The effect of 1-hydroxy-vitamin D treatment in hospitalized patients with COVID-19: A retrospective study
et al., Clinical Nutrition, doi:10.1016/j.clnu.2023.08.021, Sep 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
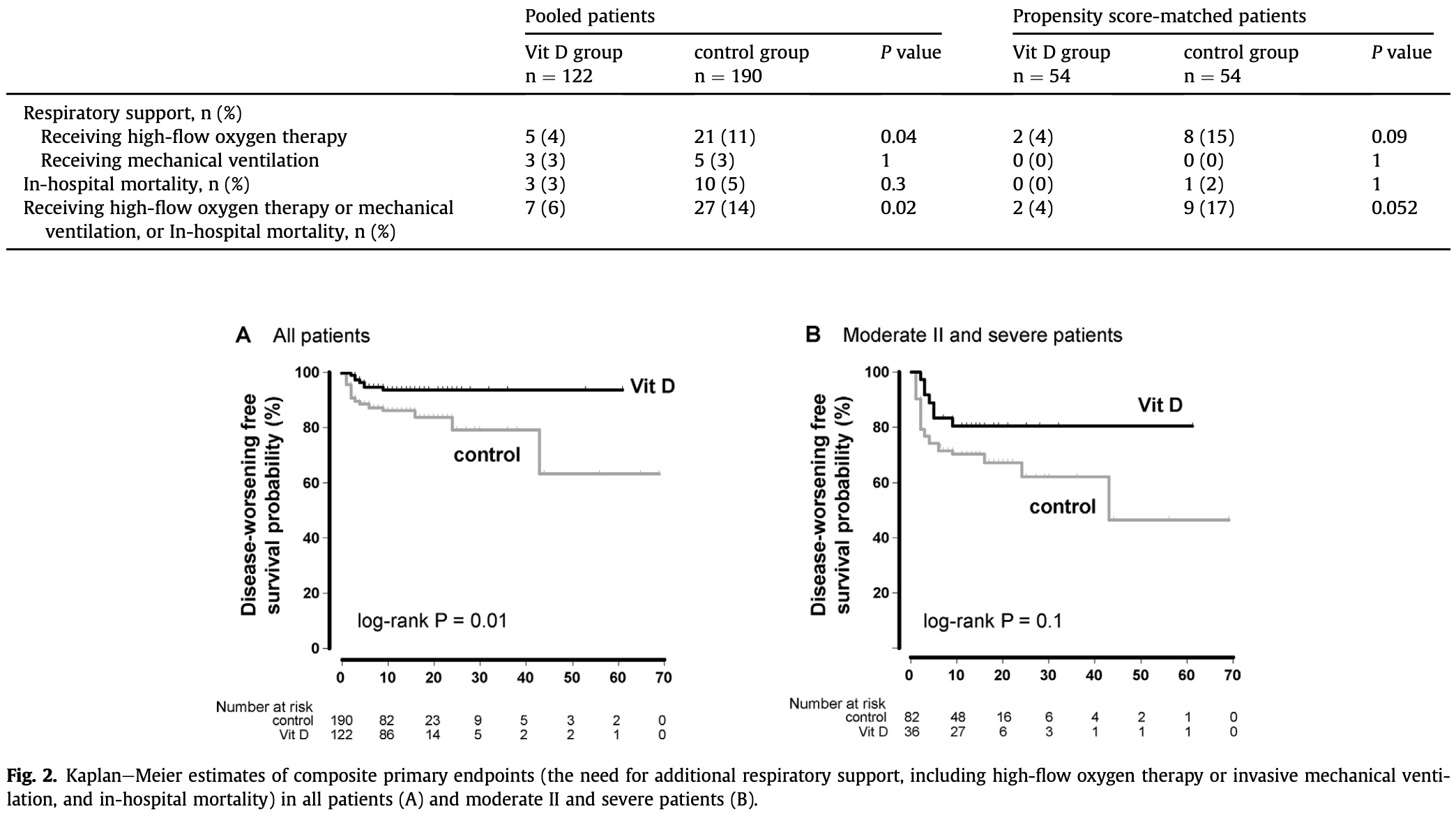
PSM retrospective 312 hospitalized patients in Japan, showing lower progression with vitamin D (alfacalcidol) treatment, statistically significant via KM log-rank.
Meta-analysis shows that late stage treatment with calcitriol / calcifediol (or
paricalcitol, alfacalcidol, etc.) is more effective than cholecalciferol: 66% [47‑78%] lower risk vs. 44% [33‑53%] lower risk.
Cholecalciferol requires two hydroxylation steps to become activated - first
in the liver to calcifediol, then in the kidney to calcitriol. Calcitriol,
paricalcitol, and alfacalcidol are active vitamin D analogs that do not
require conversion. This allows them to have more rapid onset of action
compared to cholecalciferol. The time delay for cholecalciferol to increase
serum calcifediol levels can be 2-3 days, and the delay for converting
calcifediol to active calcitriol can be up to 7 days.
This is the 124th of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
Standard of Care (SOC) for COVID-19 in the study country,
Japan, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 66.7% lower, RR 0.33, p = 1.00, treatment 0 of 54 (0.0%), control 1 of 54 (1.9%), NNT 54, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
|
risk of progression, 77.8% lower, RR 0.22, p = 0.05, treatment 2 of 54 (3.7%), control 9 of 54 (16.7%), NNT 7.7, high-flow oxygen, mechanical ventilation, or mortality, primary outcome.
|
|
risk of oxygen therapy, 75.0% lower, RR 0.25, p = 0.09, treatment 2 of 54 (3.7%), control 8 of 54 (14.8%), NNT 9.0.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ogasawara et al., 1 Sep 2023, retrospective, Japan, peer-reviewed, 10 authors, study period April 2021 - September 2022, dosage alfacalcidol 1μg days 1-8, median duration, alfacalcidol and eldecalcitol used.
Contact: shikatarawasagao@gmail.com.
The effect of 1-hydroxy-vitamin D treatment in hospitalized patients with COVID-19: A retrospective study
Clinical Nutrition, doi:10.1016/j.clnu.2023.08.021
Background & aims: The efficacy of vitamin D supplementation in coronavirus disease 2019 remains unclear. This study aimed to evaluate the effect of 1-hydroxy-vitamin D on the prevention of severe disease and mortality in patients hospitalized for COVID-19. Methods: This retrospective study included 312 patients with COVID-19 who were admitted to our hospital between April 2021 and October 2021 (primarily the Delta variant) and between July 2022 and September 2022 (primarily Omicron variant). Serum 25-hydroxyvitamin D (25(OH)D) levels were measured at the time of admission and 1-hydroxy-vitamin D was prescribed by the treating physicians. The patients were divided into two groups: those administered 1-hydroxy-vitamin D (Vit D group) and those who were not (control group). The composite primary endpoint was the need for additional respiratory support, including high-flow oxygen therapy or invasive mechanical ventilation, and in-hospital mortality rate. Results: Of 312 patients, 122 (39%) received 1-hydroxy-vitamin D treatment. Although the median age was not significantly higher in the Vit D group than in the control group (66 vs. 58 years old, P ¼ 0.06) and there was no significant difference in the proportion of vitamin D deficiency (defined as serum 25(OH)D level less than 20 ng/mL, 77% vs. 65%, P ¼ 0.07), patients in the control group had a more severe baseline profile compared to the Vit D group according to the Japanese disease severity definition for COVID-19 (P ¼ 0.01). The proportion of those requiring more respiratory support and in-hospital mortality was significantly lower in the Vit D group than in the control group (6% vs. 14%, P ¼ 0.01 log-rank test). After propensity score matching, a statistically significant difference in the primary endpoint was observed (P ¼ 0.03 log-rank test). Conclusions: 1-hydroxy-vitamin treatment may improve outcomes in hospitalized patients with COVID-19, reducing composite outcomes including the need for additional respiratory support and in-hospital mortality.
Author contributions TO and YT conceived and designed this study. TO, YT, NN, HK, YO, MS, MN and WM did acquisition, analyses, and interpretation of data. TO drafted manuscript. TO, YT, NN, WM, MN, MO and JS contributed to reviewing or revising the paper. All authors read and approved the final manuscript.
Conflicts of interest None of the authors declared a conflict of interest.
References
Ahmad, Arora, Khan, Mohsin, Manda, Vitamin D and its therapeutic relevance in pulmonary diseases, J Nutr Biochem, doi:10.1016/j.jnutbio.2020.108571
Argano, Bocchio, Natoli, Scibetta, Monaco et al., Protective effect of vitamin D supplementation on COVID-19-related intensive care hospitalization and mortality: definitive evidence from meta-analysis and trial sequential analysis, Pharmaceuticals, doi:10.3390/ph16010130
Bae, Choe, Holick, Lim, Association of vitamin D status with COVID-19 and its severity : vitamin D and COVID-19: a narrative review, Rev Endocr Metab Disord, doi:10.1007/s11154-021-09705-6
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med, doi:10.1136/postgradmedj-2020-138712
Ben-Eltriki, Hopefl, Wright, Association between vitamin D status and risk of developing severe COVID-19 infection: a meta-analysis of observational studies, J Am Nutraceutical Assoc, doi:10.1080/07315724.2021.1951891
Beran, Mhanna, Srour, Ayesh, Stewart et al., Clinical significance of micronutrient supplements in patients with coronavirus disease 2019: a comprehensive systematic review and meta-analysis, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2021.12.033
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., Mechanisms in endocrinology: vitamin D and COVID-19, Eur J Endocrinol, doi:10.1530/EJE-20-0665
Cashman, Global differences in vitamin D status and dietary intake: a review of the data, Endocr Connect, doi:10.1530/EC-21-0282
Castillo, Costa, Barrios, Díaz, Opez Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D status and SARS-CoV-2 infection and COVID-19 clinical outcomes, Front Public Health, doi:10.3389/fpubh.2021.736665
Dror, Morozov, Daoud, Namir, Yakir et al., Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness, PLoS One, doi:10.1371/journal.pone.0263069
Giustina, Bouillon, Dawson-Hughes, Ebeling, Lazaretti-Castro et al., Vitamin D in the older population: a consensus statement, Endocrine, doi:10.1007/s12020-022-03208-3
Gombart, The vitamin D-antimicrobial peptide pathway and its role in protection against infection, Future Microbiol, doi:10.2217/fmb.09.87
Gotelli, Soldano, Hysa, Paolino, Campitiello et al., Vitamin D and COVID-19: narrative review after 3 Years of pandemic, Nutrients, doi:10.3390/nu14224907
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Griffin, Hewison, Hopkin, Kenny, Quinton et al., Perspective: vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19, Clin Med, doi:10.7861/clinmed.2021-0035
Harrison, Fazio-Eynullayeva, Lane, Underhill, Lip, Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: a federated electronic medical record analysis, PLoS Med, doi:10.1371/journal.pmed.1003321
Hilger, Friedel, Herr, Rausch, Roos et al., A systematic review of vitamin D status in populations worldwide, Br J Nutr, doi:10.1017/S0007114513001840
Jones, Prosser, Kaufmann, 25-Hydroxyvitamin D-24-hydroxylase (CYP24A1): its important role in the degradation of vitamin D, Arch Biochem Biophys, doi:10.1016/j.abb.2011.11.003
Jordan, Siuka, Rotovnik, Pfeifer, COVID-19 and vitamin D-a systematic review, Zdr Varst, doi:10.2478/sjph-2022-0017
Kanda, Free statistical software: EZR (Easy R) on R commander
Kanda, Investigation of the freely available easy-to-use software 'EZR' for medical statistics, Bone Marrow Transplant, doi:10.1038/bmt.2012.244
Mansur, Tajer, Mariani, Inserra, Ferder et al., Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection, English, Spanish Clín Invest Arterioscler, doi:10.1016/j.arteri.2020.05.003
Mariani, Antonietti, Tajer, Ferder, Inserra et al., High-dose vitamin D versus placebo to prevent complications in COVID-19 patients: multicentre randomized controlled clinical trial, PLoS One, doi:10.1371/journal.pone.0267918
Oristrell, Oliva, Casado, Subirana, Domínguez et al., Vitamin D supplementation and COVID-19 risk: a population-based, cohort study, J Endocrinol Invest, doi:10.1007/s40618-021-01639-9
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis, J Endocrinol Invest, doi:10.1007/s40618-021-01614-4
Płudowski, Kos-Kudła, Walczak, Fal, Zozuli Nska-Zi Ołkiewicz et al., Guidelines for preventing and treating vitamin D deficiency: a 2023 update in Poland, Nutrients, doi:10.3390/nu15030695
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: vitamin D deficiency and COVID-19 severity -plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J Intern Med, doi:10.1111/joim.13149
Ringe, Schacht, Improving the outcome of established therapies for osteoporosis by adding the active D-hormone analog alfacalcidol, Rheumatol Int, doi:10.1007/s00296-007-0422-6
Sabico, Enani, Sheshah, Aljohani, Aldisi et al., Effects of a 2-week 5000 IU versus 1000 IU vitamin D3 supplementation on recovery of symptoms in patients with mild to moderate covid-19: a randomized clinical trial, Nutrients, doi:10.3390/nu13072170
Sarhan, Warda, Sarhan, Boshra, Mostafa-Hedeab et al., Evidence for the efficacy of a high dose of vitamin D on the hyperinflammation state in moderate-to-severe COVID-19 patients: a randomized clinical trial, doi:10.3390/medicina58101358
Sîrbu, Sabin, Bocșan, Vesa, Buzoianu, The effect of vitamin D supplementation on the length of hospitalisation, intensive care unit admission, and mortality in COVID-19-A systematic review and meta-analysis, Nutrients, doi:10.3390/nu15153470
Van Der Wielen, L€ Owik Mr, Van Den Berg, De Groot, Haller et al., Serum vitamin D concentrations among elderly people in Europe, Lancet, doi:10.1016/s0140-6736(95)91266-5
Van Diepen, Mcalister, Chu, Youngson, Kaul et al., Association between vaccination status and outcomes in patients admitted to the ICU with COVID-19, Crit Care Med, doi:10.1097/CCM.0000000000005928
DOI record:
{
"DOI": "10.1016/j.clnu.2023.08.021",
"ISSN": [
"0261-5614"
],
"URL": "http://dx.doi.org/10.1016/j.clnu.2023.08.021",
"alternative-id": [
"S0261561423002790"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "The effect of 1-hydroxy-vitamin D treatment in hospitalized patients with COVID-19: A retrospective study"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Clinical Nutrition"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.clnu.2023.08.021"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 Elsevier Ltd and European Society for Clinical Nutrition and Metabolism. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0009-0009-8707-3264",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ogasawara",
"given": "Takashi",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-6977-195X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tajima",
"given": "Yasuhisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nakamura",
"given": "Naoto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kanasaki",
"given": "Hiroki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Matsuyama",
"given": "Wataru",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Niwa",
"given": "Mitsuru",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3798-3488",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ozawa",
"given": "Yuichi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sugiura",
"given": "Masayuki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ogiku",
"given": "Masahito",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sato",
"given": "Jun",
"sequence": "additional"
}
],
"container-title": "Clinical Nutrition",
"container-title-short": "Clinical Nutrition",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"clinicalnutritionjournal.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
9,
1
]
],
"date-time": "2023-09-01T15:21:32Z",
"timestamp": 1693581692000
},
"deposited": {
"date-parts": [
[
2023,
9,
6
]
],
"date-time": "2023-09-06T21:27:38Z",
"timestamp": 1694035658000
},
"indexed": {
"date-parts": [
[
2023,
9,
7
]
],
"date-time": "2023-09-07T21:14:41Z",
"timestamp": 1694121281695
},
"is-referenced-by-count": 0,
"issue": "10",
"issued": {
"date-parts": [
[
2023,
10
]
]
},
"journal-issue": {
"issue": "10",
"published-print": {
"date-parts": [
[
2023,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
10,
1
]
],
"date-time": "2023-10-01T00:00:00Z",
"timestamp": 1696118400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0261561423002790?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0261561423002790?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "2045-2050",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
10
]
]
},
"published-print": {
"date-parts": [
[
2023,
10
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"key": "10.1016/j.clnu.2023.08.021_bib1",
"unstructured": "WHO Coronavirus (COVID-19) Dashboard (Accessed August 16, 2023, at https://covid19.who.int/)."
},
{
"key": "10.1016/j.clnu.2023.08.021_bib2",
"unstructured": "Underlying Medical Conditions Associated with High Risk for Severe COVID-19 : Information for Healthcare Professionals : CDC (Accessed August 16, 2023, at https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html)."
},
{
"DOI": "10.1371/journal.pmed.1003321",
"article-title": "Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: a federated electronic medical record analysis",
"author": "Harrison",
"doi-asserted-by": "crossref",
"journal-title": "PLoS Med",
"key": "10.1016/j.clnu.2023.08.021_bib3",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.jnutbio.2020.108571",
"article-title": "Vitamin D and its therapeutic relevance in pulmonary diseases",
"author": "Ahmad",
"doi-asserted-by": "crossref",
"journal-title": "J Nutr Biochem",
"key": "10.1016/j.clnu.2023.08.021_bib4",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.3390/nu12040988",
"article-title": "Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths",
"author": "Grant",
"doi-asserted-by": "crossref",
"first-page": "988",
"journal-title": "Nutrients",
"key": "10.1016/j.clnu.2023.08.021_bib5",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1017/S0007114513001840",
"article-title": "A systematic review of vitamin D status in populations worldwide",
"author": "Hilger",
"doi-asserted-by": "crossref",
"first-page": "23",
"journal-title": "Br J Nutr",
"key": "10.1016/j.clnu.2023.08.021_bib6",
"volume": "111",
"year": "2014"
},
{
"DOI": "10.1530/EC-21-0282",
"article-title": "Global differences in vitamin D status and dietary intake: a review of the data",
"author": "Cashman",
"doi-asserted-by": "crossref",
"journal-title": "Endocr Connect",
"key": "10.1016/j.clnu.2023.08.021_bib7",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(95)91266-5",
"article-title": "Serum vitamin D concentrations among elderly people in Europe",
"author": "van der Wielen",
"doi-asserted-by": "crossref",
"first-page": "207",
"journal-title": "Lancet",
"key": "10.1016/j.clnu.2023.08.021_bib8",
"volume": "346",
"year": "1995"
},
{
"DOI": "10.1007/s12020-022-03208-3",
"article-title": "Vitamin D in the older population: a consensus statement",
"author": "Giustina",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Endocrine",
"key": "10.1016/j.clnu.2023.08.021_bib9",
"volume": "79",
"year": "2023"
},
{
"DOI": "10.1111/joim.13149",
"article-title": "Perspective: vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis",
"author": "Rhodes",
"doi-asserted-by": "crossref",
"first-page": "97",
"journal-title": "J Intern Med",
"key": "10.1016/j.clnu.2023.08.021_bib10",
"volume": "289",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"author": "Baktash",
"doi-asserted-by": "crossref",
"first-page": "442",
"journal-title": "Postgrad Med",
"key": "10.1016/j.clnu.2023.08.021_bib11",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0263069",
"article-title": "Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness",
"author": "Dror",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "10.1016/j.clnu.2023.08.021_bib12",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.2217/fmb.09.87",
"article-title": "The vitamin D-antimicrobial peptide pathway and its role in protection against infection",
"author": "Gombart",
"doi-asserted-by": "crossref",
"first-page": "1151",
"journal-title": "Future Microbiol",
"key": "10.1016/j.clnu.2023.08.021_bib13",
"volume": "4",
"year": "2009"
},
{
"DOI": "10.1530/EJE-20-0665",
"article-title": "Mechanisms in endocrinology: vitamin D and COVID-19",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "R133",
"journal-title": "Eur J Endocrinol",
"key": "10.1016/j.clnu.2023.08.021_bib14",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1016/j.arteri.2020.05.003",
"article-title": "Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection",
"author": "Mansur",
"doi-asserted-by": "crossref",
"first-page": "267",
"journal-title": "Clín Invest Arterioscler",
"key": "10.1016/j.clnu.2023.08.021_bib15",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1007/s40618-021-01614-4",
"article-title": "Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis",
"author": "Pal",
"doi-asserted-by": "crossref",
"first-page": "53",
"journal-title": "J Endocrinol Invest",
"key": "10.1016/j.clnu.2023.08.021_bib16",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.3390/nu13072170",
"article-title": "Effects of a 2-week 5000 IU versus 1000 IU vitamin D3 supplementation on recovery of symptoms in patients with mild to moderate covid-19: a randomized clinical trial",
"author": "Sabico",
"doi-asserted-by": "crossref",
"first-page": "2170",
"journal-title": "Nutrients",
"key": "10.1016/j.clnu.2023.08.021_bib17",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/ph16010130",
"article-title": "Protective effect of vitamin D supplementation on COVID-19-related intensive care hospitalization and mortality: definitive evidence from meta-analysis and trial sequential analysis",
"author": "Argano",
"doi-asserted-by": "crossref",
"first-page": "130",
"journal-title": "Pharmaceuticals",
"key": "10.1016/j.clnu.2023.08.021_bib18",
"volume": "16",
"year": "2023"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study",
"author": "Entrenas Castillo",
"doi-asserted-by": "crossref",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "10.1016/j.clnu.2023.08.021_bib19",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.3390/nu15153470",
"article-title": "The effect of vitamin D supplementation on the length of hospitalisation, intensive care unit admission, and mortality in COVID-19-A systematic review and meta-analysis",
"author": "Sîrbu",
"doi-asserted-by": "crossref",
"first-page": "3470",
"journal-title": "Nutrients",
"key": "10.1016/j.clnu.2023.08.021_bib20",
"volume": "15",
"year": "2023"
},
{
"key": "10.1016/j.clnu.2023.08.021_bib21",
"unstructured": "Clinical management of patients with COVID-19 in Japan (Accessed June 8, 2023 at https://www.mhlw.go.jp/content/000936655.pdf)."
},
{
"key": "10.1016/j.clnu.2023.08.021_bib22",
"unstructured": "Kanda Y. Free statistical software: EZR (Easy R) on R commander. Available from: fihttp://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmedEN.html."
},
{
"DOI": "10.1038/bmt.2012.244",
"article-title": "Investigation of the freely available easy-to-use software 'EZR' for medical statistics",
"author": "Kanda",
"doi-asserted-by": "crossref",
"first-page": "452",
"journal-title": "Bone Marrow Transplant",
"key": "10.1016/j.clnu.2023.08.021_bib23",
"volume": "48",
"year": "2013"
},
{
"article-title": "Association between vitamin D status and risk of developing severe COVID-19 infection: a meta-analysis of observational studies",
"author": "Ben-Eltriki",
"first-page": "679",
"journal-title": "J Am Nutraceutical Assoc",
"key": "10.1016/j.clnu.2023.08.021_bib24",
"volume": "41",
"year": "2022"
},
{
"article-title": "COVID-19 and vitamin D- a systematic review",
"author": "Jordan",
"first-page": "124",
"journal-title": "Zdr Varst",
"key": "10.1016/j.clnu.2023.08.021_bib25",
"volume": "61",
"year": "2022"
},
{
"DOI": "10.1007/s40618-021-01639-9",
"article-title": "Vitamin D supplementation and COVID-19 risk: a population-based, cohort study",
"author": "Oristrell",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "J Endocrinol Invest",
"key": "10.1016/j.clnu.2023.08.021_bib26",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.3389/fpubh.2021.736665",
"article-title": "Vitamin D status and SARS-CoV-2 infection and COVID-19 clinical outcomes",
"author": "Chiodini",
"doi-asserted-by": "crossref",
"journal-title": "Front Public Health",
"key": "10.1016/j.clnu.2023.08.021_bib27",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2021.12.033",
"article-title": "Clinical significance of micronutrient supplements in patients with coronavirus disease 2019: a comprehensive systematic review and meta-analysis",
"author": "Beran",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "Clin Nutr ESPEN",
"key": "10.1016/j.clnu.2023.08.021_bib28",
"volume": "48",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0267918",
"article-title": "High-dose vitamin D versus placebo to prevent complications in COVID-19 patients: multicentre randomized controlled clinical trial",
"author": "Mariani",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "10.1016/j.clnu.2023.08.021_bib29",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1016/j.abb.2011.11.003",
"article-title": "25-Hydroxyvitamin D-24-hydroxylase (CYP24A1): its important role in the degradation of vitamin D",
"author": "Jones",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Arch Biochem Biophys",
"key": "10.1016/j.clnu.2023.08.021_bib30",
"volume": "523",
"year": "2012"
},
{
"DOI": "10.7861/clinmed.2021-0035",
"article-title": "Perspective: vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19",
"author": "Griffin",
"doi-asserted-by": "crossref",
"first-page": "e144",
"journal-title": "Clin Med",
"key": "10.1016/j.clnu.2023.08.021_bib31",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.3390/nu14224907",
"article-title": "Vitamin D and COVID-19: narrative review after 3 Years of pandemic",
"author": "Gotelli",
"doi-asserted-by": "crossref",
"first-page": "4907",
"journal-title": "Nutrients",
"key": "10.1016/j.clnu.2023.08.021_bib32",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1007/s11154-021-09705-6",
"article-title": "Association of vitamin D status with COVID-19 and its severity : vitamin D and COVID-19: a narrative review",
"author": "Bae",
"doi-asserted-by": "crossref",
"first-page": "579",
"journal-title": "Rev Endocr Metab Disord",
"key": "10.1016/j.clnu.2023.08.021_bib33",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1097/CCM.0000000000005928",
"article-title": "Association between vaccination status and outcomes in patients admitted to the ICU with COVID-19",
"author": "van Diepen",
"doi-asserted-by": "crossref",
"journal-title": "Crit Care Med",
"key": "10.1016/j.clnu.2023.08.021_bib34",
"year": "2023"
},
{
"DOI": "10.1007/s00296-007-0422-6",
"article-title": "Improving the outcome of established therapies for osteoporosis by adding the active D-hormone analog alfacalcidol",
"author": "Ringe",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "Rheumatol Int",
"key": "10.1016/j.clnu.2023.08.021_bib35",
"volume": "28",
"year": "2007"
},
{
"DOI": "10.3390/medicina58101358",
"article-title": "Evidence for the efficacy of a high dose of vitamin D on the hyperinflammation state in moderate-to-severe COVID-19 patients: a randomized clinical trial",
"author": "Sarhan",
"doi-asserted-by": "crossref",
"first-page": "1358",
"journal-title": "Medicina (Kaunas)",
"key": "10.1016/j.clnu.2023.08.021_bib36",
"volume": "58",
"year": "2022"
},
{
"DOI": "10.3390/nu15030695",
"article-title": "Guidelines for preventing and treating vitamin D deficiency: a 2023 update in Poland",
"author": "Płudowski",
"doi-asserted-by": "crossref",
"first-page": "695",
"journal-title": "Nutrients",
"key": "10.1016/j.clnu.2023.08.021_bib37",
"volume": "15",
"year": "2023"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0261561423002790"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Critical Care and Intensive Care Medicine",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "The effect of 1-hydroxy-vitamin D treatment in hospitalized patients with COVID-19: A retrospective study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "42"
}
