Repurposing selective serotonin reuptake inhibitors for severity of COVID-19: A population-based study
et al., European Neuropsychopharmacology, doi:10.1016/j.euroneuro.2023.03.011, Apr 2023
31st treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
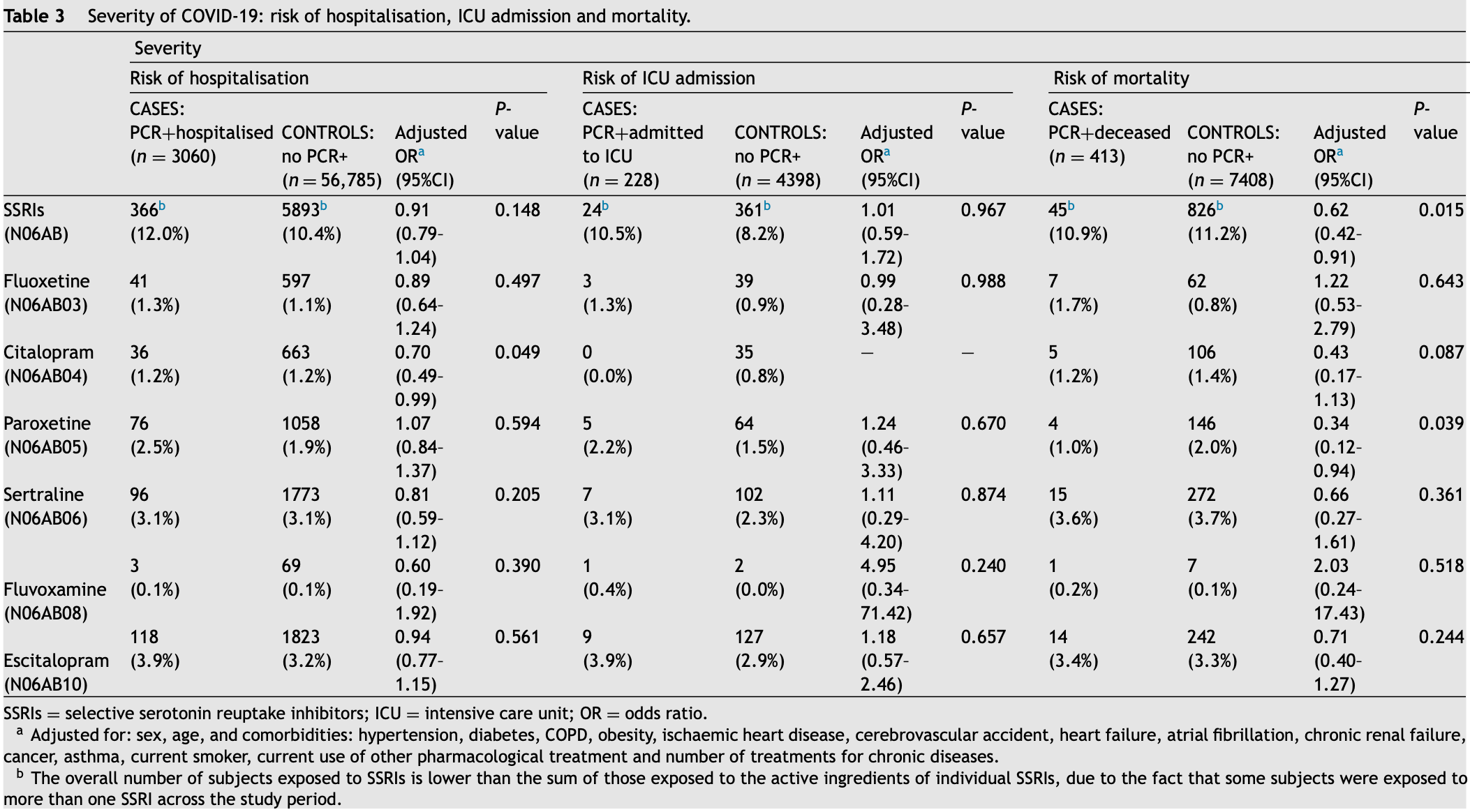
Retrospective 86,602 patients in Spain, showing lower COVID-19 risk SSRIs citalopram and paroxetine. There were no significant difference for fluvoxamine, which few patients were taking.
|
risk of death, 103.0% higher, OR 2.03, p = 0.52, treatment 1 of 413 (0.2%) cases,
7 of 7,408 (0.1%) controls, adjusted per study, case control OR.
|
|
risk of ICU admission, 395.0% higher, OR 4.95, p = 0.24, treatment 1 of 228 (0.4%) cases,
2 of 4,398 (0.0%) controls, adjusted per study, case control OR.
|
|
risk of hospitalization, 40.0% lower, OR 0.60, p = 0.39, treatment 3 of 3,060 (0.1%) cases,
69 of 56,785 (0.1%) controls, adjusted per study, case control OR.
|
|
risk of progression, 32.0% lower, OR 0.68, p = 0.56, treatment 3 of 3,060 (0.1%) cases,
25 of 26,757 (0.1%) controls, adjusted per study, case control OR.
|
|
risk of case, 12.0% lower, OR 0.88, p = 0.60, treatment 28 of 29,817 (0.1%) cases,
69 of 56,785 (0.1%) controls, adjusted per study, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Visos-Varela et al., 23 Apr 2023, retrospective, Spain, peer-reviewed, 8 authors.
Contact: maruxa.zapata@usc.es.
Repurposing selective serotonin reuptake inhibitors for severity of COVID-19: A population-based study
European Neuropsychopharmacology, doi:10.1016/j.euroneuro.2023.03.011
The World Health Organization has proposed that a search be made for alternatives to vaccines for the prevention and treatment of COVID-19, with one such alternative being selective serotonin reuptake inhibitors (SSRIs). This study thus sought to assess: the impact of previous treatment with SSRI antidepressants on the severity of COVID-19 (risk of hospitalisation, admission to an intensive care unit [ICU], and mortality), its influence on susceptibility to SARS-CoV-2 and progression to severe COVID-19. We conducted a population-based multiple case-control study in a region in the north-west of Spain. Data were sourced from electronic health records. Adjusted odds ratios (aORs) and 95%CIs were calculated using multilevel logistic regression. We collected data from a total of 86,602 subjects: 3060 cases PCR + , 26,757 non-hospitalised cases PCR + and 56,785 controls (without PCR + ). Citalopram displayed a statistically significant
Role of funding source This study was sponsored by the Carlos III Institute of Health via the "COV20/00470" project (co-funded by the European Regional Development Fund , "A way to make Europe").
Contributors IVV: wrote paper. MZC: designed study, wrote paper. MPL: designed study, analysed data, revised paper. ECM: designed study, revised paper MS: analysed data, revised paper. MTH: designed study, revised paper. AF: designed study, analysed data, revised paper. ASB: designed study, analysed data, revised paper. All authors contributed to and have approved the final manuscript.
Conflicts of Interest The authors declare that they have no conflicts of interest.
Supplementary materials Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.euroneuro. 2023.03.011 .
References
Abajo, De, Rodríguez-Martín, Lerma, Mejía-Abril et al., Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study, Lancet, doi:10.1016/S0140-6736(20)31030-8
Alsabhan, Alshammari, New Use of the SSRI Fluvoxamine in the Treatment of COVID-19 Symptoms, IntechOpen, doi:10.5772/intechopen.105023
Arteaga-Henríquez, Simon, Burger, Weidinger, Wijkhuijs et al., Low-grade inflammation as a predictor of antidepressant and anti-inflammatory therapy response in MDD patients: a systematic review of the literature in combination with an analysis of experimental data collected in the EU-MOODINFLAME consortium, Front. Psychiatry, doi:10.3389/fpsyt.2019.00458
Benton, Lynch, Dubé, Gettes, Tustin et al., Selective serotonin reuptake inhibitor suppression of HIV infectivity and replication, Psychosom. Med, doi:10.1097/PSY.0b013e3181f883ce
Brandal, Macdonald, Veneti, Ravlo, Lange et al., Outbreak caused by the SARS-CoV-2 Omicron variant in Norway, Euro. Surveill, doi:10.2807/1560-7917.ES.2021.26.50.2101147
Brown, Prescott, Applied Mixed Models in Medicine
Callaway, Could new COVID variants undermine vaccines? Labs scramble to find out, Nature, doi:10.1038/d41586-021-00031-0
Callaway, Ledford, How to redesign COVID vaccines so they protect against variants, Nature, doi:10.1038/d41586-021-00241-6
Calusic, Marcec, Luksa, Jurkovic, Kovac et al., Safety and efficacy of fluvoxamine in COVID-19 ICU patients: an open label, prospective cohort trial with matched controls, Br. J. Clin. Pharmacol, doi:10.1111/bcp.15126
Carpinteiro, Edwards, Hoffmann, Kochs, Gripp et al., Pharmacological inhibition of acid sphingomyelinase prevents uptake of SARS-CoV-2 by epithelial cells, Cell. Rep. Med, doi:10.1016/j.xcrm.2020.100142
Christie, Mbaeyi, Walensky, CDC interim recommendations for fully vaccinated people: an important first step, JAMA, doi:10.1001/jama.2021.4367
Del Rio, Malani, COVID-19 in 2022-the beginning of the end or the end of the beginning, JAMA, doi:10.1001/jama.2022.9655
Deng, Rayner, Ramaraju, Abbas, Garcia et al., Efficacy and safety of selective serotonin reuptake inhibitors in COVID-19 management: a systematic review and meta-analysis, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2023.01.010
Devane, Comparative safety and tolerability of selective serotonin reuptake inhibitors, Hum. Psychopharmacol, doi:10.1002/hup.470100907
Dong, Zhang, Yao, Ren, Yang et al., Effects of escitalopram, Rcitalopram, and reboxetine on serum levels of tumor necrosis factor-α, interleukin-10, and depression-like behavior in mice after lipopolysaccharide administration, Pharmacol. Biochem. Behav, doi:10.1016/j.pbb.2016.02.005
Fico, Isayeva, De Prisco, Oliva, Solè et al., Psychotropic drug repurposing for COVID-19: A systematic review and meta-analysis, Eur. Neuropsychopharmacol, doi:10.1016/j.euroneuro.2022.10.004
Fred, Kuivanen, Ugurlu, Casarotto, Levanov et al., Antidepressant and antipsychotic drugs reduce viral infection by SARS-CoV-2 and fluoxetine shows antiviral activity against the novel variants in vitro, Front. Pharmacol, doi:10.3389/fphar.2021.755600
Fritz, Hoertel, Lenze, Jalali, Reiersen, Association between antidepressant use and ED or hospital visits in outpatients with SARS-CoV-2, Transl. Psychiatry, doi:10.1038/s41398-022-02109-3
Greeson, Gettes, Spitsin, Dubé, Benton et al., The selective serotonin reuptake inhibitor citalopram decreases human immunodeficiency virus receptor and coreceptor expression in immune cells, Biol. Psychiatry, doi:10.1016/j.biopsych.2015.11.003
Hashimoto, Repurposing of CNS drugs to treat COVID-19 infection: targeting the sigma-1 receptor, Eur. Arch. Psychiatry Clin. Neurosci, doi:10.1007/s00406-020-01231-x
Hashimoto, Suzuki, Hashimoto, Mechanisms of action of fluvoxamine for COVID-19: a historical review, Mol. Psychiatry, doi:10.1038/s41380-021-01432-3
Hassan, Sawyer, Peek, Lovell, Carvalho et al., Heightened COVID-19 mortality in people with severe mental illness persists after vaccination: a cohort study of greater manchester residents, Schizophr. Bull, doi:10.1093/schbul/sbac118
Hoertel, Sánchez-Rico, Cougoule, Gulbins, Kornhuber et al., Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: current evidence and potential mechanisms, Mol. Psychiatry, doi:10.1038/s41380-021-01254-3
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Carpinteiro et al., 2022a. Association between FIASMA psychotropic medications and reduced risk of intubation or death in individuals with psychiatric disorders hospitalized for severe COVID-19: an observational multicenter study, Transl. Psychiatry, doi:10.1038/s41398-022-01804-5
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Vernet et al., AP-HP/Université de Paris/INSERM COVID-19 Research Collaboration/AP-HP COVID CDR Initiative/'Entrepôt de Données de Santé' AP-HP Consortium, 2022c. Association between benzodiazepine receptor agonist use and mortality in patients hospitalised for COVID-19: a multicentre observational study, Epidemiol. Psychiatr. Sci, doi:10.1017/S2045796021000743
Hoertel, Sánchez-Rico, Kornhuber, Gulbins, Reiersen et al., On Behalf Of Ap-Hp/Université Paris Cité/Inserm Covid-Research Collaboration Ap-Hp Covid Cdr Initiative And Entrepôt de Données de Santé Ap-Hp Consortium, 2022b. Antidepressant use and its association with 28-day mortality in inpatients with SARS-CoV-2: support for the FIASMA model against COVID-19, J. Clin. Med, doi:10.3390/jcm11195882
Hoertel, Sánchez-Rico, Vernet, Beeker, Jannot et al., AP-HP /Universities / IN-SERM COVID-19 Research Collaboration and AP-HP COVID CDR Initiative, 2021a. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study, Mol. Psychiatry, doi:10.1038/s41380-021-01021-4
Huber, Szucs, Rapold, Reich, Identifying patients with chronic conditions using pharmacy data in Switzerland: an updated mapping approach to the classification of medications, BMC Public Health, doi:10.1186/1471-2458-13-1030
Imran, Kumar Arora, Asdaq, Khan, Alaqel et al., Discovery, development, and patent trends on molnupiravir: a prospective oral treatment for COVID-19, Molecules, doi:10.3390/molecules26195795
Israel, Shenhar, Green, Merzon, Golan-Cohen et al., Largescale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 infection, Vaccines, doi:10.3390/vaccines10010064
Kornhuber, Hoertel, Gulbins, The acid sphingomyelinase/ceramide system in COVID-19, Mol. Psychiatry, doi:10.1038/s41380-021-01309-5
Kumar, Li, Park, Hart, Song et al., Sphingolipid Biosynthesis Inhibition as a Host Strategy Against Diverse Pathogens, bioRxiv, doi:10.1101/2020.04.10.035683
Kutkat, Moatasim, Al-Karmalawy, Abulkhair, Gomaa et al., Robust antiviral activity of commonly prescribed antidepressants against emerging coronaviruses: in vitro and in silico drug repurposing studies, Sci. Rep, doi:10.1038/s41598-022-17082-6
Lam, Fresco, Medication adherence measures: an overview, Biomed Res. Int, doi:10.1155/2015/217047
Landes, Finan, Turk, COVID-19 mortality burden and comorbidity patterns among decedents with and without intellectual and developmental disability in the US, Disabil. Health J, doi:10.1016/j.dhjo.2022.101376
Lenze, Mattar, Zorumski, Stevens, Schweiger et al., Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial, JAMA, doi:10.1001/jama.2020.22760
Letendre, Marquie-Beck, Ellis, Woods, Best et al., The role of cohort studies in drug development: clinical evidence of antiviral activity of serotonin reuptake inhibitors and HMG-CoA reductase inhibitors in the central nervous system, J. Neuroimmune Pharmacol, doi:10.1007/s11481-006-9054-y
Liu, Sun, Wang, Zhao, Huang et al., The impact of dementia on the clinical outcome of COVID-19: a systematic review and meta-analysis, J. Alzheimers Dis, doi:10.3233/JAD-201016
Lu, Chao, Chang, Lan, Lai, Effect of fluvoxamine on outcomes of nonhospitalized patients with COVID-19: a systematic review and meta-analysis, J. Infect. Public Health, doi:10.1016/j.jiph.2022.10.010
Marcec, Majta, Likic, Will vaccination refusal prolong the war on SARS-CoV-2?, Postgrad. Med. J, doi:10.1136/postgradmedj-2020-138903
Meikle, Creeden, Mccullumsmith, Worth, SSRIs: applications in inflammatory lung disease and implications for COVID-19, Neuropsychopharmacol. Rep, doi:10.1002/npr2.12194
Menni, Valdes, Polidori, Antonelli, Penamakuri et al., Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study, Lancet, doi:10.1016/S0140-6736(22)00327-0
Nakhaee, Bayati, Rahmanian, Jolfayi, Zangiabadian et al., The Effect of Antidepressants on Severity of COVID-19 in Hospitalized Patients: A Systematic Review and Meta-Analysis, medRxiv, doi:10.1101/2022.04.11.22273709
Ohgi, Futamura, Kikuchi, Hashimoto, Effects of antidepressants on alternations in serum cytokines and depressive-like behavior in mice after lipopolysaccharide administration, Pharmacol. Biochem. Behav, doi:10.1016/j.pbb.2012.12.003
Pan, Peto, Henao-Restrepo, Preziosi, Sathiyamoorthy et al., Repurposed antiviral drugs for Covid-19-interim WHO solidarity trial results, N. Engl. J. Med, doi:10.1056/NEJMoa2023184
Pashaei, Drug repurposing of selective serotonin reuptake inhibitors: could these drugs help fight COVID-19 and save lives?, J. Clin. Neurosci, doi:10.1016/j.jocn.2021.03.010
Pinheiro, Bates, Mixed-Effects Models in S and S-PLUS
Planas, Veyer, Baidaliuk, Staropoli, Guivel-Benhassine et al., Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization, Nature, doi:10.1038/s41586-021-03777-9
Plotkin, Robinson, Cunningham, Iqbal, Larsen, The complexity and cost of vaccine manufacturing-an overview, Vaccine, doi:10.1016/j.vaccine.2017.06.003
Rajpoot, Alagumuthu, Baig, Dual targeting of 3CLpro and PLpro of SARS-CoV-2: a novel structure-based design approach to treat COVID-19, Curr. Res. Struct. Biol, doi:10.1016/j.crstbi.2020.12.001
Rauchman, Mendelson, Rauchman, Kasselman, Pinkhasov et al., Ongoing use of SSRIs does not alter outcome in hospitalized COVID-19 patients: a retrospective analysis, J. Clin. Med, doi:10.3390/penalty-@Mjcm11010070
Reis, Dos, Moreira-Silva, Silva, Thabane et al., Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial, Lancet Global Health, doi:10.1016/S2214-109X(21)00448-4
Rose, Van Der Laan, Why match? Investigating matched case-control study designs with causal effect estimation, Int. J. Biostat, doi:10.2202/1557-4679.1127
Rothman, Greenland, Lash, Case-control studies. Encyclopedia of Quantitative Risk Analysis and Assessment, doi:10.1002/9780470061596.risk0599
Sachs, Karim, Aknin, Allen, Brosbøl et al., The Lancet Commission on lessons for the future from the COVID-19 pandemic, Lancet, doi:10.1016/S0140-6736(22)01585-9
Sacre, Medghalchi, Gregory, Brennan, Williams, Fluoxetine and citalopram exhibit potent antiinflammatory activity in human and murine models of rheumatoid arthritis and inhibit toll-like receptors, Arthritis Rheum, doi:10.1002/art.27304
Saha, Tanmoy, Tanni, Goswami, Sium et al., New waves, new variants, old inequity: a continuing COVID-19 crisis, BMJ Global Health, doi:10.1136/bmjgh-2021-007031
Seftel, Boulware, Prospective cohort of fluvoxamine for early treatment of coronavirus disease 19, Open Forum Infect. Dis, doi:10.1093/ofid/ofab050
Sherman, Anderson, Dal Pan, Gray, Gross et al., Real-world evidence-what is it and what can it tell us?, N. Engl. J. Med, doi:10.1056/NEJMsb1609216
Shrotri, Navaratnam, Nguyen, Byrne, Geismar et al., Virus Watch Collaborative, 2021. Spike-antibody waning after second dose of BNT162b2 or ChAdOx1, Lancet, doi:10.1016/S0140-6736(21)01642-1
Smith, Lipsitch, Almond, Vaccine production, distribution, access, and uptake, Lancet, doi:10.1016/S0140-6736(11)60478-9
Stroup, Generalized Linear Mixed Models: Modern Concepts
Sukhatme, Reiersen, Vayttaden, Sukhatme, Fluvoxamine: a review of its mechanism of action and its role in COVID-19, Front. Pharmacol, doi:10.3389/fphar.2021.652688
Thom, Alexander, Baron, Garakani, Gross et al., Selective serotonin reuptake inhibitors: how long is long enough?, J. Psychiatr. Pract, doi:10.1097/PRA.0000000000000578
Torres, Artaza, Profeta, Alonso, Kang, COVID-19 vaccination: returning to WHO's health for all, Lancet Global Health, doi:10.1016/S2214-109X(20)30415-0
Tynan, Weidenhofer, Hinwood, Cairns, Day et al., A comparative examination of the antiinflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia, Brain Behav. Immun, doi:10.1016/j.bbi.2011.12.011
Venkatesan, Repurposing drugs for treatment of COVID-19, Lancet Respir. Med, doi:10.1016/S2213-2600(21)00270-8
Wang, Liu, Multilevel determinants of COVID-19 vaccination hesitancy in the United States: a rapid systematic review, Prev. Med. Rep, doi:10.1016/j.pmedr.2021.penalty-@M101673
Wang, Wang, Liu, Qiao, Baldwin et al., Effects of SSRIs on peripheral inflammatory markers in patients with major depressive disorder: a systematic review and meta-analysis, Brain Behav. Immun, doi:10.1016/j.bbi.2019.02.021
Xiao, Wang, Chang, Wang, Dong et al., Identification of potent and safe antiviral therapeutic candidates against SARS-CoV-2, Front. Immunol, doi:10.3389/fimmu.2020.586572
Zimniak, Kirschner, Hilpert, Geiger, Danov et al., The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue, Sci. Rep, doi:10.1038/s41598-021-85049-0
DOI record:
{
"DOI": "10.1016/j.euroneuro.2023.03.011",
"ISSN": [
"0924-977X"
],
"URL": "http://dx.doi.org/10.1016/j.euroneuro.2023.03.011",
"alternative-id": [
"S0924977X23000639"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Repurposing selective serotonin reuptake inhibitors for severity of COVID-19: A population-based study"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "European Neuropsychopharmacology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.euroneuro.2023.03.011"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Author(s). Published by Elsevier B.V."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6466-6213",
"affiliation": [],
"authenticated-orcid": false,
"family": "Visos-Varela",
"given": "Irene",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-0648-7716",
"affiliation": [],
"authenticated-orcid": false,
"family": "Zapata-Cachafeiro",
"given": "Maruxa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3655-100X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Piñeiro-Lamas",
"given": "María",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Carracedo-Martínez",
"given": "Eduardo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saez",
"given": "Marc",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Herdeiro",
"given": "María Teresa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Figueiras",
"given": "Adolfo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Salgado-Barreira",
"given": "Ángel",
"sequence": "additional"
}
],
"container-title": "European Neuropsychopharmacology",
"container-title-short": "European Neuropsychopharmacology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
4,
4
]
],
"date-time": "2023-04-04T07:35:03Z",
"timestamp": 1680593703000
},
"deposited": {
"date-parts": [
[
2023,
4,
26
]
],
"date-time": "2023-04-26T17:11:37Z",
"timestamp": 1682529097000
},
"funder": [
{
"DOI": "10.13039/501100008530",
"doi-asserted-by": "publisher",
"name": "European Regional Development Fund"
},
{
"DOI": "10.13039/501100004587",
"doi-asserted-by": "publisher",
"name": "Instituto de Salud Carlos III"
}
],
"indexed": {
"date-parts": [
[
2023,
4,
27
]
],
"date-time": "2023-04-27T04:47:05Z",
"timestamp": 1682570825909
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
6
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
1
]
],
"date-time": "2023-06-01T00:00:00Z",
"timestamp": 1685577600000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
2
]
],
"date-time": "2023-04-02T00:00:00Z",
"timestamp": 1680393600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0924977X23000639?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0924977X23000639?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "96-108",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
6
]
]
},
"published-print": {
"date-parts": [
[
2023,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)31030-8",
"article-title": "Use of renin–angiotensin–aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study",
"author": "Abajo",
"doi-asserted-by": "crossref",
"first-page": "1705",
"journal-title": "Lancet",
"key": "10.1016/j.euroneuro.2023.03.011_bib0001",
"volume": "395",
"year": "2020"
},
{
"author": "Alsabhan",
"key": "10.1016/j.euroneuro.2023.03.011_bib0002",
"series-title": "New Use of the SSRI Fluvoxamine in the Treatment of COVID-19 Symptoms",
"year": "2022"
},
{
"DOI": "10.3389/fpsyt.2019.00458",
"article-title": "Low-grade inflammation as a predictor of antidepressant and anti-inflammatory therapy response in MDD patients: a systematic review of the literature in combination with an analysis of experimental data collected in the EU-MOODINFLAME consortium",
"author": "Arteaga-Henríquez",
"doi-asserted-by": "crossref",
"first-page": "458",
"journal-title": "Front. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0003",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1097/PSY.0b013e3181f883ce",
"article-title": "Selective serotonin reuptake inhibitor suppression of HIV infectivity and replication",
"author": "Benton",
"doi-asserted-by": "crossref",
"first-page": "925",
"journal-title": "Psychosom. Med.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0004",
"volume": "72",
"year": "2010"
},
{
"DOI": "10.2807/1560-7917.ES.2021.26.50.2101147",
"article-title": "Outbreak caused by the SARS-CoV-2 Omicron variant in Norway, November to December 2021",
"author": "Brandal",
"doi-asserted-by": "crossref",
"journal-title": "Euro. Surveill.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0005",
"volume": "26",
"year": "2021"
},
{
"author": "Brown",
"key": "10.1016/j.euroneuro.2023.03.011_bib0006",
"series-title": "Applied Mixed Models in Medicine",
"year": "2006"
},
{
"DOI": "10.1038/d41586-021-00031-0",
"article-title": "Could new COVID variants undermine vaccines? Labs scramble to find out",
"author": "Callaway",
"doi-asserted-by": "crossref",
"first-page": "177",
"journal-title": "Nature",
"key": "10.1016/j.euroneuro.2023.03.011_bib0007",
"volume": "589",
"year": "2021"
},
{
"DOI": "10.1038/d41586-021-00241-6",
"article-title": "How to redesign COVID vaccines so they protect against variants",
"author": "Callaway",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Nature",
"key": "10.1016/j.euroneuro.2023.03.011_bib0008",
"volume": "590",
"year": "2021"
},
{
"DOI": "10.1111/bcp.15126",
"article-title": "Safety and efficacy of fluvoxamine in COVID-19 ICU patients: an open label, prospective cohort trial with matched controls",
"author": "Calusic",
"doi-asserted-by": "crossref",
"first-page": "2065",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0009",
"volume": "88",
"year": "2022"
},
{
"article-title": "Pharmacological inhibition of acid sphingomyelinase prevents uptake of SARS-CoV-2 by epithelial cells",
"author": "Carpinteiro",
"issue": "8",
"journal-title": "Cell. Rep. Med.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0010",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1001/jama.2021.4367",
"article-title": "CDC interim recommendations for fully vaccinated people: an important first step",
"author": "Christie",
"doi-asserted-by": "crossref",
"first-page": "1501",
"journal-title": "JAMA",
"key": "10.1016/j.euroneuro.2023.03.011_bib0011",
"volume": "325",
"year": "2021"
},
{
"article-title": "Efficacy and safety of selective serotonin reuptake inhibitors in COVID-19 management: a systematic review and meta-analysis",
"author": "Deng",
"journal-title": "Clin. Microbiol. Infect.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0012",
"year": "2023"
},
{
"DOI": "10.1002/hup.470100907",
"article-title": "Comparative safety and tolerability of selective serotonin reuptake inhibitors",
"author": "Devane",
"doi-asserted-by": "crossref",
"first-page": "S185",
"issue": "Suppl 3(S3)",
"journal-title": "Hum. Psychopharmacol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0013",
"volume": "10",
"year": "1995"
},
{
"DOI": "10.1016/j.pbb.2016.02.005",
"article-title": "Effects of escitalopram, R-citalopram, and reboxetine on serum levels of tumor necrosis factor-α, interleukin-10, and depression-like behavior in mice after lipopolysaccharide administration",
"author": "Dong",
"doi-asserted-by": "crossref",
"first-page": "7",
"journal-title": "Pharmacol. Biochem. Behav.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0014",
"volume": "144",
"year": "2016"
},
{
"DOI": "10.1016/j.euroneuro.2022.10.004",
"article-title": "Psychotropic drug repurposing for COVID-19: A systematic review and meta-analysis",
"author": "Fico",
"doi-asserted-by": "crossref",
"first-page": "30",
"journal-title": "Eur. Neuropsychopharmacol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0073",
"volume": "66",
"year": "2023"
},
{
"article-title": "Antidepressant and antipsychotic drugs reduce viral infection by SARS-CoV-2 and fluoxetine shows antiviral activity against the novel variants in vitro",
"author": "Fred",
"journal-title": "Front. Pharmacol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0016",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41398-022-02109-3",
"article-title": "Association between antidepressant use and ED or hospital visits in outpatients with SARS-CoV-2",
"author": "Fritz",
"doi-asserted-by": "crossref",
"first-page": "341",
"issue": "1",
"journal-title": "Transl. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0017",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.biopsych.2015.11.003",
"article-title": "The selective serotonin reuptake inhibitor citalopram decreases human immunodeficiency virus receptor and coreceptor expression in immune cells",
"author": "Greeson",
"doi-asserted-by": "crossref",
"first-page": "33",
"journal-title": "Biol. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0018",
"volume": "80",
"year": "2016"
},
{
"DOI": "10.1007/s00406-020-01231-x",
"article-title": "Repurposing of CNS drugs to treat COVID-19 infection: targeting the sigma-1 receptor",
"author": "Hashimoto",
"doi-asserted-by": "crossref",
"first-page": "249",
"issue": "2",
"journal-title": "Eur. Arch. Psychiatry Clin. Neurosci.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0019",
"volume": "271",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01432-3",
"article-title": "Mechanisms of action of fluvoxamine for COVID-19: a historical review",
"author": "Hashimoto",
"doi-asserted-by": "crossref",
"first-page": "1898",
"issue": "4",
"journal-title": "Mol. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0020",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1093/schbul/sbac118",
"article-title": "Heightened COVID-19 mortality in people with severe mental illness persists after vaccination: a cohort study of greater manchester residents",
"author": "Hassan",
"doi-asserted-by": "crossref",
"first-page": "275",
"issue": "2",
"journal-title": "Schizophr. Bull.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0021",
"volume": "49",
"year": "2023"
},
{
"DOI": "10.1038/s41380-021-01021-4",
"article-title": "Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "5199",
"journal-title": "Mol. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0022",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01254-3",
"article-title": "Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: current evidence and potential mechanisms",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "7098",
"issue": "12",
"journal-title": "Mol. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0023",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1038/s41398-022-01804-5",
"article-title": "Association between FIASMA psychotropic medications and reduced risk of intubation or death in individuals with psychiatric disorders hospitalized for severe COVID-19: an observational multicenter study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "90",
"issue": "1",
"journal-title": "Transl. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0024",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3390/jcm11195882",
"article-title": "Antidepressant use and its association with 28-day mortality in inpatients with SARS-CoV-2: support for the FIASMA model against COVID-19",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "5882",
"issue": "19",
"journal-title": "J. Clin. Med.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0025",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1017/S2045796021000743",
"article-title": "Association between benzodiazepine receptor agonist use and mortality in patients hospitalised for COVID-19: a multicentre observational study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "e18",
"journal-title": "Epidemiol. Psychiatr. Sci.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0026",
"volume": "31",
"year": "2022"
},
{
"DOI": "10.1186/1471-2458-13-1030",
"article-title": "Identifying patients with chronic conditions using pharmacy data in Switzerland: an updated mapping approach to the classification of medications",
"author": "Huber",
"doi-asserted-by": "crossref",
"first-page": "1030",
"journal-title": "BMC Public Health",
"key": "10.1016/j.euroneuro.2023.03.011_bib0027",
"volume": "13",
"year": "2013"
},
{
"DOI": "10.3390/molecules26195795",
"article-title": "Discovery, development, and patent trends on molnupiravir: a prospective oral treatment for COVID-19",
"author": "Imran",
"doi-asserted-by": "crossref",
"first-page": "5795",
"journal-title": "Molecules",
"key": "10.1016/j.euroneuro.2023.03.011_bib0028",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.3390/vaccines10010064",
"article-title": "Large-scale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 infection",
"author": "Israel",
"doi-asserted-by": "crossref",
"first-page": "64",
"journal-title": "Vaccines (Basel)",
"key": "10.1016/j.euroneuro.2023.03.011_bib0029",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01309-5",
"article-title": "The acid sphingomyelinase/ceramide system in COVID-19",
"author": "Kornhuber",
"doi-asserted-by": "crossref",
"first-page": "307",
"issue": "1",
"journal-title": "Mol. Psychiatry",
"key": "10.1016/j.euroneuro.2023.03.011_bib0030",
"volume": "27",
"year": "2022"
},
{
"author": "Kumar",
"key": "10.1016/j.euroneuro.2023.03.011_bib0031",
"series-title": "Sphingolipid Biosynthesis Inhibition as a Host Strategy Against Diverse Pathogens",
"year": "2020"
},
{
"DOI": "10.1038/s41598-022-17082-6",
"article-title": "Robust antiviral activity of commonly prescribed antidepressants against emerging coronaviruses: in vitro and in silico drug repurposing studies",
"author": "Kutkat",
"doi-asserted-by": "crossref",
"first-page": "12920",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0032",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.dhjo.2022.101376",
"article-title": "COVID-19 mortality burden and comorbidity patterns among decedents with and without intellectual and developmental disability in the US",
"author": "Landes",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Disabil. Health J.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0033",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.1155/2015/217047",
"article-title": "Medication adherence measures: an overview",
"author": "Lam",
"doi-asserted-by": "crossref",
"journal-title": "Biomed Res. Int.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0034",
"volume": "2015",
"year": "2015"
},
{
"DOI": "10.1001/jama.2020.22760",
"article-title": "Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial",
"author": "Lenze",
"doi-asserted-by": "crossref",
"first-page": "2292",
"journal-title": "JAMA",
"key": "10.1016/j.euroneuro.2023.03.011_bib0035",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1007/s11481-006-9054-y",
"article-title": "The role of cohort studies in drug development: clinical evidence of antiviral activity of serotonin reuptake inhibitors and HMG-CoA reductase inhibitors in the central nervous system",
"author": "Letendre",
"doi-asserted-by": "crossref",
"first-page": "120",
"journal-title": "J. Neuroimmune Pharmacol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0036",
"volume": "2",
"year": "2007"
},
{
"DOI": "10.3233/JAD-201016",
"article-title": "The impact of dementia on the clinical outcome of COVID-19: a systematic review and meta-analysis",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1775",
"issue": "4",
"journal-title": "J. Alzheimers Dis.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0037",
"volume": "78",
"year": "2020"
},
{
"DOI": "10.1016/j.jiph.2022.10.010",
"article-title": "Effect of fluvoxamine on outcomes of nonhospitalized patients with COVID-19: a systematic review and meta-analysis",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "1259",
"issue": "11",
"journal-title": "J. Infect. Public Health",
"key": "10.1016/j.euroneuro.2023.03.011_bib0038",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.1136/postgradmedj-2020-138903",
"article-title": "Will vaccination refusal prolong the war on SARS-CoV-2?",
"author": "Marcec",
"doi-asserted-by": "crossref",
"first-page": "143",
"journal-title": "Postgrad. Med. J.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0039",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.1002/npr2.12194",
"article-title": "SSRIs: applications in inflammatory lung disease and implications for COVID-19",
"author": "Meikle",
"doi-asserted-by": "crossref",
"first-page": "325",
"journal-title": "Neuropsychopharmacol. Rep.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0040",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(22)00327-0",
"article-title": "Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study",
"author": "Menni",
"doi-asserted-by": "crossref",
"first-page": "1618",
"journal-title": "Lancet",
"key": "10.1016/j.euroneuro.2023.03.011_bib0041",
"volume": "399",
"year": "2022"
},
{
"author": "Nakhaee",
"key": "10.1016/j.euroneuro.2023.03.011_bib0042",
"series-title": "The Effect of Antidepressants on Severity of COVID-19 in Hospitalized Patients: A Systematic Review and Meta-Analysis",
"year": "2022"
},
{
"DOI": "10.1016/j.pbb.2012.12.003",
"article-title": "Effects of antidepressants on alternations in serum cytokines and depressive-like behavior in mice after lipopolysaccharide administration",
"author": "Ohgi",
"doi-asserted-by": "crossref",
"first-page": "853",
"issue": "4",
"journal-title": "Pharmacol. Biochem. Behav.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0043",
"volume": "103",
"year": "2013"
},
{
"DOI": "10.1016/j.jocn.2021.03.010",
"article-title": "Drug repurposing of selective serotonin reuptake inhibitors: could these drugs help fight COVID-19 and save lives?",
"author": "Pashaei",
"doi-asserted-by": "crossref",
"first-page": "163",
"journal-title": "J. Clin. Neurosci.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0044",
"volume": "88",
"year": "2021"
},
{
"author": "Pinheiro",
"key": "10.1016/j.euroneuro.2023.03.011_bib0045",
"series-title": "Mixed-Effects Models in S and S-PLUS",
"year": "2000"
},
{
"DOI": "10.1038/s41586-021-03777-9",
"article-title": "Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization",
"author": "Planas",
"doi-asserted-by": "crossref",
"first-page": "276",
"journal-title": "Nature",
"key": "10.1016/j.euroneuro.2023.03.011_bib0046",
"volume": "596",
"year": "2021"
},
{
"DOI": "10.1016/j.vaccine.2017.06.003",
"article-title": "The complexity and cost of vaccine manufacturing—an overview",
"author": "Plotkin",
"doi-asserted-by": "crossref",
"first-page": "4064",
"journal-title": "Vaccine",
"key": "10.1016/j.euroneuro.2023.03.011_bib0047",
"volume": "35",
"year": "2017"
},
{
"DOI": "10.1016/j.crstbi.2020.12.001",
"article-title": "Dual targeting of 3CLpro and PLpro of SARS-CoV-2: a novel structure-based design approach to treat COVID-19",
"author": "Rajpoot",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Curr. Res. Struct. Biol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0048",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.3390/jcm11010070",
"article-title": "Ongoing use of SSRIs does not alter outcome in hospitalized COVID-19 patients: a retrospective analysis",
"author": "Rauchman",
"doi-asserted-by": "crossref",
"first-page": "70",
"issue": "1",
"journal-title": "J. Clin. Med.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0049",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/S2214-109X(21)00448-4",
"article-title": "Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "Lancet Global Health",
"key": "10.1016/j.euroneuro.2023.03.011_bib0050",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1001/jama.2022.9655",
"article-title": "COVID-19 in 2022—the beginning of the end or the end of the beginning?",
"author": "del Rio",
"doi-asserted-by": "crossref",
"first-page": "2389",
"journal-title": "JAMA",
"key": "10.1016/j.euroneuro.2023.03.011_bib0051",
"volume": "327",
"year": "2022"
},
{
"article-title": "Why match? Investigating matched case-control study designs with causal effect estimation",
"author": "Rose",
"first-page": "1",
"journal-title": "Int. J. Biostat.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0052",
"volume": "5",
"year": "2009"
},
{
"article-title": "Case–control studies",
"author": "Rothman",
"key": "10.1016/j.euroneuro.2023.03.011_bib0053",
"series-title": "Encyclopedia of Quantitative Risk Analysis and Assessment",
"year": "2008"
},
{
"DOI": "10.1016/S0140-6736(22)01585-9",
"article-title": "The Lancet Commission on lessons for the future from the COVID-19 pandemic",
"author": "Sachs",
"doi-asserted-by": "crossref",
"first-page": "1224",
"issue": "10359",
"journal-title": "Lancet",
"key": "10.1016/j.euroneuro.2023.03.011_bib0054",
"volume": "400",
"year": "2022"
},
{
"DOI": "10.1002/art.27304",
"article-title": "Fluoxetine and citalopram exhibit potent antiinflammatory activity in human and murine models of rheumatoid arthritis and inhibit toll-like receptors",
"author": "Sacre",
"doi-asserted-by": "crossref",
"first-page": "683",
"journal-title": "Arthritis Rheum.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0055",
"volume": "62",
"year": "2010"
},
{
"DOI": "10.1136/bmjgh-2021-007031",
"article-title": "New waves, new variants, old inequity: a continuing COVID-19 crisis",
"author": "Saha",
"doi-asserted-by": "crossref",
"journal-title": "BMJ Global Health",
"key": "10.1016/j.euroneuro.2023.03.011_bib0056",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1093/ofid/ofab050",
"article-title": "Prospective cohort of fluvoxamine for early treatment of coronavirus disease 19",
"author": "Seftel",
"doi-asserted-by": "crossref",
"first-page": "ofab050",
"journal-title": "Open Forum Infect. Dis.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0057",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1056/NEJMsb1609216",
"article-title": "Real-world evidence—what is it and what can it tell us?",
"author": "Sherman",
"doi-asserted-by": "crossref",
"first-page": "2293",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0058",
"volume": "375",
"year": "2016"
},
{
"DOI": "10.1016/S0140-6736(21)01642-1",
"article-title": "Spike-antibody waning after second dose of BNT162b2 or ChAdOx1",
"author": "Shrotri",
"doi-asserted-by": "crossref",
"first-page": "385",
"journal-title": "Lancet",
"key": "10.1016/j.euroneuro.2023.03.011_bib0059",
"volume": "398",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(11)60478-9",
"article-title": "Vaccine production, distribution, access, and uptake",
"author": "Smith",
"doi-asserted-by": "crossref",
"first-page": "428",
"journal-title": "Lancet",
"key": "10.1016/j.euroneuro.2023.03.011_bib0060",
"volume": "378",
"year": "2011"
},
{
"author": "Stroup",
"key": "10.1016/j.euroneuro.2023.03.011_bib0061",
"series-title": "Generalized Linear Mixed Models: Modern Concepts, Methods and Applications. 1a",
"year": "2021"
},
{
"DOI": "10.3389/fphar.2021.652688",
"article-title": "Fluvoxamine: a review of its mechanism of action and its role in COVID-19",
"author": "Sukhatme",
"doi-asserted-by": "crossref",
"journal-title": "Front. Pharmacol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0062",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1097/PRA.0000000000000578",
"article-title": "Selective serotonin reuptake inhibitors: how long is long enough?",
"author": "Thom",
"doi-asserted-by": "crossref",
"first-page": "361",
"journal-title": "J. Psychiatr. Pract.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0063",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/S2214-109X(20)30415-0",
"article-title": "COVID-19 vaccination: returning to WHO's health for all",
"author": "Torres",
"doi-asserted-by": "crossref",
"first-page": "e1355",
"journal-title": "Lancet Global Health",
"key": "10.1016/j.euroneuro.2023.03.011_bib0064",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2011.12.011",
"article-title": "A comparative examination of the anti-inflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia",
"author": "Tynan",
"doi-asserted-by": "crossref",
"first-page": "469",
"issue": "3",
"journal-title": "Brain Behav. Immun.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0065",
"volume": "26",
"year": "2012"
},
{
"DOI": "10.1016/S2213-2600(21)00270-8",
"article-title": "Repurposing drugs for treatment of COVID-19",
"author": "Venkatesan",
"doi-asserted-by": "crossref",
"first-page": "e63",
"journal-title": "Lancet Respir. Med.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0066",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2019.02.021",
"article-title": "Effects of SSRIs on peripheral inflammatory markers in patients with major depressive disorder: a systematic review and meta-analysis",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "24",
"journal-title": "Brain Behav. Immun.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0067",
"volume": "79",
"year": "2019"
},
{
"article-title": "Multilevel determinants of COVID-19 vaccination hesitancy in the United States: a rapid systematic review",
"author": "Wang",
"journal-title": "Prev. Med. Rep.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0068",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2023184",
"article-title": "Repurposed antiviral drugs for Covid-19—interim WHO solidarity trial results",
"author": "Solidarity Trial Consortium",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0069",
"volume": "384",
"year": "2021"
},
{
"key": "10.1016/j.euroneuro.2023.03.011_bib0070",
"series-title": "Therapeutics and COVID-19: Living Guideline",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2020.586572",
"article-title": "Identification of potent and safe antiviral therapeutic candidates against SARS-CoV-2",
"author": "Xiao",
"doi-asserted-by": "crossref",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0071",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-85049-0",
"article-title": "The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue",
"author": "Zimniak",
"doi-asserted-by": "crossref",
"first-page": "5890",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.euroneuro.2023.03.011_bib0072",
"volume": "11",
"year": "2021"
}
],
"reference-count": 72,
"references-count": 72,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0924977X23000639"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Biological Psychiatry",
"Psychiatry and Mental health",
"Neurology (clinical)",
"Neurology",
"Pharmacology"
],
"subtitle": [],
"title": "Repurposing selective serotonin reuptake inhibitors for severity of COVID-19: A population-based study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "71"
}
