Metformin reduces the risk of developing influenza A virus related cardiovascular disease
et al., Heliyon, doi:10.1016/j.heliyon.2023.e20284, Sep 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
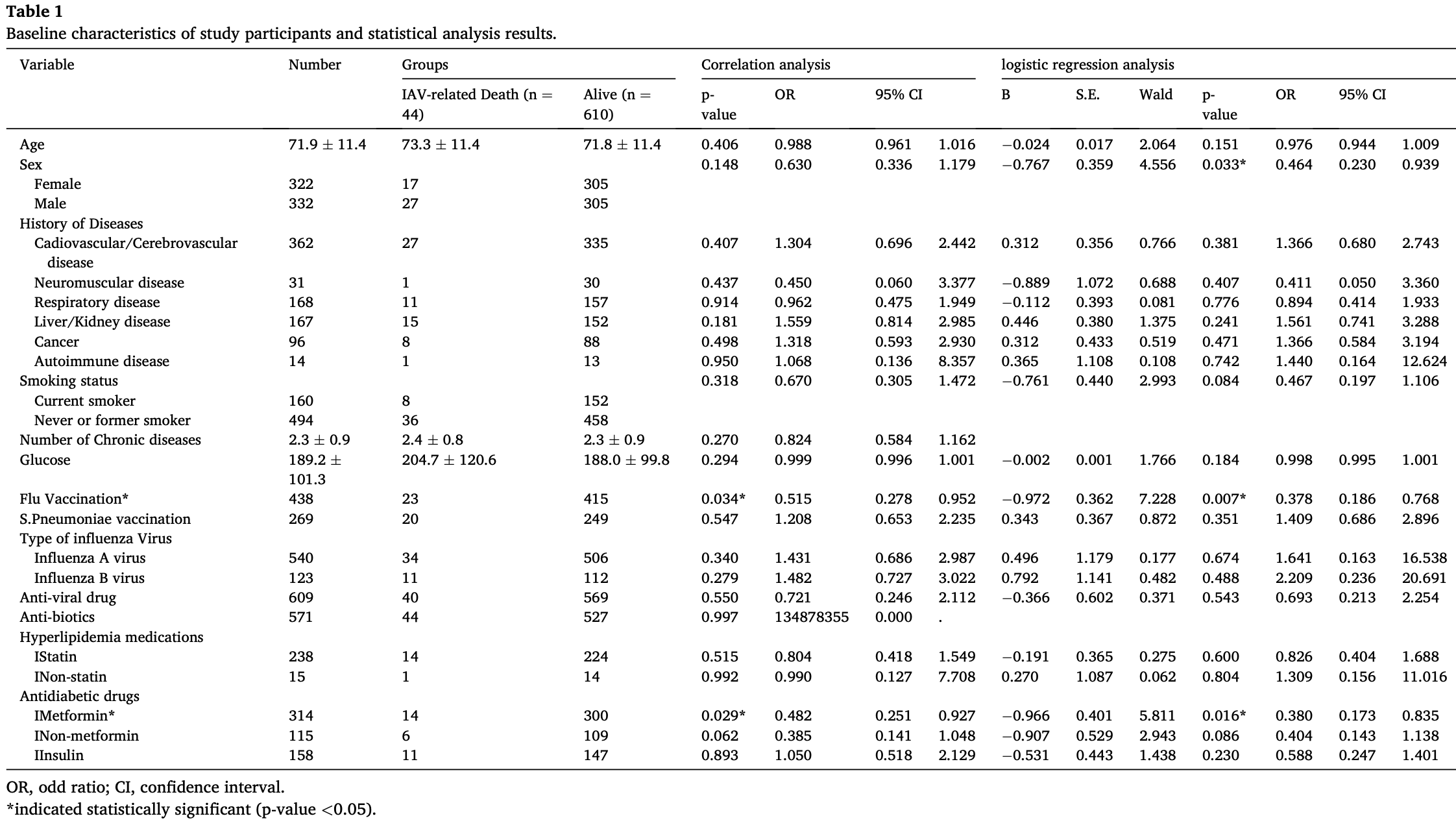
Retrospective clinical study, in vitro study, and mouse study of metformin for influenza A virus (IAV) infection. Authors performed a retrospective analysis of 654 diabetic patients, finding that metformin treatment was associated with a 62% reduction in IAV-related mortality. In vitro experiments in IAV-infected cells showed that metformin suppressed viral replication and reduced expression of the pro-inflammatory cytokines MCP-1 and IP-10, which are implicated in cardiovascular disease. In vivo studies in atherosclerotic mice confirmed that metformin treatment inhibited IAV-induced MCP-1 and IP-10 expression and attenuated IAV-exacerbated atherosclerotic plaque development. Authors suggest metformin's immunomodulatory effects, mediated through AKT/MAPK signaling, may alleviate acute cardiovascular events in IAV-infected patients. Overall, this study demonstrates metformin's antiviral and anti-inflammatory properties and its potential to reduce influenza-related cardiovascular complications.
Lee et al., 28 Sep 2023, peer-reviewed, 5 authors.
Contact: wjkim@korea.ac.kr.
Metformin reduces the risk of developing influenza A virus related cardiovascular disease
Heliyon, doi:10.1016/j.heliyon.2023.e20284
A C T This study investigated the drug repositioning potential of metformin for cardiovascular risk due to influenza A virus infection. Statistical analysis was performed to analyze factors related to the risk of death after IAV infection in diabetic patients. Through in vitro and in vivo experiments, the effect of metformin on influenza A virus infection in non-diabetic conditions was analyzed. In logistic regression analysis, influenza vaccination (OR = 0.378, p-value = 0.007, 0.186 < 95% C⋅I < 0.768) and metformin treatment (OR = 0.380, p-value = 0.016, 0.173 < 95% C⋅I < 0.835) were associated with a decreased influenza-related mortality in diabetic patients. In vitro and in vivo studies showed that viral replication and influenza A virus-induced cytokine expression were inhibited by metformin. In particular, MCP-1 and IP-10, cytokines related to cell infiltration and cardiovascular disease development, were significantly reduced by metformin under influenza A virus infection condition. As a result, the acute exacerbation of atherosclerosis caused by influenza A virus in mouse aorta was inhibited by metformin. In addition, we found that regulation of AKT/MAPK signaling plays an important role in the mechanism of metformin. In conclusion, we demonstrated the potential and mechanism of metformin as a treatment for acute exacerbation of atherosclerosis caused by influenza A virus infection.
Heliyon 9 (2023) e20284
Author contribution statement Han Sol Lee: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper. Woo Joo Kim: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper. Ji Yun Noh, Joon Young Song, Hee Jin Cheong: Analyzed and interpreted the data.
Declaration of competing interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e20284.
References
References
Abdel Monem, Farid, Abbassi, Youssry, Andraues et al., The potential hepatoprotective effect of metformin in hepatitis C virus-infected adolescent patients with beta thalassemia major: randomised clinical trial, Int. J. Clin. Pract, doi:10.1111/ijcp.14104
Amoani, Sakyi, Mantey, Laing, Ephraim et al., Increased metformin dosage suppresses proinflammatory cytokine levels in systemic circulation and might contribute to its beneficial effects, J. Immunoassay Immunochem, doi:10.1080/15321819.2020.1862861
Arkun, Dynamic modeling and analysis of the cross-talk between insulin/AKT and MAPK/ERK signaling pathways, PLoS One, doi:10.1371/journal.pone.0149684
Aroda, Ratner, Metformin and type 2 diabetes prevention, Diabetes Spectr, doi:10.2337/ds18-0020
Benjamin, Virani, Callaway, Chamberlain, Chang et al., American heart association council on epidemiology and prevention statistics committee and stroke statistics subcommittee. Heart disease and stroke statistics-2018 update: a report from the American heart association, Circulation, doi:10.1161/CIR.0000000000000558
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Lancet Healthy Longev, doi:10.1016/S2666-7568(20)30033-7
Chen, Liu, Ye, Effects of metformin on blood and urine pro-inflammatory mediators in patients with type 2 diabetes, J. Inflamm, doi:10.1186/s12950-016-0142-3
Chen, Wang, Liu, Su, Zhang et al., IP-10 and MCP-1 as biomarkers associated with disease severity of COVID-19, Mol. Med, doi:10.1186/s10020-020-00230-x
Christodoulidis, Vittorio, Fudim, Lerakis, Kosmas, Inflammation in coronary artery disease, Cardiol. Rev, doi:10.1097/CRD.0000000000000006
Ding, Zhou, Long, Chen, Zhao et al., DUSP8 phosphatase: structure, functions, expression regulation and the role in human diseases, Cell Biosci, doi:10.1186/s13578-019-0329-4
Dragomir, Simionescu, Monocyte chemoattractant protein-1-a major contributor to the inflammatory process associated with diabetes, Arch. Physiol. Biochem, doi:10.1080/13813450601094672
Farfan-Morales, Cordero-Rivera, Osuna-Ramos, Monroy-Muñoz, De Jesús-González et al., The antiviral effect of metformin on zika and dengue virus infection, Sci. Rep, doi:10.1038/s41598-021-87707-9
Fey, Croucher, Kolch, Kholodenko, Crosstalk and signaling switches in mitogen-activated protein kinase cascades, Front. Physiol, doi:10.3389/fphys.2012.00355
Han, Xie, Liu, Gao, Yang et al., Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: a systematic review and an updated meta-analysis, Cardiovasc. Diabetol, doi:10.1186/s12933-019-0900-7
Ko, Fujiwara, Krishnan, Abe, En face preparation of mouse blood vessels, J. Vis. Exp, doi:10.3791/55460
Lang, Raffi, Dual-specificity phosphatases in immunity and infection: an update, Int. J. Mol. Sci, doi:10.3390/ijms20112710
Lee, Noh, Shin, Song, Cheong et al., Matrix metalloproteinase-13 in atherosclerotic plaque is increased by influenza A virus infection, J. Infect. Dis, doi:10.1093/infdis/jiz580
Lexis, Van Der Horst-Schrivers, Lipsic, Valente, Muller Kobold et al., The effect of metformin on cardiovascular risk profile in patients without diabetes presenting with acute myocardial infarction: data from the Glycometabolic Intervention as adjunct to Primary Coronary Intervention in ST Elevation Myocardial Infarction (GIPS-III) trial, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2015-000090
Lloyd-Jones, Braun, Ndumele, Smith, Sperling et al., Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American heart association and American College of cardiology, Circulation, doi:10.1161/CIR.0000000000000638
Lopez, Mathers, Ezzati, Jamison, Murray, Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data, Lancet, doi:10.1016/S0140-6736(06)68770-9
Luo, Das, Chen, Wu, Li et al., Metformin in patients with and without diabetes: a paradigm shift in cardiovascular disease management, Cardiovasc. Diabetol, doi:10.1186/s12933-019-0860-y
Matheus, Tannus, Cobas, Palma, Negrato et al., Impact of diabetes on cardiovascular disease: an update, Int. J. Hypertens, doi:10.1155/2013/653789
Mócsai, Ruland, Tybulewicz, The SYK tyrosine kinase: a crucial player in diverse biological functions, Nat. Rev. Immunol, doi:10.1038/nri2765
Noels, Weber, Koenen, Chemokines as therapeutic targets in cardiovascular disease, Arterioscler. Thromb. Vasc. Biol, doi:10.1161/ATVBAHA.118.312037
Rena, Hardie, Pearson, The mechanisms of action of metformin, Diabetologia, doi:10.1007/s00125-017-4342-z
Rena, Lang, Repurposing metformin for cardiovascular disease, Circulation, doi:10.1161/CIRCULATIONAHA.117.031735
Saisho, Metformin and inflammation: its potential beyond glucose-lowering effect, Endocr., Metab. Immune Disord.: Drug Targets, doi:10.2174/1871530315666150316124019
Saraei, Asadi, Kakar, Moradi-Kor, The beneficial effects of metformin on cancer prevention and therapy: a comprehensive review of recent advances, Cancer Manag. Res, doi:10.2147/CMAR.S200059
Tsuji, Hashimoto-Hachiya, Yen, Takemura, Yumine et al., Metformin inhibits IL-1β secretion via impairment of NLRP3 inflammasome in keratinocytes: implications for preventing the development of psoriasis, Cell Death Dis, doi:10.1038/s41420-020-0245-8
Webster, Scott, What cardiologists need to know about diabetes, Lancet, doi:10.1016/s0140-6736(97)90025-8
Yang, Qin, Wang, Meng, Xian et al., Metformin inhibits the NLRP3 inflammasome via AMPK/mTORdependent effects in diabetic cardiomyopathy, Int. J. Biol. Sci, doi:10.7150/ijbs.29680
Zheng, Xu, Dong, Li, NLRP3 inflammasome: the rising star in cardiovascular diseases, Front Cardiovasc Med, doi:10.3389/fcvm.2022.927061
DOI record:
{
"DOI": "10.1016/j.heliyon.2023.e20284",
"ISSN": [
"2405-8440"
],
"URL": "http://dx.doi.org/10.1016/j.heliyon.2023.e20284",
"alternative-id": [
"S2405844023074923"
],
"article-number": "e20284",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Metformin reduces the risk of developing influenza A virus related cardiovascular disease"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Heliyon"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.heliyon.2023.e20284"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Authors. Published by Elsevier Ltd."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1846-1772",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lee",
"given": "Han Sol",
"sequence": "first"
},
{
"affiliation": [],
"family": "Noh",
"given": "Ji Yun",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0148-7194",
"affiliation": [],
"authenticated-orcid": false,
"family": "Song",
"given": "Joon Young",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cheong",
"given": "Hee Jin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4546-3880",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kim",
"given": "Woo Joo",
"sequence": "additional"
}
],
"container-title": "Heliyon",
"container-title-short": "Heliyon",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"cell.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
9,
21
]
],
"date-time": "2023-09-21T23:55:26Z",
"timestamp": 1695340526000
},
"deposited": {
"date-parts": [
[
2023,
10,
2
]
],
"date-time": "2023-10-02T06:39:47Z",
"timestamp": 1696228787000
},
"funder": [
{
"DOI": "10.13039/501100003621",
"award": [
"2016R1A5A1010148"
],
"doi-asserted-by": "publisher",
"name": "Ministry of Science, ICT and Future Planning"
},
{
"DOI": "10.13039/501100003725",
"doi-asserted-by": "publisher",
"name": "National Research Foundation of Korea"
}
],
"indexed": {
"date-parts": [
[
2023,
10,
3
]
],
"date-time": "2023-10-03T13:40:57Z",
"timestamp": 1696340457685
},
"is-referenced-by-count": 0,
"issue": "10",
"issued": {
"date-parts": [
[
2023,
10
]
]
},
"journal-issue": {
"issue": "10",
"published-print": {
"date-parts": [
[
2023,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
10,
1
]
],
"date-time": "2023-10-01T00:00:00Z",
"timestamp": 1696118400000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
18
]
],
"date-time": "2023-09-18T00:00:00Z",
"timestamp": 1694995200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2405844023074923?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2405844023074923?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "e20284",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
10
]
]
},
"published-print": {
"date-parts": [
[
2023,
10
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S0140-6736(06)68770-9",
"article-title": "Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data",
"author": "Lopez",
"doi-asserted-by": "crossref",
"first-page": "1747",
"issue": "9524",
"journal-title": "Lancet",
"key": "10.1016/j.heliyon.2023.e20284_bib1",
"volume": "367",
"year": "2006"
},
{
"DOI": "10.1161/CIR.0000000000000558",
"article-title": "American heart association council on epidemiology and prevention statistics committee and stroke statistics subcommittee. Heart disease and stroke statistics-2018 update: a report from the American heart association",
"author": "Benjamin",
"doi-asserted-by": "crossref",
"first-page": "e67",
"issue": "12",
"journal-title": "Circulation",
"key": "10.1016/j.heliyon.2023.e20284_bib2",
"volume": "137",
"year": "2018"
},
{
"DOI": "10.1161/CIR.0000000000000638",
"article-title": "Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American heart association and American College of cardiology",
"author": "Lloyd-Jones",
"doi-asserted-by": "crossref",
"first-page": "e1162",
"issue": "25",
"journal-title": "Circulation",
"key": "10.1016/j.heliyon.2023.e20284_bib3",
"volume": "139",
"year": "2019"
},
{
"DOI": "10.1016/S0140-6736(97)90025-8",
"article-title": "What cardiologists need to know about diabetes",
"author": "Webster",
"doi-asserted-by": "crossref",
"first-page": "SI23",
"issue": "Suppl 1",
"journal-title": "Lancet",
"key": "10.1016/j.heliyon.2023.e20284_bib4",
"volume": "350",
"year": "1997"
},
{
"DOI": "10.1155/2013/653789",
"article-title": "Impact of diabetes on cardiovascular disease: an update",
"author": "Matheus",
"doi-asserted-by": "crossref",
"journal-title": "Int. J. Hypertens.",
"key": "10.1016/j.heliyon.2023.e20284_bib5",
"volume": "2013",
"year": "2013"
},
{
"DOI": "10.1097/CRD.0000000000000006",
"article-title": "Inflammation in coronary artery disease",
"author": "Christodoulidis",
"doi-asserted-by": "crossref",
"first-page": "279",
"issue": "6",
"journal-title": "Cardiol. Rev.",
"key": "10.1016/j.heliyon.2023.e20284_bib6",
"volume": "22",
"year": "2014"
},
{
"DOI": "10.1007/s00125-017-4342-z",
"article-title": "The mechanisms of action of metformin",
"author": "Rena",
"doi-asserted-by": "crossref",
"first-page": "1577",
"issue": "9",
"journal-title": "Diabetologia",
"key": "10.1016/j.heliyon.2023.e20284_bib7",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.2337/ds18-0020",
"article-title": "Metformin and type 2 diabetes prevention",
"author": "Aroda",
"doi-asserted-by": "crossref",
"first-page": "336",
"issue": "4",
"journal-title": "Diabetes Spectr.",
"key": "10.1016/j.heliyon.2023.e20284_bib8",
"volume": "31",
"year": "2018"
},
{
"DOI": "10.1080/15321819.2020.1862861",
"article-title": "Increased metformin dosage suppresses pro-inflammatory cytokine levels in systemic circulation and might contribute to its beneficial effects",
"author": "Amoani",
"doi-asserted-by": "crossref",
"first-page": "252",
"issue": "3",
"journal-title": "J. Immunoassay Immunochem.",
"key": "10.1016/j.heliyon.2023.e20284_bib9",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1186/s12950-016-0142-3",
"article-title": "Effects of metformin on blood and urine pro-inflammatory mediators in patients with type 2 diabetes",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "34",
"journal-title": "J. Inflamm.",
"key": "10.1016/j.heliyon.2023.e20284_bib10",
"volume": "13",
"year": "2016"
},
{
"DOI": "10.1186/s12933-019-0860-y",
"article-title": "Metformin in patients with and without diabetes: a paradigm shift in cardiovascular disease management",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "54",
"issue": "1",
"journal-title": "Cardiovasc. Diabetol.",
"key": "10.1016/j.heliyon.2023.e20284_bib11",
"volume": "18",
"year": "2019"
},
{
"DOI": "10.1186/s12933-019-0900-7",
"article-title": "Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: a systematic review and an updated meta-analysis",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "96",
"issue": "1",
"journal-title": "Cardiovasc. Diabetol.",
"key": "10.1016/j.heliyon.2023.e20284_bib12",
"volume": "18",
"year": "2019"
},
{
"DOI": "10.1136/bmjdrc-2015-000090",
"author": "Lexis",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "BMJ Open Diabetes Res Care",
"key": "10.1016/j.heliyon.2023.e20284_bib13",
"volume": "3",
"year": "2015"
},
{
"DOI": "10.1161/CIRCULATIONAHA.117.031735",
"article-title": "Repurposing metformin for cardiovascular disease",
"author": "Rena",
"doi-asserted-by": "crossref",
"first-page": "422",
"issue": "5",
"journal-title": "Circulation",
"key": "10.1016/j.heliyon.2023.e20284_bib14",
"volume": "137",
"year": "2018"
},
{
"DOI": "10.2147/CMAR.S200059",
"article-title": "The beneficial effects of metformin on cancer prevention and therapy: a comprehensive review of recent advances",
"author": "Saraei",
"doi-asserted-by": "crossref",
"first-page": "3295",
"journal-title": "Cancer Manag. Res.",
"key": "10.1016/j.heliyon.2023.e20284_bib15",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.2174/1871530315666150316124019",
"article-title": "Metformin and inflammation: its potential beyond glucose-lowering effect",
"author": "Saisho",
"doi-asserted-by": "crossref",
"first-page": "196",
"issue": "3",
"journal-title": "Endocr., Metab. Immune Disord.: Drug Targets",
"key": "10.1016/j.heliyon.2023.e20284_bib16",
"volume": "15",
"year": "2015"
},
{
"DOI": "10.1093/infdis/jiz580",
"article-title": "Matrix metalloproteinase-13 in atherosclerotic plaque is increased by influenza A virus infection",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "256",
"issue": "2",
"journal-title": "J. Infect. Dis.",
"key": "10.1016/j.heliyon.2023.e20284_bib17",
"volume": "221",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0149684",
"article-title": "Dynamic modeling and analysis of the cross-talk between insulin/AKT and MAPK/ERK signaling pathways",
"author": "Arkun",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "PLoS One",
"key": "10.1016/j.heliyon.2023.e20284_bib18",
"volume": "11",
"year": "2016"
},
{
"DOI": "10.3389/fphys.2012.00355",
"article-title": "Crosstalk and signaling switches in mitogen-activated protein kinase cascades",
"author": "Fey",
"doi-asserted-by": "crossref",
"first-page": "355",
"journal-title": "Front. Physiol.",
"key": "10.1016/j.heliyon.2023.e20284_bib19",
"volume": "3",
"year": "2012"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "e34",
"issue": "1",
"journal-title": "Lancet Healthy Longev",
"key": "10.1016/j.heliyon.2023.e20284_bib20",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-87707-9",
"article-title": "The antiviral effect of metformin on zika and dengue virus infection",
"author": "Farfan-Morales",
"doi-asserted-by": "crossref",
"first-page": "8743",
"issue": "1",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.heliyon.2023.e20284_bib21",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1111/ijcp.14104",
"article-title": "The potential hepatoprotective effect of metformin in hepatitis C virus-infected adolescent patients with beta thalassemia major: randomised clinical trial",
"author": "Abdel Monem",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Int. J. Clin. Pract.",
"key": "10.1016/j.heliyon.2023.e20284_bib22",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1161/ATVBAHA.118.312037",
"article-title": "Chemokines as therapeutic targets in cardiovascular disease",
"author": "Noels",
"doi-asserted-by": "crossref",
"first-page": "583",
"issue": "4",
"journal-title": "Arterioscler. Thromb. Vasc. Biol.",
"key": "10.1016/j.heliyon.2023.e20284_bib23",
"volume": "39",
"year": "2019"
},
{
"DOI": "10.1080/13813450601094672",
"article-title": "Monocyte chemoattractant protein-1--a major contributor to the inflammatory process associated with diabetes",
"author": "Dragomir",
"doi-asserted-by": "crossref",
"first-page": "239",
"issue": "4–5",
"journal-title": "Arch. Physiol. Biochem.",
"key": "10.1016/j.heliyon.2023.e20284_bib24",
"volume": "112",
"year": "2006"
},
{
"DOI": "10.1186/s10020-020-00230-x",
"article-title": "IP-10 and MCP-1 as biomarkers associated with disease severity of COVID-19",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "97",
"issue": "1",
"journal-title": "Mol. Med.",
"key": "10.1016/j.heliyon.2023.e20284_bib25",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1038/s41420-020-0245-8",
"article-title": "Metformin inhibits IL-1β secretion via impairment of NLRP3 inflammasome in keratinocytes: implications for preventing the development of psoriasis",
"author": "Tsuji",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "Cell Death Dis.",
"key": "10.1016/j.heliyon.2023.e20284_bib26",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.7150/ijbs.29680",
"article-title": "Metformin inhibits the NLRP3 inflammasome via AMPK/mTOR-dependent effects in diabetic cardiomyopathy",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "1010",
"issue": "5",
"journal-title": "Int. J. Biol. Sci.",
"key": "10.1016/j.heliyon.2023.e20284_bib27",
"volume": "15",
"year": "2019"
},
{
"DOI": "10.3389/fcvm.2022.927061",
"article-title": "NLRP3 inflammasome: the rising star in cardiovascular diseases",
"author": "Zheng",
"doi-asserted-by": "crossref",
"journal-title": "Front Cardiovasc Med",
"key": "10.1016/j.heliyon.2023.e20284_bib28",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.3390/ijms20112710",
"article-title": "Dual-specificity phosphatases in immunity and infection: an update",
"author": "Lang",
"doi-asserted-by": "crossref",
"first-page": "2710",
"issue": "11",
"journal-title": "Int. J. Mol. Sci.",
"key": "10.1016/j.heliyon.2023.e20284_bib29",
"volume": "20",
"year": "2019"
},
{
"DOI": "10.1186/s13578-019-0329-4",
"article-title": "DUSP8 phosphatase: structure, functions, expression regulation and the role in human diseases",
"author": "Ding",
"doi-asserted-by": "crossref",
"first-page": "70",
"journal-title": "Cell Biosci.",
"key": "10.1016/j.heliyon.2023.e20284_bib30",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1038/nri2765",
"article-title": "The SYK tyrosine kinase: a crucial player in diverse biological functions",
"author": "Mócsai",
"doi-asserted-by": "crossref",
"first-page": "387",
"issue": "6",
"journal-title": "Nat. Rev. Immunol.",
"key": "10.1016/j.heliyon.2023.e20284_bib31",
"volume": "10",
"year": "2010"
},
{
"article-title": "En face preparation of mouse blood vessels",
"author": "Ko",
"journal-title": "J. Vis. Exp.",
"key": "10.1016/j.heliyon.2023.e20284_bib32",
"volume": "123",
"year": "2017"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2405844023074923"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Metformin reduces the risk of developing influenza A virus related cardiovascular disease",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "9"
}
