Stephen P.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Mayo Clinic, Rochester, MN, USA"
}
],
"family": "Park",
"given": "John G.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7644-8173",
"affiliation": [
{
"name": "Mayo Clinic, Rochester, MN, USA"
}
],
"authenticated-orcid": false,
"family": "Thacher",
"given": "Tom D.",
"sequence": "additional"
}
],
"container-title": "Journal of Primary Care & Community Health",
"container-title-short": "J Prim Care Community Health",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.sagepub.com"
]
},
"created": {
"date-parts": [
[
2021,
8,
28
]
],
"date-time": "2021-08-28T06:50:50Z",
"timestamp": 1630133450000
},
"deposited": {
"date-parts": [
[
2021,
8,
28
]
],
"date-time": "2021-08-28T06:50:55Z",
"timestamp": 1630133455000
},
"indexed": {
"date-parts": [
[
2023,
8,
10
]
],
"date-time": "2023-08-10T17:35:10Z",
"timestamp": 1691688910719
},
"is-referenced-by-count": 10,
"issued": {
"date-parts": [
[
2021,
1
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/21501327211041206",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/full-xml/10.1177/21501327211041206",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/21501327211041206",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "179",
"original-title": [],
"page": "215013272110412",
"prefix": "10.1177",
"published": {
"date-parts": [
[
2021,
1
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
27
]
]
},
"published-print": {
"date-parts": [
[
2021,
1
]
]
},
"publisher": "SAGE Publications",
"reference": [
{
"author": "Cascella M",
"key": "bibr1-21501327211041206",
"volume-title": "Features, Evaluation, and Treatment of Coronavirus",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "bibr2-21501327211041206"
},
{
"DOI": "10.1001/jama.2020.12839",
"doi-asserted-by": "publisher",
"key": "bibr3-21501327211041206"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "bibr4-21501327211041206"
},
{
"author": "Daneshkhah A",
"key": "bibr5-21501327211041206",
"volume": "2020",
"volume-title": "medRxiv",
"year": "2020"
},
{
"DOI": "10.3390/nu13051714",
"doi-asserted-by": "publisher",
"key": "bibr6-21501327211041206"
},
{
"DOI": "10.1001/archinternmed.2008.560",
"doi-asserted-by": "publisher",
"key": "bibr7-21501327211041206"
},
{
"DOI": "10.1093/ajcn/86.3.714",
"doi-asserted-by": "publisher",
"key": "bibr8-21501327211041206"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "bibr9-21501327211041206"
},
{
"DOI": "10.1530/EJE-20-0665",
"doi-asserted-by": "publisher",
"key": "bibr10-21501327211041206"
},
{
"DOI": "10.2310/JIM.0b013e31821b8755",
"doi-asserted-by": "publisher",
"key": "bibr11-21501327211041206"
},
{
"DOI": "10.1007/s00394-012-0449-7",
"doi-asserted-by": "publisher",
"key": "bibr12-21501327211041206"
},
{
"DOI": "10.3390/nu12051359",
"author": "D’Avolio A",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Nutrients",
"key": "bibr13-21501327211041206",
"volume": "12",
"year": "2020"
},
{
"author": "De Smet DDSK",
"journal-title": "medRxiv",
"key": "bibr14-21501327211041206",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "bibr15-21501327211041206"
},
{
"author": "Daneshkhah Va A",
"journal-title": "medRxiv",
"key": "bibr16-21501327211041206",
"year": "2020"
},
{
"author": "Hastie CE",
"first-page": "545",
"key": "bibr17-21501327211041206",
"volume": "60",
"volume-title": "Eur J Nutr",
"year": "2021"
},
{
"DOI": "10.1016/j.annepidem.2007.12.001",
"doi-asserted-by": "publisher",
"key": "bibr18-21501327211041206"
},
{
"DOI": "10.1210/jc.2010-2704",
"doi-asserted-by": "publisher",
"key": "bibr20-21501327211041206"
},
{
"author": "Hernández JL",
"first-page": "e1343",
"key": "bibr21-21501327211041206",
"volume": "106",
"volume-title": "J Clin Endocrinol Metab",
"year": "2021"
},
{
"DOI": "10.2139/ssrn.3771318",
"doi-asserted-by": "publisher",
"key": "bibr22-21501327211041206"
},
{
"DOI": "10.1038/s41467-020-19741-6",
"doi-asserted-by": "publisher",
"key": "bibr23-21501327211041206"
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "publisher",
"key": "bibr24-21501327211041206"
},
{
"DOI": "10.1056/NEJMoa1911124",
"doi-asserted-by": "publisher",
"key": "bibr25-21501327211041206"
},
{
"DOI": "10.1016/j.amjcard.2011.08.032",
"doi-asserted-by": "publisher",
"key": "bibr26-21501327211041206"
},
{
"DOI": "10.3945/ajcn.110.008490",
"doi-asserted-by": "publisher",
"key": "bibr27-21501327211041206"
},
{
"DOI": "10.1186/s13063-020-04928-5",
"doi-asserted-by": "publisher",
"key": "bibr28-21501327211041206"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "http://journals.sagepub.com/doi/10.1177/21501327211041206"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health",
"Community and Home Care"
],
"subtitle": [],
"title": "Vitamin D Status and Severe COVID-19 Disease Outcomes in Hospitalized Patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1177/sage-journals-update-policy",
"volume": "12"
}
