Effectiveness of Sotrovimab and Molnupiravir in community settings in England across the Omicron BA.1 and BA.2 sublineages: emulated target trials using the OpenSAFELY platform
et al., medRxiv, doi:10.1101/2023.05.12.23289914, May 2023
Sotrovimab for COVID-19
45th treatment shown to reduce risk in
August 2022, now with p = 0.00048 from 29 studies, recognized in 42 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
OpenSAFELY retrospective 75,048 outpatients in the UK, using the clone-censor-weight approach to address immortal time bias, showing lower combined mortality/hospitalization with sotrovimab treatment.
Efficacy is variant dependent. In Vitro studies predict lower efficacy for BA.11-3, BA.4, BA.54, XBB.1.9.3, XBB.1.5.24, XBB.2.9, CH.1.15, and no efficacy for BA.26, XBB, XBB.1.5, ХВВ.1.9.17, XBB.1.16, BQ.1.1.45, and CL.15. US EUA has been revoked.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments8.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
Study covers molnupiravir and sotrovimab.
|
risk of death/hospitalization, 16.0% lower, HR 0.84, p = 0.002, treatment 6,408, control 65,568.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Liu et al., Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2, bioRxiv, doi:10.1101/2021.12.14.472719.
2.
Sheward et al., Variable loss of antibody potency against SARS-CoV-2 B.1.1.529 (Omicron), bioRxiv, doi:10.1101/2021.12.19.473354.
3.
VanBlargan et al., An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by several therapeutic monoclonal antibodies, bioRxiv, doi:10.1101/2021.12.15.472828.
4.
Haars et al., Prevalence of SARS-CoV-2 Omicron Sublineages and Spike Protein Mutations Conferring Resistance against Monoclonal Antibodies in a Swedish Cohort during 2022–2023, Microorganisms, doi:10.3390/microorganisms11102417.
5.
Pochtovyi et al., In Vitro Efficacy of Antivirals and Monoclonal Antibodies against SARS-CoV-2 Omicron Lineages XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1, Vaccines, doi:10.3390/vaccines11101533.
6.
Zhou et al., SARS-CoV-2 Omicron BA.2 Variant Evades Neutralization by Therapeutic Monoclonal Antibodies, bioRxiv, doi:10.1101/2022.02.15.480166.
Tazare et al., 16 May 2023, retrospective, United Kingdom, preprint, 31 authors, study period 16 December, 2021 - 21 May, 2022.
Effectiveness of Sotrovimab and Molnupiravir in community settings in England across the Omicron BA.1 and BA.2 sublineages: emulated target trials using the OpenSAFELY platform
doi:10.1101/2023.05.12.23289914
Background The effectiveness of COVID-19 monoclonal antibody and antiviral therapies against severe COVID-19 outcomes is unclear. Initial benefit was shown in unvaccinated patients and before the Omicron variant emerged. We used the OpenSAFELY platform to emulate target trials to estimate the effectiveness of sotrovimab or molnupiravir, versus no treatment.
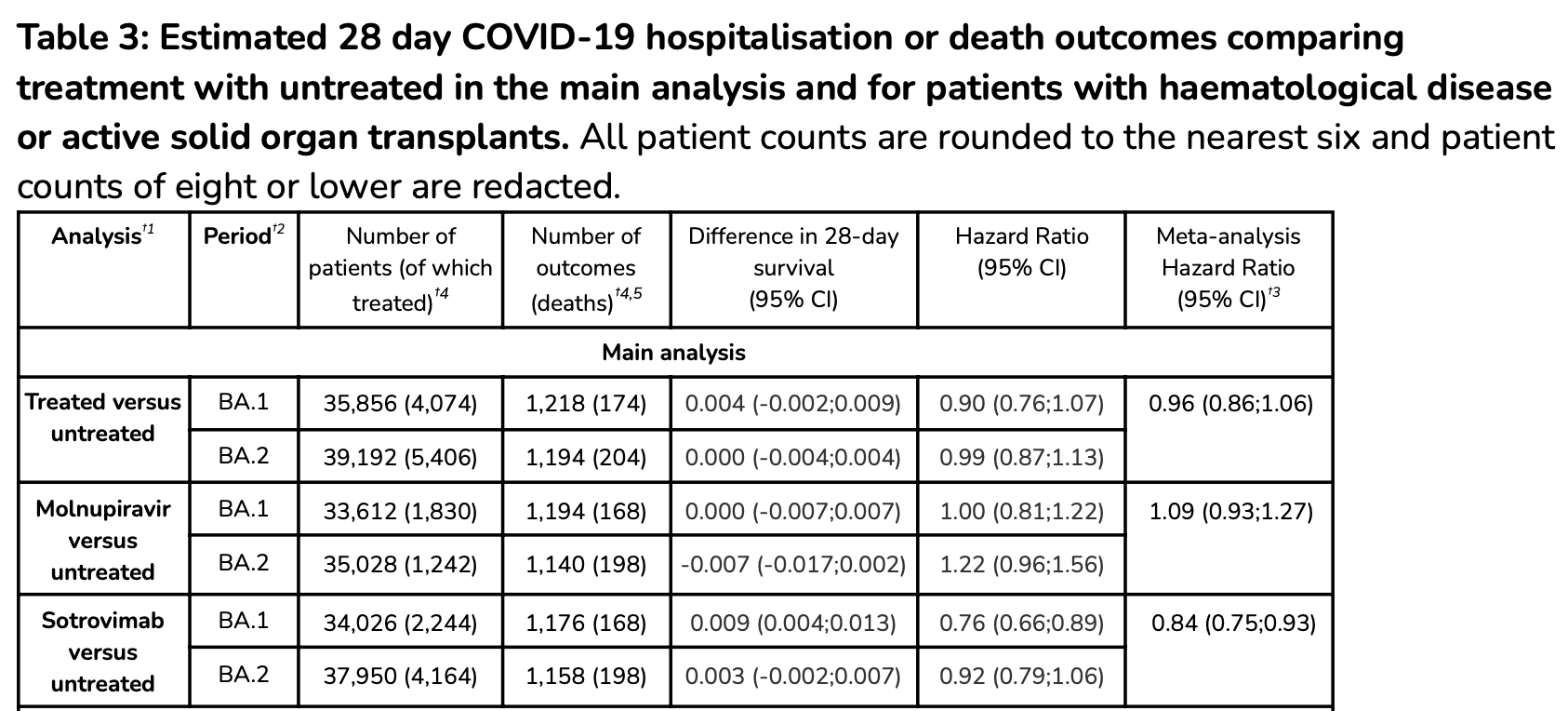
Methods With the approval of NHS England, we derived population-based cohorts of non-hospitalised high-risk individuals in England testing positive for SARS-CoV-2 during periods of dominance of the BA.1 (16/12/2021-10/02/2022) and BA.2 (11/02/2022-21/05/2022) Omicron sublineages. We used the clone-censor-weight approach to estimate the effect of treatment with sotrovimab or molnupiravir initiated within 5 days after positive test versus no treatment. Hazard ratios (HR) for COVID-19 hospitalisation or death within 28 days were estimated using weighted Cox models.
Results
Of the 35,856 [BA.1 period] and 39,192 [BA.2 period] patients, 1,830 [BA.1] and 1,242 [BA.2] were treated with molnupiravir and 2,244 [BA.1] and 4,164 [BA.2] with sotrovimab. The estimated HRs for molnupiravir versus untreated were 1.00 (95%CI: 0.81;1.22) [BA.1] and 1.22 (0.96;1.56) [BA.2]; corresponding HRs for sotrovimab versus untreated were 0.76 (0.66;0.89) [BA.1] and 0.92 (0.79;1.06) [BA.2].
Interpretation Compared with no treatment, sotrovimab was associated with reduced risk of adverse outcomes after COVID-19 in the BA.1 period, but there was weaker evidence of benefit in the BA2 period. Molnupiravir was not associated with reduced risk in either period.
Authors' contributors The study was conceptualised by LAT, IJD, JACS, JT, LN, BZ, SJWE, BG and BMK; data was curated by LN, JT, BZ, ACAG, HJC, RH, RMS, CB, JC, JP, FH and SH; and formally analysed by LN and JT; funding was acquired by BG; the investigation was done by LN and JT; to the methodology was contributed by JT, LN, JACS, LAT, IJD, BZ, WJH, AS, CM, C; project administration was done by JT, LN, AJW, BMK, LAT and IJD; resources were provided by AM, AJW, BG, BMK and LAT; software was developed by LN, JT, ACAG, HJC, RH and RMS; the project was supervised by IJD and LAT; the study was validated by JT, LN, BZ, WJH, ACAG, HJC and RH; the results were visualised by JT and LN; the original draft was written by JT, LN and LAT; all authors were involved in draft revisions and approving the final draft for submission; all authors had full access to the OpenSAFELY platform and accept responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. Bennett Institute for Applied Data Science developers and principal investigators (WJH, RMS, AJW and BG) holding contracts with NHS England have access to the OpenSAFELY pseudonymised data tables as needed to develop the OpenSAFELY tools; these tools in turn enable researchers with OpenSAFELY Data Access Agreements to write and execute code for data management and data analysis (LN and JT) without direct..
References
Aggarwal, Beaty, Bennett, Change in effectiveness of sotrovimab for preventing hospitalization and mortality for at-risk COVID-19 outpatients during an Omicron BA.1 and BA.1.1-predominant phase, Int J Infect Dis IJID Off Publ Int Soc Infect Dis, doi:10.1016/j.ijid.2022.10.002
Aggarwal, Beaty, Bennett, Real-World Evidence of the Neutralizing Monoclonal Antibody Sotrovimab for Preventing Hospitalization and Mortality in COVID-19 Outpatients, J Infect Dis, doi:10.1093/infdis/jiac206
Bajema, Berry, Streja, Effectiveness of COVID-19 treatment with nirmatrelvir-ritonavir or molnupiravir among U.S. Veterans: target trial emulation studies with one-month and six-month outcomes, MedRxiv Prepr Serv Health Sci. Published online December, doi:10.1101/2022.12.05.22283134
Bernal, Da Silva, Musungaie, Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients, N Engl J Med, doi:10.1056/NEJMoa2116044
Blake, Leyrat, Mansfield, Propensity scores using missingness pattern information: a practical guide, Stat Med, doi:10.1002/sim.8503
Borenstein, Hedges, Higgins, Hr, A basic introduction to fixed-effect and random-effects models for meta-analysis, Res Synth Methods, doi:10.1002/jrsm.12
Brophy, Molnupiravir's authorisation was premature, BMJ, doi:10.1136/bmj.o443
Brown, Saund, Qureshi, Demographics and Outcomes of Initial Phase of COVID-19 Medicines Delivery Units Across 4 UK Centers During Peak B1.1.529 Omicron Epidemic: A Service Evaluation, Open Forum Infect Dis, doi:10.1093/ofid/ofac527
Butler, Hobbs, Gbinigie, Molnupiravir plus usual care versus usual care alone as early treatment for adults with COVID-19 at increased risk of adverse outcomes (PANORAMIC): an open-label, platform-adaptive randomised controlled trial, The Lancet, doi:10.1016/S0140-6736(22)02597-1
Cheng, Reyes, Satram, Real-World Effectiveness of Sotrovimab for the Early Treatment of COVID-19 During SARS-CoV-2 Delta and Omicron Waves in the USA, Infect Dis Ther, doi:10.1007/s40121-022-00755-0
England, Coronavirus, Interim clinical commissioning policy: Treatments for non-hospitalised patients with COVID-19
Fda, FDA updates Sotrovimab emergency use authorization
Green, Curtis, Higgins, Trends, variation, and clinical characteristics of recipients of antiviral drugs and neutralising monoclonal antibodies for covid-19 in community settings: retrospective, descriptive cohort study of 23.4 million people in OpenSAFELY, BMJ Med, doi:10.1136/bmjmed-2022-000276
Gupta, Gonzalez-Rojas, Juarez, Early Treatment for Covid-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab, N Engl J Med, doi:10.1056/NEJMoa2107934
Hernán, How to estimate the effect of treatment duration on survival outcomes using observational data, BMJ, doi:10.1136/bmj.k182
Hernán, Robins, Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available, Am J Epidemiol, doi:10.1093/aje/kwv254
Hernán, Sauer, Hernández-Díaz, Platt, Shrier, Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses, J Clin Epidemiol, doi:10.1016/j.jclinepi.2016.04.014
Hernán, The Hazards of Hazard Ratios, Epidemiol Camb Mass, doi:10.1097/EDE.0b013e3181c1ea43
Lamontagne, Agarwal, Rochwerg, A living WHO guideline on drugs for covid-19, BMJ, doi:10.1136/bmj.m3379
Lund, Richardson, Stürmer, The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application, Curr Epidemiol Rep, doi:10.1007/s40471-015-0053-5
Maringe, Benitez Majano, Exarchakou, Assessing the benefit of major surgery for elderly lung cancer patients using observational data, Int J Epidemiol, doi:10.1093/ije/dyaa057
Nab, Parker, Andrews, Changes in COVID-19-related mortality across key demographic and clinical subgroups in England from 2020 to 2022: a retrospective cohort study using the OpenSAFELY platform, Lancet Public Health, doi:10.1016/S2468-2667(23)00079-8
Nice, NICE recommends 3 treatments for COVID-19 in final draft guidance
Piccicacco, Zeitler, Ing, Real-world effectiveness of early remdesivir and sotrovimab in the highest-risk COVID-19 outpatients during the Omicron surge, J Antimicrob Chemother, doi:10.1093/jac/dkac256
Schneeweiss, Avorn, A review of uses of health care utilization databases for epidemiologic research on therapeutics, J Clin Epidemiol, doi:10.1016/j.jclinepi.2004.10.012
Schneeweiss, Patrick, Stürmer, Increasing levels of restriction in pharmacoepidemiologic database studies of elderly and comparison with randomized trial results, Med Care, doi:10.1097/MLR.0b013e318070c08e
Stürmer, Wang, Golightly, Keil, Lund et al., Methodological considerations when analysing and interpreting real-world data, Rheumatol Oxf Engl, doi:10.1093/rheumatology/kez320
Suissa, Immortal Time Bias in Pharmacoepidemiology, Am J Epidemiol, doi:10.1093/aje/kwm324
Vanderweele, Unmeasured confounding and hazard scales: sensitivity analysis for total, direct, and indirect effects, Eur J Epidemiol, doi:10.1007/s10654-013-9770-6
Who, Therapeutics and COVID-19: Living guideline
Wu, Carr, Harvey, WHO's Therapeutics and COVID-19 Living Guideline on mAbs needs to be reassessed, The Lancet, doi:10.1016/S0140-6736(22)01938-9
Xie, Bowe, Al-Aly, Molnupiravir and risk of hospital admission or death in adults with covid-19: emulation of a randomized target trial using electronic health records, BMJ, doi:10.1136/bmj-2022-072705
Zaqout, Almaslamani, Chemaitelly, Effectiveness of the neutralizing antibody sotrovimab among high-risk patients with mild-to-moderate SARS-CoV-2 in Qatar, Int J Infect Dis IJID Off Publ Int Soc Infect Dis, doi:10.1016/j.ijid.2022.09.023
Zheng, Green, Tazare, Comparative effectiveness of sotrovimab and molnupiravir for prevention of severe covid-19 outcomes in patients in the community: observational cohort study with the OpenSAFELY platform, BMJ, doi:10.1136/bmj-2022-071932
DOI record:
{
"DOI": "10.1101/2023.05.12.23289914",
"URL": "http://dx.doi.org/10.1101/2023.05.12.23289914",
"abstract": "<jats:p>Background The effectiveness of COVID-19 monoclonal antibody and antiviral therapies against severe COVID-19 outcomes is unclear. Initial benefit was shown in unvaccinated patients and before the Omicron variant emerged. We used the OpenSAFELY platform to emulate target trials to estimate the effectiveness of sotrovimab or molnupiravir, versus no treatment. Methods With the approval of NHS England, we derived population-based cohorts of non-hospitalised high-risk individuals in England testing positive for SARS-CoV-2 during periods of dominance of the BA.1 (16/12/2021-10/02/2022) and BA.2 (11/02/2022-21/05/2022) Omicron sublineages. We used the clone-censor-weight approach to estimate the effect of treatment with sotrovimab or molnupiravir initiated within 5 days after positive test versus no treatment. Hazard ratios (HR) for COVID-19 hospitalisation or death within 28 days were estimated using weighted Cox models. Results Of the 35,856 [BA.1 period] and 39,192 [BA.2 period] patients, 1,830 [BA.1] and 1,242 [BA.2] were treated with molnupiravir and 2,244 [BA.1] and 4,164 [BA.2] with sotrovimab. The estimated HRs for molnupiravir versus untreated were 1.00 (95%CI: 0.81;1.22) [BA.1] and 1.22 (0.96;1.56) [BA.2]; corresponding HRs for sotrovimab versus untreated were 0.76 (0.66;0.89) [BA.1] and 0.92 (0.79;1.06) [BA.2]. Interpretation Compared with no treatment, sotrovimab was associated with reduced risk of adverse outcomes after COVID-19 in the BA.1 period, but there was weaker evidence of benefit in the BA2 period. Molnupiravir was not associated with reduced risk in either period.</jats:p>",
"accepted": {
"date-parts": [
[
2023,
5,
16
]
]
},
"author": [
{
"affiliation": [],
"name": "The OpenSAFELY Collaborative",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-7194-2615",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tazare",
"given": "John",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1821-7246",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nab",
"given": "Linda",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1814-6692",
"affiliation": [],
"authenticated-orcid": false,
"family": "Zheng",
"given": "Bang",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9162-4999",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hulme",
"given": "William J",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7246-2074",
"affiliation": [],
"authenticated-orcid": false,
"family": "Green",
"given": "Amelia CA",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3429-9576",
"affiliation": [],
"authenticated-orcid": false,
"family": "Curtis",
"given": "Helen J",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3157-1127",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mahalingasivam",
"given": "Viyaasan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5295-4370",
"affiliation": [],
"authenticated-orcid": false,
"family": "Higgins",
"given": "Rose",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1637-837X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Schultze",
"given": "Anna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5364-8757",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bhaskaran",
"given": "Krishnan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2098-1278",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mehrkar",
"given": "Amir",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3701-4997",
"affiliation": [],
"authenticated-orcid": false,
"family": "Schaffer",
"given": "Andrea L",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith",
"given": "Rebecca M",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0113-2593",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bates",
"given": "Christopher",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4681-4873",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cockburn",
"given": "Jonathan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Parry",
"given": "John",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hester",
"given": "Frank",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Harper",
"given": "Sam",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0362-6717",
"affiliation": [],
"authenticated-orcid": false,
"family": "Eggo",
"given": "Rosalind M",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4932-6135",
"affiliation": [],
"authenticated-orcid": false,
"family": "Walker",
"given": "Alex J",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7585-4743",
"affiliation": [],
"authenticated-orcid": false,
"family": "Marks",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brown",
"given": "Michael",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8739-9565",
"affiliation": [],
"authenticated-orcid": false,
"family": "Maringe",
"given": "Camille",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4097-4577",
"affiliation": [],
"authenticated-orcid": false,
"family": "Leyrat",
"given": "Clemence",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1474-2596",
"affiliation": [],
"authenticated-orcid": false,
"family": "Evans",
"given": "Stephen JW",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5127-4728",
"affiliation": [],
"authenticated-orcid": false,
"family": "Goldacre",
"given": "Ben",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3786-9063",
"affiliation": [],
"authenticated-orcid": false,
"family": "MacKenna",
"given": "Brian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8496-6053",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sterne",
"given": "Jonathan AC",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8848-9493",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tomlinson",
"given": "Laurie A",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8970-1406",
"affiliation": [],
"authenticated-orcid": false,
"family": "Douglas",
"given": "Ian J",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
5,
16
]
],
"date-time": "2023-05-16T21:15:21Z",
"timestamp": 1684271721000
},
"deposited": {
"date-parts": [
[
2023,
5,
16
]
],
"date-time": "2023-05-16T21:15:21Z",
"timestamp": 1684271721000
},
"group-title": "Epidemiology",
"indexed": {
"date-parts": [
[
2023,
5,
17
]
],
"date-time": "2023-05-17T04:55:30Z",
"timestamp": 1684299330035
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
5,
16
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2023.05.12.23289914",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2023,
5,
16
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2023,
5,
16
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2023.05.12.23289914"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Effectiveness of Sotrovimab and Molnupiravir in community settings in England across the Omicron BA.1 and BA.2 sublineages: emulated target trials using the OpenSAFELY platform",
"type": "posted-content"
}
tazare
