The Impact of Vitamin D Level on the Severity and Outcome of Hospitalized Patients with COVID-19 Disease
et al., International Journal of General Medicine, doi:10.2147/ijgm.s346169, Jan 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 203 hospitalized COVID-19 patients in Saudi Arabia, showing no significant difference in outcomes with vitamin D deficiency.
This is the 116th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 38.6% lower, RR 0.61, p = 0.50, high D levels (≥20ng/mL) 2 of 76 (2.6%), low D levels (<20ng/mL) 13 of 127 (10.2%), inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk.
|
|
risk of mechanical ventilation, 31.0% lower, RR 0.69, p = 0.51, high D levels (≥20ng/mL) 2 of 76 (2.6%), low D levels (<20ng/mL) 13 of 127 (10.2%), inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk.
|
|
risk of ICU admission, 41.8% lower, RR 0.58, p = 0.20, high D levels (≥20ng/mL) 2 of 76 (2.6%), low D levels (<20ng/mL) 13 of 127 (10.2%), inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
AlKhafaji et al., 31 Jan 2022, retrospective, Saudi Arabia, peer-reviewed, mean age 56.8, 16 authors, study period January 2021 - August 2021.
Contact: mtalhariri@iau.edu.sa.
The Impact of Vitamin D Level on the Severity and Outcome of Hospitalized Patients with COVID-19 Disease
International Journal of General Medicine, doi:10.2147/ijgm.s346169
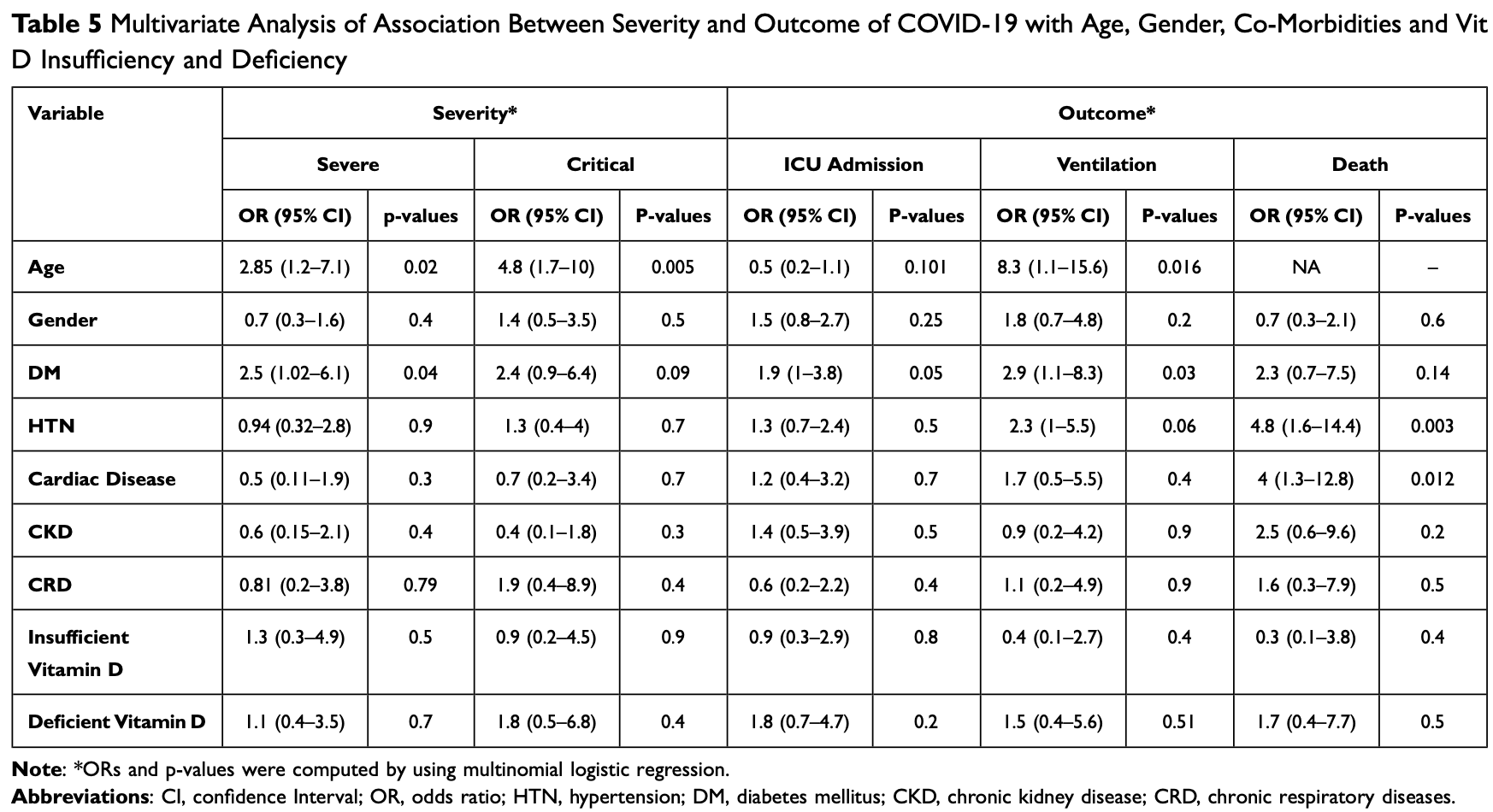
The world is experiencing a life-altering and extraordinary situation in response to the COVID-19 pandemic. There are limited data and controversies regarding the relationship between vitamin D (Vit D) status and COVID-19 disease. Thus, this study was designed to investigate the association between Vit D levels and the severity or outcomes of COVID-19 disease. Methods: A cross-sectional observational study was conducted in the Eastern province of Saudi Arabia from January to August 2021. All the admitted patients who were diagnosed with COVID-19 infection were distributed into three groups depending on their Vit D levels: normal, insufficiency, and deficiency. For the three groups, demographic data, and laboratory investigations as well as data regarding the severity of COVID-19 were collected and analysed. Results: A total of 203 diagnosed cases of COVID-19 were included in this study. The Vit D level was normal (>30) in 31 (15.3%) cases, insufficient in 45 (22.2%) cases and deficient in 127 (62.6%) cases. Among the included cases, 58 (28.6%) were critical cases, 109 (53.7%) were severe and 36 (17.7%) had a mild-moderate COVID-19 infection. The most prevalent comorbidity of patients was diabetes mellitus 117 (57.6%), followed by hypertension 70 (34.5%), cardiac disease 24 (11.8%), chronic kidney disease 19 (9.4%) and chronic respiratory disease in 17 (8.4%) cases. Importantly, the current study did not detect any significant association between Vit D status and COVID-19 severity (p-value=0.371) or outcomes (hospital stay, intensive care units admission, ventilation, and mortality rate) (p-value > 0.05), even after adjusting the statistical model for the confounders.
Conclusion: In hospital settings, Vit D levels are not associated with the severity or outcomes of COVID-19 disease. Further, well-designed studies are required to determine whether Vit D status provides protective effects against worse COVID-19 outcomes.
Author Contributions All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure The authors report no conflicts of interest in this work.
International Journal of General Medicine
Dovepress
References
Al-Alyani, Ha, On, Alani, Sadat-Ali, Vitamin D deficiency in Saudi Arabians: a reality or simply hype: a meta-analysis (2008-2015), J Family Community Med, doi:10.4103/jfcm.JFCM_73_17
Al-Harbi, Ya, Abdellatif, Al-Ahmadey, Alahmadi, Retrospective evaluation of the serum level of vitamin D among COVID-19 patients in Al Madinah, Saudi Arabia, Biotechnol Biochem Res, doi:10.30918/BBR.91.21.018
Al-Raddadi, Bahijri, Borai, Alraddadi, Prevalence of lifestyle practices that might affect bone health in relation to vitamin D status among female Saudi adolescents, Nutrition, doi:10.1016/J.NUT.2017.07.015
Alahmari, Khan, Elganainy, Epidemiological and clinical features of COVID-19 patients in Saudi Arabia, J Infect Public Health, doi:10.1016/j.jiph.2021.01.003
Alguwaihes, Sabico, Hasanato, Severe vitamin D deficiency is not related to SARS-CoV-2 infection but may increase mortality risk in hospitalized adults: a retrospective casecontrol study in an Arab Gulf country, Aging Clin Exp Res, doi:10.1007/S40520-021-01831-0
Ali, Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19, J Med Virol, doi:10.1002/JMV.26097
Ali, Noman, Guo, Myoglobin and C-reactive protein are efficient and reliable early predictors of COVID-19 associated mortality, Sci Rep, doi:10.1038/S41598-021-85426-9
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J Infect Public Health, doi:10.1016/J.JIPH.2020.06.021
Aljohani, Os, Dairy products consumption and serum 25-hydroxyvitamin D level in Saudi children and adults, Int J Clin Exp Pathol
Alkerwi, Sauvageot, Gilson, Stranges, Prevalence and correlates of vitamin D deficiency and insufficiency in Luxembourg adults: evidence from the observation of cardiovascular risk factors (ORISCAV-LUX) study, Nutrients, doi:10.3390/nu7085308
Alyami, Naser, Orabi, Alwafi, Alyami, Epidemiology of COVID-19 in the Kingdom of Saudi Arabia: an ecological study, Front Public Health, doi:10.3389/fpubh.2020.00506
Alzaheb, Al-Amer, Prevalence and predictors of hypovitaminosis D among female university students in Tabuk, Saudi Arabia, Clin Med Insights Womens Health, doi:10.1177/1179562X17702391
Alzaheb, The prevalence of hypovitaminosis D and its associated risk factors among women of reproductive age in Saudi Arabia: a systematic review and meta-analysis, Clin Med Insights Womens Health, doi:10.1177/1179562x18767884
Butler-Laporte, Nakanishi, Mooser, Vitamin D and COVID-19 susceptibility and severity in the COVID-19 host genetics initiative: a Mendelian randomization study, PLoS Med, doi:10.1371/journal.pmed.1003605
Cannell, Vieth, Umhau, Epidemic influenza and vitamin D, Epidemiol Infect, doi:10.1017/S0950268806007175
Carpagnano, Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Castillo, Costa, Barrios, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
Darling, Ahmadi, Ward, Vitamin D concentration, body mass index, ethnicity and SARS-CoV-2/COVID-19: initial analysis of the first-reported UK Biobank Cohort positive cases (n 1474) compared with negative controls (n 4643), Proc Nutr Soc, doi:10.1017/S0029665121000185
Gibson-Moore, Vitamin D: what's new a year on from the COVID-19 outbreak?, Nutr Bull, doi:10.1111/nbu.12499
Goweiz, Aldhafery, Potential cause affecting bone quality in Saudi Arabia: new insights, J Fam Med Prim Care, doi:10.4103/JFMPC.JFMPC_1872_20
Grant, Lahore, Mcdonnell, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/NU12040988
Hammad, Benajiba, Lifestyle factors influencing bone health in young adult women in Saudi Arabia, Afr Health Sci, doi:10.4314/AHS.V17I2.28
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr Clin Res Rev, doi:10.1016/j.dsx.2020.04.050
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr, doi:10.1007/s00394-020-02372-4
Holick, Binkley, Bischoff-Ferrari, Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab, doi:10.1210/JC.2011-0385
Honardoost, Ghavideldarestani, Khamseh, Role of vitamin D in pathogenesis and severity of COVID-19 infection, Arch Physiol Biochem, doi:10.1080/13813455.2020.1792505
Itkonen, Erkkola, Cje, Vitamin D fortification of fluid milk products and their contribution to vitamin D intake and vitamin D status in observational studies-a review, Nutrients, doi:10.3390/nu10081054
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep, doi:10.1038/s41598-020-77093-z
Jolliffe, Stefanidis, Wang, Vitamin d metabolism is dysregulated in asthma and chronic obstructive pulmonary disease, Am J Respir Crit Care Med, doi:10.1164/rccm.201909-1867OC
Kanan, Saleh, Fakhoury, Adham, Aljaser et al., Year-round vitamin D deficiency among Saudi female out-patients, Public Health Nutr, doi:10.1017/S1368980012002947
Kruit, Zanen, The association between vitamin D and C-reactive protein levels in patients with inflammatory and non-inflammatory diseases, Clin Biochem, doi:10.1016/J.CLINBIOCHEM.2016.01.002
Lu, Chen, Zhang, An evaluation of the vitamin D3 content in fish: is the vitamin D content adequate to satisfy the dietary requirement for vitamin D?, J Steroid Biochem Mol Biol, doi:10.1016/J.JSBMB.2006.12.010
Mahmudpour, Roozbeh, Keshavarz, Farrokhi, Nabipour, COVID-19 cytokine storm: the anger of inflammation, Cytokine, doi:10.1016/j.cyto.2020.155151
Mansur, Tajer, Mariani, Inserra, Ferder et al., Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection, Clin e Investig En Arterioscler, doi:10.1016/j.arteri.2020.05.003
Mckee, Stuckler, If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future, Nat Med, doi:10.1038/s41591-020-0863-y
Mercola, Grant, Wagner, Evidence regarding vitamin d and risk of covid-19 and its severity, Nutrients, doi:10.3390/nu12113361
Murai, Fernandes, Sales, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA, doi:10.1001/jama.2020.26848
Murai, Fernandes, Sales, Effect of vitamin D3 supplementation vs placebo on hospital length of stay in patients with severe COVID-19: a multicenter, double-blind, randomized controlled trial, medRxiv, doi:10.1001/jama.2020.26848
Nm, Vitamin D in Saudi Arabia: prevalence, distribution and disease associations, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2016.12.017
Palacios, The role of nutrients in bone health, from A to Z, Crit Rev Food Sci Nutr, doi:10.1080/10408390500466174
Panfili, Roversi, Argenio, Rossi, Cappa et al., Possible role of vitamin D in Covid-19 infection in pediatric population, J Endocrinol Invest, doi:10.1007/s40618-020-01327-0
Pepys, Hirschfield, C-reactive protein: a critical update, J Clin Invest, doi:10.1172/JCI18921
Rabenberg, Scheidt-Nave, Busch, Rieckmann, Hintzpeter et al., Vitamin D status among adults in Germany -results from the German Health Interview and Examination Survey for Adults (DEGS1) chronic disease epidemiology, International Journal of General Medicine, doi:10.1186/s12889-015-2016-7
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality, Am J Clin Pathol, doi:10.1093/AJCP/AQAA252
Teymoori-Rad, Shokri, Salimi, Marashi, The interplay between vitamin D and viral infections, Rev Med Virol, doi:10.1002/RMV.2032
Zareef, Jackson, Alkahtani, Vitamin D intake among premenopausal women living in Jeddah: food sources and relationship to demographic factors and bone health, J Nutr Metab, doi:10.1155/2018/8570986
DOI record:
{
"DOI": "10.2147/ijgm.s346169",
"ISSN": [
"1178-7074"
],
"URL": "http://dx.doi.org/10.2147/ijgm.s346169",
"author": [
{
"affiliation": [],
"family": "AlKhafaji",
"given": "Dania",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6056-8616",
"affiliation": [],
"authenticated-orcid": true,
"family": "Al Argan",
"given": "Reem",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Albaker",
"given": "Waleed",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3906-0188",
"affiliation": [],
"authenticated-orcid": true,
"family": "Al Elq",
"given": "Abdulmohsen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9807-4870",
"affiliation": [],
"authenticated-orcid": true,
"family": "Al-Hariri",
"given": "Mohammed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "AlSaid",
"given": "Abir",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alwaheed",
"given": "Abrar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alqatari",
"given": "Safi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7680-8562",
"affiliation": [],
"authenticated-orcid": true,
"family": "Alzaki",
"given": "Alaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alwarthan",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "AlRubaish",
"given": "Fatima",
"sequence": "additional"
},
{
"affiliation": [],
"family": "AlGuaimi",
"given": "Haya",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4633-5645",
"affiliation": [],
"authenticated-orcid": true,
"family": "Ismaeel",
"given": "Fatema",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4407-8654",
"affiliation": [],
"authenticated-orcid": true,
"family": "Alsaeed",
"given": "Nidaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "AlElq",
"given": "Zainab",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zainuddin",
"given": "Fatma",
"sequence": "additional"
}
],
"container-title": "International Journal of General Medicine",
"container-title-short": "IJGM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T08:10:28Z",
"timestamp": 1641543028000
},
"deposited": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T08:10:34Z",
"timestamp": 1641543034000
},
"indexed": {
"date-parts": [
[
2023,
4,
17
]
],
"date-time": "2023-04-17T13:56:36Z",
"timestamp": 1681739796588
},
"is-referenced-by-count": 10,
"issued": {
"date-parts": [
[
2022,
1
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
1
]
],
"date-time": "2022-01-01T00:00:00Z",
"timestamp": 1640995200000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=77454",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=77454",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "343-352",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2022,
1
]
]
},
"published-online": {
"date-parts": [
[
2022,
1
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1016/j.jsbmb.2016.12.017",
"author": "Al-Daghri",
"doi-asserted-by": "publisher",
"first-page": "102",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "ref1",
"volume": "175",
"year": "2018"
},
{
"DOI": "10.3390/nu7085308",
"author": "Alkerwi",
"doi-asserted-by": "publisher",
"first-page": "6780",
"journal-title": "Nutrients",
"key": "ref2",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1080/10408390500466174",
"author": "Palacios",
"doi-asserted-by": "publisher",
"first-page": "621",
"journal-title": "Crit Rev Food Sci Nutr",
"key": "ref3",
"volume": "46",
"year": "2006"
},
{
"DOI": "10.1186/s12889-015-2016-7",
"author": "Rabenberg",
"doi-asserted-by": "publisher",
"first-page": "641",
"journal-title": "BMC Public Health",
"key": "ref4",
"volume": "15",
"year": "2015"
},
{
"author": "Al-Daghri",
"first-page": "8480",
"journal-title": "Int J Clin Exp Pathol",
"key": "ref5",
"volume": "8",
"year": "2015"
},
{
"DOI": "10.1177/1179562x18767884",
"author": "Alzaheb",
"doi-asserted-by": "publisher",
"first-page": "1179562X18767884",
"journal-title": "Clin Med Insights Womens Health",
"key": "ref6",
"volume": "3",
"year": "2018"
},
{
"DOI": "10.1155/2018/8570986",
"author": "Zareef",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Nutr Metab",
"key": "ref7",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.4103/JFMPC.JFMPC_1872_20",
"author": "Al-Hariri",
"doi-asserted-by": "publisher",
"first-page": "533",
"journal-title": "J Fam Med Prim Care",
"key": "ref8",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.4314/AHS.V17I2.28",
"author": "Hammad",
"doi-asserted-by": "publisher",
"first-page": "524",
"journal-title": "Afr Health Sci",
"key": "ref9",
"volume": "17",
"year": "2017"
},
{
"DOI": "10.1016/J.JSBMB.2006.12.010",
"author": "Lu",
"doi-asserted-by": "publisher",
"first-page": "642",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "ref10",
"volume": "103",
"year": "2007"
},
{
"DOI": "10.3390/nu10081054",
"author": "Itkonen",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Nutrients",
"key": "ref11",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1017/S1368980012002947",
"author": "Kanan",
"doi-asserted-by": "publisher",
"first-page": "544",
"journal-title": "Public Health Nutr",
"key": "ref12",
"volume": "16",
"year": "2013"
},
{
"DOI": "10.1177/1179562X17702391",
"author": "Alzaheb",
"doi-asserted-by": "publisher",
"first-page": "1179562X1770239",
"journal-title": "Clin Med Insights Womens Health",
"key": "ref13",
"volume": "10",
"year": "2017"
},
{
"DOI": "10.1016/J.NUT.2017.07.015",
"author": "Al-Raddadi",
"doi-asserted-by": "publisher",
"first-page": "108",
"journal-title": "Nutrition",
"key": "ref14",
"volume": "45",
"year": "2018"
},
{
"DOI": "10.1038/s41591-020-0863-y",
"author": "McKee",
"doi-asserted-by": "publisher",
"first-page": "640",
"journal-title": "Nat Med",
"key": "ref15",
"volume": "26",
"year": "2020"
},
{
"key": "ref16",
"unstructured": "World Health Organization. Available from: https://covid19.who.int/region/emro/country/sa. Accessed December 29, 2021."
},
{
"DOI": "10.1016/j.arteri.2020.05.003",
"author": "Mansur",
"doi-asserted-by": "publisher",
"first-page": "267",
"journal-title": "Clin e Investig En Arterioscler",
"key": "ref17",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.3390/NU12040988",
"author": "Grant",
"doi-asserted-by": "publisher",
"first-page": "988",
"journal-title": "Nutrients",
"key": "ref18",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1002/RMV.2032",
"author": "Teymoori-Rad",
"doi-asserted-by": "publisher",
"first-page": "e2032",
"journal-title": "Rev Med Virol",
"key": "ref19",
"volume": "29",
"year": "2019"
},
{
"DOI": "10.1093/AJCP/AQAA252",
"author": "De Smet",
"doi-asserted-by": "publisher",
"first-page": "381",
"journal-title": "Am J Clin Pathol",
"key": "ref20",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"author": "Hastie",
"doi-asserted-by": "publisher",
"first-page": "561",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "ref21",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1017/S0029665121000185",
"author": "Darling",
"doi-asserted-by": "publisher",
"first-page": "7",
"journal-title": "Proc Nutr Soc",
"key": "ref22",
"volume": "80",
"year": "2021"
},
{
"DOI": "10.1016/J.JIPH.2020.06.021",
"author": "Ali",
"doi-asserted-by": "publisher",
"first-page": "1373",
"journal-title": "J Infect Public Health",
"key": "ref23",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1003605",
"author": "Butler-Laporte",
"doi-asserted-by": "publisher",
"first-page": "e1003605",
"journal-title": "PLoS Med",
"key": "ref24",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1007/s40618-020-01327-0",
"author": "Panfili",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Endocrinol Invest",
"key": "ref25",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1080/13813455.2020.1792505",
"author": "Honardoost",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Arch Physiol Biochem",
"key": "ref26",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"author": "Entrenas Castillo",
"doi-asserted-by": "publisher",
"first-page": "105751",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "ref27",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.26848",
"author": "Murai",
"doi-asserted-by": "publisher",
"first-page": "1053",
"journal-title": "JAMA",
"key": "ref28",
"volume": "325",
"year": "2021"
},
{
"key": "ref29",
"unstructured": "Public Health Authority. Laboratory diagnosis. Available from: https://covid19.cdc.gov.sa/professionals-health-workers/laboratory-diagnosis/. Accessed December 9, 2021."
},
{
"DOI": "10.1210/JC.2011-0385",
"author": "Holick",
"doi-asserted-by": "publisher",
"first-page": "1911",
"journal-title": "J Clin Endocrinol Metab",
"key": "ref30",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.1007/s00394-020-02372-4",
"author": "Hastie",
"doi-asserted-by": "publisher",
"first-page": "545",
"journal-title": "Eur J Nutr",
"key": "ref31",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"author": "Murai",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "ref32",
"year": "2020"
},
{
"DOI": "10.4103/jfcm.JFCM_73_17",
"author": "Al-Alyani",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Family Community Med",
"key": "ref33",
"volume": "25",
"year": "2018"
},
{
"DOI": "10.3389/fpubh.2020.00506",
"author": "Alyami",
"doi-asserted-by": "publisher",
"first-page": "506",
"journal-title": "Front Public Health",
"key": "ref34",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.jiph.2021.01.003",
"author": "Alahmari",
"doi-asserted-by": "publisher",
"first-page": "437",
"journal-title": "J Infect Public Health",
"key": "ref35",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1007/S40520-021-01831-0",
"author": "Alguwaihes",
"doi-asserted-by": "publisher",
"first-page": "1415",
"journal-title": "Aging Clin Exp Res",
"key": "ref36",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"author": "Jain",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Sci Rep",
"key": "ref37",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.30918/BBR.91.21.018",
"author": "Al-Harbi",
"doi-asserted-by": "publisher",
"first-page": "8",
"journal-title": "Biotechnol Biochem Res",
"key": "ref38",
"volume": "9",
"year": "2021"
},
{
"key": "ref39",
"unstructured": "GOV.UK. SACN rapid review: vitamin D and acute respiratory tract infections. Available from: https://www.gov.uk/government/publications/sacn-rapid-review-vitamin-d-and-acute-respiratory-tract-infections. Accessed October 4, 2021."
},
{
"DOI": "10.1017/S0950268806007175",
"author": "Cannell",
"doi-asserted-by": "publisher",
"first-page": "1129",
"journal-title": "Epidemiol Infect",
"key": "ref40",
"volume": "134",
"year": "2006"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"author": "Carpagnano",
"doi-asserted-by": "publisher",
"first-page": "765",
"journal-title": "J Endocrinol Invest",
"key": "ref41",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.3390/nu12113361",
"author": "Mercola",
"doi-asserted-by": "publisher",
"first-page": "3361",
"journal-title": "Nutrients",
"key": "ref42",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.cyto.2020.155151",
"author": "Mahmudpour",
"doi-asserted-by": "publisher",
"first-page": "155151",
"journal-title": "Cytokine",
"key": "ref43",
"volume": "133",
"year": "2020"
},
{
"DOI": "10.1164/rccm.201909-1867OC",
"author": "Jolliffe",
"doi-asserted-by": "publisher",
"first-page": "371",
"journal-title": "Am J Respir Crit Care Med",
"key": "ref44",
"volume": "202",
"year": "2020"
},
{
"DOI": "10.1172/JCI18921",
"author": "Pepys",
"doi-asserted-by": "publisher",
"first-page": "1805",
"journal-title": "J Clin Invest",
"key": "ref45",
"volume": "111",
"year": "2003"
},
{
"DOI": "10.1002/JMV.26097",
"author": "Ali",
"doi-asserted-by": "publisher",
"first-page": "2409",
"journal-title": "J Med Virol",
"key": "ref46",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1038/S41598-021-85426-9",
"author": "Ali",
"doi-asserted-by": "publisher",
"journal-title": "Sci Rep",
"key": "ref47",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/J.CLINBIOCHEM.2016.01.002",
"author": "Kruit",
"doi-asserted-by": "publisher",
"first-page": "534",
"journal-title": "Clin Biochem",
"key": "ref48",
"volume": "49",
"year": "2016"
},
{
"DOI": "10.1111/nbu.12499",
"author": "Gibson-Moore",
"doi-asserted-by": "publisher",
"first-page": "195",
"journal-title": "Nutr Bull",
"key": "ref49",
"volume": "46",
"year": "2021"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/the-impact-of-vitamin-d-level-on-the-severity-and-outcome-of-hospitali-peer-reviewed-fulltext-article-IJGM"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "The Impact of Vitamin D Level on the Severity and Outcome of Hospitalized Patients with COVID-19 Disease",
"type": "journal-article",
"volume": "Volume 15"
}
