A Dual Pharmacological Strategy against COVID-19: The Therapeutic Potential of Metformin and Atorvastatin
et al., Microorganisms, doi:10.3390/microorganisms12020383, Feb 2024
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
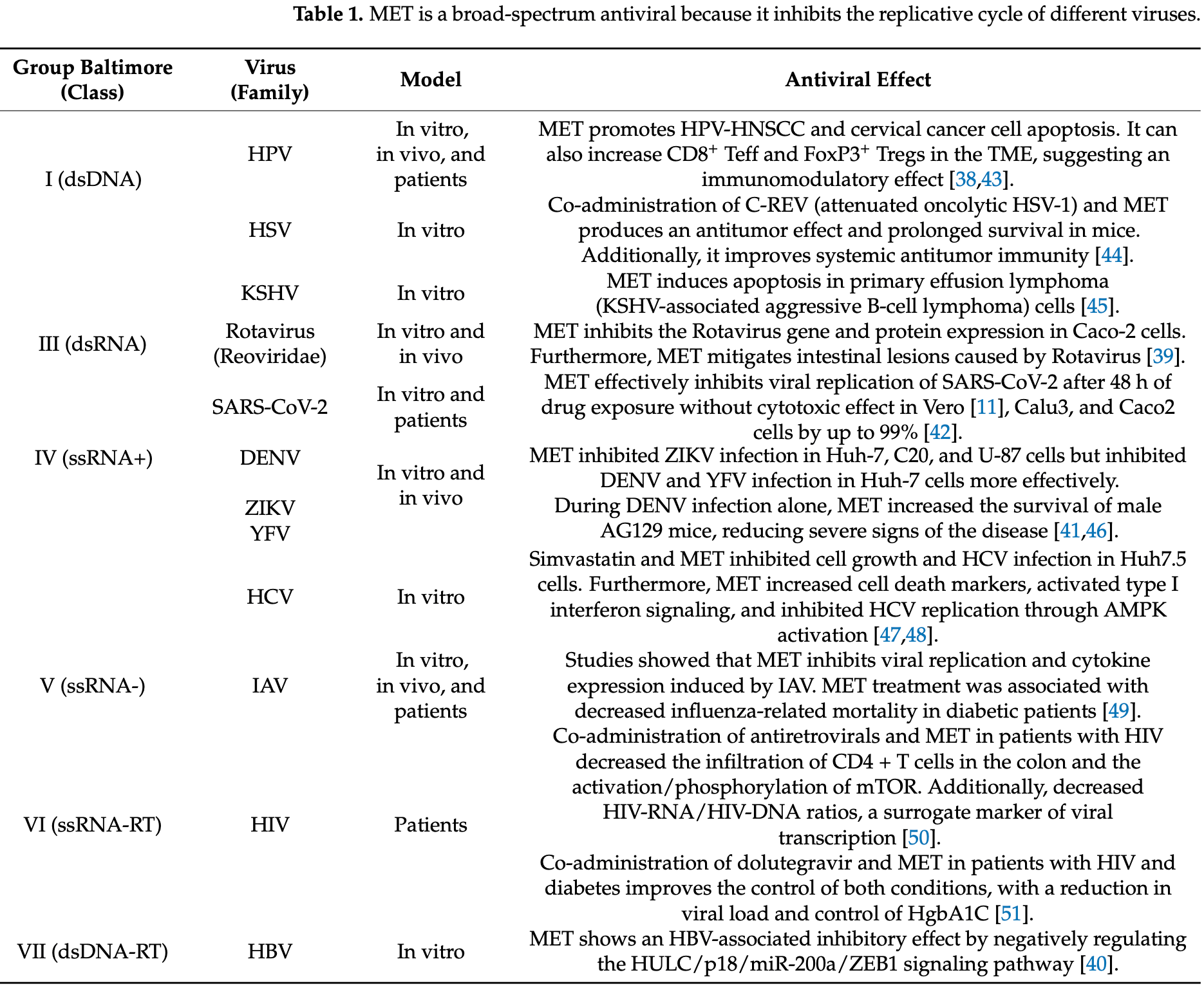
Review of the therapeutic potential of metformin and atorvastatin against COVID-19. Authors discuss the immunomodulatory and antiviral capabilities of these commonly prescribed diabetes and cholesterol medications. They note metformin's ability to inhibit SARS-CoV-2 replication by activating AMPK, reducing inflammation, and potentially preventing viral entry by phosphorylating the ACE2 receptor. Meanwhile atorvastatin may disrupt lipid metabolism required for viral replication and assembly. Retrospective studies suggest reduced COVID-19 mortality and severity among patients already taking these drugs. Authors suggest that the wide availability, safety profiles, and low costs of metformin and atorvastatin make them promising candidates for repurposing against SARS-CoV-2.
1.
Monsalve et al., NETosis: A key player in autoimmunity, COVID-19, and long COVID, Journal of Translational Autoimmunity, doi:10.1016/j.jtauto.2025.100280.
2.
Halabitska et al., Metformin in Antiviral Therapy: Evidence and Perspectives, Viruses, doi:10.3390/v16121938.
3.
Plowman et al., Anti-Inflammatory Potential of the Anti-Diabetic Drug Metformin in the Prevention of Inflammatory Complications and Infectious Diseases Including COVID-19: A Narrative Review, International Journal of Molecular Sciences, doi:10.3390/ijms25105190.
4.
De Jesús-González et al., A Dual Pharmacological Strategy against COVID-19: The Therapeutic Potential of Metformin and Atorvastatin, Microorganisms, doi:10.3390/microorganisms12020383.
5.
Halma et al., Exploring autophagy in treating SARS-CoV-2 spike protein-related pathology, Endocrine and Metabolic Science, doi:10.1016/j.endmts.2024.100163.
6.
Zhang et al., SARS-CoV-2 ORF3a Protein as a Therapeutic Target against COVID-19 and Long-Term Post-Infection Effects, Pathogens, doi:10.3390/pathogens13010075.
7.
Gomaa et al., Pharmacological evaluation of vitamin D in COVID-19 and long COVID-19: recent studies confirm clinical validation and highlight metformin to improve VDR sensitivity and efficacy, Inflammopharmacology, doi:10.1007/s10787-023-01383-x.
De Jesús-González et al., 13 Feb 2024, retrospective, placebo-controlled, Mexico, peer-reviewed, 15 authors.
Contact: luis.dejesus@cinvestav.mx (corresponding author), rdz.carlos09@hotmail.com, taneiro87@hotmail.com, rondo_vm@yahoo.com, ana.garciaher@imss.gob.mx, ramcor16@hotmail.com, erykagandara@gmail.com, estefania_940@yahoo.com.mx, selvin.palacios@cinvestav.mx, carlos.cordero@cinvestav.mx, carlos.farfan@cinvestav.mx, osunajuanfidel.fm@uas.edu.mx, jose.reyesr@imss.gob.mx, moisesleoninper@gmail.com, rmangel@cinvestav.mx.
A Dual Pharmacological Strategy against COVID-19: The Therapeutic Potential of Metformin and Atorvastatin
Microorganisms, doi:10.3390/microorganisms12020383
Metformin (MET) and atorvastatin (ATO) are promising treatments for COVID-19. This review explores the potential of MET and ATO, commonly prescribed for diabetes and dyslipidemia, respectively, as versatile medicines against SARS-CoV-2. Due to their immunomodulatory and antiviral capabilities, as well as their cost-effectiveness and ubiquitous availability, they are highly suitable options for treating the virus. MET's effect extends beyond managing blood sugar, impacting pathways that can potentially decrease the severity and fatality rates linked with COVID-19. It can partially block mitochondrial complex I and stimulate AMPK, which indicates that it can be used more widely in managing viral infections. ATO, however, impacts cholesterol metabolism, a crucial element of the viral replicative cycle, and demonstrates anti-inflammatory characteristics that could modulate intense immune reactions in individuals with COVID-19. Retrospective investigations and clinical trials show decreased hospitalizations, severity, and mortality rates in patients receiving these medications. Nevertheless, the journey from observing something to applying it in a therapeutic setting is intricate, and the inherent diversity of the data necessitates carefully executed, forwardlooking clinical trials. This review highlights the requirement for efficacious, easily obtainable, and secure COVID-19 therapeutics and identifies MET and ATO as promising treatments in this worldwide health emergency.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Abdelmoneim, Eissa, Aboalela, Naoe, Matsumura et al., Metformin Enhances the Antitumor Activity of Oncolytic Herpes Simplex Virus HF10 (Canerpaturev) in a Pancreatic Cell Cancer Subcutaneous Model, Sci. Rep, doi:10.1038/s41598-022-25065-w
Akkiz, Implications of the Novel Mutations in the SARS-CoV-2 Genome for Transmission, Disease Severity, and the Vaccine Development, Front. Med, doi:10.3389/fmed.2021.636532
Al-Kuraishy, Al-Gareeb, Saad, Batiha, The Potential Therapeutic Effect of Statins in Multiple Sclerosis: Beneficial or Detrimental Effects, Inflammopharmacology, doi:10.1007/s10787-023-01240-x
Badr, Kurban, Abbas, Metformin in Dermatology: An Overview, J. Eur. Acad. Dermatol. Venereol, doi:10.1111/jdv.12116
Bailey, Turner, Metformin, None, N. Engl. J. Med, doi:10.1056/NEJM199602293340906
Bian, Li, Angiotensin-Converting Enzyme 2 (ACE2): SARS-CoV-2 Receptor and RAS Modulator, Acta Pharm. Sin. B, doi:10.1016/j.apsb.2020.10.006
Blankier, Mccrindle, Ito, Yeung, The Role of Atorvastatin in Regulating the Immune Response Leading to Vascular Damage in a Model of Kawasaki Disease, Clin. Exp. Immunol, doi:10.1111/j.1365-2249.2011.04331.x
Boulware, Bramante, Pullen, Buse, Odde et al., Metformin Reduced SARS-CoV-2 Viral Load in a Phase 3 Randomized Clinical Trial, Top. Antivir. Med
Bramante, Buse, Liebovitz, Nicklas, Puskarich et al., Outpatient Treatment of COVID-19 and Incidence of Post-COVID-19 Condition over 10 Months (COVID-OUT): A Multicentre, Randomised, Quadruple-Blind, Parallel-Group, Phase 3 Trial, Lancet Infect. Dis, doi:10.1016/S1473-3099(23)00299-2
Bramante, Huling, Tignanelli, Buse, Liebovitz et al., Randomized Trial of Metformin, Ivermectin, and Fluvoxamine for COVID-19, N. Engl. J. Med, doi:10.1056/NEJMoa2201662
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and Risk of Mortality in Patients Hospitalised with COVID-19: A Retrospective Cohort Analysis, Lancet Healthy Longev, doi:10.1016/S2666-7568(20)30033-7
Bryan-Marrugo, Arellanos-Soto, Rojas-Martinez, Barrera-Saldaña, Ramos-Jimenez et al., The Anti-dengue Virus Properties of Statins May Be Associated with Alterations in the Cellular Antiviral Profile Expression, Mol. Med. Rep, doi:10.3892/mmr.2016.5519
Calza, Trapani, Bartoletti, Manfredi, Colangeli et al., Statin Therapy Decreases Serum Levels of High-Sensitivity C-Reactive Protein and Tumor Necrosis Factor-α in HIV-Infected Patients Treated with Ritonavir-Boosted Protease Inhibitors, HIV Clin. Trials, doi:10.1310/hct1303-153
Carro, Damonte, Requirement of Cholesterol in the Viral Envelope for Dengue Virus Infection, Virus Res, doi:10.1016/j.virusres.2013.03.005
Cascella, Rajnik, Aleem, Dulebohn, Di Napoli et al., Evaluation, and Treatment of Coronavirus (COVID-19)
Chaudhary, Kurundkar, Elmets, Kopelovich, Athar et al., an Antidiabetic Agent Reduces Growth of Cutaneous Squamous Cell Carcinoma by Targeting mTOR Signaling Pathway †, Photochem. Photobiol, doi:10.1111/j.1751-1097.2012.01165.x
Chen, Guo, Qiu, Zhang, Deng et al., Immunomodulatory and Antiviral Activity of Metformin and Its Potential Implications in Treating Coronavirus Disease 2019 and Lung Injury, Front. Immunol, doi:10.3389/fimmu.2020.02056
Chen, Quach, Combining Immunomodulators and Antivirals for COVID-19, Lancet Microbe, doi:10.1016/S2666-5247(21)00114-2
Chi, Wang, Huang, Stamnes, Chen, Roles of Rho GTPases in Intracellular Transport and Cellular Transformation, Int. J. Mol. Sci, doi:10.3390/ijms14047089
Chong, Seeger, Atorvastatin Calcium: An Addition to HMG-CoA Reductase Inhibitors, Pharmacotherapy, doi:10.1002/j.1875-9114.1997.tb03081.x
Conde, Pineda, Newton, Fernandez, Hypocholesterolemic Effects of 3-Hydroxy-3-Methylglutaryl Coenzyme A (HMG-CoA) Reductase Inhibitors in the Guinea Pig: Atorvastatin versus Simvastatin, Biochem. Pharmacol, doi:10.1016/S0006-2952(99)00203-8
Corcoran, Jacobs, Metformin, None
Cortés, Brischetto, Martinez-Campanario, Ninfali, Domínguez et al., Inflammatory Macrophages Reprogram to Immunosuppression by Reducing Mitochondrial Translation, Nat. Commun, doi:10.1038/s41467-023-42277-4
Curry, Johnson, Mollaee, Tassone, Amin et al., Metformin Clinical Trial in HPV+ and HPV-Head and Neck Squamous Cell Carcinoma: Impact on Cancer Cell Apoptosis and Immune Infiltrate, Front. Oncol, doi:10.3389/fonc.2018.00436
Davoodi, Jafarpour, Oladi, Zakariaei, Tabarestani et al., Atorvastatin Therapy in COVID-19 Adult Inpatients: A Double-Blind, Randomized Controlled Trial, Int. J. Cardiol. Heart Vasc, doi:10.1016/j.ijcha.2021.100875
Defronzo, Goodman, Efficacy of Metformin in Patients with Non-Insulin-Dependent Diabetes Mellitus, N. Engl. J. Med, doi:10.1056/NEJM199508313330902
Del Campo, García, Valdecasas, Gil Gómez, Rojas Alvarez-Ossorio et al., Simvastatin and Metformin Inhibit Cell Growth in Hepatitis C Virus Infected Cells via mTOR Increasing PTEN and Autophagy, PLoS ONE, doi:10.1371/journal.pone.0191805
Ding, Liang, Yao, Zhang, Liu et al., Metformin Prevents Cancer Metastasis by Inhibiting M2-like Polarization of Tumor Associated Macrophages, Oncotarget, doi:10.18632/oncotarget.5541
Duarte, Copertino, Iñiguez, Marston, Bram et al., Identifying FDA-Approved Drugs with Multimodal Properties against COVID-19 Using a Data-Driven Approach and a Lung Organoid Model of SARS-CoV-2 Entry, Mol. Med, doi:10.1186/s10020-021-00356-6
El-Mir, Nogueira, Fontaine, Avéret, Rigoulet et al., Dimethylbiguanide Inhibits Cell Respiration via an Indirect Effect Targeted on the Respiratory Chain Complex I, J. Biol. Chem, doi:10.1074/jbc.275.1.223
Endo, The Discovery and Development of HMG-CoA Reductase Inhibitors, J. Lipid Res, doi:10.1016/S0022-2275(20)41379-3
Episcopio, Aminov, Benjamin, Germain, Datan et al., Atorvastatin Restricts the Ability of Influenza Virus to Generate Lipid Droplets and Severely Suppresses the Replication of the Virus, FASEB J, doi:10.1096/fj.201900428RR
Españo, Kim, Effects of Statin Combinations on Zika Virus Infection in Vero Cells, Pharmaceutics, doi:10.3390/pharmaceutics15010050
Farfan-Morales, Cordero-Rivera, Osuna-Ramos, Monroy-Muñoz, De Jesús-González et al., The Antiviral Effect of Metformin on Zika and Dengue Virus Infection, Sci. Rep, doi:10.1038/s41598-021-87707-9
Farfan-Morales, Cordero-Rivera, Reyes-Ruiz, Hurtado-Monzón, Osuna-Ramos et al., Anti-Flavivirus Properties of Lipid-Lowering Drugs, Front. Physiol, doi:10.3389/fphys.2021.749770
Fessler, Regulation of Adaptive Immunity in Health and Disease by Cholesterol Metabolism, Curr. Allergy Asthma Rep, doi:10.1007/s11882-015-0548-7
Fontaine, Metformin-Induced Mitochondrial Complex I Inhibition: Facts, Uncertainties, and Consequences, Front. Endocrinol, doi:10.3389/fendo.2018.00753
Foretz, Guigas, Bertrand, Pollak, Viollet, Metformin: From Mechanisms of Action to Therapies, Cell Metab, doi:10.1016/j.cmet.2014.09.018
Frid, Sterner, Löndahl, Wiklander, Cato et al., Novel Assay of Metformin Levels in Patients with Type 2 Diabetes and Varying Levels of Renal Function: Clinical Recommendations, Diabetes Care, doi:10.2337/dc09-1284
Fullerton, Galic, Marcinko, Sikkema, Pulinilkunnil et al., Single Phosphorylation Sites in Acc1 and Acc2 Regulate Lipid Homeostasis and the Insulin-Sensitizing Effects of Metformin, Nat. Med, doi:10.1038/nm.3372
Ganesan, Crum-Cianflone, Higgins, Qin, Rehm et al., High Dose Atorvastatin Decreases Cellular Markers of Immune Activation without Affecting HIV-1 RNA Levels: Results of a Double-Blind Randomized Placebo Controlled Clinical Trial, J. Infect. Dis, doi:10.1093/infdis/jiq115
Gheblawi, Wang, Viveiros, Nguyen, Zhong et al., Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System, Circ. Res, doi:10.1161/CIRCRESAHA.120.317015
Giannarelli, Aragona, Coppelli, Del Prato, Reducing Insulin Resistance with Metformin: The Evidence Today, Diabetes Metab, doi:10.1016/S1262-3636(03)72785-2
Goldstein, Brown, Regulation of the Mevalonate Pathway, Nature, doi:10.1038/343425a0
Granato, Gilardini Montani, Romeo, Santarelli, Gonnella et al., Metformin Triggers Apoptosis in PEL Cells and Alters Bortezomib-Induced Unfolded Protein Response Increasing Its Cytotoxicity and Inhibiting KSHV Lytic Cycle Activation, Cell. Signal, doi:10.1016/j.cellsig.2017.09.020
Guan, Sun, Liang, Dong, Zhang et al., Atorvastatin Attenuates Coxsackie Virus B3m-Induced Viral Myocarditis in Mice, J. Cardiovasc. Pharmacol, doi:10.1097/FJC.0b013e3181f6b28d
Haji Aghajani, Moradi, Azhdari Tehrani, Amini, Pourheidar et al., Promising Effects of Atorvastatin on Mortality and Need for Mechanical Ventilation in Patients with Severe COVID-19; a Retrospective Cohort Study, Int. J. Clin. Pract, doi:10.1111/ijcp.14434
Hawley, Boudeau, Reid, Mustard, Udd et al., Complexes between the LKB1 Tumor Suppressor, STRAD Alpha/Beta and MO25 Alpha/Beta Are Upstream Kinases in the AMP-Activated Protein Kinase Cascade, J. Biol, doi:10.1186/1475-4924-2-28
Hawley, Pan, Mustard, Ross, Bain et al., Calmodulin-Dependent Protein Kinase Kinase-Beta Is an Alternative Upstream Kinase for AMP-Activated Protein Kinase, Cell Metab, doi:10.1016/j.cmet.2005.05.009
Hawley, Ross, Chevtzoff, Green, Evans et al., Use of Cells Expressing Gamma Subunit Variants to Identify Diverse Mechanisms of AMPK Activation, Cell Metab, doi:10.1016/j.cmet.2010.04.001
Herrera-Moro Huitron, De Jesús-González, Martínez-Castillo, Ulloa-Aguilar, Cabello-Gutierrez et al., Multifaceted Nature of Lipid Droplets in Viral Interactions and Pathogenesis, Microorganisms, doi:10.3390/microorganisms11071851
Honda, Shirasaki, Terashima, Kawaguchi, Nakamura et al., Hepatitis B Virus (HBV) Core-Related Antigen During Nucleos(t)Ide Analog Therapy Is Related to Intra-Hepatic HBV Replication and Development of Hepatocellular Carcinoma, J. Infect. Dis, doi:10.1093/infdis/jiv572
Hoppe-Seyler, Herrmann, Däschle, Kuhn, Strobel et al., Effects of Metformin on the Virus/Host Cell Crosstalk in Human Papillomavirus-Positive Cancer Cells, Int. J. Cancer, doi:10.1002/ijc.33594
Huang, Wang, Li, Ren, Zhao et al., Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Ianevski, Yao, Zusinaite, Lysvand, Oksenych et al., Active Components of Commonly Prescribed Medicines Affect Influenza A Virus-Host Cell Interaction: A Pilot Study, Viruses, doi:10.3390/v13081537
Ikeda, Abe, Yamada, Dansako, Naka et al., Different Anti-HCV Profiles of Statins and Their Potential for Combination Therapy with Interferon, Hepatology, doi:10.1002/hep.21232
Ikeda, Kato, Life Style-Related Diseases of the Digestive System: Cell Culture System for the Screening of Anti-Hepatitis C Virus (HCV) Reagents: Suppression of HCV Replication by Statins and Synergistic Action with Interferon, J. Pharmacol. Sci, doi:10.1254/jphs.FM0070050
Investigators, Atorvastatin versus Placebo in Patients with COVID-19 in Intensive Care: Randomized Controlled Trial, BMJ, doi:10.1136/bmj-2021-068407
Jiang, Liu, Metformin Inhibits Tumorigenesis in HBV-Induced Hepatocellular Carcinoma by Suppressing HULC Overexpression Caused by HBX, J. Cell Biochem, doi:10.1002/jcb.26555
Kelly, Tannahill, Murphy, O'neill, Metformin Inhibits the Production of Reactive Oxygen Species from NADH:Ubiquinone Oxidoreductase to Limit Induction of Interleukin-1β (IL-1β) and Boosts Interleukin-10 (IL-10) in Lipopolysaccharide (LPS)-Activated Macrophages *, J. Biol. Chem, doi:10.1074/jbc.M115.662114
Kouhpeikar, Khosaravizade Tabasi, Khazir, Naghipour, Mohammadi Moghadam et al., Statin Use in COVID-19 Hospitalized Patients and Outcomes: A Retrospective Study, Front. Cardiovasc. Med, doi:10.3389/fcvm.2022.820260
Kumar, Liu, Wu, Drug Repurposing against SARS-CoV-2 Receptor Binding Domain Using Ensemble-Based Virtual Screening and Molecular Dynamics Simulations, Comput. Biol. Med, doi:10.1016/j.compbiomed.2021.104634
Kumari, Lu, Li, Huang, Hsu et al., A Critical Overview of Current Progress for COVID-19: Development of Vaccines, Antiviral Drugs, and Therapeutic Antibodies, J. Biomed. Sci, doi:10.1186/s12929-022-00852-9
Lamoia, Shulman, Cellular and Molecular Mechanisms of Metformin Action, Endocr. Rev, doi:10.1210/endrev/bnaa023
Lee, Noh, Song, Cheong, Kim, Metformin Reduces the Risk of Developing Influenza A Virus Related Cardiovascular Disease, Heliyon, doi:10.1016/j.heliyon.2023.e20284
Li, Hilgenfeld, Whitley, De Clercq, Therapeutic Strategies for COVID-19: Progress and Lessons Learned, Nat. Rev. Drug Discov, doi:10.1038/s41573-023-00672-y
Li, Zhang, Zhang, Zhang, Gu et al., Neutrophils in COVID-19: Recent Insights and Advances, Virol. J, doi:10.1186/s12985-023-02116-w
Liu, Yu, Xu, Wang, Chen et al., Metformin Induces Tolerogenicity of Dendritic Cells by Promoting Metabolic Reprogramming, Cell Mol. Life Sci, doi:10.1007/s00018-023-04932-3
Lv, Guo, Metformin and Its Benefits for Various Diseases, Front. Endocrinol, doi:10.3389/fendo.2020.00191
Madiraju, Erion, Rahimi, Zhang, Braddock et al., Metformin Suppresses Gluconeogenesis by Inhibiting Mitochondrial Glycerophosphate Dehydrogenase, Nature, doi:10.1038/nature13270
Marcianò, Palleria, Casarella, Rania, Basile et al., Effect of Statins on Lung Cancer Molecular Pathways: A Possible Therapeutic Role, Pharmaceuticals, doi:10.3390/ph15050589
Marcucci, Romeo, Caserta, Rumio, Lefoulon, Context-Dependent Pharmacological Effects of Metformin on the Immune System, Trends Pharmacol. Sci, doi:10.1016/j.tips.2020.01.003
Masich, Thompson, Fulco, Bictegravir and Metformin Drug-Drug Interaction in People with Human Immunodeficiency Virus (HIV), Infect. Dis. Rep, doi:10.3390/idr15030024
Mills, M1 and M2 Macrophages: Oracles of Health and Disease, CRI, doi:10.1615/CritRevImmunol.v32.i6.10
Moreno-Corona, López-Ortega, Pérez-Martínez, Martínez-Castillo, De Jesús-González et al., Dynamics of the Microbiota and Its Relationship with Post-COVID-19 Syndrome, Int. J. Mol. Sci, doi:10.3390/ijms241914822
Mystakelis, Wilson, Laidlaw, Poole, Krishnan et al., An Open Label Randomized Controlled Trial of Atorvastatin versus Aspirin in Elite Controllers and Antiretroviral-Treated People with HIV, AIDS, doi:10.1097/QAD.0000000000003656
Nasri, Rafieian-Kopaei, Metformin: Current Knowledge, J. Res. Med. Sci
Negredo, Clotet, Puig, Pérez-Alvarez, Ruiz et al., The Effect of Atorvastatin Treatment on HIV-1-Infected Patients Interrupting Antiretroviral Therapy, AIDS, doi:10.1097/01.aids.0000210617.90954.0e
Negredo, Puigdomènech, Marfil, Puig, Pérez-Alvarez et al., Association between HIV Replication and Cholesterol in Peripheral Blood Mononuclear Cells in HIV-Infected Patients Interrupting HAART, J. Antimicrob. Chemother, doi:10.1093/jac/dkm470
Osuna-Ramos, Farfan-Morales, Cordero-Rivera, De Jesús-González, Reyes-Ruiz et al., Cholesterol-Lowering Drugs as Potential Antivirals: A Repurposing Approach against Flavivirus Infections, Viruses, doi:10.3390/v15071465
Overton, Sterrett, Westfall, Kahan, Burkholder et al., Effects of Atorvastatin and Pravastatin on Immune Activation and T-Cell Function in Antiretroviral Therapy-Suppressed HIV-1-Infected Patients, AIDS, doi:10.1097/QAD.0000000000000475
Owen, Doran, Halestrap, Evidence That Metformin Exerts Its Anti-Diabetic Effects through Inhibition of Complex 1 of the Mitochondrial Respiratory Chain, Biochem. J, doi:10.1042/bj3480607
Palacios-Rápalo, Farfan-Morales, Cordero-Rivera, De Jesús-González, Reyes-Ruiz et al., An Ivermectin-Atorvastatin Combination Impairs Nuclear Transport Inhibiting Dengue Infection in Vitro and in Vivo, iScience, doi:10.1016/j.isci.2023.108294
Parthasarathy, Tandel, Siddiqui, Harshan, Metformin Suppresses SARS-CoV-2 in Cell Culture, Virus Res, doi:10.1016/j.virusres.2022.199010
Pedrosa, Martins, Rizzo, Silva-Nunes, Metformin in SARS-CoV-2 Infection: A Hidden Path-From Altered Inflammation to Reduced Mortality. A Review from the Literature, J. Diabetes Complicat, doi:10.1016/j.jdiacomp.2022.108391
Pepperrell, Ellis, Wang, Hill, Barriers to Worldwide Access for Paxlovid, a New Treatment for COVID-19, Open Forum Infect. Dis, doi:10.1093/ofid/ofac174
Petakh, Griga, Mohammed, Loshak, Poliak et al., Effects of Metformin, Insulin on Hematological Parameters of COVID-19 Patients with Type 2 Diabetes, Med. Arch, doi:10.5455/medarh.2022.76.329-332
Petakh, Kamyshna, Nykyforuk, Yao, Imbery et al., Immunoregulatory Intestinal Microbiota and COVID-19 in Patients with Type Two Diabetes: A Double-Edged Sword, Viruses, doi:10.3390/v14030477
Petakh, Kamyshna, Oksenych, Kainov, Kamyshnyi, Metformin Therapy Changes Gut Microbiota Alpha-Diversity in COVID-19 Patients with Type 2 Diabetes: The Role of SARS-CoV-2 Variants and Antibiotic Treatment, Pharmaceuticals, doi:10.3390/ph16060904
Planas, Pagliuzza, Ponte, Fert, Marchand et al., LILAC Pilot Study: Effects of Metformin on mTOR Activation and HIV Reservoir Persistence during Antiretroviral Therapy, EBioMedicine, doi:10.1016/j.ebiom.2021.103270
Reis, Silva, Silva, Thabane, Milagres et al., Effect of Early Treatment with Metformin on Risk of Emergency Care and Hospitalization among Patients with COVID-19: The TOGETHER Randomized Platform Clinical Trial, Lancet Reg. Health Am, doi:10.1016/j.lana.2021.100142
Reyes-Ruiz, García-Hernández, Martínez-Mier, Osuna-Ramos, De Jesús-González et al., The Role of Aspartate Aminotransferase-to-Lymphocyte Ratio Index (ALRI) in Predicting Mortality in SARS-CoV-2 Infection, Microorganisms, doi:10.3390/microorganisms11122894
Riestenberg, Furman, Cowen, Pawlowksi, Schneider et al., Differences in Statin Utilization and Lipid Lowering by Race, Ethnicity, and HIV Status in a Real-World Cohort of Persons with Human Immunodeficiency Virus and Uninfected Persons, Am. Heart J, doi:10.1016/j.ahj.2018.11.012
Rodriguez-Nava, Trelles-Garcia, Yanez-Bello, Chung, Trelles-Garcia et al., Atorvastatin Associated with Decreased Hazard for Death in COVID-19 Patients Admitted to an ICU: A Retrospective Cohort Study, Crit. Care, doi:10.1186/s13054-020-03154-4
Roglans, Verd, Peris, Alegret, Vázquez et al., High Doses of Atorvastatin and Simvastatin Induce Key Enzymes Involved in VLDL Production, Lipids, doi:10.1007/s11745-002-0916-0
Saito, Koinuma, Kawashima, Miyato, Ohzawa et al., Metformin May Improve the Outcome of Patients with Colorectal Cancer and Type 2 Diabetes Mellitus Partly through Effects on Neutrophil Extracellular Traps, BJC Rep, doi:10.1038/s44276-023-00022-w
Scarpello, Howlett, Metformin Therapy and Clinical Uses, Diab. Vasc. Dis. Res, doi:10.3132/dvdr.2008.027
Scheen, Metformin and COVID-19: From Cellular Mechanisms to Reduced Mortality, Diabetes Metab, doi:10.1016/j.diabet.2020.07.006
Schieffer, Schieffer, The Rationale for the Treatment of Long-Covid Symptoms-A Cardiologist's View, Front. Cardiovasc. Med, doi:10.3389/fcvm.2022.992686
Segatori, Garona, Caligiuri, Bizzotto, Lavignolle et al., Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2-Positive Patients, Viruses, doi:10.3390/v13102084
Sharma, Abohashrh, Baig, Dong, Alam et al., Screening of Drug Databank against WT and Mutant Main Protease of SARS-CoV-2: Towards Finding Potential Compound for Repurposing against COVID-19, Saudi J. Biol. Sci, doi:10.1016/j.sjbs.2021.02.059
Shaw, Lamia, Vasquez, Koo, Bardeesy et al., The Kinase LKB1 Mediates Glucose Homeostasis in Liver and Therapeutic Effects of Metformin, Science, doi:10.1126/science.1120781
Sheridan, Wheeler-Jones, Gage, The Immunomodulatory Effects of Statins on Macrophages, Immuno, doi:10.3390/immuno2020021
Simon, Bonilla, Yan, Chung, Butt, Atorvastatin and Fluvastatin Are Associated with Dose-Dependent Reductions in Cirrhosis and Hepatocellular Carcinoma, among Patients with Hepatitis C Virus: Results from ERCHIVES, Hepatology, doi:10.1002/hep.28506
Simões E Silva, Silveira, Ferreira, Teixeira, ACE2, Angiotensin-(1-7) and Mas Receptor Axis in Inflammation and Fibrosis, Br. J. Pharmacol, doi:10.1111/bph.12159
Sorathia, Al-Rubaye, Zal, The Effect of Statins on the Functionality of CD4+CD25+FOXP3+ Regulatory T-Cells in Acute Coronary Syndrome: A Systematic Review and Meta-Analysis of Randomised Controlled Trials in Asian Populations, Eur. Cardiol, doi:10.15420/ecr.2019.9.2
Soto-Acosta, Bautista-Carbajal, Cervantes-Salazar, Angel-Ambrocio, Del et al., DENV Up-Regulates the HMG-CoA Reductase Activity through the Impairment of AMPK Phosphorylation: A Potential Antiviral Target, PLoS Pathog, doi:10.1371/journal.ppat.1006257
Stoyanova, Jabeen, Landazuri Vinueza, Ghosh Roy, Lockshin et al., Virus Triggers Autophagy to Exploit Host Lipid Metabolism and Drive Viral Replication, Cell Commun. Signal, doi:10.1186/s12964-022-01026-8
Sum, Webster, Johnson, Catalano, Cooper et al., The Effect of Intravenous Metformin on Glucose Metabolism during Hyperglycaemia in Type 2 Diabetes, Diabet. Med, doi:10.1111/j.1464-5491.1992.tb01716.x
Sun, Tian, Gao, Liu, Hou et al., Metformin Ameliorates the Development of Experimental Autoimmune Encephalomyelitis by Regulating T Helper 17 and Regulatory T Cells in Mice, J. Neuroimmunol, doi:10.1016/j.jneuroim.2016.01.014
Todorovska, Caloska-Ivanova, Dimitrova-Genadieva, Trajkovska, Popova-Jovanovska et al., Atorvastatin in Combination with Pegylated Interferon and Ribavirin Provided High Rate of Sustained Virological Response in Patients with Genotype 3 Hepatitis C Virus. Open Access Maced, J. Med. Sci, doi:10.3889/oamjms.2019.459
Tsai, Chang, Sun, Chan, Wu et al., Metformin Activates Type I Interferon Signaling against HCV via Activation of Adenosine Monophosphate-Activated Protein Kinase, Oncotarget, doi:10.18632/oncotarget.20248
Tárraga López, Celada Rodríguez, ; Cerdán, Oliver, Solera Albero et al., Análisis coste-efectividad de atorvastatina frente a simvastatina como tratamiento hipolipemiante en pacientes hipercolesterolémicos en atención primaria, Aten Primaria, doi:10.1016/S0212-6567(01)78767-7
Ventura-López, Cervantes-Luevano, Aguirre-Sánchez, Flores-Caballero, Alvarez-Delgado et al., Treatment with Metformin Glycinate Reduces SARS-CoV-2 Viral Load: An in Vitro Model and Randomized, Double-Blind, Phase IIb Clinical Trial, Biomed. Pharmacother, doi:10.1016/j.biopha.2022.113223
Visos-Varela, Zapata-Cachafeiro, Pintos-Rodríguez, Bugarín-González, González-Barcala et al., Outpatient Atorvastatin Use and Severe COVID-19 Outcomes: A Population-Based Study, J. Med. Virol, doi:10.1002/jmv.28971
Wagstaff, Sivakumaran, Heaton, Harrich, Jans, Ivermectin Is a Specific Inhibitor of Importin α/β-Mediated Nuclear Import Able to Inhibit Replication of HIV-1 and Dengue Virus, Biochem. J, doi:10.1042/BJ20120150
Wang, Wang, Yi, Baker, Casey et al., Metformin Restrains ZIKV Replication and Alleviates Virus-Induced Inflammatory Responses in Microglia, Int. Immunopharmacol, doi:10.1016/j.intimp.2023.110512
Wani, Mukherjee, Mallick, Akbar, Basu, Atorvastatin Ameliorates Viral Burden and Neural Stem/Progenitor Cell (NSPC) Death in an Experimental Model of Japanese Encephalitis, J. Biosci, doi:10.1007/s12038-020-00052-3
Wierzbicki, Atorvastatin, None, Expert Opin. Pharmacother, doi:10.1517/14656566.2.5.819
Wiklund, Mattsson-Hultén, Hurt-Camejo, Oscarsson, Effects of Simvastatin and Atorvastatin on Inflammation Markers in Plasma, J. Intern. Med, doi:10.1046/j.1365-2796.2002.00966.x
Xiao, Heath, Saiu, Leiper, Leone et al., Structural Basis for AMP Binding to Mammalian AMP-Activated Protein Kinase, Nature, doi:10.1038/nature06161
Xun, Zhang, Pan, Mao, Qin et al., Metformin Inhibits Hepatitis B Virus Protein Production and Replication in Human Hepatoma Cells, J. Viral. Hepat, doi:10.1111/jvh.12187
Yu, Sun, Zhao, Kang, Yan, The Effect of Metformin on the Efficacy of Antiviral Therapy in Patients with Genotype 1 Chronic Hepatitis C and Insulin Resistance, Int. J. Infect. Dis, doi:10.1016/j.ijid.2012.02.004
Zapata-Cardona, Flórez-Álvarez, Zapata-Builes, Guerra-Sandoval, Guerra-Almonacid et al., Atorvastatin Effectively Inhibits Ancestral and Two Emerging Variants of SARS-CoV-2 in Vitro, Front. Microbiol, doi:10.3389/fmicb.2022.721103
Zhang, Dong, Martin, He, Gongol et al., AMP-Activated Protein Kinase Phosphorylation of Angiotensin-Converting Enzyme 2 in Endothelium Mitigates Pulmonary Hypertension, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.201712-2570OC
Zhang, Feng, Luo, Zhao, Kannan et al., Metformin Hydrochloride Significantly Inhibits Rotavirus Infection in Caco2 Cell Line, Intestinal Organoids, and Mice, Pharmaceuticals, doi:10.3390/ph16091279
Zhao, Zeng, Chen, Liu, Chen et al., Lipid Droplets Are Beneficial for Rabies Virus Replication by Facilitating Viral Budding, J. Virol, doi:10.1128/JVI.01473-21
DOI record:
{
"DOI": "10.3390/microorganisms12020383",
"ISSN": [
"2076-2607"
],
"URL": "http://dx.doi.org/10.3390/microorganisms12020383",
"abstract": "<jats:p>Metformin (MET) and atorvastatin (ATO) are promising treatments for COVID-19. This review explores the potential of MET and ATO, commonly prescribed for diabetes and dyslipidemia, respectively, as versatile medicines against SARS-CoV-2. Due to their immunomodulatory and antiviral capabilities, as well as their cost-effectiveness and ubiquitous availability, they are highly suitable options for treating the virus. MET’s effect extends beyond managing blood sugar, impacting pathways that can potentially decrease the severity and fatality rates linked with COVID-19. It can partially block mitochondrial complex I and stimulate AMPK, which indicates that it can be used more widely in managing viral infections. ATO, however, impacts cholesterol metabolism, a crucial element of the viral replicative cycle, and demonstrates anti-inflammatory characteristics that could modulate intense immune reactions in individuals with COVID-19. Retrospective investigations and clinical trials show decreased hospitalizations, severity, and mortality rates in patients receiving these medications. Nevertheless, the journey from observing something to applying it in a therapeutic setting is intricate, and the inherent diversity of the data necessitates carefully executed, forward-looking clinical trials. This review highlights the requirement for efficacious, easily obtainable, and secure COVID-19 therapeutics and identifies MET and ATO as promising treatments in this worldwide health emergency.</jats:p>",
"alternative-id": [
"microorganisms12020383"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1415-6260",
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
},
{
"name": "Department of Infectomics and Molecular Pathogenesis, Center for Research and Advanced Studies (CINVESTAV-IPN), Mexico City 07360, Mexico"
}
],
"authenticated-orcid": false,
"family": "De Jesús-González",
"given": "Luis Adrián",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-6785-2035",
"affiliation": [
{
"name": "Department of Infectomics and Molecular Pathogenesis, Center for Research and Advanced Studies (CINVESTAV-IPN), Mexico City 07360, Mexico"
}
],
"authenticated-orcid": false,
"family": "del Ángel",
"given": "Rosa María",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2184-6529",
"affiliation": [
{
"name": "Department of Infectomics and Molecular Pathogenesis, Center for Research and Advanced Studies (CINVESTAV-IPN), Mexico City 07360, Mexico"
}
],
"authenticated-orcid": false,
"family": "Palacios-Rápalo",
"given": "Selvin Noé",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5052-2670",
"affiliation": [
{
"name": "Department of Infectomics and Molecular Pathogenesis, Center for Research and Advanced Studies (CINVESTAV-IPN), Mexico City 07360, Mexico"
}
],
"authenticated-orcid": false,
"family": "Cordero-Rivera",
"given": "Carlos Daniel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3514-5299",
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
}
],
"authenticated-orcid": false,
"family": "Rodríguez-Carlos",
"given": "Adrián",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
}
],
"family": "Trujillo-Paez",
"given": "Juan Valentin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9787-5588",
"affiliation": [
{
"name": "Departamento de Ciencias Naturales, Universidad Autónoma Metropolitana (UAM), Unidad Cuajimalpa, Ciudad de México 05348, Mexico"
}
],
"authenticated-orcid": false,
"family": "Farfan-Morales",
"given": "Carlos Noe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8280-9812",
"affiliation": [
{
"name": "Facultad de Medicina, Universidad Autónoma de Sinaloa, Culiacán 80019, Mexico"
}
],
"authenticated-orcid": false,
"family": "Osuna-Ramos",
"given": "Juan Fidel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2379-8591",
"affiliation": [
{
"name": "División de Investigación en Salud, Unidad Médica de Alta Especialidad, Hospital de Especialidades No. 14, Centro Médico Nacional “Adolfo Ruiz Cortines”, Instituto Mexicano del Seguro Social (IMSS), Veracruz 91897, Mexico"
},
{
"name": "Facultad de Medicina, Región Veracruz, Universidad Veracruzana (UV), Veracruz 91700, Mexico"
}
],
"authenticated-orcid": false,
"family": "Reyes-Ruiz",
"given": "José Manuel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1521-1519",
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
}
],
"authenticated-orcid": false,
"family": "Rivas-Santiago",
"given": "Bruno",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5726-5953",
"affiliation": [
{
"name": "Laboratorio de Virología Perinatal y Diseño Molecular de Antígenos y Biomarcadores, Departamento de Inmunobioquímica, Instituto Nacional de Perinatología, Ciudad de México 11000, Mexico"
}
],
"authenticated-orcid": false,
"family": "León-Juárez",
"given": "Moisés",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
}
],
"family": "García-Herrera",
"given": "Ana Cristina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
}
],
"family": "Ramos-Cortes",
"given": "Adriana Clara",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
}
],
"family": "López-Gándara",
"given": "Erika Alejandra",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unidad de Investigación Biomédica de Zacatecas, Instituto Mexicano del Seguro Social, Zacatecas 98000, Mexico"
}
],
"family": "Martínez-Rodríguez",
"given": "Estefanía",
"sequence": "additional"
}
],
"container-title": "Microorganisms",
"container-title-short": "Microorganisms",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
2,
14
]
],
"date-time": "2024-02-14T09:18:22Z",
"timestamp": 1707902302000
},
"deposited": {
"date-parts": [
[
2024,
2,
14
]
],
"date-time": "2024-02-14T10:14:34Z",
"timestamp": 1707905674000
},
"funder": [
{
"award": [
"Pronaii 302979",
"A1-S-9005 CONAHCyT (México)"
],
"name": "R.M.D.Á."
},
{
"name": "FUNDACIÓN IMSS, AC"
}
],
"indexed": {
"date-parts": [
[
2024,
2,
15
]
],
"date-time": "2024-02-15T00:44:20Z",
"timestamp": 1707957860740
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2024,
2,
13
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2024,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
13
]
],
"date-time": "2024-02-13T00:00:00Z",
"timestamp": 1707782400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-2607/12/2/383/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "383",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
2,
13
]
]
},
"published-online": {
"date-parts": [
[
2024,
2,
13
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "Cascella, M., Rajnik, M., Aleem, A., Dulebohn, S.C., and Di Napoli, R. (2023). StatPearls, StatPearls Publishing."
},
{
"DOI": "10.3390/microorganisms11122894",
"doi-asserted-by": "crossref",
"key": "ref_2",
"unstructured": "Reyes-Ruiz, J.M., García-Hernández, O., Martínez-Mier, G., Osuna-Ramos, J.F., De Jesús-González, L.A., Farfan-Morales, C.N., Palacios-Rápalo, S.N., Cordero-Rivera, C.D., Ordoñez-Rodríguez, T., and Ángel, R.M.d. (2023). The Role of Aspartate Aminotransferase-to-Lymphocyte Ratio Index (ALRI) in Predicting Mortality in SARS-CoV-2 Infection. Microorganisms, 11."
},
{
"DOI": "10.1038/s41573-023-00672-y",
"article-title": "Therapeutic Strategies for COVID-19: Progress and Lessons Learned",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "449",
"journal-title": "Nat. Rev. Drug Discov.",
"key": "ref_3",
"volume": "22",
"year": "2023"
},
{
"DOI": "10.1186/s12929-022-00852-9",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Kumari, M., Lu, R.-M., Li, M.-C., Huang, J.-L., Hsu, F.-F., Ko, S.-H., Ke, F.-Y., Su, S.-C., Liang, K.-H., and Yuan, J.P.-Y. (2022). A Critical Overview of Current Progress for COVID-19: Development of Vaccines, Antiviral Drugs, and Therapeutic Antibodies. J. Biomed. Sci., 29."
},
{
"DOI": "10.3389/fmed.2021.636532",
"article-title": "Implications of the Novel Mutations in the SARS-CoV-2 Genome for Transmission, Disease Severity, and the Vaccine Development",
"author": "Akkiz",
"doi-asserted-by": "crossref",
"first-page": "636532",
"journal-title": "Front. Med.",
"key": "ref_5",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1074/jbc.275.1.223",
"article-title": "Dimethylbiguanide Inhibits Cell Respiration via an Indirect Effect Targeted on the Respiratory Chain Complex I",
"author": "Nogueira",
"doi-asserted-by": "crossref",
"first-page": "223",
"journal-title": "J. Biol. Chem.",
"key": "ref_6",
"volume": "275",
"year": "2000"
},
{
"DOI": "10.1016/j.cmet.2010.04.001",
"article-title": "Use of Cells Expressing Gamma Subunit Variants to Identify Diverse Mechanisms of AMPK Activation",
"author": "Hawley",
"doi-asserted-by": "crossref",
"first-page": "554",
"journal-title": "Cell Metab.",
"key": "ref_7",
"volume": "11",
"year": "2010"
},
{
"DOI": "10.1016/S0006-2952(99)00203-8",
"article-title": "Hypocholesterolemic Effects of 3-Hydroxy-3-Methylglutaryl Coenzyme A (HMG-CoA) Reductase Inhibitors in the Guinea Pig: Atorvastatin versus Simvastatin",
"author": "Conde",
"doi-asserted-by": "crossref",
"first-page": "1209",
"journal-title": "Biochem. Pharmacol.",
"key": "ref_8",
"volume": "58",
"year": "1999"
},
{
"DOI": "10.1002/j.1875-9114.1997.tb03081.x",
"article-title": "Atorvastatin Calcium: An Addition to HMG-CoA Reductase Inhibitors",
"author": "Chong",
"doi-asserted-by": "crossref",
"first-page": "1157",
"journal-title": "Pharmacotherapy",
"key": "ref_9",
"volume": "17",
"year": "1997"
},
{
"article-title": "Effect of Early Treatment with Metformin on Risk of Emergency Care and Hospitalization among Patients with COVID-19: The TOGETHER Randomized Platform Clinical Trial",
"author": "Reis",
"first-page": "100142",
"journal-title": "Lancet Reg. Health Am.",
"key": "ref_10",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1016/j.biopha.2022.113223",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Ventura-López, C., Cervantes-Luevano, K., Aguirre-Sánchez, J.S., Flores-Caballero, J.C., Alvarez-Delgado, C., Bernaldez-Sarabia, J., Sánchez-Campos, N., Lugo-Sánchez, L.A., Rodríguez-Vázquez, I.C., and Sander-Padilla, J.G. (2022). Treatment with Metformin Glycinate Reduces SARS-CoV-2 Viral Load: An in Vitro Model and Randomized, Double-Blind, Phase IIb Clinical Trial. Biomed. Pharmacother., 152."
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and Risk of Mortality in Patients Hospitalised with COVID-19: A Retrospective Cohort Analysis",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "e34",
"journal-title": "Lancet Healthy Longev.",
"key": "ref_12",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2201662",
"article-title": "Randomized Trial of Metformin, Ivermectin, and Fluvoxamine for COVID-19",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "599",
"journal-title": "N. Engl. J. Med.",
"key": "ref_13",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1016/S1473-3099(23)00299-2",
"article-title": "Outpatient Treatment of COVID-19 and Incidence of Post-COVID-19 Condition over 10 Months (COVID-OUT): A Multicentre, Randomised, Quadruple-Blind, Parallel-Group, Phase 3 Trial",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "1119",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_14",
"volume": "23",
"year": "2023"
},
{
"article-title": "Atorvastatin Therapy in COVID-19 Adult Inpatients: A Double-Blind, Randomized Controlled Trial",
"author": "Davoodi",
"first-page": "100875",
"journal-title": "Int. J. Cardiol. Heart Vasc.",
"key": "ref_15",
"volume": "36",
"year": "2021"
},
{
"article-title": "Atorvastatin versus Placebo in Patients with COVID-19 in Intensive Care: Randomized Controlled Trial",
"author": "Investigators",
"first-page": "e068407",
"journal-title": "BMJ",
"key": "ref_16",
"volume": "376",
"year": "2022"
},
{
"article-title": "Metformin: Current Knowledge",
"author": "Nasri",
"first-page": "658",
"journal-title": "J. Res. Med. Sci.",
"key": "ref_17",
"volume": "19",
"year": "2014"
},
{
"DOI": "10.1056/NEJM199602293340906",
"article-title": "Metformin",
"author": "Bailey",
"doi-asserted-by": "crossref",
"first-page": "574",
"journal-title": "N. Engl. J. Med.",
"key": "ref_18",
"volume": "334",
"year": "1996"
},
{
"DOI": "10.1111/j.1464-5491.1992.tb01716.x",
"article-title": "The Effect of Intravenous Metformin on Glucose Metabolism during Hyperglycaemia in Type 2 Diabetes",
"author": "Sum",
"doi-asserted-by": "crossref",
"first-page": "61",
"journal-title": "Diabet. Med.",
"key": "ref_19",
"volume": "9",
"year": "1992"
},
{
"DOI": "10.3132/dvdr.2008.027",
"article-title": "Metformin Therapy and Clinical Uses",
"author": "Scarpello",
"doi-asserted-by": "crossref",
"first-page": "157",
"journal-title": "Diab. Vasc. Dis. Res.",
"key": "ref_20",
"volume": "5",
"year": "2008"
},
{
"DOI": "10.1056/NEJM199508313330902",
"article-title": "Efficacy of Metformin in Patients with Non-Insulin-Dependent Diabetes Mellitus",
"author": "DeFronzo",
"doi-asserted-by": "crossref",
"first-page": "541",
"journal-title": "N. Engl. J. Med.",
"key": "ref_21",
"volume": "333",
"year": "1995"
},
{
"DOI": "10.1016/S1262-3636(03)72785-2",
"article-title": "Reducing Insulin Resistance with Metformin: The Evidence Today",
"author": "Giannarelli",
"doi-asserted-by": "crossref",
"first-page": "6S28",
"journal-title": "Diabetes Metab.",
"key": "ref_22",
"volume": "29",
"year": "2003"
},
{
"DOI": "10.1038/nature13270",
"article-title": "Metformin Suppresses Gluconeogenesis by Inhibiting Mitochondrial Glycerophosphate Dehydrogenase",
"author": "Madiraju",
"doi-asserted-by": "crossref",
"first-page": "542",
"journal-title": "Nature",
"key": "ref_23",
"volume": "510",
"year": "2014"
},
{
"DOI": "10.1210/endrev/bnaa023",
"article-title": "Cellular and Molecular Mechanisms of Metformin Action",
"author": "LaMoia",
"doi-asserted-by": "crossref",
"first-page": "77",
"journal-title": "Endocr. Rev.",
"key": "ref_24",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1038/nature06161",
"article-title": "Structural Basis for AMP Binding to Mammalian AMP-Activated Protein Kinase",
"author": "Xiao",
"doi-asserted-by": "crossref",
"first-page": "496",
"journal-title": "Nature",
"key": "ref_25",
"volume": "449",
"year": "2007"
},
{
"key": "ref_26",
"unstructured": "Hawley, S.A., Boudeau, J., Reid, J.L., Mustard, K.J., Udd, L., Mäkelä, T.P., Alessi, D.R., and Hardie, D.G. (2003). Complexes between the LKB1 Tumor Suppressor, STRAD Alpha/Beta and MO25 Alpha/Beta Are Upstream Kinases in the AMP-Activated Protein Kinase Cascade. J. Biol., 2."
},
{
"DOI": "10.1016/j.cmet.2005.05.009",
"article-title": "Calmodulin-Dependent Protein Kinase Kinase-Beta Is an Alternative Upstream Kinase for AMP-Activated Protein Kinase",
"author": "Hawley",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Cell Metab.",
"key": "ref_27",
"volume": "2",
"year": "2005"
},
{
"DOI": "10.1126/science.1120781",
"article-title": "The Kinase LKB1 Mediates Glucose Homeostasis in Liver and Therapeutic Effects of Metformin",
"author": "Shaw",
"doi-asserted-by": "crossref",
"first-page": "1642",
"journal-title": "Science",
"key": "ref_28",
"volume": "310",
"year": "2005"
},
{
"DOI": "10.1038/nm.3372",
"article-title": "Single Phosphorylation Sites in Acc1 and Acc2 Regulate Lipid Homeostasis and the Insulin-Sensitizing Effects of Metformin",
"author": "Fullerton",
"doi-asserted-by": "crossref",
"first-page": "1649",
"journal-title": "Nat. Med.",
"key": "ref_29",
"volume": "19",
"year": "2013"
},
{
"DOI": "10.1111/jdv.12116",
"article-title": "Metformin in Dermatology: An Overview",
"author": "Badr",
"doi-asserted-by": "crossref",
"first-page": "1329",
"journal-title": "J. Eur. Acad. Dermatol. Venereol.",
"key": "ref_30",
"volume": "27",
"year": "2013"
},
{
"DOI": "10.2337/dc09-1284",
"article-title": "Novel Assay of Metformin Levels in Patients with Type 2 Diabetes and Varying Levels of Renal Function: Clinical Recommendations",
"author": "Frid",
"doi-asserted-by": "crossref",
"first-page": "1291",
"journal-title": "Diabetes Care",
"key": "ref_31",
"volume": "33",
"year": "2010"
},
{
"DOI": "10.1016/S0022-2275(20)41379-3",
"article-title": "The Discovery and Development of HMG-CoA Reductase Inhibitors",
"author": "Endo",
"doi-asserted-by": "crossref",
"first-page": "1569",
"journal-title": "J. Lipid Res.",
"key": "ref_32",
"volume": "33",
"year": "1992"
},
{
"DOI": "10.1038/343425a0",
"article-title": "Regulation of the Mevalonate Pathway",
"author": "Goldstein",
"doi-asserted-by": "crossref",
"first-page": "425",
"journal-title": "Nature",
"key": "ref_33",
"volume": "343",
"year": "1990"
},
{
"DOI": "10.1007/s11745-002-0916-0",
"article-title": "High Doses of Atorvastatin and Simvastatin Induce Key Enzymes Involved in VLDL Production",
"author": "Roglans",
"doi-asserted-by": "crossref",
"first-page": "445",
"journal-title": "Lipids",
"key": "ref_34",
"volume": "37",
"year": "2002"
},
{
"DOI": "10.1517/14656566.2.5.819",
"article-title": "Atorvastatin",
"author": "Wierzbicki",
"doi-asserted-by": "crossref",
"first-page": "819",
"journal-title": "Expert Opin. Pharmacother.",
"key": "ref_35",
"volume": "2",
"year": "2001"
},
{
"DOI": "10.1016/j.virusres.2013.03.005",
"article-title": "Requirement of Cholesterol in the Viral Envelope for Dengue Virus Infection",
"author": "Carro",
"doi-asserted-by": "crossref",
"first-page": "78",
"journal-title": "Virus Res.",
"key": "ref_36",
"volume": "174",
"year": "2013"
},
{
"DOI": "10.1111/jvh.12187",
"article-title": "Metformin Inhibits Hepatitis B Virus Protein Production and Replication in Human Hepatoma Cells",
"author": "Xun",
"doi-asserted-by": "crossref",
"first-page": "597",
"journal-title": "J. Viral. Hepat.",
"key": "ref_37",
"volume": "21",
"year": "2014"
},
{
"DOI": "10.1002/ijc.33594",
"article-title": "Effects of Metformin on the Virus/Host Cell Crosstalk in Human Papillomavirus-Positive Cancer Cells",
"author": "Herrmann",
"doi-asserted-by": "crossref",
"first-page": "1137",
"journal-title": "Int. J. Cancer",
"key": "ref_38",
"volume": "149",
"year": "2021"
},
{
"DOI": "10.3390/ph16091279",
"doi-asserted-by": "crossref",
"key": "ref_39",
"unstructured": "Zhang, R., Feng, C., Luo, D., Zhao, R., Kannan, P.R., Yin, Y., Iqbal, M.Z., Hu, Y., and Kong, X. (2023). Metformin Hydrochloride Significantly Inhibits Rotavirus Infection in Caco2 Cell Line, Intestinal Organoids, and Mice. Pharmaceuticals, 16."
},
{
"DOI": "10.1002/jcb.26555",
"article-title": "Metformin Inhibits Tumorigenesis in HBV-Induced Hepatocellular Carcinoma by Suppressing HULC Overexpression Caused by HBX",
"author": "Jiang",
"doi-asserted-by": "crossref",
"first-page": "4482",
"journal-title": "J. Cell Biochem.",
"key": "ref_40",
"volume": "119",
"year": "2018"
},
{
"DOI": "10.1038/s41598-021-87707-9",
"article-title": "The Antiviral Effect of Metformin on Zika and Dengue Virus Infection",
"doi-asserted-by": "crossref",
"first-page": "8743",
"journal-title": "Sci. Rep.",
"key": "ref_41",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.virusres.2022.199010",
"article-title": "Metformin Suppresses SARS-CoV-2 in Cell Culture",
"author": "Parthasarathy",
"doi-asserted-by": "crossref",
"first-page": "199010",
"journal-title": "Virus Res.",
"key": "ref_42",
"volume": "323",
"year": "2022"
},
{
"DOI": "10.3389/fonc.2018.00436",
"article-title": "Metformin Clinical Trial in HPV+ and HPV- Head and Neck Squamous Cell Carcinoma: Impact on Cancer Cell Apoptosis and Immune Infiltrate",
"author": "Curry",
"doi-asserted-by": "crossref",
"first-page": "436",
"journal-title": "Front. Oncol.",
"key": "ref_43",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1038/s41598-022-25065-w",
"article-title": "Metformin Enhances the Antitumor Activity of Oncolytic Herpes Simplex Virus HF10 (Canerpaturev) in a Pancreatic Cell Cancer Subcutaneous Model",
"author": "Abdelmoneim",
"doi-asserted-by": "crossref",
"first-page": "21570",
"journal-title": "Sci. Rep.",
"key": "ref_44",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.cellsig.2017.09.020",
"article-title": "Metformin Triggers Apoptosis in PEL Cells and Alters Bortezomib-Induced Unfolded Protein Response Increasing Its Cytotoxicity and Inhibiting KSHV Lytic Cycle Activation",
"author": "Granato",
"doi-asserted-by": "crossref",
"first-page": "239",
"journal-title": "Cell. Signal.",
"key": "ref_45",
"volume": "40",
"year": "2017"
},
{
"DOI": "10.1016/j.intimp.2023.110512",
"article-title": "Metformin Restrains ZIKV Replication and Alleviates Virus-Induced Inflammatory Responses in Microglia",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "110512",
"journal-title": "Int. Immunopharmacol.",
"key": "ref_46",
"volume": "121",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0191805",
"doi-asserted-by": "crossref",
"key": "ref_47",
"unstructured": "del Campo, J.A., García Valdecasas, M., Gil Gómez, A., Rojas Alvarez-Ossorio, M.A., Gallego, P., Ampuero Herrojo, J., Gallego Durán, R., Pastor, H., Grande, L., and Padillo Ruiz, F.J. (2018). Simvastatin and Metformin Inhibit Cell Growth in Hepatitis C Virus Infected Cells via mTOR Increasing PTEN and Autophagy. PLoS ONE, 13."
},
{
"DOI": "10.18632/oncotarget.20248",
"article-title": "Metformin Activates Type I Interferon Signaling against HCV via Activation of Adenosine Monophosphate-Activated Protein Kinase",
"author": "Tsai",
"doi-asserted-by": "crossref",
"first-page": "91928",
"journal-title": "Oncotarget",
"key": "ref_48",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1016/j.heliyon.2023.e20284",
"article-title": "Metformin Reduces the Risk of Developing Influenza A Virus Related Cardiovascular Disease",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "e20284",
"journal-title": "Heliyon",
"key": "ref_49",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.1016/j.ebiom.2021.103270",
"doi-asserted-by": "crossref",
"key": "ref_50",
"unstructured": "Planas, D., Pagliuzza, A., Ponte, R., Fert, A., Marchand, L.R., Massanella, M., Gosselin, A., Mehraj, V., Dupuy, F.P., and Isnard, S. (2021). LILAC Pilot Study: Effects of Metformin on mTOR Activation and HIV Reservoir Persistence during Antiretroviral Therapy. EBioMedicine, 65."
},
{
"DOI": "10.3390/idr15030024",
"article-title": "Bictegravir and Metformin Drug-Drug Interaction in People with Human Immunodeficiency Virus (HIV)",
"author": "Masich",
"doi-asserted-by": "crossref",
"first-page": "231",
"journal-title": "Infect. Dis. Rep.",
"key": "ref_51",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.3389/fphys.2021.749770",
"article-title": "Anti-Flavivirus Properties of Lipid-Lowering Drugs",
"doi-asserted-by": "crossref",
"first-page": "749770",
"journal-title": "Front. Physiol.",
"key": "ref_52",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3390/v15071465",
"doi-asserted-by": "crossref",
"key": "ref_53",
"unstructured": "Osuna-Ramos, J.F., Farfan-Morales, C.N., Cordero-Rivera, C.D., De Jesús-González, L.A., Reyes-Ruiz, J.M., Hurtado-Monzón, A.M., Palacios-Rápalo, S.N., Jiménez-Camacho, R., Meraz-Ríos, M.A., and Del Ángel, R.M. (2023). Cholesterol-Lowering Drugs as Potential Antivirals: A Repurposing Approach against Flavivirus Infections. Viruses, 15."
},
{
"DOI": "10.3390/microorganisms11071851",
"doi-asserted-by": "crossref",
"key": "ref_54",
"unstructured": "Herrera-Moro Huitron, L., De Jesús-González, L.A., Martínez-Castillo, M., Ulloa-Aguilar, J.M., Cabello-Gutierrez, C., Helguera-Repetto, C., Garcia-Cordero, J., and León Juárez, M. (2023). Multifaceted Nature of Lipid Droplets in Viral Interactions and Pathogenesis. Microorganisms, 11."
},
{
"DOI": "10.1042/bj3480607",
"article-title": "Evidence That Metformin Exerts Its Anti-Diabetic Effects through Inhibition of Complex 1 of the Mitochondrial Respiratory Chain",
"author": "Owen",
"doi-asserted-by": "crossref",
"first-page": "607",
"journal-title": "Biochem. J.",
"key": "ref_55",
"volume": "348",
"year": "2000"
},
{
"DOI": "10.3389/fendo.2018.00753",
"article-title": "Metformin-Induced Mitochondrial Complex I Inhibition: Facts, Uncertainties, and Consequences",
"author": "Fontaine",
"doi-asserted-by": "crossref",
"first-page": "753",
"journal-title": "Front. Endocrinol.",
"key": "ref_56",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1371/journal.ppat.1006257",
"doi-asserted-by": "crossref",
"key": "ref_57",
"unstructured": "Soto-Acosta, R., Bautista-Carbajal, P., Cervantes-Salazar, M., Angel-Ambrocio, A.H., and Del Angel, R.M. (2017). DENV Up-Regulates the HMG-CoA Reductase Activity through the Impairment of AMPK Phosphorylation: A Potential Antiviral Target. PLoS Pathog., 13."
},
{
"DOI": "10.1093/infdis/jiv572",
"article-title": "Hepatitis B Virus (HBV) Core-Related Antigen During Nucleos(t)Ide Analog Therapy Is Related to Intra-Hepatic HBV Replication and Development of Hepatocellular Carcinoma",
"author": "Honda",
"doi-asserted-by": "crossref",
"first-page": "1096",
"journal-title": "J. Infect. Dis.",
"key": "ref_58",
"volume": "213",
"year": "2016"
},
{
"DOI": "10.1016/j.sjbs.2021.02.059",
"article-title": "Screening of Drug Databank against WT and Mutant Main Protease of SARS-CoV-2: Towards Finding Potential Compound for Repurposing against COVID-19",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "3152",
"journal-title": "Saudi J. Biol. Sci.",
"key": "ref_59",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.compbiomed.2021.104634",
"doi-asserted-by": "crossref",
"key": "ref_60",
"unstructured": "Kumar, V., Liu, H., and Wu, C. (2021). Drug Repurposing against SARS-CoV-2 Receptor Binding Domain Using Ensemble-Based Virtual Screening and Molecular Dynamics Simulations. Comput. Biol. Med., 135."
},
{
"DOI": "10.1186/s10020-021-00356-6",
"article-title": "Identifying FDA-Approved Drugs with Multimodal Properties against COVID-19 Using a Data-Driven Approach and a Lung Organoid Model of SARS-CoV-2 Entry",
"author": "Duarte",
"doi-asserted-by": "crossref",
"first-page": "105",
"journal-title": "Mol. Med.",
"key": "ref_61",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.3389/fmicb.2022.721103",
"doi-asserted-by": "crossref",
"key": "ref_62",
"unstructured": "Zapata-Cardona, M.I., Flórez-Álvarez, L., Zapata-Builes, W., Guerra-Sandoval, A.L., Guerra-Almonacid, C.M., Hincapié-García, J., Rugeles, M.T., and Hernandez, J.C. (2022). Atorvastatin Effectively Inhibits Ancestral and Two Emerging Variants of SARS-CoV-2 in Vitro. Front. Microbiol., 13."
},
{
"DOI": "10.3390/v13102084",
"doi-asserted-by": "crossref",
"key": "ref_63",
"unstructured": "Segatori, V.I., Garona, J., Caligiuri, L.G., Bizzotto, J., Lavignolle, R., Toro, A., Sanchis, P., Spitzer, E., Krolewiecki, A., and Gueron, G. (2021). Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2-Positive Patients. Viruses, 13."
},
{
"DOI": "10.3892/mmr.2016.5519",
"article-title": "The Anti-dengue Virus Properties of Statins May Be Associated with Alterations in the Cellular Antiviral Profile Expression",
"author": "Vidaltamayo",
"doi-asserted-by": "crossref",
"first-page": "2155",
"journal-title": "Mol. Med. Rep.",
"key": "ref_64",
"volume": "14",
"year": "2016"
},
{
"DOI": "10.1016/j.isci.2023.108294",
"article-title": "An Ivermectin—Atorvastatin Combination Impairs Nuclear Transport Inhibiting Dengue Infection in Vitro and in Vivo",
"doi-asserted-by": "crossref",
"first-page": "108294",
"journal-title": "iScience",
"key": "ref_65",
"volume": "26",
"year": "2023"
},
{
"DOI": "10.3390/pharmaceutics15010050",
"doi-asserted-by": "crossref",
"key": "ref_66",
"unstructured": "Españo, E., and Kim, J.-K. (2022). Effects of Statin Combinations on Zika Virus Infection in Vero Cells. Pharmaceutics, 15."
},
{
"DOI": "10.1186/s12964-022-01026-8",
"article-title": "Zika Virus Triggers Autophagy to Exploit Host Lipid Metabolism and Drive Viral Replication",
"author": "Stoyanova",
"doi-asserted-by": "crossref",
"first-page": "114",
"journal-title": "Cell Commun. Signal.",
"key": "ref_67",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1007/s12038-020-00052-3",
"doi-asserted-by": "crossref",
"key": "ref_68",
"unstructured": "Wani, M.A., Mukherjee, S., Mallick, S., Akbar, I., and Basu, A. (2020). Atorvastatin Ameliorates Viral Burden and Neural Stem/Progenitor Cell (NSPC) Death in an Experimental Model of Japanese Encephalitis. J. Biosci., 45."
},
{
"DOI": "10.1254/jphs.FM0070050",
"article-title": "Life Style-Related Diseases of the Digestive System: Cell Culture System for the Screening of Anti-Hepatitis C Virus (HCV) Reagents: Suppression of HCV Replication by Statins and Synergistic Action with Interferon",
"author": "Ikeda",
"doi-asserted-by": "crossref",
"first-page": "145",
"journal-title": "J. Pharmacol. Sci.",
"key": "ref_69",
"volume": "105",
"year": "2007"
},
{
"DOI": "10.1002/hep.21232",
"article-title": "Different Anti-HCV Profiles of Statins and Their Potential for Combination Therapy with Interferon",
"author": "Ikeda",
"doi-asserted-by": "crossref",
"first-page": "117",
"journal-title": "Hepatology",
"key": "ref_70",
"volume": "44",
"year": "2006"
},
{
"DOI": "10.3889/oamjms.2019.459",
"article-title": "Atorvastatin in Combination with Pegylated Interferon and Ribavirin Provided High Rate of Sustained Virological Response in Patients with Genotype 3 Hepatitis C Virus",
"author": "Todorovska",
"doi-asserted-by": "crossref",
"first-page": "1641",
"journal-title": "Open Access Maced. J. Med. Sci.",
"key": "ref_71",
"volume": "7",
"year": "2019"
},
{
"DOI": "10.1002/hep.28506",
"article-title": "Atorvastatin and Fluvastatin Are Associated with Dose-Dependent Reductions in Cirrhosis and Hepatocellular Carcinoma, among Patients with Hepatitis C Virus: Results from ERCHIVES",
"author": "Simon",
"doi-asserted-by": "crossref",
"first-page": "47",
"journal-title": "Hepatology",
"key": "ref_72",
"volume": "64",
"year": "2016"
},
{
"DOI": "10.1097/FJC.0b013e3181f6b28d",
"article-title": "Atorvastatin Attenuates Coxsackie Virus B3m-Induced Viral Myocarditis in Mice",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "540",
"journal-title": "J. Cardiovasc. Pharmacol.",
"key": "ref_73",
"volume": "56",
"year": "2010"
},
{
"DOI": "10.1096/fj.201900428RR",
"article-title": "Atorvastatin Restricts the Ability of Influenza Virus to Generate Lipid Droplets and Severely Suppresses the Replication of the Virus",
"author": "Episcopio",
"doi-asserted-by": "crossref",
"first-page": "9516",
"journal-title": "FASEB J.",
"key": "ref_74",
"volume": "33",
"year": "2019"
},
{
"DOI": "10.20944/preprints202107.0246.v1",
"doi-asserted-by": "crossref",
"key": "ref_75",
"unstructured": "Ianevski, A., Yao, R., Zusinaite, E., Lysvand, H., Oksenych, V., Tenson, T., Bjørås, M., and Kainov, D. (2021). Active Components of Commonly Prescribed Medicines Affect Influenza A Virus-Host Cell Interaction: A Pilot Study. Viruses, 13."
},
{
"DOI": "10.1128/JVI.01473-21",
"article-title": "Lipid Droplets Are Beneficial for Rabies Virus Replication by Facilitating Viral Budding",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "e0147321",
"journal-title": "J. Virol.",
"key": "ref_76",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.1097/QAD.0000000000003656",
"article-title": "An Open Label Randomized Controlled Trial of Atorvastatin versus Aspirin in Elite Controllers and Antiretroviral-Treated People with HIV",
"author": "Mystakelis",
"doi-asserted-by": "crossref",
"first-page": "1827",
"journal-title": "AIDS",
"key": "ref_77",
"volume": "37",
"year": "2023"
},
{
"DOI": "10.1097/QAD.0000000000000475",
"article-title": "Effects of Atorvastatin and Pravastatin on Immune Activation and T-Cell Function in Antiretroviral Therapy-Suppressed HIV-1-Infected Patients",
"author": "Overton",
"doi-asserted-by": "crossref",
"first-page": "2627",
"journal-title": "AIDS",
"key": "ref_78",
"volume": "28",
"year": "2014"
},
{
"DOI": "10.1093/infdis/jiq115",
"article-title": "High Dose Atorvastatin Decreases Cellular Markers of Immune Activation without Affecting HIV-1 RNA Levels: Results of a Double-Blind Randomized Placebo Controlled Clinical Trial",
"author": "Ganesan",
"doi-asserted-by": "crossref",
"first-page": "756",
"journal-title": "J. Infect. Dis.",
"key": "ref_79",
"volume": "203",
"year": "2011"
},
{
"DOI": "10.1097/01.aids.0000210617.90954.0e",
"article-title": "The Effect of Atorvastatin Treatment on HIV-1-Infected Patients Interrupting Antiretroviral Therapy",
"author": "Negredo",
"doi-asserted-by": "crossref",
"first-page": "619",
"journal-title": "AIDS",
"key": "ref_80",
"volume": "20",
"year": "2006"
},
{
"DOI": "10.1016/j.ahj.2018.11.012",
"article-title": "Differences in Statin Utilization and Lipid Lowering by Race, Ethnicity, and HIV Status in a Real-World Cohort of Persons with Human Immunodeficiency Virus and Uninfected Persons",
"author": "Riestenberg",
"doi-asserted-by": "crossref",
"first-page": "79",
"journal-title": "Am. Heart J.",
"key": "ref_81",
"volume": "209",
"year": "2019"
},
{
"DOI": "10.1093/jac/dkm470",
"article-title": "Association between HIV Replication and Cholesterol in Peripheral Blood Mononuclear Cells in HIV-Infected Patients Interrupting HAART",
"author": "Negredo",
"doi-asserted-by": "crossref",
"first-page": "400",
"journal-title": "J. Antimicrob. Chemother.",
"key": "ref_82",
"volume": "61",
"year": "2008"
},
{
"DOI": "10.1310/hct1303-153",
"article-title": "Statin Therapy Decreases Serum Levels of High-Sensitivity C-Reactive Protein and Tumor Necrosis Factor-α in HIV-Infected Patients Treated with Ritonavir-Boosted Protease Inhibitors",
"author": "Calza",
"doi-asserted-by": "crossref",
"first-page": "153",
"journal-title": "HIV Clin. Trials",
"key": "ref_83",
"volume": "13",
"year": "2012"
},
{
"DOI": "10.1164/rccm.201712-2570OC",
"article-title": "AMP-Activated Protein Kinase Phosphorylation of Angiotensin-Converting Enzyme 2 in Endothelium Mitigates Pulmonary Hypertension",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "509",
"journal-title": "Am. J. Respir. Crit. Care Med.",
"key": "ref_84",
"volume": "198",
"year": "2018"
},
{
"DOI": "10.1111/bph.12159",
"article-title": "ACE2, Angiotensin-(1-7) and Mas Receptor Axis in Inflammation and Fibrosis",
"author": "Silveira",
"doi-asserted-by": "crossref",
"first-page": "477",
"journal-title": "Br. J. Pharmacol.",
"key": "ref_85",
"volume": "169",
"year": "2013"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317015",
"article-title": "Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System",
"author": "Gheblawi",
"doi-asserted-by": "crossref",
"first-page": "1456",
"journal-title": "Circ. Res.",
"key": "ref_86",
"volume": "126",
"year": "2020"
},
{
"DOI": "10.1016/j.apsb.2020.10.006",
"article-title": "Angiotensin-Converting Enzyme 2 (ACE2): SARS-CoV-2 Receptor and RAS Modulator",
"author": "Bian",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Acta Pharm. Sin. B",
"key": "ref_87",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3390/ijms14047089",
"article-title": "Roles of Rho GTPases in Intracellular Transport and Cellular Transformation",
"author": "Chi",
"doi-asserted-by": "crossref",
"first-page": "7089",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref_88",
"volume": "14",
"year": "2013"
},
{
"DOI": "10.3390/ph15050589",
"doi-asserted-by": "crossref",
"key": "ref_89",
"unstructured": "Marcianò, G., Palleria, C., Casarella, A., Rania, V., Basile, E., Catarisano, L., Vocca, C., Bianco, L., Pelaia, C., and Cione, E. (2022). Effect of Statins on Lung Cancer Molecular Pathways: A Possible Therapeutic Role. Pharmaceuticals, 15."
},
{
"DOI": "10.1042/BJ20120150",
"article-title": "Ivermectin Is a Specific Inhibitor of Importin α/β-Mediated Nuclear Import Able to Inhibit Replication of HIV-1 and Dengue Virus",
"author": "Wagstaff",
"doi-asserted-by": "crossref",
"first-page": "851",
"journal-title": "Biochem. J.",
"key": "ref_90",
"volume": "443",
"year": "2012"
},
{
"DOI": "10.1016/S2666-5247(21)00114-2",
"article-title": "Combining Immunomodulators and Antivirals for COVID-19",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "e233",
"journal-title": "Lancet Microbe",
"key": "ref_91",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.02056",
"article-title": "Immunomodulatory and Antiviral Activity of Metformin and Its Potential Implications in Treating Coronavirus Disease 2019 and Lung Injury",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "2056",
"journal-title": "Front. Immunol.",
"key": "ref_92",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2014.09.018",
"article-title": "Metformin: From Mechanisms of Action to Therapies",
"author": "Foretz",
"doi-asserted-by": "crossref",
"first-page": "953",
"journal-title": "Cell Metab.",
"key": "ref_93",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1111/j.1751-1097.2012.01165.x",
"article-title": "Metformin, an Antidiabetic Agent Reduces Growth of Cutaneous Squamous Cell Carcinoma by Targeting mTOR Signaling Pathway†",
"author": "Chaudhary",
"doi-asserted-by": "crossref",
"first-page": "1149",
"journal-title": "Photochem. Photobiol.",
"key": "ref_94",
"volume": "88",
"year": "2012"
},
{
"DOI": "10.1016/j.tips.2020.01.003",
"article-title": "Context-Dependent Pharmacological Effects of Metformin on the Immune System",
"author": "Marcucci",
"doi-asserted-by": "crossref",
"first-page": "162",
"journal-title": "Trends Pharmacol. Sci.",
"key": "ref_95",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref_96",
"volume": "395",
"year": "2020"
},
{
"article-title": "M1 and M2 Macrophages: Oracles of Health and Disease",
"author": "Mills",
"first-page": "463",
"journal-title": "CRI",
"key": "ref_97",
"volume": "32",
"year": "2012"
},
{
"DOI": "10.1074/jbc.M115.662114",
"article-title": "Metformin Inhibits the Production of Reactive Oxygen Species from NADH:Ubiquinone Oxidoreductase to Limit Induction of Interleukin-1β (IL-1β) and Boosts Interleukin-10 (IL-10) in Lipopolysaccharide (LPS)-Activated Macrophages *",
"author": "Kelly",
"doi-asserted-by": "crossref",
"first-page": "20348",
"journal-title": "J. Biol. Chem.",
"key": "ref_98",
"volume": "290",
"year": "2015"
},
{
"DOI": "10.18632/oncotarget.5541",
"article-title": "Metformin Prevents Cancer Metastasis by Inhibiting M2-like Polarization of Tumor Associated Macrophages",
"author": "Ding",
"doi-asserted-by": "crossref",
"first-page": "36441",
"journal-title": "Oncotarget",
"key": "ref_99",
"volume": "6",
"year": "2015"
},
{
"DOI": "10.1038/s44276-023-00022-w",
"article-title": "Metformin May Improve the Outcome of Patients with Colorectal Cancer and Type 2 Diabetes Mellitus Partly through Effects on Neutrophil Extracellular Traps",
"author": "Saito",
"doi-asserted-by": "crossref",
"first-page": "20",
"journal-title": "BJC Rep.",
"key": "ref_100",
"volume": "1",
"year": "2023"
},
{
"DOI": "10.1186/s12985-023-02116-w",
"article-title": "Neutrophils in COVID-19: Recent Insights and Advances",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "169",
"journal-title": "Virol. J.",
"key": "ref_101",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1016/j.jneuroim.2016.01.014",
"article-title": "Metformin Ameliorates the Development of Experimental Autoimmune Encephalomyelitis by Regulating T Helper 17 and Regulatory T Cells in Mice",
"author": "Sun",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "J. Neuroimmunol.",
"key": "ref_102",
"volume": "292",
"year": "2016"
},
{
"DOI": "10.1007/s00018-023-04932-3",
"article-title": "Metformin Induces Tolerogenicity of Dendritic Cells by Promoting Metabolic Reprogramming",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "283",
"journal-title": "Cell Mol. Life Sci.",
"key": "ref_103",
"volume": "80",
"year": "2023"
},
{
"DOI": "10.1038/s41467-023-42277-4",
"article-title": "Inflammatory Macrophages Reprogram to Immunosuppression by Reducing Mitochondrial Translation",
"author": "Brischetto",
"doi-asserted-by": "crossref",
"first-page": "7471",
"journal-title": "Nat. Commun.",
"key": "ref_104",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1046/j.1365-2796.2002.00966.x",
"article-title": "Effects of Simvastatin and Atorvastatin on Inflammation Markers in Plasma",
"author": "Wiklund",
"doi-asserted-by": "crossref",
"first-page": "338",
"journal-title": "J. Intern. Med.",
"key": "ref_105",
"volume": "251",
"year": "2002"
},
{
"DOI": "10.1007/s10787-023-01240-x",
"article-title": "The Potential Therapeutic Effect of Statins in Multiple Sclerosis: Beneficial or Detrimental Effects",
"author": "Saad",
"doi-asserted-by": "crossref",
"first-page": "1671",
"journal-title": "Inflammopharmacology",
"key": "ref_106",
"volume": "31",
"year": "2023"
},
{
"DOI": "10.1111/j.1365-2249.2011.04331.x",
"article-title": "The Role of Atorvastatin in Regulating the Immune Response Leading to Vascular Damage in a Model of Kawasaki Disease",
"author": "Blankier",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Clin. Exp. Immunol.",
"key": "ref_107",
"volume": "164",
"year": "2011"
},
{
"DOI": "10.15420/ecr.2019.9.2",
"article-title": "The Effect of Statins on the Functionality of CD4+CD25+FOXP3+ Regulatory T-Cells in Acute Coronary Syndrome: A Systematic Review and Meta-Analysis of Randomised Controlled Trials in Asian Populations",
"author": "Sorathia",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Eur. Cardiol.",
"key": "ref_108",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1007/s11882-015-0548-7",
"article-title": "Regulation of Adaptive Immunity in Health and Disease by Cholesterol Metabolism",
"author": "Fessler",
"doi-asserted-by": "crossref",
"first-page": "48",
"journal-title": "Curr. Allergy Asthma Rep.",
"key": "ref_109",
"volume": "15",
"year": "2015"
},
{
"DOI": "10.3390/immuno2020021",
"article-title": "The Immunomodulatory Effects of Statins on Macrophages",
"author": "Sheridan",
"doi-asserted-by": "crossref",
"first-page": "317",
"journal-title": "Immuno",
"key": "ref_110",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1016/j.jdiacomp.2022.108391",
"article-title": "Metformin in SARS-CoV-2 Infection: A Hidden Path—From Altered Inflammation to Reduced Mortality. A Review from the Literature",
"author": "Pedrosa",
"doi-asserted-by": "crossref",
"first-page": "108391",
"journal-title": "J. Diabetes Complicat.",
"key": "ref_111",
"volume": "37",
"year": "2023"
},
{
"DOI": "10.1016/j.diabet.2020.07.006",
"article-title": "Metformin and COVID-19: From Cellular Mechanisms to Reduced Mortality",
"author": "Scheen",
"doi-asserted-by": "crossref",
"first-page": "423",
"journal-title": "Diabetes Metab.",
"key": "ref_112",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.5455/medarh.2022.76.329-332",
"article-title": "Effects of Metformin, Insulin on Hematological Parameters of COVID-19 Patients with Type 2 Diabetes",
"author": "Petakh",
"doi-asserted-by": "crossref",
"first-page": "329",
"journal-title": "Med. Arch.",
"key": "ref_113",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.3390/ijms241914822",
"doi-asserted-by": "crossref",
"key": "ref_114",
"unstructured": "Moreno-Corona, N.C., López-Ortega, O., Pérez-Martínez, C.A., Martínez-Castillo, M., De Jesús-González, L.A., León-Reyes, G., and León-Juárez, M. (2023). Dynamics of the Microbiota and Its Relationship with Post-COVID-19 Syndrome. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.3390/v14030477",
"doi-asserted-by": "crossref",
"key": "ref_115",
"unstructured": "Petakh, P., Kamyshna, I., Nykyforuk, A., Yao, R., Imbery, J.F., Oksenych, V., Korda, M., and Kamyshnyi, A. (2022). Immunoregulatory Intestinal Microbiota and COVID-19 in Patients with Type Two Diabetes: A Double-Edged Sword. Viruses, 14."
},
{
"DOI": "10.20944/preprints202304.1127.v1",
"doi-asserted-by": "crossref",
"key": "ref_116",
"unstructured": "Petakh, P., Kamyshna, I., Oksenych, V., Kainov, D., and Kamyshnyi, A. (2023). Metformin Therapy Changes Gut Microbiota Alpha-Diversity in COVID-19 Patients with Type 2 Diabetes: The Role of SARS-CoV-2 Variants and Antibiotic Treatment. Pharmaceuticals, 16."
},
{
"DOI": "10.1186/s13054-020-03154-4",
"article-title": "Atorvastatin Associated with Decreased Hazard for Death in COVID-19 Patients Admitted to an ICU: A Retrospective Cohort Study",
"author": "Chung",
"doi-asserted-by": "crossref",
"first-page": "429",
"journal-title": "Crit. Care",
"key": "ref_117",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.3389/fcvm.2022.820260",
"article-title": "Statin Use in COVID-19 Hospitalized Patients and Outcomes: A Retrospective Study",
"author": "Kouhpeikar",
"doi-asserted-by": "crossref",
"first-page": "820260",
"journal-title": "Front. Cardiovasc. Med.",
"key": "ref_118",
"volume": "9",
"year": "2022"
},
{
"article-title": "Promising Effects of Atorvastatin on Mortality and Need for Mechanical Ventilation in Patients with Severe COVID-19; a Retrospective Cohort Study",
"author": "Moradi",
"first-page": "e14434",
"journal-title": "Int. J. Clin. Pract.",
"key": "ref_119",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.3389/fcvm.2022.992686",
"article-title": "The Rationale for the Treatment of Long-Covid Symptoms—A Cardiologist’s View",
"author": "Schieffer",
"doi-asserted-by": "crossref",
"first-page": "992686",
"journal-title": "Front. Cardiovasc. Med.",
"key": "ref_120",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1002/jmv.28971",
"article-title": "Outpatient Atorvastatin Use and Severe COVID-19 Outcomes: A Population-Based Study",
"author": "Herdeiro",
"doi-asserted-by": "crossref",
"first-page": "e28971",
"journal-title": "J. Med. Virol.",
"key": "ref_121",
"volume": "95",
"year": "2023"
},
{
"article-title": "Metformin Reduced SARS-CoV-2 Viral Load in a Phase 3 Randomized Clinical Trial",
"author": "Boulware",
"first-page": "70",
"journal-title": "Top. Antivir. Med.",
"key": "ref_122",
"volume": "31",
"year": "2023"
},
{
"DOI": "10.1016/j.ijid.2012.02.004",
"article-title": "The Effect of Metformin on the Efficacy of Antiviral Therapy in Patients with Genotype 1 Chronic Hepatitis C and Insulin Resistance",
"author": "Yu",
"doi-asserted-by": "crossref",
"first-page": "e436",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_123",
"volume": "16",
"year": "2012"
},
{
"DOI": "10.3389/fendo.2020.00191",
"article-title": "Metformin and Its Benefits for Various Diseases",
"author": "Lv",
"doi-asserted-by": "crossref",
"first-page": "191",
"journal-title": "Front. Endocrinol.",
"key": "ref_124",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/S0212-6567(01)78767-7",
"article-title": "Análisis coste-efectividad de atorvastatina frente a simvastatina como tratamiento hipolipemiante en pacientes hipercolesterolémicos en atención primaria",
"doi-asserted-by": "crossref",
"first-page": "18",
"journal-title": "Aten Primaria",
"key": "ref_125",
"volume": "27",
"year": "2001"
},
{
"DOI": "10.1093/ofid/ofac174",
"article-title": "Barriers to Worldwide Access for Paxlovid, a New Treatment for COVID-19",
"author": "Pepperrell",
"doi-asserted-by": "crossref",
"first-page": "ofac174",
"journal-title": "Open Forum Infect. Dis.",
"key": "ref_126",
"volume": "9",
"year": "2022"
},
{
"key": "ref_127",
"unstructured": "Corcoran, C., and Jacobs, T.F. (2023). StatPearls, StatPearls Publishing."
},
{
"key": "ref_128",
"unstructured": "(2023, June 13). DOF—Diario Oficial de La Federación. Available online: https://www.dof.gob.mx/nota_detalle.php?codigo=5588819&fecha=10/03/2020#gsc.tab=0."
}
],
"reference-count": 128,
"references-count": 128,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-2607/12/2/383"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Virology",
"Microbiology (medical)",
"Microbiology"
],
"subtitle": [],
"title": "A Dual Pharmacological Strategy against COVID-19: The Therapeutic Potential of Metformin and Atorvastatin",
"type": "journal-article",
"volume": "12"
}
