Association Between Vitamin D Levels and Long COVID Signs and Symptoms
et al., Medical Sciences, doi:10.3390/medsci13030199, Sep 2025
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 170 outpatients with mild COVID-19 showing higher risk of long COVID with vitamin D deficiency.
This is the 224th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
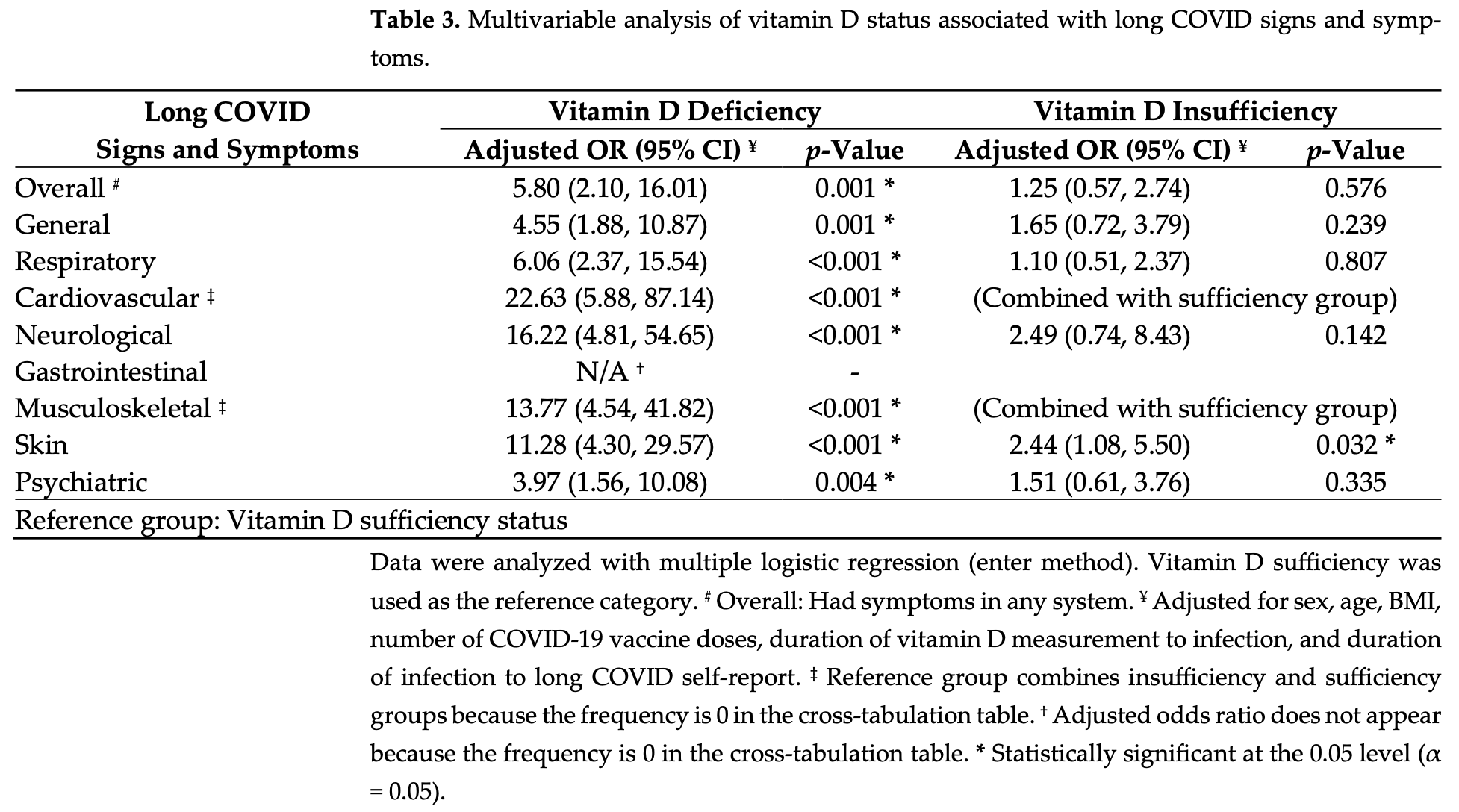
risk of long COVID, 82.8% lower, OR 0.17, p < 0.001, high D levels (≥30 ng/mL) 48, low D levels (<20 ng/mL) 52, adjusted per study, inverted to make OR<1 favor high D levels (≥30 ng/mL), multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Matangkha et al., 18 Sep 2025, retrospective, Thailand, peer-reviewed, mean age 45.9, 4 authors.
Contact: wichian.sit@mfu.ac.th (corresponding author), mdkarn.m@gmail.com, vichit.pun@mfu.ac.th, jarasphol.rin@mfu.ac.th.
Association Between Vitamin D Levels and Long COVID Signs and Symptoms
Medical Sciences, doi:10.3390/medsci13030199
Background: "Long COVID" refers to a condition in which individuals continue to experience persistent signs and symptoms even after recovering from the initial COVID-19 infection. Signs and symptoms that persist can affect multiple organs in the body. Vitamin D is an essential nutrient that plays a crucial role, particularly in the immune system, and may be linked to the development of long COVID. Objective: The study aimed to investigate the association between vitamin D levels and the prevalence of long COVID signs and symptoms in COVID-19 patients. Materials and Methods: The study enrolled 170 COVID-19 patients with mild signs and symptoms and confirmed COVID-Ag or RT-PCR tests. The subjects were aged 18-59 years. All patients had 25(OH)D levels measured within 60 days of COVID-19 diagnosis and had been followed for at least 3 months postinfection. Data collected included demographic characteristics, serum 25(OH)D levels, and self-reported long COVID signs and symptoms questionnaire responses. Results: The study results indicated a female-to-male ratio of 1.1:1 and a mean age of 45.87 ± 8.65 years; of these, 62.4% received three doses of the COVID-19 vaccine, and 64.7% developed long COVID. The most prevalent signs and symptoms were respiratory (55.3%), skin (50.6%), and general (39.4%). The median blood vitamin D level was 22.96 ng/mL, with 41.2% of subjects having insufficient levels, 30.6% having deficient levels, and 28.2% having sufficient levels. Patients with long COVID had significantly lower vitamin D levels compared with those without long COVID (21.52 ng/mL vs. 25.46 ng/mL; p < 0.05). Multivariable analysis found that vitamin D deficiency was significantly associated with overall long COVID signs and symptoms (Adj. OR, 5.80 [95% CI: 2.10, 16.13]). Additionally, vitamin D deficiency significantly increased the number of long COVID systemic signs and symptoms (Adj. IRR, 3.30 [2.12, 5.12]). Conclusion: Assessing and maintaining vitamin D levels, vitamin D supplementation, and sunlight exposure in COVID-19 patients can reduce the risk and severity of long-term COVID-19 signs and symptoms.
Author Contributions: Conceptualization: K.M. and J.R.; Data curation: K.M.; Formal analysis: K.M. and P.S.; Methodology: K.M. and J.R.; Visualization: P.S.; Investigation: K.M. and J.R.; Resources: K.M.; Software: K.M.; Validation: P.S.; Writing-original draft preparation: K.M. and P.S.; Writingreview and editing, P.S.; Supervision: V.P., J.R. and P.S.; Project administration: V.P.; Funding acquisition: K.M. and P.S. All authors have read and agreed to the published version of the manuscript. Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Ashique, Gupta, Gupta, Mishra, Singh et al., Vitamin D-A prominent immunomodulator to prevent COVID-19 infection, Int. J. Rheum. Dis, doi:10.1111/1756-185X.14477
Azambuja, Bastos, Batista-Da-Silva, Ramos, Kurtz et al., Prevalence, risk factors, and impact of long COVID in a socially vulnerable community in Brazil: A prospective cohort study, Lancet Reg. Health Am, doi:10.1016/j.lana.2024.100839
Barrea, Verde, Grant, Frias-Toral, Sarno et al., Vitamin D: A Role Also in Long COVID-19?, Nutrients, doi:10.3390/nu14081625
Beale, Yavlinsky, Moncunill, Fong, Nguyen et al., Anti-nucleocapsid and anti-spike antibody trajectories in people with post-COVID condition versus acute-only infections: A nested longitudinal case-control study within the Virus Watch prospective cohort, Nat. Commun, doi:10.1038/s41467-025-58766-7
Bigman, Diet and nutrition in long COVID: Low vitamin D and clinical trial of magnesium and vitamin D-A comprehensive scoping review, Nutrients, doi:10.3390/nu17030523
Cardoso, Araújo, Silva, Guimarães, Taveiro et al., Vitamin D levels and COVID-19 severe pneumonia: A prospective case-control study, medRxiv, doi:10.1101/2024.06.10.24308690
Cazé, Cerqueira-Silva, Bomfim, De Souza, Azevedo et al., Prevalence and risk factors for long COVID after mild disease: A cohort study with a symptomatic control group, J. Glob. Health, doi:10.7189/jogh.13.06015
Chailurkit, Ongphiphadhanakul, Aekplakorn, Update on vitamin D status in sunshine-abundant Thailand, 2019-2020, Nutrition, doi:10.1016/j.nut.2023.112161
Chen, Haupert, Zimmermann, Shi, Fritsche et al., Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review, J. Infect. Dis, doi:10.1093/infdis/jiac136
Davis, Mccorkell, Vogel, Topol, Long, Major findings, mechanisms and recommendations, Nat. Rev. Microbiol, doi:10.1038/s41579-022-00846-2
Di Filippo, Frara, Nannipieri, Cotellessa, Locatelli et al., Low Vitamin D Levels Are Associated with Long COVID Syndrome in COVID-19 Survivors, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgad207
Di Gennaro, Belati, Tulone, Diella, Fiore Bavaro et al., Incidence of long COVID-19 in people with previous SARS-CoV2 infection: A systematic review and meta-analysis of 120,970 patients, Intern. Emerg. Med, doi:10.1007/s11739-022-03164-w
Fenercioglu, The Anti-Inflammatory Roles of Vitamin D for Improving Human Health, Curr. Issues Mol. Biol, doi:10.3390/cimb46120807
Ford, Slaughter, Edwards, Dalton, Perrine et al., Long COVID and Significant Activity Limitation Among Adults, by Age-United States, 1-13 June 2022 to 7, MMWR Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm7232a3
Garg, Maralakunte, Garg, Dhooria, Sehgal et al., The Conundrum of Long-COVID-19 : A Narrative Review, Int. J. Gen. Med, doi:10.2147/IJGM.S316708
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Grant, Boucher, Cheng, Pludowski, Wimalawansa, Vitamin D and Cardiovascular Health: A Narrative Review of Risk Reduction Evidence, Nutrients, doi:10.3390/nu17132102
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Guerrero-Romero, Gamboa-Gómez, Rodríguez-Morán, Orrante, Rosales-Galindo et al., Hypomagnesemia and 25-hydroxyvitamin D deficiency in patients with long COVID, Magnes. Res, doi:10.1684/mrh.2023.0519
Hou, Gu, Ni, Shi, Ranney et al., Global Prevalence of Long COVID, its Subtypes and Risk factors: An Updated Systematic Review and Meta-Analysis, medRxiv, doi:10.1101/2025.01.01.24319384
Imran, Zia, Ali, Nisar, Iqbal et al., Therapeutic role of vitamin D in COVID-19 patients, Clin. Nutr. Open Sci, doi:10.1016/j.nutos.2024.07.004
Kaur, Khare, Sizar, Givler, Vitamin et al., StatPearls
Kokolevich, Crowe, Mendez, Biros, Reznik, Most Common Long COVID Physical Symptoms in Working Age Adults Who Experienced Mild COVID-19 Infection: A Scoping Review, Healthcare, doi:10.3390/healthcare10122577
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics with COVID-19 Test Results, JAMA Netw. Open, doi:10.1001/jamanetworko-pen.2020.19722
Nielsen, Junker, Boelt, Cohen, Munger et al., Vitamin D status and severity of COVID-19, Sci. Rep, doi:10.1038/s41598-022-21513-9
Sartini, Del Puente, Carbone, Schinca, Ottria et al., The Effect of Vitamin D Supplementation Post COVID-19 Infection and Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu16223794
Sk Abd Razak, Ismail, Abdul Aziz, Suddin, Azzeri et al., Post-COVID syndrome prevalence: A systematic review and meta-analysis, BMC Public Health, doi:10.1186/s12889-024-19264-5
Thompson, Williams, Walker, Mitchell, Niedzwiedz et al., Risk factors for long COVID: Analyses of 10 longitudinal studies and electronic health records in the UK, Nat. Commun, doi:10.1038/s41467-022-30836-0
Varnai, Molnar, Zavori, Tőkés-Füzesi, Illes et al., Serum Level of Anti-Nucleocapsid, but Not Anti-Spike Antibody, Is Associated with Improvement of Long COVID Symptoms, Vaccines, doi:10.3390/vaccines10020165
Wangchalabovorn, Weerametachai, Leesri, Prevalence of post COVID-19 conditions in SARS-CoV-2-infected patients at 3-month telephone follow-up, Reg. Health Promot. Cent
Wong, Huang, Wong, Wong, Yip et al., Symptomatology, and Risk Factors for Long COVID Symptoms: Population-Based, Multicenter Study, JMIR Public Health Surveill, doi:10.2196/42315
Wongsoemsin, Chinoraso, Yeekian, Symptom and Factors Affecting Severity of Long COVID, Chonburi Hosp. J
DOI record:
{
"DOI": "10.3390/medsci13030199",
"ISSN": [
"2076-3271"
],
"URL": "http://dx.doi.org/10.3390/medsci13030199",
"abstract": "<jats:p>Background: “Long COVID” refers to a condition in which individuals continue to experience persistent signs and symptoms even after recovering from the initial COVID-19 infection. Signs and symptoms that persist can affect multiple organs in the body. Vitamin D is an essential nutrient that plays a crucial role, particularly in the immune system, and may be linked to the development of long COVID. Objective: The study aimed to investigate the association between vitamin D levels and the prevalence of long COVID signs and symptoms in COVID-19 patients. Materials and Methods: The study enrolled 170 COVID-19 patients with mild signs and symptoms and confirmed COVID-Ag or RT-PCR tests. The subjects were aged 18–59 years. All patients had 25(OH)D levels measured within 60 days of COVID-19 diagnosis and had been followed for at least 3 months post-infection. Data collected included demographic characteristics, serum 25(OH)D levels, and self-reported long COVID signs and symptoms questionnaire responses. Results: The study results indicated a female-to-male ratio of 1.1:1 and a mean age of 45.87 ± 8.65 years; of these, 62.4% received three doses of the COVID-19 vaccine, and 64.7% developed long COVID. The most prevalent signs and symptoms were respiratory (55.3%), skin (50.6%), and general (39.4%). The median blood vitamin D level was 22.96 ng/mL, with 41.2% of subjects having insufficient levels, 30.6% having deficient levels, and 28.2% having sufficient levels. Patients with long COVID had significantly lower vitamin D levels compared with those without long COVID (21.52 ng/mL vs. 25.46 ng/mL; p < 0.05). Multivariable analysis found that vitamin D deficiency was significantly associated with overall long COVID signs and symptoms (Adj. OR, 5.80 [95% CI: 2.10, 16.13]). Additionally, vitamin D deficiency significantly increased the number of long COVID systemic signs and symptoms (Adj. IRR, 3.30 [2.12, 5.12]). Conclusion: Assessing and maintaining vitamin D levels, vitamin D supplementation, and sunlight exposure in COVID-19 patients can reduce the risk and severity of long-term COVID-19 signs and symptoms.</jats:p>",
"alternative-id": [
"medsci13030199"
],
"author": [
{
"affiliation": [
{
"name": "Department of Anti-Aging and Regenerative Medicine, School of Anti-Aging and Regenerative Medicine, Mae Fah Luang University, Bangkok 10110, Thailand"
}
],
"family": "Matangkha",
"given": "Karn",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Anti-Aging and Regenerative Medicine, School of Anti-Aging and Regenerative Medicine, Mae Fah Luang University, Bangkok 10110, Thailand"
}
],
"family": "Punyahotara",
"given": "Vichit",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Anti-Aging and Regenerative Medicine, School of Anti-Aging and Regenerative Medicine, Mae Fah Luang University, Bangkok 10110, Thailand"
}
],
"family": "Rintra",
"given": "Jarasphol",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-4103-9396",
"affiliation": [
{
"name": "Department of Anti-Aging and Regenerative Science, School of Anti-Aging and Regenerative Medicine, Mae Fah Luang University, Bangkok 10110, Thailand"
},
{
"name": "MAS Neuroscience Center, School of Anti-Aging and Regenerative Medicine, Mae Fah Luang University, Bangkok 10110, Thailand"
}
],
"authenticated-orcid": false,
"family": "Sittiprapaporn",
"given": "Phakkharawat",
"sequence": "additional"
}
],
"container-title": "Medical Sciences",
"container-title-short": "Medical Sciences",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
9,
18
]
],
"date-time": "2025-09-18T14:45:46Z",
"timestamp": 1758206746000
},
"deposited": {
"date-parts": [
[
2025,
9,
18
]
],
"date-time": "2025-09-18T15:28:24Z",
"timestamp": 1758209304000
},
"indexed": {
"date-parts": [
[
2025,
9,
19
]
],
"date-time": "2025-09-19T00:48:30Z",
"timestamp": 1758242910052,
"version": "3.44.0"
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2025,
9,
18
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2025,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
9,
18
]
],
"date-time": "2025-09-18T00:00:00Z",
"timestamp": 1758153600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-3271/13/3/199/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "199",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2025,
9,
18
]
]
},
"published-online": {
"date-parts": [
[
2025,
9,
18
]
]
},
"publisher": "MDPI AG",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-3271/13/3/199"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Association Between Vitamin D Levels and Long COVID Signs and Symptoms",
"type": "journal-article",
"volume": "13"
}
