Low vitamin D levels are associated with Long COVID syndrome in COVID-19 survivors
et al., The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgad207, Apr 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 50 COVID-19 patients with long COVID and 50 matched patients without long COVID, showing lower vitamin D levels associated with long COVID.
di Filippo et al., 13 Apr 2023, retrospective, Italy, peer-reviewed, 7 authors, study period 31 August, 2020 - 30 November, 2020.
Contact: giustina.andrea@hsr.it.
Low vitamin D levels are associated with Long COVID syndrome in COVID-19 survivors
doi:10.1210/clinem/dgad207/7116659
Purpose: Long-COVID is an emerging syndrome affecting 50-70% of COVID-19 survivors which still lacks predicting factors. Due to the extra-skeletal effects of vitamin D, we retrospectively assessed in COVID-19 survivors 6-months after hospitalization the association between 25(OH)vitamin D levels and Long-COVID. Methods: Long-COVID was defined according to NICE-guidelines. Fifty Long-COVID and 50 non-Long-COVID subjects matched on a 1:1-basis were enrolled from an outpatient-post-COVID clinic-cohort seen from August to November 2020. Therapies/comorbidities affecting calcium/vitamin-D/bone metabolism, and/or admission in ICU during hospitalization were exclusion criteria. 25(OH)vitamin D was measured at hospital-admission and 6-months after discharge.
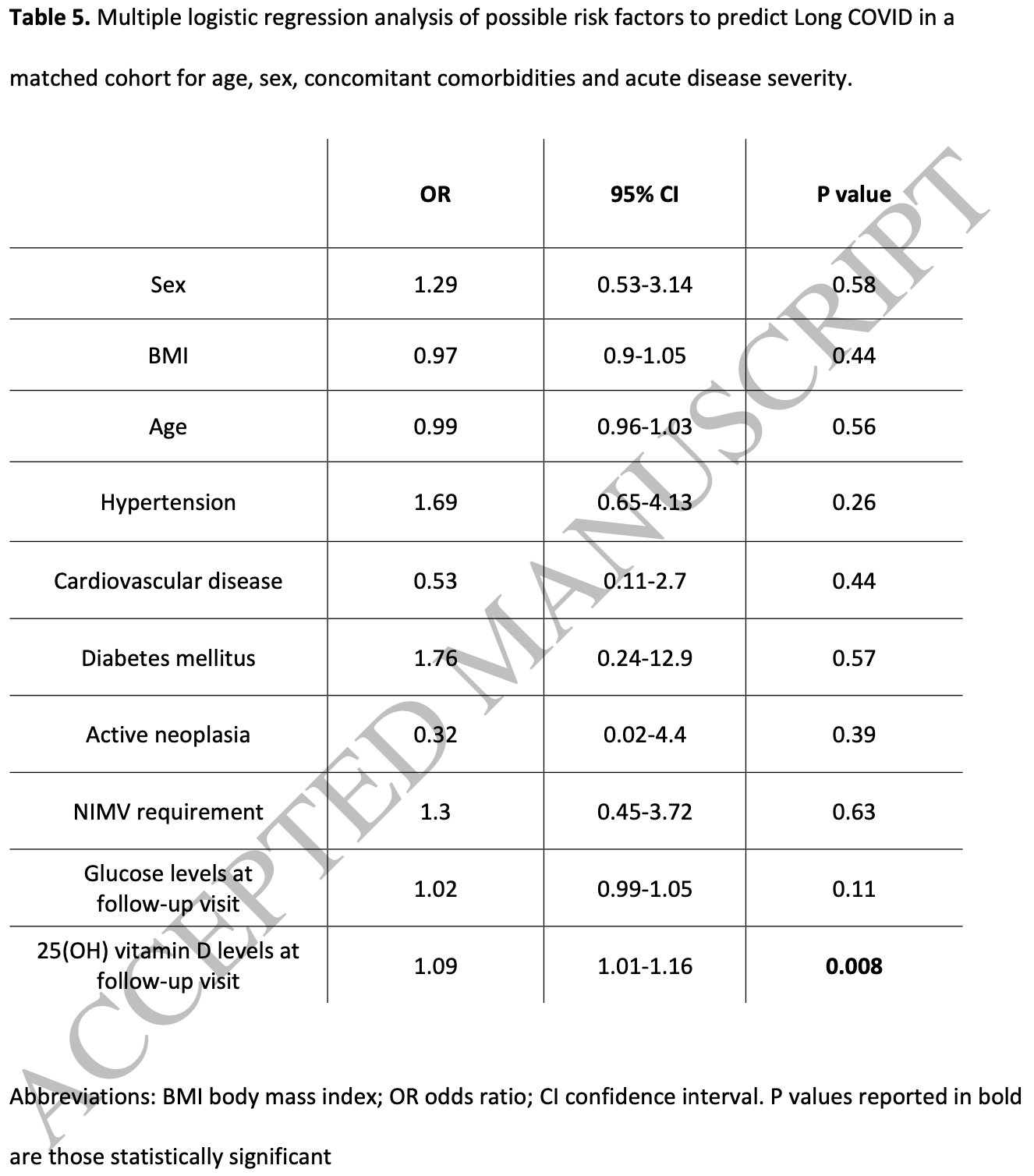
Results: We observed lower 25(OH)vitamin D levels, evaluated at follow-up, in subjects with Long-COVID than those without (20.1vs23.2 ng/mL-p=0.03). Regarding the affected health-areas evaluated in the entire cohort, we observed lower 25(OH)vitamin D levels in those with neurocognitive symptoms at follow-up (n.7) as compared to those without (n.93) (14.6vs20.6 ng/mL-p=0.042). In patients presenting vitamin D deficiency (<20 ng/mL) both at admission and at follow-up (n.42), those affected by Long-COVID (n.22) presented lower 25(OH)vitamin D levels, at follow-up, compared to those not affected (n.20) (12.7vs15.2 ng/mL-p=0.041). In multiple-regression analyses, lower 25(OH)vitamin D levels, at follow-up, resulted as the only variable significantly associated with Long-COVID in our cohort (p=0.008, OR 1.09-CI 1.01-1.16).
Conclusions : COVID-19 survivors with Long-COVID have lower 25(OH)vitamin D levels as compared to matched-patients without Long-COVID. Our data suggest that vitamin D levels should be evaluated in COVID-19 patients after hospital-discharge. Role of vitamin D supplementation as preventive strategy of COVID-19 sequelae should be tested in randomized-controlled trials.
References
Afzal, Bojesen, Nordestgaard, Low 25-hydroxyvitamin D and risk of type 2 diabetes: a prospective cohort study and metaanalysis, Clin Chem
Akbar, Wibowo, Pranata, Setiabudiawan, Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated With Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis [published correction appears, Front Nutr
Alkodaymi, Omrani, Fawzy, Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis, Clin Microbiol Infect, doi:10.1016/j.cmi.2022.01.014
Bianconi, Mannarino, Figorilli, Prevalence of vitamin D deficiency and its prognostic impact on patients hospitalized with COVID-19, Nutrition, doi:10.1016/j.nut.2021.111408
Bilezikian, Bikle, Hewison, MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19, Eur J Endocrinol, doi:10.1530/EJE-20-0665
Bilezikian, Binkley, Luca, Consensus and Controversial Aspects of Vitamin D and COVID-19
Bogliolo, Cereda, Klersy, Vitamin D 25OH Deficiency and Mortality in Moderate to Severe COVID-19: A Multi-Center Prospective Observational Study, Front Nutr, doi:10.3389/fnut.2022.934258
Bouillon, Marcocci, Carmeliet, Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions, Endocr Rev, doi:10.1210/er.2018-00126
Caballero-García, Pérez-Valdecantos, Guallar, Effect of Vitamin D Supplementation on Muscle Status in Old Patients Recovering from COVID-19 Infection, Medicina (Kaunas), doi:10.3390/medicina57101079
Campi, Gennari, Merlotti, Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy, BMC Infect Dis, doi:10.1186/s12879-021-06281-7
Charoenngam, Holick, Immunologic Effects of Vitamin D on Human Health and Disease, Nutrients, doi:10.3390/nu12072097
Chiodini, Gatti, Soranna, Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front Public Health, doi:10.3389/fpubh.2021.736665
Clemente, Sinatti, Cirella, Santini, Balsano, Alteration of Inflammatory Parameters and Psychological Post-Traumatic Syndrome in Long-COVID Patients, Int J Environ Res Public Health, doi:10.3390/ijerph19127103
Di Filippo, Allora, Doga, Vitamin D Levels Are Associated With Blood Glucose and BMI in COVID-19 Patients, Predicting Disease Severity, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab599
Di Filippo, Compagnone, Frara, Vertebral fractures at hospitalization predict impaired respiratory function during follow-up of COVID-19 survivors, Endocrine, doi:10.1007/s12020-022-03096-7
Di Filippo, Doga, Frara, Giustina, Hypocalcemia in COVID-19: Prevalence, clinical significance and therapeutic implications
Di Filippo, Formenti, Doga, Pedone, Rovere-Querini et al., Radiological Thoracic Vertebral Fractures are Highly Prevalent in COVID-19 and Predict Disease Outcomes, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa738
Di Filippo, Frara, Giustina, The emerging osteo-metabolic phenotype of COVID-19: clinical and pathophysiological aspects, Nat Rev Endocrinol, doi:10.1038/s41574-021-00516-y
Di Filippo, Uygur, Locatelli, Nannipieri, Frara et al., Low vitamin D levels predict outcomes of COVID-19 in patients with both severe and non-severe disease at hospitalization
Dissanayake, Silva, Sumanatilleke, Prognostic and Therapeutic Role of Vitamin D in COVID-19: Systematic Review and Meta-analysis, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab892
Dossari, Ahmad, Aljowair, Association of vitamin D with glycemic control in Saudi patients with type 2 diabetes: a retrospective chart review study in an emerging university hospital, J Clin Lab Anal
Ellis, Kelly, Shurlock, Hepburn, The role of vitamin D testing and replacement in fibromyalgia: a systematic literature review, BMC Rheumatol, doi:10.1186/s41927-018-0035-6
Fernandes, Sales, Santos, Caparbo, Murai et al., Persistent or new symptoms 1 year after a single high dose of vitamin D3 in patients with moderate to severe COVID-19, Front Nutr, doi:10.3389/fnut.2022.979667
Fernández-De-Las-Peñas, Palacios-Ceña, Gómez-Mayordomo, Cuadrado, Florencio, Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification, Int J Environ Res Public Health, doi:10.3390/ijerph18052621
Filippo, Formenti, Rovere-Querini, Hypocalcemia is highly prevalent and predicts hospitalization in patients with COVID-19, Endocrine, doi:10.1007/s12020-020-02383-5
Galluzzo, Ciciarello, Tosato, Association between vitamin D status and physical performance in COVID-19 survivors: Results from the Gemelli against COVID-19 post-acute care project, Mech Ageing Dev, doi:10.1016/j.mad.2022.111684
Garcia, Seelaender, Sotiropoulos, Coletti, Lancha, Vitamin D, muscle recovery, sarcopenia, cachexia, and muscle atrophy, Nutrition, doi:10.1016/j.nut.2018.09.031
Giustina, Adler, Binkley, Consensus statement from 2nd International Conference on Controversies in Vitamin D, Rev Endocr Metab Disord, doi:10.1007/s11154-019-09532-w
Giustina, Bouillon, Binkley, Controversies in Vitamin D: A Statement From the Third International Conference, JBMR Plus, doi:10.1002/jbm4.10417
Giustina, Hypovitaminosis D and the endocrine phenotype of COVID-19, Endocrine, doi:10.1007/s12020-021-02671-8
Gáll, Székely, Role of Vitamin D in Cognitive Dysfunction: New Molecular Concepts and Discrepancies between Animal and Human Findings, Nutrients, doi:10.3390/nu13113672
Haugen, Basnet, Hardang, Vitamin D status is associated with treatment failure and duration of illness in Nepalese children with severe pneumonia, Pediatr Res, doi:10.1038/pr.2017.71
Hussein, Galal, Amin, Prevalence of vitamin D deficiency among patients attending Post COVID-19 follow-up clinic: a cross-sectional study, Eur Rev Med Pharmacol Sci, doi:10.26355/eurrev_202204_28635
Jolliffe, Camargo, Jr, Sluyter, Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00051-6
Kalichuran, Van Blydenstein, Venter, Omar, Vitamin D status and COVID-19 severity, S Afr J Infect Dis, doi:10.4102/sajid.v37i1.359
Khairy, Attia, Protective effects of vitamin D on neurophysiologic alterations in brain aging: role of brain-derived neurotrophic factor (BDNF), Nutr Neurosci, doi:10.1080/1028415X.2019.1665854
Lai, Yang, Sun, Risk of incident diabetes after COVID-19 infection: A systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155330
Lorenzo, Conte, Lanzani, Residual clinical damage after COVID-19: A retrospective and prospective observational cohort study, PLoS One, doi:10.1371/journal.pone.0239570
Maddaloni, Cavallari, Napoli, Conte, Vitamin D and Diabetes Mellitus, Front Horm Res, doi:10.1159/000486083
Maglietta, Diodati, Puntoni, Prognostic Factors for Post-COVID-19 Syndrome: A Systematic Review and Meta-Analysis, J Clin Med, doi:10.3390/jcm11061541
Makrani, Afshari, Ghajar, Forooghi, Moosazadeh, Vitamin D and fibromyalgia: a meta-analysis, Korean J Pain, doi:10.3344/kjp.2017.30.4.250
Mandal, Barnett, Brill, Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19
Notarte, De Oliveira, Peligro, Sex and Previous Comorbidities as Risk Factors Not Associated with SARS-CoV-2 Infection for Long COVID-19: A Systematic Review and Meta-Analysis, J Clin Med, doi:10.3390/jcm11247314
Nowaczewska, Wiciński, Osiński, Kaźmierczak, The Role of Vitamin D in Primary Headache-from Potential Mechanism to Treatment, Nutrients, doi:10.3390/nu12010243
Olsson, Saini, Strömberg, Evidence for Vitamin D Receptor Expression and Direct Effects of 1α,25(OH)2D3 in Human Skeletal Muscle Precursor Cells, Endocrinology, doi:10.1210/en.2015-1685
Parra-Ortega, Alcara-Ramírez, Ronzon-Ronzon, 25-Hydroxyvitamin D level is associated with mortality in patients with critical COVID-19: a prospective observational study in Mexico City, Nutr Res Pract, doi:10.4162/nrp.2021.15.S1.S32
Plotnikoff, Quigley, Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain, Mayo Clin Proc
Puig-Domingo, Marazuela, Yildiz, Giustina, COVID-19 and endocrine and metabolic diseases. An updated statement from the European Society of Endocrinology, Endocrine, doi:10.1007/s12020-021-02734-w
Querini, Lorenzo, Conte, Post-COVID-19 follow-up clinic: depicting chronicity of a new disease, Acta Biomed, doi:10.23750/abm.v91i9-S.10146
Raveendran, Misra, Post COVID-19 Syndrome ("Long COVID") and Diabetes: Challenges in Diagnosis and Management, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.102235
Rovere-Querini, Tresoldi, Conte, Ruggeri, Ghezzi et al., Biobanking for COVID-19 research, Panminerva Med, doi:10.23736/S0031-0808.20.04168-3
Sempos, Heijboer, Bikle, Vitamin D assays and the definition of hypovitaminosis D: results from the First International Conference on Controversies in Vitamin D, Br J Clin Pharmacol, doi:10.1111/bcp.13652
Sivan, Taylor, NICE guideline on long covid, BMJ, doi:10.1136/bmj.m4938
Su, Yuan, Chen, Multiple early factors anticipate post-acute COVID-19 sequelae, Cell, doi:10.1016/j.cell.2022.01.014
Tecilazich, Formenti, Giustina, Role of vitamin D in diabetic retinopathy: Pathophysiological and clinical aspects, Rev Endocr Metab Disord, doi:10.1007/s11154-020-09575-4
Townsend, Dyer, Mccluskey, Investigating the Relationship between Vitamin D and Persistent Symptoms Following SARS-CoV-2 Infection, Nutrients, doi:10.3390/nu13072430
Tsur, Feldman, Feldhammer, Hoshen, Leibowitz et al., Decreased serum concentrations of 25-hydroxycholecalciferol are associated with increased risk of progression to impaired fasting glucose and diabetes, Diabetes Care
Wagatsuma, Sakuma, Vitamin D signaling in myogenesis: potential for treatment of sarcopenia, Biomed Res Int, doi:10.1155/2014/121254
Xie, Al-Aly, Risks and burdens of incident diabetes in long COVID: a cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(22)00044-4
Zhang, Mei, Zhang, Risk for newly diagnosed diabetes after COVID-19: a systematic review and meta-analysis, BMC Med, doi:10.1186/s12916-022-02656-y
DOI record:
{
"DOI": "10.1210/clinem/dgad207",
"ISSN": [
"0021-972X",
"1945-7197"
],
"URL": "http://dx.doi.org/10.1210/clinem/dgad207",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Purpose</jats:title>\n <jats:p>Long-COVID is an emerging syndrome affecting 50-70% of COVID-19 survivors which still lacks predicting factors. Due to the extra-skeletal effects of vitamin D, we retrospectively assessed in COVID-19 survivors 6-months after hospitalization the association between 25(OH)vitamin D levels and Long-COVID.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Long-COVID was defined according to NICE-guidelines. Fifty Long-COVID and 50 non-Long-COVID subjects matched on a 1:1-basis were enrolled from an outpatient-post-COVID clinic-cohort seen from August to November 2020. Therapies/comorbidities affecting calcium/vitamin-D/bone metabolism, and/or admission in ICU during hospitalization were exclusion criteria. 25(OH)vitamin D was measured at hospital-admission and 6-months after discharge.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>We observed lower 25(OH)vitamin D levels, evaluated at follow-up, in subjects with Long-COVID than those without (20.1vs23.2 ng/mL-p = 0.03). Regarding the affected health-areas evaluated in the entire cohort, we observed lower 25(OH)vitamin D levels in those with neurocognitive symptoms at follow-up (n.7) as compared to those without (n.93) (14.6vs20.6 ng/mL-p = 0.042). In patients presenting vitamin D deficiency (&lt;20 ng/mL) both at admission and at follow-up (n.42), those affected by Long-COVID (n.22) presented lower 25(OH)vitamin D levels, at follow-up, compared to those not affected (n.20) (12.7vs15.2 ng/mL-p = 0.041). In multiple-regression analyses, lower 25(OH)vitamin D levels, at follow-up, resulted as the only variable significantly associated with Long-COVID in our cohort (p = 0.008, OR 1.09-CI 1.01-1.16).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>COVID-19 survivors with Long-COVID have lower 25(OH)vitamin D levels as compared to matched-patients without Long-COVID. Our data suggest that vitamin D levels should be evaluated in COVID-19 patients after hospital-discharge. Role of vitamin D supplementation as preventive strategy of COVID-19 sequelae should be tested in randomized-controlled trials.</jats:p>\n </jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Institute of Endocrine and Metabolic Sciences, Università Vita-Salute San Raffaele , IRCCS Ospedale San Raffaele, Milan , Italy"
}
],
"family": "di Filippo",
"given": "Luigi",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Institute of Endocrine and Metabolic Sciences, Università Vita-Salute San Raffaele , IRCCS Ospedale San Raffaele, Milan , Italy"
}
],
"family": "Frara",
"given": "Stefano",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Research, Abiogen Pharma , Pisa , Italy"
}
],
"family": "Nannipieri",
"given": "Fabrizio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Laboratory Medicine Service , IRCCS Ospedale San Raffaele, Milan , Italy"
}
],
"family": "Cotellessa",
"given": "Alice",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Laboratory Medicine Service , IRCCS Ospedale San Raffaele, Milan , Italy"
}
],
"family": "Locatelli",
"given": "Massimo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2615-3649",
"affiliation": [
{
"name": "Division of Immunology, Transplantation & Infectious Diseases, Università Vita-Salute San Raffaele , IRCCS Ospedale San Raffaele, Milan , Italy"
}
],
"authenticated-orcid": false,
"family": "Rovere Querini",
"given": "Patrizia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6783-3398",
"affiliation": [
{
"name": "Institute of Endocrine and Metabolic Sciences, Università Vita-Salute San Raffaele , IRCCS Ospedale San Raffaele, Milan , Italy"
}
],
"authenticated-orcid": false,
"family": "Giustina",
"given": "Andrea",
"sequence": "additional"
}
],
"container-title": "The Journal of Clinical Endocrinology & Metabolism",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
4,
13
]
],
"date-time": "2023-04-13T07:43:41Z",
"timestamp": 1681371821000
},
"deposited": {
"date-parts": [
[
2023,
4,
13
]
],
"date-time": "2023-04-13T07:43:42Z",
"timestamp": 1681371822000
},
"indexed": {
"date-parts": [
[
2023,
4,
14
]
],
"date-time": "2023-04-14T05:16:11Z",
"timestamp": 1681449371031
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
4,
13
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "am",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
13
]
],
"date-time": "2023-04-13T00:00:00Z",
"timestamp": 1681344000000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/jcem/advance-article-pdf/doi/10.1210/clinem/dgad207/49873434/dgad207.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/jcem/advance-article-pdf/doi/10.1210/clinem/dgad207/49873434/dgad207.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "80",
"original-title": [],
"prefix": "10.1210",
"published": {
"date-parts": [
[
2023,
4,
13
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
13
]
]
},
"publisher": "The Endocrine Society",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgad207/7116659"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biochemistry (medical)",
"Clinical Biochemistry",
"Endocrinology",
"Biochemistry",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Low vitamin D levels are associated with Long COVID syndrome in COVID-19 survivors",
"type": "journal-article"
}
