Hospital Outcomes in Patients Hospitalized for COVID-19 Pneumonia: The Effect of SARS-CoV-2 Vaccination and Vitamin D Status
et al., Nutrients, doi:10.3390/nu15132976, Jun 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
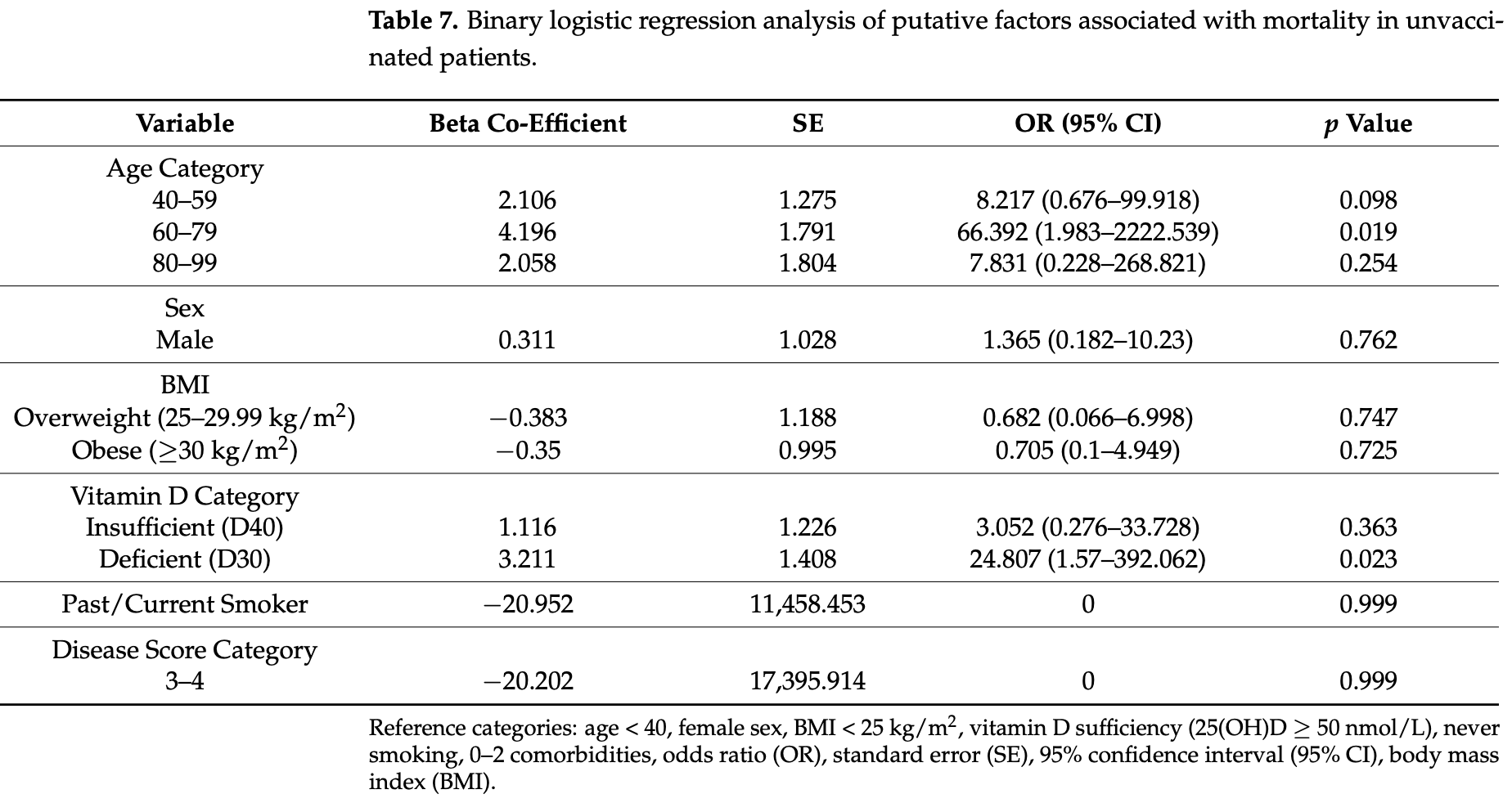
Prospective study of 171 hospitalized COVID-19 patients in Ireland, showing significantly lower mortality and ICU admission with sufficient vitamin D levels among unvaccinated patients. There were no significant differences for vaccinated patients. Authors note that high vitamin D levels or recent vaccination were associated with lower mortality. Adjusted results are only reported for unvaccinated patients and mortality/ICU admission, where results were significant. More vaccinated patients had sufficient vitamin D levels despite the group being older (mean age 69 vs. 46). There may be a link based on health conscientiousness between vaccination, vitamin D supplementation, and other measures and lifestyle factors that reduce risk.
|
risk of death, 94.9% lower, RR 0.05, p = 0.03, high D levels (≥50nmol/L) 1 of 39 (2.6%), low D levels (<30nmol/L) 4 of 18 (22.2%), NNT 5.1, adjusted per study, inverted to make RR<1 favor high D levels (≥50nmol/L), odds ratio converted to relative risk, unvaccinated patients, multivariable.
|
|
risk of ICU admission, 80.9% lower, RR 0.19, p = 0.05, high D levels (≥50nmol/L) 3 of 39 (7.7%), low D levels (<30nmol/L) 5 of 18 (27.8%), NNT 5.0, adjusted per study, inverted to make RR<1 favor high D levels (≥50nmol/L), odds ratio converted to relative risk, unvaccinated patients, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sanecka et al., 30 Jun 2023, prospective, Ireland, peer-reviewed, 16 authors, study period June 2021 - December 2021.
Contact: johnfaul@rsci.ie (corresponding author), martynasanecka@gmail.com, daniel.mccartney@tudublin.ie.
Hospital Outcomes in Patients Hospitalized for COVID-19 Pneumonia: The Effect of SARS-CoV-2 Vaccination and Vitamin D Status
Nutrients, doi:10.3390/nu15132976
SARS-CoV-2 vaccination promises to improve outcomes for patients with COVID-19 pneumonia (most notably those with advanced age and at high risk for severe disease). Here, we examine serum 25-Hydroxyvitamin D (25(OH)D) status and outcomes in both old (>70 years) and young vaccinated (n = 80) and unvaccinated (n = 91) subjects, who were hospitalized due to COVID-19 pneumonia in a single center (Connolly Hospital Dublin). Outcomes included ICU admission and mortality. Serum 25(OH)D levels were categorized as D30 (<30 nmol/L), D40 (30-49.99 nmol/L) and D50 (≥50 nmol/L). In multivariate analyses, D30 was independently associated with ICU admission (OR: 6.87 (95% CI: 1.13-41.85) (p = 0.036)) and mortality (OR: 24.81 (95% CI: 1.57-392.1) (p = 0.023)) in unvaccinated patients, even after adjustment for major confounders including age, sex, obesity and pre-existing diabetes mellitus. While mortality was consistently higher in all categories of patients over 70 years of age, the highest observed mortality rate of 50%, seen in patients over 70 years with a low vitamin D state (D30), appeared to be almost completely corrected by either vaccination, or having a higher vitamin D state, i.e., mortality was 14% for vaccinated patients over 70 years with D30 and 16% for unvaccinated patients over 70 years with a 25(OH)D level greater than 30 nmol/L. We observe that high mortality from COVID-19 pneumonia occurs in older patients, especially those who are unvaccinated or have a low vitamin D state. Recent vaccination or having a high vitamin D status are both associated with reduced mortality, although these effects do not fully mitigate the mortality risk associated with advanced age.
Author Contributions: M.S., data processing, data analysis, data interpretation, manuscript drafts; J.L.F. and D.M.A.M., study design, data interpretation, manuscript drafts, data analysis; M.Y., M.A., S.F.R., A.Q., J.I., A.A., S.I.S., J.F., W.P.T., E.O., L.J.C., E.P.J. and A.A.L. data collection, processing, analysis and interpretation; J.L.F., study design, data collection, processing, analysis and interpretation, manuscript drafts. All authors have read and agreed to the published version of the manuscript. Funding: This research received no external funding.
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Connolly Hospital Dublin. Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflict of interest.
References
Andrews, Stowe, Kirsebom, Toffa, Rickeard et al., COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant, N. Engl. J. Med, doi:10.1056/NEJMoa2119451
Angelidi, Belanger, Lorinsky, Karamanis, Chamorro-Pareja et al., Vitamin D Status Is Associated with In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients, Mayo Clin. Proc, doi:10.1016/j.mayocp.2021.01.001
Aranow, Vitamin D and the immune system, J. Investig. Med, doi:10.2310/JIM.0b013e31821b8755
Argano, Mallaci Bocchio, Natoli, Scibetta, Lo Monaco et al., Protective Effect of Vitamin D Supplementation on COVID-19-Related Intensive Care Hospitalization and Mortality: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis, Pharmaceuticals, doi:10.3390/ph16010130
Barrett, Youssef, Shah, Ioana, Lawati et al., Vitamin D Status and Mortality from SARS CoV-2: A Prospective Study of Unvaccinated Caucasian Adults, Nutrients, doi:10.3390/nu14163252
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., Mechanisms In Endocrinology: Vitamin D and COVID-19, doi:10.1530/EJE-20-0665
Borsche, Glauner, Von Mendel, COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu13103596
Cashman, Dowling, Škrabáková, Gonzalez-Gross, Valtueña et al., Vitamin D deficiency in Europe: Pandemic?, Am. J. Clin. Nutr, doi:10.3945/ajcn.115.120873
Chauss, Freiwald, Mcgregor, Yan, Wang et al., Autocrine vitamin D signaling switches off pro-inflammatory programs of T H 1 cells, Nat. Immunol, doi:10.1038/s41590-021-01080-3
Chen, Mei, Xie, Yuan, Ma et al., Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs, Nutr. J, doi:10.1186/s12937-021-00744-y
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front. Public Health, doi:10.3389/fpubh.2021.736665
Chiu, Tsai, Wu, Zheng, Yang et al., Putative Role of Vitamin D for COVID-19 Vaccination, Int. J. Mol. Sci, doi:10.3390/ijms22168988
D'ecclesiis, Gavioli, Martinoli, Raimondi, Chiocca et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0268396
Dror, Morozov, Daoud, Namir, Yakir et al., Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness, PLoS ONE, doi:10.1371/journal.pone.0263069
Griffin, Haddix, Danza, Fisher, Koo et al., SARS-CoV-2 Infections and Hospitalizations among Persons Aged ≥16 Years, by Vaccination Status, Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm7034e5
Hall, Foulkes, Insalata, Kirwan, Saei et al., Protection against SARS-CoV-2 after COVID-19 Vaccination and Previous Infection, N. Engl. J. Med, doi:10.1056/NEJMoa2118691
Hanna, Dalvi, Sălăgean, Pop, Bordea et al., Understanding COVID-19 Pandemic: Molecular Mechanisms and Potential Therapeutic Strategies. An Evidence-Based Review, J. Inflamm. Res, doi:10.2147/JIR.S282213
Hariyanto, Intan, Hananto, Harapan, Kurniawan, Vitamin D supplementation and COVID-19 outcomes: A systematic review, meta-analysis and meta-regression, Rev. Med. Virol, doi:10.1002/rmv.2269
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci. Rep, doi:10.1038/s41598-020-77093-z
Jeong, Vacanti, Disclaimer/Publisher's Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, Nutr. Metab, doi:10.1186/s12986-020-00491-7
Jolliffe, Vivaldi, Chambers, Cai, Li et al., Vitamin D Supplementation Does Not Influence SARS-CoV-2 Vaccine Efficacy or Immunogenicity: Sub-Studies Nested within the CORONAVIT Randomised Controlled Trial, Nutrients, doi:10.3390/nu14183821
Lamacchia, Mazzoni, Spinicci, Vanni, Salvati et al., Clinical and Immunological Features of SARS-CoV-2 Breakthrough Infections in Vaccinated Individuals Requiring Hospitalization, J. Clin. Immunol. 2022, doi:10.1007/s10875-022-01325-2
Lustig, Sapir, Regev-Yochay, Cohen, Fluss et al., COVID-19 vaccine and correlates of humoral immune responses and dynamics: A prospective, single-centre, longitudinal cohort study in health-care workers, Lancet Respir. Med, doi:10.1016/S2213-2600(21)00220-4
Mccartney, O'shea, Healy, Walsh, Griffin et al., The Causal Role of Vitamin D Deficiency in Worse COVID-19 Outcomes: Implications for Policy and Practice Development, Ir. Med. J
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis, J. Endocrinol. Investig, doi:10.1007/s40618-021-01614-4
Piec, Cook, Dervisevic, Fraser, Ruetten et al., Age and vitamin D affect the magnitude of the antibody response to the first dose of the SARS-CoV-2 BNT162b2 vaccine, Curr. Res. Transl. Med, doi:10.1016/j.retram.2022.103344
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Shah, Varna, Sharma, Mavalankar, Does vitamin D supplementation reduce COVID-19 severity? a systematic review, QJM, doi:10.1093/qjmed/hcac040
Walsh, Mccartney, Laird, Mccarroll, Byrne et al., Understanding a Low Vitamin D State in the Context of COVID-19, Front. Pharmacol, doi:10.3389/fphar.2022.835480
Wolff, Nee, Hickey, Marschollek, Risk factors for COVID-19 severity and fatality: A structured literature review, Infection, doi:10.1007/s15010-020-01509-1
Zdrenghea, Makrinioti, Bagacean, Bush, Johnston et al., Vitamin D modulation of innate immune responses to respiratory viral infections, Rev. Med. Virol, doi:10.1002/rmv.1909
Zelini, Angelo, Cereda, Klersy, Sabrina et al., Association between Vitamin D Serum Levels and Immune Response to the BNT162b2 Vaccine for SARS-CoV-2, Biomedicines, doi:10.3390/biomedicines10081993
Zhou, Zhu, Chu, Role of COVID-19 Vaccines in SARS-CoV-2 Variants, Front. Immunol, doi:10.3389/fimmu.2022.898192
DOI record:
{
"DOI": "10.3390/nu15132976",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu15132976",
"abstract": "<jats:p>SARS-CoV-2 vaccination promises to improve outcomes for patients with COVID-19 pneumonia (most notably those with advanced age and at high risk for severe disease). Here, we examine serum 25-Hydroxyvitamin D (25(OH)D) status and outcomes in both old (>70 years) and young vaccinated (n = 80) and unvaccinated (n = 91) subjects, who were hospitalized due to COVID-19 pneumonia in a single center (Connolly Hospital Dublin). Outcomes included ICU admission and mortality. Serum 25(OH)D levels were categorized as D30 (<30 nmol/L), D40 (30–49.99 nmol/L) and D50 (≥50 nmol/L). In multivariate analyses, D30 was independently associated with ICU admission (OR: 6.87 (95% CI: 1.13–41.85) (p = 0.036)) and mortality (OR: 24.81 (95% CI: 1.57–392.1) (p = 0.023)) in unvaccinated patients, even after adjustment for major confounders including age, sex, obesity and pre-existing diabetes mellitus. While mortality was consistently higher in all categories of patients over 70 years of age, the highest observed mortality rate of 50%, seen in patients over 70 years with a low vitamin D state (D30), appeared to be almost completely corrected by either vaccination, or having a higher vitamin D state, i.e., mortality was 14% for vaccinated patients over 70 years with D30 and 16% for unvaccinated patients over 70 years with a 25(OH)D level greater than 30 nmol/L. We observe that high mortality from COVID-19 pneumonia occurs in older patients, especially those who are unvaccinated or have a low vitamin D state. Recent vaccination or having a high vitamin D status are both associated with reduced mortality, although these effects do not fully mitigate the mortality risk associated with advanced age.</jats:p>",
"alternative-id": [
"nu15132976"
],
"author": [
{
"affiliation": [
{
"name": "School of Biological, Health & Sports Sciences, Technological University Dublin, D07 XT95 Dublin, Ireland"
}
],
"family": "Sanecka",
"given": "Martyna",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Youssef",
"given": "Modar",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Abdulsalam",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Raza",
"given": "Syed F.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Qadeer",
"given": "Abdul",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Ioana",
"given": "Julia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Aldoresi",
"given": "Alya",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Shah",
"given": "Syed I.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Al Lawati",
"given": "Abdul",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biochemistry, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Feely",
"given": "Joseph",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biochemistry, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Tormey",
"given": "William P.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Microbiology, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "O’Neill",
"given": "Eoghan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Cormican",
"given": "Liam J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
}
],
"family": "Judge",
"given": "Eoin P.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "School of Biological, Health & Sports Sciences, Technological University Dublin, D07 XT95 Dublin, Ireland"
}
],
"family": "McCartney",
"given": "Daniel M. A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2538-0030",
"affiliation": [
{
"name": "Department of Respiratory and Sleep Medicine, Connolly Hospital Dublin, D15 X40D Dublin, Ireland"
},
{
"name": "Department of Medicine, University College Dublin, D04 V1W8 Dublin, Ireland"
},
{
"name": "Department of Medicine, Royal College of Surgeons in Ireland, D02 YN77 Dublin, Ireland"
}
],
"authenticated-orcid": false,
"family": "Faul",
"given": "John L.",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
7,
3
]
],
"date-time": "2023-07-03T04:42:46Z",
"timestamp": 1688359366000
},
"deposited": {
"date-parts": [
[
2023,
7,
3
]
],
"date-time": "2023-07-03T04:50:49Z",
"timestamp": 1688359849000
},
"indexed": {
"date-parts": [
[
2023,
7,
4
]
],
"date-time": "2023-07-04T04:32:44Z",
"timestamp": 1688445164314
},
"is-referenced-by-count": 0,
"issue": "13",
"issued": {
"date-parts": [
[
2023,
6,
30
]
]
},
"journal-issue": {
"issue": "13",
"published-online": {
"date-parts": [
[
2023,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
30
]
],
"date-time": "2023-06-30T00:00:00Z",
"timestamp": 1688083200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/15/13/2976/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2976",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
6,
30
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
30
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1056/NEJMoa2118691",
"article-title": "Protection against SARS-CoV-2 after COVID-19 Vaccination and Previous Infection",
"author": "Hall",
"doi-asserted-by": "crossref",
"first-page": "1207",
"journal-title": "N. Engl. J. Med.",
"key": "ref_1",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2119451",
"article-title": "COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant",
"author": "Andrews",
"doi-asserted-by": "crossref",
"first-page": "1532",
"journal-title": "N. Engl. J. Med.",
"key": "ref_2",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2022.898192",
"article-title": "Role of COVID-19 Vaccines in SARS-CoV-2 Variants",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "898192",
"journal-title": "Front. Immunol.",
"key": "ref_3",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3390/ijms22168988",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Chiu, S.K., Tsai, K.W., Wu, C.C., Zheng, C.M., Yang, C.H., Hu, W.C., Hou, Y.C., Lu, K.C., and Chao, Y.C. (2021). Putative Role of Vitamin D for COVID-19 Vaccination. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.3390/nu14183821",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Jolliffe, D.A., Vivaldi, G., Chambers, E.S., Cai, W., Li, W., Faustini, S.E., Gibbons, J.M., Pade, C., Coussens, A.K., and Richter, A.G. (2022). Vitamin D Supplementation Does Not Influence SARS-CoV-2 Vaccine Efficacy or Immunogenicity: Sub-Studies Nested within the CORONAVIT Randomised Controlled Trial. Nutrients, 14."
},
{
"DOI": "10.3390/biomedicines10081993",
"doi-asserted-by": "crossref",
"key": "ref_6",
"unstructured": "Zelini, P., d’Angelo, P., Cereda, E., Klersy, C., Sabrina, P., Albertini, R., Grugnetti, G., Grugnetti, A.M., Marena, C., and Cutti, S. (2022). Association between Vitamin D Serum Levels and Immune Response to the BNT162b2 Vaccine for SARS-CoV-2. Biomedicines, 10."
},
{
"DOI": "10.1016/j.retram.2022.103344",
"article-title": "Age and vitamin D affect the magnitude of the antibody response to the first dose of the SARS-CoV-2 BNT162b2 vaccine",
"author": "Piec",
"doi-asserted-by": "crossref",
"first-page": "103344",
"journal-title": "Curr. Res. Transl. Med.",
"key": "ref_7",
"volume": "70",
"year": "2022"
},
{
"DOI": "10.1016/S2213-2600(21)00220-4",
"article-title": "BNT162b2 COVID-19 vaccine and correlates of humoral immune responses and dynamics: A prospective, single-centre, longitudinal cohort study in health-care workers",
"author": "Lustig",
"doi-asserted-by": "crossref",
"first-page": "999",
"journal-title": "Lancet Respir. Med.",
"key": "ref_8",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "crossref",
"key": "ref_9",
"unstructured": "Radujkovic, A., Hippchen, T., Tiwari-Heckler, S., Dreher, S., Boxberger, M., and Merle, U. (2020). Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients, 12."
},
{
"DOI": "10.1007/s10875-022-01325-2",
"article-title": "Clinical and Immunological Features of SARS-CoV-2 Breakthrough Infections in Vaccinated Individuals Requiring Hospitalization",
"author": "Lamacchia",
"doi-asserted-by": "crossref",
"first-page": "1379",
"journal-title": "J. Clin. Immunol.",
"key": "ref_10",
"volume": "42",
"year": "2022"
},
{
"DOI": "10.15585/mmwr.mm7034e5",
"article-title": "SARS-CoV-2 Infections and Hospitalizations among Persons Aged ≥16 Years, by Vaccination Status—Los Angeles County, California, May 1–July 25, 2021",
"author": "Griffin",
"doi-asserted-by": "crossref",
"first-page": "1170",
"journal-title": "Morb. Mortal. Wkly. Rep.",
"key": "ref_11",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"article-title": "Vitamin D Status Is Associated with In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients",
"author": "Angelidi",
"doi-asserted-by": "crossref",
"first-page": "875",
"journal-title": "Mayo Clin. Proc.",
"key": "ref_12",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0263069",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Dror, A.A., Morozov, N., Daoud, A., Namir, Y., Yakir, O., Shachar, Y., Lifshitz, M., Segal, E., Fisher, L., and Mizrachi, M. (2022). Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness. PLoS ONE, 17."
},
{
"DOI": "10.3390/nu14163252",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Barrett, R., Youssef, M., Shah, I., Ioana, J., Lawati, A.A., Bukhari, A., Hegarty, S., Cormican, L.J., Judge, E., and Burke, C.M. (2022). Vitamin D Status and Mortality from SARS CoV-2: A Prospective Study of Unvaccinated Caucasian Adults. Nutrients, 14."
},
{
"DOI": "10.1101/2021.09.22.21263977",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Borsche, L., Glauner, B., and von Mendel, J. (2021). COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis. Nutrients, 13."
},
{
"DOI": "10.1093/qjmed/hcac040",
"article-title": "Does vitamin D supplementation reduce COVID-19 severity? a systematic review",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "665",
"journal-title": "QJM",
"key": "ref_16",
"volume": "115",
"year": "2022"
},
{
"article-title": "Vitamin D supplementation and COVID-19 outcomes: A systematic review, meta-analysis and meta-regression",
"author": "Hariyanto",
"first-page": "e2269",
"journal-title": "Rev. Med. Virol.",
"key": "ref_17",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.1186/s12937-021-00744-y",
"article-title": "Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "89",
"journal-title": "Nutr. J.",
"key": "ref_18",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1530/EJE-20-0665",
"article-title": "Mechanisms In Endocrinology: Vitamin D and COVID-19",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "R133",
"journal-title": "Eur. J. Endocrinol.",
"key": "ref_19",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0268396",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "D’Ecclesiis, O., Gavioli, C., Martinoli, C., Raimondi, S., Chiocca, S., Miccolo, C., Bossi, P., Cortinovis, D., Chiaradonna, F., and Palorini, R. (2022). Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis. PLoS ONE, 17."
},
{
"DOI": "10.3389/fpubh.2021.736665",
"article-title": "Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes",
"author": "Chiodini",
"doi-asserted-by": "crossref",
"first-page": "736665",
"journal-title": "Front. Public Health",
"key": "ref_21",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.3390/ph16010130",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Argano, C., Mallaci Bocchio, R., Natoli, G., Scibetta, S., Lo Monaco, M., and Corrao, S. (2023). Protective Effect of Vitamin D Supplementation on COVID-19-Related Intensive Care Hospitalization and Mortality: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis. Pharmaceuticals, 16."
},
{
"DOI": "10.1007/s40618-021-01614-4",
"article-title": "Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis",
"author": "Pal",
"doi-asserted-by": "crossref",
"first-page": "53",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref_23",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.3945/ajcn.115.120873",
"article-title": "Vitamin D deficiency in Europe: Pandemic?",
"author": "Cashman",
"doi-asserted-by": "crossref",
"first-page": "1033",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_24",
"volume": "103",
"year": "2016"
},
{
"DOI": "10.1002/rmv.1909",
"article-title": "Vitamin D modulation of innate immune responses to respiratory viral infections",
"author": "Zdrenghea",
"doi-asserted-by": "crossref",
"first-page": "e1909",
"journal-title": "Rev. Med. Virol.",
"key": "ref_25",
"volume": "27",
"year": "2017"
},
{
"DOI": "10.2147/JIR.S282213",
"article-title": "Understanding COVID-19 Pandemic: Molecular Mechanisms and Potential Therapeutic Strategies. An Evidence-Based Review",
"author": "Hanna",
"doi-asserted-by": "crossref",
"first-page": "13",
"journal-title": "J. Inflamm. Res.",
"key": "ref_26",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1038/s41590-021-01080-3",
"article-title": "Autocrine vitamin D signaling switches off pro-inflammatory programs of TH1 cells",
"author": "Chauss",
"doi-asserted-by": "crossref",
"first-page": "62",
"journal-title": "Nat. Immunol.",
"key": "ref_27",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1007/s15010-020-01509-1",
"article-title": "Risk factors for COVID-19 severity and fatality: A structured literature review",
"author": "Wolff",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Infection",
"key": "ref_28",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.2310/JIM.0b013e31821b8755",
"article-title": "Vitamin D and the immune system",
"author": "Aranow",
"doi-asserted-by": "crossref",
"first-page": "881",
"journal-title": "J. Investig. Med.",
"key": "ref_29",
"volume": "59",
"year": "2011"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"article-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers",
"author": "Jain",
"doi-asserted-by": "crossref",
"first-page": "20191",
"journal-title": "Sci. Rep.",
"key": "ref_30",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.3389/fphar.2022.835480",
"article-title": "Understanding a Low Vitamin D State in the Context of COVID-19",
"author": "Walsh",
"doi-asserted-by": "crossref",
"first-page": "835480",
"journal-title": "Front. Pharmacol.",
"key": "ref_31",
"volume": "13",
"year": "2022"
},
{
"article-title": "The Causal Role of Vitamin D Deficiency in Worse COVID-19 Outcomes: Implications for Policy and Practice Development",
"author": "McCartney",
"first-page": "P733",
"journal-title": "Ir. Med. J.",
"key": "ref_32",
"volume": "116",
"year": "2023"
},
{
"DOI": "10.1186/s12986-020-00491-7",
"article-title": "Systemic vitamin intake impacting tissue proteomes",
"author": "Jeong",
"doi-asserted-by": "crossref",
"first-page": "73",
"journal-title": "Nutr. Metab.",
"key": "ref_33",
"volume": "17",
"year": "2020"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/15/13/2976"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Hospital Outcomes in Patients Hospitalized for COVID-19 Pneumonia: The Effect of SARS-CoV-2 Vaccination and Vitamin D Status",
"type": "journal-article",
"volume": "15"
}
