The Role of the NRF2 Pathway in the Pathogenesis of Viral Respiratory Infections
et al., Pathogens, doi:10.3390/pathogens13010039, Dec 2023
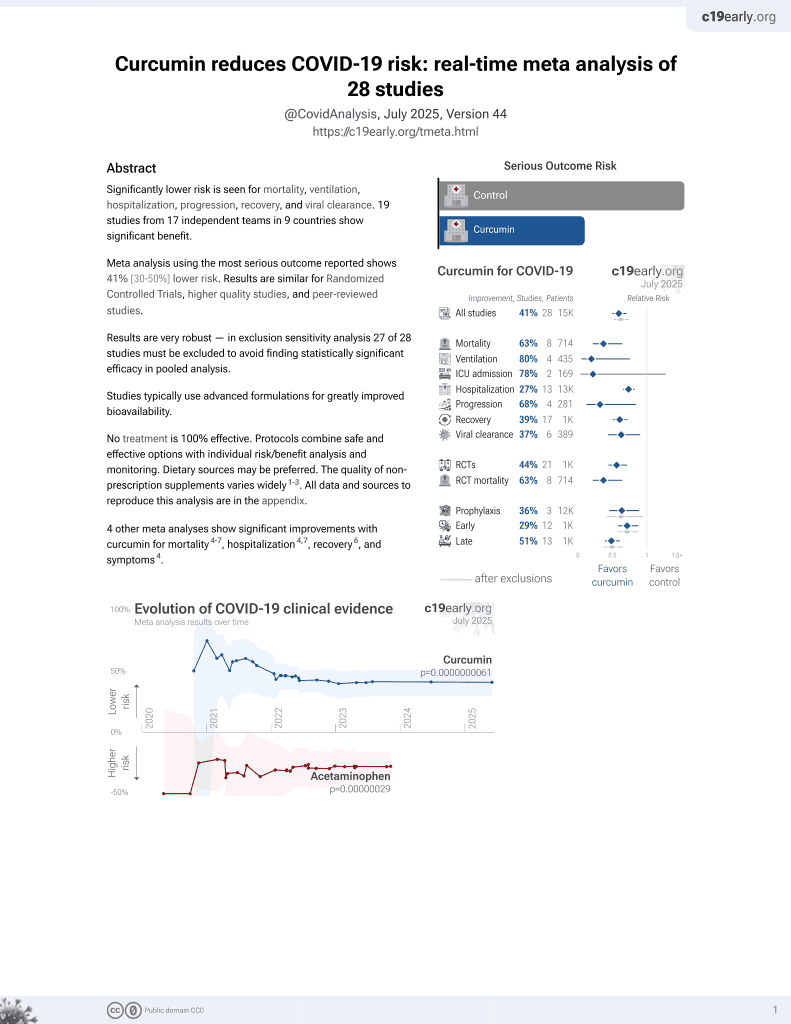
Curcumin for COVID-19
17th treatment shown to reduce risk in
February 2021, now with p = 0.0000000061 from 28 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
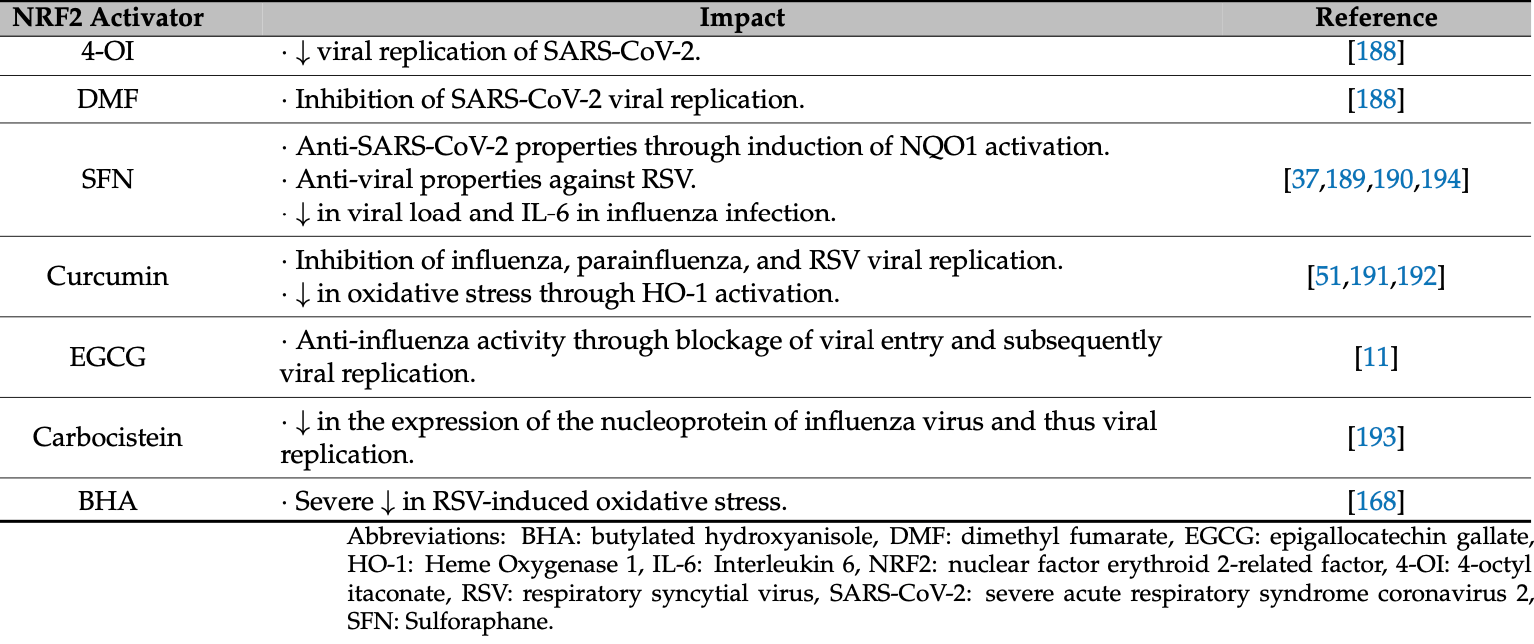
Review discussing the role of the NRF2 antioxidant pathway in regulating viral replication and associated inflammation and cell damage pathways during respiratory viral infections. Authors summarize evidence showing that respiratory viruses like SARS-CoV-2, influenza, RSV, and rhinoviruses can either activate or inhibit NRF2 signaling, while NRF2 activation also impacts viral entry, replication, apoptosis, and ferroptosis. NRF2-induced heme oxygenase-1 in particular demonstrates antiviral properties against these viruses. Authors conclude that balancing physiologic NRF2 pathway activation holds therapeutic potential for ameliorating viral pathogenesis, and suggest NRF2 agonists like curcumin, sulforaphane, and epigallocatechin gallate may be beneficial as adjuvants for COVID-19 and other respiratory viral infections.
Review covers curcumin and epigallocatechin gallate.
1.
Shokri-Afra et al., Targeting SIRT1: A Potential Strategy for Combating Severe COVID‐19, BioMed Research International, doi:10.1155/bmri/9507417.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Duan et al., Bioactive compounds,quercetin, curcumin and β-glucan,regulate innate immunity via the gut-liver-brain axis, Trends in Food Science & Technology, doi:10.1016/j.tifs.2024.104864.
4.
Rajak et al., Antiallergic Implications of Curcumin During COVID-19: Current Status and Perspectives, Biotechnology of Medicinal Plants with Antiallergy Properties, doi:10.1007/978-981-97-1467-4_4.
5.
Kali et al., Curcumin as a Promising Therapy for COVID-19: A Review, Global Journal of Medical, Pharmaceutical, and Biomedical Update, doi:10.25259/GJMPBU_78_2023.
6.
Vajdi et al., Effect of polyphenols against complications of COVID-19: current evidence and potential efficacy, Pharmacological Reports, doi:10.1007/s43440-024-00585-6.
7.
Yong et al., Natural Products-Based Inhaled Formulations for Treating Pulmonary Diseases, International Journal of Nanomedicine, doi:10.2147/ijn.s451206.
8.
Halma et al., Exploring autophagy in treating SARS-CoV-2 spike protein-related pathology, Endocrine and Metabolic Science, doi:10.1016/j.endmts.2024.100163.
9.
Arab et al., Immunoregulatory effects of nanocurcumin in inflammatory milieu: Focus on COVID-19, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2024.116131.
10.
Daskou et al., The Role of the NRF2 Pathway in the Pathogenesis of Viral Respiratory Infections, Pathogens, doi:10.3390/pathogens13010039.
11.
Law et al., Photodynamic Action of Curcumin and Methylene Blue against Bacteria and SARS-CoV-2—A Review, Pharmaceuticals, doi:10.3390/ph17010034.
12.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
13.
Hulscher et al., Clinical Approach to Post-acute Sequelae After COVID-19 Infection and Vaccination, Cureus, doi:10.7759/cureus.49204.
14.
Hegde et al., Curcumin Formulations for Better Bioavailability: What We Learned from Clinical Trials Thus Far?, ACS Omega, doi:10.1021/acsomega.2c07326.
Daskou et al., 31 Dec 2023, peer-reviewed, 8 authors.
The Role of the NRF2 Pathway in the Pathogenesis of Viral Respiratory Infections
Pathogens, doi:10.3390/pathogens13010039
In humans, acute and chronic respiratory infections caused by viruses are associated with considerable morbidity and mortality. Respiratory viruses infect airway epithelial cells and induce oxidative stress, yet the exact pathogenesis remains unclear. Oxidative stress activates the transcription factor NRF2, which plays a key role in alleviating redox-induced cellular injury. The transcriptional activation of NRF2 has been reported to affect both viral replication and associated inflammation pathways. There is complex bidirectional crosstalk between virus replication and the NRF2 pathway because virus replication directly or indirectly regulates NRF2 expression, and NRF2 activation can reversely hamper viral replication and viral spread across cells and tissues. In this review, we discuss the complex role of the NRF2 pathway in the regulation of the pathogenesis of the main respiratory viruses, including coronaviruses, influenza viruses, respiratory syncytial virus (RSV), and rhinoviruses. We also summarize the scientific evidence regarding the effects of the known NRF2 agonists that can be utilized to alter the NRF2 pathway.
Informed Consent Statement: Not applicable.
References
Ahmed, Luo, Namani, Wang, Tang, Nrf2 signaling pathway: Pivotal roles in inflammation, Biochim. Biophys. Acta Mol. Basis Dis, doi:10.1016/j.bbadis.2016.11.005
Ai, Zheng, Zhang, Fan, Inhibition of 12/15-LO ameliorates CVB3-induced myocarditis by activating Nrf2, Chem. Biol. Interact, doi:10.1016/j.cbi.2017.05.010
Alsuwaidi, Almarzooqi, Albawardi, Benedict, Kochiyil et al., Cellular bioenergetics, caspase activity and glutathione in murine lungs infected with influenza A virus, Virology, doi:10.1016/j.virol.2013.07.034
Andrew, Joseph, Sarah, Aurica, Patrick et al., LSC Abstract-Rhinovirus infection induces NRF2 in monocytes but not in epithelial cells, via distinct intracellular pathways, Eur. Respir. J, doi:10.1183/13993003.congress-2015.PA2607
Ashrafizadeh, Ahmadi, Mohammadinejad, Farkhondeh, Samarghandian, Curcumin Activates the Nrf2 Pathway and Induces Cellular Protection Against Oxidative Injury, Curr. Mol. Med, doi:10.2174/1566524019666191016150757
Bai, Zhao, Li, Sheng, Li, EV71 virus reduces Nrf2 activation to promote production of reactive oxygen species in infected cells, Gut Pathog, doi:10.1186/s13099-020-00361-w
Baird, Dinkova-Kostova, Diffusion dynamics of the Keap1-Cullin3 interaction in single live cells, Biochem. Biophys. Res. Commun, doi:10.1016/j.bbrc.2013.02.065
Baird, Lleres, Swift, Dinkova-Kostova, Regulatory flexibility in the Nrf2-mediated stress response is conferred by conformational cycling of the Keap1-Nrf2 protein complex, Proc. Natl. Acad. Sci, doi:10.1073/pnas.1305687110
Barati, Caster, The Potential of Nrf2 Activation as a Therapeutic Target in Systemic Lupus Erythematosus, Metabolites, doi:10.3390/metabo12020151
Batra, De Souza, Batra, Raetz, Yu, The HMOX1 Pathway as a Promising Target for the Treatment and Prevention of SARS-CoV-2 of 2019 (COVID-19), Int. J. Mol. Sci, doi:10.3390/ijms21176412
Bender, Hildt, Effect of Hepatitis Viruses on the Nrf2/Keap1-Signaling Pathway and Its Impact on Viral Replication and Pathogenesis, Int. J. Mol. Sci, doi:10.3390/ijms20184659
Berryman, Brooks, Burman, Hawes, Roberts et al., Foot-and-mouth disease virus induces autophagosomes during cell entry via a class III phosphatidylinositol 3-kinaseindependent pathway, J. Virol, doi:10.1128/JVI.00846-12
Biagioli, Kaul, Singh, Turner, The role of oxidative stress in rhinovirus induced elaboration of IL-8 by respiratory epithelial cells, Free Radic. Biol. Med, doi:10.1016/S0891-5849(98)00233-0
Campagna, Herranz, Garcia, Marcos-Villar, Gonzalez-Santamaria et al., SIRT1 stabilizes PML promoting its sumoylation, Cell Death Differ, doi:10.1038/cdd.2010.77
Carvajal-Yepes, Himmelsbach, Schaedler, Ploen, Krause et al., Hepatitis C virus impairs the induction of cytoprotective Nrf2 target genes by delocalization of small Maf proteins, J. Biol. Chem, doi:10.1074/jbc.M110.186684
Casola, Burger, Liu, Jamaluddin, Brasier et al., Oxidant tone regulates RANTES gene expression in airway epithelial cells infected with respiratory syncytial virus. Role in viral-induced interferon regulatory factor activation, J. Biol. Chem, doi:10.1074/jbc.M101526200
Castro, Guerrero-Plata, Suarez-Real, Adegboyega, Colasurdo et al., Antioxidant treatment ameliorates respiratory syncytial virus-induced disease and lung inflammation, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.200603-319OC
Cataneo, Tomiotto-Pellissier, Miranda-Sapla, Assolini, Panis et al., Quercetin promotes antipromastigote effect by increasing the ROS production and anti-amastigote by upregulating Nrf2/HO-1 expression, affecting iron availability, Biomed. Pharmacother, doi:10.1016/j.biopha.2019.108745
Cavezzi, Troiani, Corrao, COVID-19: Hemoglobin, iron, and hypoxia beyond inflammation. A narrative review, Clin. Pract, doi:10.4081/cp.2020.1271
Chartoumpekis, Fu, Ziros, Sykiotis, Patent Review (2017-2020) of the Keap1/Nrf2 Pathway Using PatSeer Pro: Focus on Autoimmune Diseases, Antioxidants, doi:10.3390/antiox9111138
Chen, Chen, Wen, Ou, Chiou et al., Inhibition of enveloped viruses infectivity by curcumin, PLoS ONE, doi:10.1371/journal.pone.0062482
Chen, Lee, Chuang, Li, Ning et al., Curcumin inhibits HCV replication by induction of heme oxygenase-1 and suppression of AKT, Int. J. Mol. Med, doi:10.3892/ijmm.2012.1096
Chen, Minakuchi, Wuputra, Ku, Pan et al., Redox control in the pathophysiology of influenza virus infection, BMC Microbiol, doi:10.1186/s12866-020-01890-9
Cheng, Lin, Chen, Tsai, Tsai et al., Activation of Nrf2 by the dengue virus causes an increase in CLEC5A, which enhances TNF-alpha production by mononuclear phagocytes, Sci. Rep, doi:10.1038/srep32000
Chistovich, Malinnikova, Stoliarova, Perception of single-formant vowels with irregular fluctuation of fundamental period and amplitude of glottal signals. Fiziol, Zhurnal SSSR Im. IM Sechenova
Cho, Imani, Miller-Degraff, Walters, Melendi et al., Antiviral activity of Nrf2 in a murine model of respiratory syncytial virus disease, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.200804-535OC
Choi, Bowman, Jung, Autophagy during viral infection-A double-edged sword, Nat. Rev. Microbiol, doi:10.1038/s41579-018-0003-6
Choi, Jiang, Shin, Jung, Severe Fever with Thrombocytopenia Syndrome Virus NSs Interacts with TRIM21 To Activate the p62-Keap1-Nrf2 Pathway, J. Virol, doi:10.1128/JVI.01684-19
Clementi, Ghosh, De Santis, Castelli, Criscuolo et al., Viral Respiratory Pathogens and Lung Injury, Clin. Microbiol. Rev, doi:10.1128/CMR.00103-20
Cuadrado, Pajares, Benito, Jimenez-Villegas, Escoll et al., Can Activation of NRF2 Be a Strategy against COVID-19?, Trends Pharmacol. Sci, doi:10.1016/j.tips.2020.07.003
Cullinan, Zhang, Hannink, Arvisais, Kaufman et al., Nrf2 is a direct PERK substrate and effector of PERK-dependent cell survival, Mol. Cell. Biol, doi:10.1128/MCB.23.20.7198-7209.2003
Cummins, Weaver, May, Croatt, Foreman et al., Heme oxygenase-1 regulates the immune response to influenza virus infection and vaccination in aged mice, FASEB J, doi:10.1096/fj.11-190017
Dai, Gu, Su, Wang, Zhao et al., Inhibition of curcumin on influenza A virus infection and influenzal pneumonia via oxidative stress, TLR2/4, p38/JNK MAPK and NF-kappaB pathways, Int. Immunopharmacol, doi:10.1016/j.intimp.2017.11.009
De Angelis, Amatore, Checconi, Zevini, Fraternale et al., Influenza Virus Down-Modulates G6PD Expression and Activity to Induce Oxidative Stress and Promote Its Replication, Front. Cell Infect. Microbiol, doi:10.3389/fcimb.2021.804976
Denison, Seeking membranes: Positive-strand RNA virus replication complexes, PLoS Biol, doi:10.1371/journal.pbio.0060270
Digaleh, Kiaei, Khodagholi, Nrf2 and Nrf1 signaling and ER stress crosstalk: Implication for proteasomal degradation and autophagy, Cell. Mol. Life Sci, doi:10.1007/s00018-013-1409-y
Ding, Zhang, Li, Zhong, Tang et al., The Matrix Protein of Human Parainfluenza Virus Type 3 Induces Mitophagy that Suppresses Interferon Responses, Cell Host Microbe, doi:10.1016/j.chom.2017.03.004
Ding, Zhang, Yang, Zhang, Chen et al., Phosphoprotein of human parainfluenza virus type 3 blocks autophagosome-lysosome fusion to increase virus production, Cell Host Microbe, doi:10.1016/j.chom.2014.04.004
Dixon, Lemberg, Lamprecht, Skouta, Zaitsev et al., Ferroptosis: An iron-dependent form of nonapoptotic cell death, Cell, doi:10.1016/j.cell.2012.03.042
Edeas, Saleh, Peyssonnaux, Iron: Innocent bystander or vicious culprit in COVID-19 pathogenesis?, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.05.110
Edwards, Johnson, Mire, Xu, Shabman et al., The Marburg virus VP24 protein interacts with Keap1 to activate the cytoprotective antioxidant response pathway, Cell Rep, doi:10.1016/j.celrep.2014.01.043
Eggler, Liu, Pezzuto, Van Breemen, Mesecar, Modifying specific cysteines of the electrophile-sensing human Keap1 protein is insufficient to disrupt binding to the Nrf2 domain Neh2, Proc. Natl. Acad. Sci, doi:10.1073/pnas.0502402102
Elsby, Kitteringham, Goldring, Lovatt, Chamberlain et al., Increased constitutive c-Jun N-terminal kinase signaling in mice lacking glutathione S-transferase Pi, J. Biol. Chem, doi:10.1074/jbc.M301211200
Emanuele, Celesia, D'anneo, Lauricella, Carlisi et al., The Good and Bad of Nrf2: An Update in Cancer and New Perspectives in COVID-19, Int. J. Mol. Sci, doi:10.3390/ijms22157963
Espinoza, Gonzalez, Kalergis, Modulation of Antiviral Immunity by Heme Oxygenase-1, Am. J. Pathol, doi:10.1016/j.ajpath.2016.11.011
Espinoza, Leon, Cespedes, Gomez, Canedo-Marroquin et al., Heme Oxygenase-1 Modulates Human Respiratory Syncytial Virus Replication and Lung Pathogenesis during Infection, J. Immunol, doi:10.4049/jimmunol.1601414
Everett, Mcfadden, Apoptosis: An innate immune response to virus infection, Trends Microbiol, doi:10.1016/S0966-842X(99)01487-0
Fillebeen, Rivas-Estilla, Bisaillon, Ponka, Muckenthaler et al., Iron inactivates the RNA polymerase NS5B and suppresses subgenomic replication of hepatitis C Virus, J. Biol. Chem, doi:10.1074/jbc.M412687200
Gain, Song, Angtuaco, Satta, Kelesidis, The role of oxidative stress in the pathogenesis of infections with coronaviruses, Front. Microbiol, doi:10.3389/fmicb.2022.1111930
Galluzzi, Vitale, Aaronson, Abrams, Adam et al., Molecular mechanisms of cell death: Recommendations of the Nomenclature Committee on Cell Death 2018, Cell Death Differ, doi:10.1038/s41418-017-0012-4
Gao, Yan, Huang, Liu, Zhao et al., Structure of the RNA-dependent RNA polymerase from COVID-19 virus, Science, doi:10.1126/science.abb7498
Ghosh, Shcherbik, Effects of Oxidative Stress on Protein Translation: Implications for Cardiovascular Diseases, Int. J. Mol. Sci, doi:10.3390/ijms21082661
Gjyshi, Bottero, Veettil, Dutta, Singh et al., Kaposi's sarcoma-associated herpesvirus induces Nrf2 during de novo infection of endothelial cells to create a microenvironment conducive to infection, PLoS Pathog, doi:10.1371/journal.ppat.1004460
Gjyshi, Flaherty, Veettil, Johnson, Chandran et al., Kaposi's sarcoma-associated herpesvirus induces Nrf2 activation in latently infected endothelial cells through SQSTM1 phosphorylation and interaction with polyubiquitinated Keap1, J. Virol, doi:10.1128/JVI.02742-14
Gjyshi, Roy, Dutta, Veettil, Dutta et al., Activated Nrf2 Interacts with Kaposi's Sarcoma-Associated Herpesvirus Latency Protein LANA-1 and Host Protein KAP1 To Mediate Global Lytic Gene Repression, J. Virol, doi:10.1128/JVI.00895-15
Guo, Zhou, Jiang, Cuconati, Xiao et al., Regulation of hepatitis B virus replication by the phosphatidylinositol 3-kinase-akt signal transduction pathway, J. Virol, doi:10.1128/JVI.00541-07
Hamad, Al-Kuraishy, Alexiou, Papadakis, Ahmed et al., SARS-CoV-2 infection and dysregulation of nuclear factor erythroid-2-related factor 2 (Nrf2) pathway. Cell Stress, Chaperones, doi:10.1007/s12192-023-01379-0
Han, Lu, Yin, Fu, Zhang et al., Activation of NRF2 blocks HIV replication and apoptosis in macrophages, Heliyon, doi:10.1016/j.heliyon.2022.e12575
He, Ru, Wen, NRF2, a Transcription Factor for Stress Response and Beyond, Int. J. Mol. Sci, doi:10.3390/ijms21134777
Herengt, Thyrsted, Holm, NRF2 in Viral Infection, Antioxidants, doi:10.3390/antiox10091491
Hosakote, Liu, Castro, Garofalo, Casola, Respiratory syncytial virus induces oxidative stress by modulating antioxidant enzymes, Am. J. Respir. Cell Mol. Biol, doi:10.1165/rcmb.2008-0330OC
Houghton, Fassett, Coombes, Sulforaphane and Other Nutrigenomic Nrf2 Activators: Can the Clinician's Expectation Be Matched by the Reality? Oxid, Med. Cell. Longev, doi:10.1155/2016/7857186
Hu, Zhang, Doo, Coux, Goldberg et al., Hepatitis B virus X protein is both a substrate and a potential inhibitor of the proteasome complex, J. Virol, doi:10.1128/JVI.73.9.7231-7240.1999
Hua, Chang, Tseng, Chu, Liu et al., Functional haplotypes in the promoter region of transcription factor Nrf2 in chronic obstructive pulmonary disease, Dis. Markers, doi:10.1155/2010/143142
Huang, Feng, Shi, Li, Wang et al., Protein Kinase C Inhibitors Reduce SARS-CoV-2 Replication in Cultured Cells, Microbiol. Spectr, doi:10.1128/spectrum.01056-22
Ilback, Frisk, Mohamed, Gadhasson, Blomberg et al., Virus induces metal-binding proteins and changed trace element balance in the brain during the course of a common human infection (coxsackievirus B3) in mice, Sci. Total Env, doi:10.1016/j.scitotenv.2007.03.025
Iso, Suzuki, Baird, Yamamoto, Absolute Amounts and Status of the Nrf2-Keap1-Cul3 Complex within Cells, Mol. Cell. Biol, doi:10.1128/MCB.00389-16
Ivanciuc, Sbrana, Casola, Garofalo, Protective Role of Nuclear Factor Erythroid 2-Related Factor 2 Against Respiratory Syncytial Virus and Human Metapneumovirus Infections, Front. Immunol, doi:10.3389/fimmu.2018.00854
Ivanov, Smirnova, Ivanova, Masalova, Kochetkov et al., Hepatitis C virus proteins activate NRF2/ARE pathway by distinct ROS-dependent and independent mechanisms in HUH7 cells, PLoS ONE, doi:10.1371/journal.pone.0024957
Jancova, Anzenbacher, Anzenbacherova, Phase II drug metabolizing enzymes, Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc Czech Repub, doi:10.5507/bp.2010.017
Jiang, Harder, Rojo De La Vega, Wong, Chapman et al., p62 links autophagy and Nrf2 signaling, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2015.06.014
Ju, Yan, Liu, Li, Sheng et al., Neuraminidase of Influenza A Virus Binds Lysosome-Associated Membrane Proteins Directly and Induces Lysosome Rupture, J. Virol, doi:10.1128/JVI.01411-15
Kesic, Simmons, Bauer, Jaspers, Nrf2 expression modifies influenza A entry and replication in nasal epithelial cells, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2011.04.027
Khan, Patel, Majumdar, Role of NRF2 and Sirtuin activators in COVID-19, Clin. Immunol, doi:10.1016/j.clim.2021.108879
Khomich, Kochetkov, Bartosch, Ivanov, Redox Biology of Respiratory Viral Infections, Viruses, doi:10.3390/v10080392
Kim, Seong, Shin, Enhanced Viral Replication by Cellular Replicative Senescence, Immune Netw, doi:10.4110/in.2016.16.5.286
Kobayashi, Suzuki, Funayama, Nagashima, Hayashi et al., Nrf2 suppresses macrophage inflammatory response by blocking proinflammatory cytokine transcription, Nat. Commun, doi:10.1038/ncomms11624
Komaravelli, Ansar, Garofalo, Casola, Respiratory syncytial virus induces NRF2 degradation through a promyelocytic leukemia protein-Ring finger protein 4 dependent pathway, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2017.10.380
Komaravelli, Tian, Ivanciuc, Mautemps, Brasier et al., Respiratory syncytial virus infection down-regulates antioxidant enzyme expression by triggering deacetylation-proteasomal degradation of Nrf2, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2015.05.043
Komatsu, Kurokawa, Waguri, Taguchi, Kobayashi et al., The selective autophagy substrate p62 activates the stress responsive transcription factor Nrf2 through inactivation of Keap1, Nat. Cell Biol, doi:10.1038/ncb2021
Kosmider, Messier, Janssen, Nahreini, Wang et al., Nrf2 protects human alveolar epithelial cells against injury induced by influenza A virus, Respir. Res, doi:10.1186/1465-9921-13-43
Kovac, Angelova, Holmstrom, Zhang, Dinkova-Kostova et al., Nrf2 regulates ROS production by mitochondria and NADPH oxidase, Biochim. Biophys. Acta, doi:10.1016/j.bbagen.2014.11.021
Koyuncu, Budayeva, Miteva, Ricci, Silhavy et al., Sirtuins are evolutionarily conserved viral restriction factors, mBio, doi:10.1128/mBio.02249-14
Krammer, Smith, Fouchier, Peiris, Kedzierska et al., None, Nat. Rev. Dis. Prim, doi:10.1038/s41572-018-0002-y
Kumar, Nayak, Sahoo, Pandey, Sarkar et al., Iron oxide nanoparticles based antiviral activity of H1N1 influenza A virus, J. Infect. Chemother, doi:10.1016/j.jiac.2018.12.006
Kurokawa, Motohashi, Sueno, Kimura, Takagawa et al., Structural basis of alternative DNA recognition by Maf transcription factors, Mol. Cell. Biol, doi:10.1128/MCB.00708-09
Kwon, Brent, Getachew, Jayakumar, Chen et al., Human immunodeficiency virus type 1 Tat protein inhibits the SIRT1 deacetylase and induces T cell hyperactivation, Cell Host Microbe, doi:10.1016/j.chom.2008.02.002
Lane, Metselaar, Greenough, Bush, Ayton, Ferroptosis and NRF2: An emerging battlefield in the neurodegeneration of Alzheimer's disease, Essays Biochem, doi:10.1042/EBC20210017
Lau, Villeneuve, Sun, Wong, Zhang, Dual roles of Nrf2 in cancer, Pharmacol. Res, doi:10.1016/j.phrs.2008.09.003
Lee, Han, Lee, Lee, Park et al., Hydrogen peroxide attenuates rhinovirus-induced anti-viral interferon secretion in sinonasal epithelial cells, Front. Immunol, doi:10.3389/fimmu.2023.1086381
Lee, Hur, Ryoo, Jung, Kwak et al., Involvement of the Nrf2-proteasome pathway in the endoplasmic reticulum stress response in pancreatic beta-cells, Toxicol. Appl. Pharmacol, doi:10.1016/j.taap.2012.08.021
Lee, Jang, Park, Yang, An Update on the Role of Nrf2 in Respiratory Disease: Molecular Mechanisms and Therapeutic Approaches, Int. J. Mol. Sci, doi:10.3390/ijms22168406
Lee, Koh, Kim, Ahn, Kim, Upregulation of Nrf2 expression by human cytomegalovirus infection protects host cells from oxidative stress, J. Gen. Virol, doi:10.1099/vir.0.052142-0
Li, He, Zhou, Ye, Gao, Activation of Kaposi's sarcoma-associated herpesvirus (KSHV) by inhibitors of class III histone deacetylases: Identification of sirtuin 1 as a regulator of the KSHV life cycle, J. Virol, doi:10.1128/JVI.00219-14
Li, Li, Zeng, Yang, Liu et al., Respiratory Syncytial Virus Replication Is Promoted by Autophagy-Mediated Inhibition of Apoptosis, J. Virol, doi:10.1128/JVI.02193-17
Li, Xia, Liu, Meng, Wu et al., SIRT1 inhibits rheumatoid arthritis fibroblast-like synoviocyte aggressiveness and inflammatory response via suppressing NF-kappaB pathway, Biosci. Rep, doi:10.1042/BSR20180541
Lin, Chu, Chiu, Lactoferrin inhibits enterovirus 71 infection of human embryonal rhabdomyosarcoma cells in vitro, J. Infect. Dis, doi:10.1086/343809
Lin, Hsia, Huang, Wu, Chang, Proinflammatory cytokine reactions in enterovirus 71 infections of the central nervous system, Clin. Infect. Dis, doi:10.1086/345905
Liu, Castro, Brasier, Jamaluddin, Garofalo et al., Reactive oxygen species mediate virus-induced STAT activation: Role of tyrosine phosphatases, J. Biol. Chem, doi:10.1074/jbc.M307251200
Liu, Chen, Liu, Chen, Liu et al., The role of oxidative stress in influenza virus infection, Microbes Infect, doi:10.1016/j.micinf.2017.08.008
Liu, Du, Yang, Zheng, Shen et al., SARS-CoV-2 ORF3a sensitizes cells to ferroptosis via Keap1-NRF2 axis, Redox Biol, doi:10.1016/j.redox.2023.102752
Liu, Fang, He, Cui, Jia et al., Hepatitis B virus stimulates G6PD expression through HBx-mediated Nrf2 activation, Cell Death Dis, doi:10.1038/cddis.2015.322
Liu, Gao, Ci, Role of Nrf2 and Its Activators in Respiratory Diseases, Oxid. Med. Cell. Longev, doi:10.1155/2019/7090534
Liu, Huang, Liu, Meng, Gu et al., Nrf2 and its dependent autophagy activation cooperatively counteract ferroptosis to alleviate acute liver injury, Pharmacol. Res
Luo, Zhu, Mao, Du, T cell immunobiology and cytokine storm of COVID-19, Scand. J. Immunol, doi:10.1111/sji.12989
Ma, Tuersun, Jiao, Zheng, Xiao et al., Functional Role of NRF2 in Cervical Carcinogenesis, PLoS ONE, doi:10.1371/journal.pone.0133876
Ma, Wang, Wu, Hu, Yin et al., Rupestonic acid derivative YZH-106 suppresses influenza virus replication by activation of heme oxygenase-1-mediated interferon response, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2016.04.021
Macleod, Mcmahon, Plummer, Higgins, Penning et al., Characterization of the cancer chemopreventive NRF2-dependent gene battery in human keratinocytes: Demonstration that the KEAP1-NRF2 pathway, and not the BACH1-NRF2 pathway, controls cytoprotection against electrophiles as well as redox-cycling compounds, Carcinogenesis, doi:10.1093/carcin/bgp176
Mangla, Javed, Sultan, Kumar, Kohli et al., A review of its therapeutic potentials, advances in its nanodelivery, recent patents, and clinical trials, Phytother. Res, doi:10.1002/ptr.7176
Marsh, Pelchen-Matthews, Endocytosis in viral replication, Traffic, doi:10.1034/j.1600-0854.2000.010701.x
Mastrantonio, Cervelli, Pietropaoli, Mariottini, Colasanti et al., HIV-Tat Induces the Nrf2/ARE Pathway through NMDA Receptor-Elicited Spermine Oxidase Activation in Human Neuroblastoma Cells, PLoS ONE, doi:10.1371/journal.pone.0149802
Mcauley, Tate, Mackenzie-Kludas, Pinar, Zeng et al., Activation of the NLRP3 inflammasome by IAV virulence protein PB1-F2 contributes to severe pathophysiology and disease, PLoS Pathog, doi:10.1371/journal.ppat.1003392
Mcphee, Caldera, Bemis, Mcdonagh, Kuntz et al., Bile pigments as HIV-1 protease inhibitors and their effects on HIV-1 viral maturation and infectivity in vitro, Biochem. J, doi:10.1042/bj3200681
Mihaylova, Kong, Fedorova, Sharma, Dela Cruz et al., Regional Differences in Airway Epithelial Cells Reveal Tradeoff between Defense against Oxidative Stress and Defense against Rhinovirus, Cell Rep, doi:10.1016/j.celrep.2018.08.033
Mills, Ryan, Prag, Dikovskaya, Menon et al., Itaconate is an anti-inflammatory metabolite that activates Nrf2 via alkylation of KEAP1, Nature, doi:10.1038/nature25986
Mohiuddin, Kasahara, The emerging role of oxidative stress in complications of COVID-19 and potential therapeutic approach to diminish oxidative stress, Respir. Med, doi:10.1016/j.rmed.2021.106605
Mondal, Dawson, Potts, Freiberger, Baker et al., Influenza virus recruits host protein kinase C to control assembly and activity of its replication machinery, eLife, doi:10.7554/eLife.26910
Moreno-Solis, Dela Torre-Aguilar, Torres-Borrego, Llorente-Cantarero, Fernandez-Gutierrez et al., Oxidative stress and inflamatory plasma biomarkers in respiratory syncytial virus bronchiolitis, Clin. Respir. J, doi:10.1111/crj.12425
Nencioni, Iuvara, Aquilano, Ciriolo, Cozzolino et al., Influenza A virus replication is dependent on an antioxidant pathway that involves GSH and Bcl-2, FASEB J, doi:10.1096/fj.02-0508fje
Newton, Cardani, Braciale, The host immune response in respiratory virus infection: Balancing virus clearance and immunopathology, Semin. Immunopathol, doi:10.1007/s00281-016-0558-0
Niture, Jaiswal, Nrf2 protein up-regulates antiapoptotic protein Bcl-2 and prevents cellular apoptosis, J. Biol. Chem, doi:10.1074/jbc.M111.312694
Noah, Zhang, Zhou, Glista-Baker, Muller et al., Effect of broccoli sprouts on nasal response to live attenuated influenza virus in smokers: A randomized, double-blind study, PLoS ONE, doi:10.1371/journal.pone.0098671
O'donnell, Pacheco, Larocco, Burrage, Jackson et al., Foot-and-mouth disease virus utilizes an autophagic pathway during viral replication, Virology, doi:10.1016/j.virol.2010.10.042
Olagnier, Brandtoft, Gunderstofte, Villadsen, Krapp et al., Nrf2 negatively regulates STING indicating a link between antiviral sensing and metabolic reprogramming, Nat. Commun, doi:10.1038/s41467-018-05861-7
Olagnier, Farahani, Thyrsted, Blay-Cadanet, Herengt et al., SARS-CoV2-mediated suppression of NRF2-signaling reveals potent antiviral and anti-inflammatory activity of 4-octyl-itaconate and dimethyl fumarate, Nat. Commun, doi:10.1038/s41467-020-18764-3
Ordonez, Bullen, Villabona-Rueda, Thompson, Turner et al., Sulforaphane exhibits antiviral activity against pandemic SARS-CoV-2 and seasonal HCoV-OC43 coronaviruses in vitro and in mice, Commun. Biol, doi:10.1038/s42003-022-03189-z
Pagans, Pedal, North, Kaehlcke, Marshall et al., SIRT1 regulates HIV transcription via Tat deacetylation, PLoS Biol, doi:10.1371/journal.pbio.0030041
Page, Volchkova, Reid, Mateo, Bagnaud-Baule et al., Marburgvirus hijacks nrf2-dependent pathway by targeting nrf2-negative regulator keap1, Cell Rep, doi:10.1016/j.celrep.2014.02.027
Pensabene, Lamorte, Allender, Wehr, Kaur et al., Acute Oxidative Stress Can Paradoxically Suppress Human NRF2 Protein Synthesis by Inhibiting Global Protein Translation, Antioxidants, doi:10.3390/antiox12091735
Pokharel, Shil, Bose, Autophagy, TGF-beta, and SMAD-2/3 Signaling Regulates Interferon-beta Response in Respiratory Syncytial Virus Infected Macrophages, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2016.00174
Polonikov, Endogenous Deficiency of Glutathione as the Most Likely Cause of Serious Manifestations and Death in COVID-19 Patients, ACS Infect. Dis, doi:10.1021/acsinfecdis.0c00288
Prentice, Jerome, Yoshimori, Mizushima, Denison, Coronavirus replication complex formation utilizes components of cellular autophagy, J. Biol. Chem, doi:10.1074/jbc.M306124200
Qu, Haas De Mello, Morris, Jones-Hall, Ivanciuc et al., SARS-CoV-2 Inhibits NRF2-Mediated Antioxidant Responses in Airway Epithelial Cells and in the Lung of a Murine Model of Infection, Microbiol. Spectr, doi:10.1128/spectrum.00378-23
Rada, Rojo, Chowdhry, Mcmahon, Hayes et al., SCF/beta-TrCP promotes glycogen synthase kinase 3-dependent degradation of the Nrf2 transcription factor in a Keap1-independent manner, Mol. Cell. Biol, doi:10.1128/MCB.01204-10
Ramezani, Nahad, Faghihloo, The role of Nrf2 transcription factor in viral infection, J. Cell. Biochem, doi:10.1002/jcb.26897
Rashid, Gao, Coombs, Influenza A Virus Uses PSMA2 for Downregulation of the NRF2-Mediated Oxidative Stress Response, J. Virol, doi:10.1128/jvi.01990-21
Reed, Brewah, Delaney, Welliver, Burwell et al., Macrophage impairment underlies airway occlusion in primary respiratory syncytial virus bronchiolitis, J. Infect. Dis, doi:10.1086/593173
Reggiori, Monastyrska, Verheije, Cali, Ulasli et al., Coronaviruses Hijack the LC3-I-positive EDEMosomes, ER-derived vesicles exporting short-lived ERAD regulators, for replication, Cell Host Microbe, doi:10.1016/j.chom.2010.05.013
Ren, Lv, Zhuo, Chen, Shi et al., Suppression of IRG-1 Reduces Inflammatory Cell Infiltration and Lung Injury in Respiratory Syncytial Virus Infection by Reducing Production of Reactive Oxygen Species, J. Virol, doi:10.1128/JVI.00563-16
Robinson, Tsueng, Sin, Mangale, Rahawi et al., Coxsackievirus B exits the host cell in shed microvesicles displaying autophagosomal markers, PLoS Pathog, doi:10.1371/journal.ppat.1004045
Rossi, Sacco, Capizzi, Mastromarino, Can Resveratrol-Inhaled Formulations Be Considered Potential Adjunct Treatments for COVID-19?, Front. Immunol, doi:10.3389/fimmu.2021.670955
Roulston, Marcellus, Branton, Viruses and apoptosis, Annu. Rev. Microbiol, doi:10.1146/annurev.micro.53.1.577
Rushworth, Macewan, HO-1 underlies resistance of AML cells to TNF-induced apoptosis, Blood, doi:10.1182/blood-2007-07-104042
Salimi, Ramezani, Mirzaei, Tahamtan, Faghihloo et al., Evaluation of the expression level of 12/15 lipoxygenase and the related inflammatory factors (CCL5, CCL3) in respiratory syncytial virus infection in mice model, Microb. Pathog, doi:10.1016/j.micpath.2017.05.045
San-Juan-Vergara, Peeples, Lockey, Mohapatra, Protein kinase C-alpha activity is required for respiratory syncytial virus fusion to human bronchial epithelial cells, J. Virol, doi:10.1128/JVI.78.24.13717-13726.2004
Santangelo, Mancuso, Marchetti, Di Stasio, Pani et al., An Endogenous Molecule with Antiviral Activity in vitro, Front. Pharmacol, doi:10.3389/fphar.2012.00036
Schneider, Nobs, Heer, Kurrer, Klinke et al., Alveolar macrophages are essential for protection from respiratory failure and associated morbidity following influenza virus infection, PLoS Pathog, doi:10.1371/journal.ppat.1004053
Segovia, Sabbah, Mgbemena, Tsai, Chang et al., TLR2/MyD88/NF-kappaB pathway, reactive oxygen species, potassium efflux activates NLRP3/ASC inflammasome during respiratory syncytial virus infection, PLoS ONE, doi:10.1371/journal.pone.0029695
Selvakumar, Ahmed, Raikwar, Thangavel, Kempuraj et al., CRISPR/Cas9 Editing of Glia Maturation Factor Regulates Mitochondrial Dynamics by Attenuation of the NRF2/HO-1 Dependent Ferritin Activation in Glial Cells, J. Neuroimmune Pharmacol, doi:10.1007/s11481-019-09833-6
Sena, Chandel, Physiological roles of mitochondrial reactive oxygen species, Mol. Cell, doi:10.1016/j.molcel.2012.09.025
Shen, Shenk, Viruses and apoptosis, Curr. Opin. Genet. Dev, doi:10.1016/S0959-437X(95)90061-6
Shi, Arnott, Semogas, Falsey, Openshaw et al., The Etiological Role of Common Respiratory Viruses in Acute Respiratory Infections in Older Adults: A Systematic Review and Meta-analysis, J. Infect. Dis, doi:10.1093/infdis/jiy662
Shi, Wong, Piesik, Fung, Zhang et al., Cleavage of sequestosome 1/p62 by an enteroviral protease results in disrupted selective autophagy and impaired NFKB signaling, Autophagy, doi:10.4161/auto.26059
Shoji, Arakaki, Esumi, Kohnomi, Yamamoto et al., Bakuchiol Is a Phenolic Isoprenoid with Novel Enantiomer-selective Anti-influenza A Virus Activity Involving Nrf2 Activation, J. Biol. Chem, doi:10.1074/jbc.M115.669465
Singh, Ahmad, Baid, Kumar, Host heme oxygenase-1: Friend or foe in tackling pathogens?, IUBMB Life, doi:10.1002/iub.1868
Singh, Chhabra, Ndiaye, Garcia-Peterson, Mack et al., The Role of Sirtuins in Antioxidant and Redox Signaling, Antioxid. Redox Signal, doi:10.1089/ars.2017.7290
Singh, Wasan, Reeta, Heme oxygenase-1 modulation: A potential therapeutic target for COVID-19 and associated complications, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2020.10.016
Sir, Ou, Autophagy in viral replication and pathogenesis, Mol. Cells, doi:10.1007/s10059-010-0014-2
Smirnova, Ivanova, Mukhtarov, Tunitskaya, Jansons et al., Analysis of the Domains of Hepatitis C Virus Core and NS5A Proteins that Activate the Nrf2/ARE Cascade, Acta Nat, doi:10.32607/20758251-2016-8-3-123-127
Song, Long, Nrf2 and Ferroptosis: A New Research Direction for Neurodegenerative Diseases, Front. Neurosci, doi:10.3389/fnins.2020.00267
Staitieh, Ding, Neveu, Spearman, Guidot et al., HIV-1 decreases Nrf2/ARE activity and phagocytic function in alveolar macrophages, J. Leukoc. Biol, doi:10.1189/jlb.4A0616-282RR
Staring, Von Castelmur, Blomen, Van Den Hengel, Brockmann et al., PLA2G16 represents a switch between entry and clearance of Picornaviridae, Nature, doi:10.1038/nature21032
Sun, Hoshino, Takaku, Nakajima, Muto et al., Hemoprotein Bach1 regulates enhancer availability of heme oxygenase-1 gene, EMBO J, doi:10.1093/emboj/cdf516
Tan, Lim, Liu, Ong, Tan et al., Respiratory Viral Infections in Exacerbation of Chronic Airway Inflammatory Diseases: Novel Mechanisms and Insights From the Upper Airway Epithelium, Front. Cell Dev. Biol, doi:10.3389/fcell.2020.00099
Thomson, Viruses and apoptosis, Int. J. Exp. Pathol, doi:10.1111/j.1365-2613.2001.iep195.x
Tomiotto-Pellissier, Alves, Miranda-Sapla, De Morais, Assolini et al., Caryocar coriaceum extracts exert leishmanicidal effect acting in promastigote forms by apoptosis-like mechanism and intracellular amastigotes by Nrf2/HO-1/ferritin dependent response and iron depletion: Leishmanicidal effect of Caryocar coriaceum leaf exracts, Biomed. Pharmacother, doi:10.1016/j.biopha.2017.12.083
Triantafilou, Kar, Vakakis, Kotecha, Triantafilou, Human respiratory syncytial virus viroporin SH: A viral recognition pathway used by the host to signal inflammasome activation, Thorax, doi:10.1136/thoraxjnl-2012-202182
Triantafilou, Kar, Van Kuppeveld, Triantafilou, Rhinovirus-induced calcium flux triggers NLRP3 and NLRC5 activation in bronchial cells, Am. J. Respir. Cell Mol. Biol, doi:10.1165/rcmb.2013-0032OC
Tseng, Hsu, Lin, Wu, Lee et al., Celastrol inhibits hepatitis C virus replication by upregulating heme oxygenase-1 via the JNK MAPK/Nrf2 pathway in human hepatoma cells, Antivir. Res, doi:10.1016/j.antiviral.2017.09.010
Tung, Hsieh, Lee, Yang, Enterovirus 71 induces integrin beta1/EGFR-Rac1-dependent oxidative stress in SK-N-SH cells: Role of HO-1/CO in viral replication, J. Cell. Physiol, doi:10.1002/jcp.22677
Vale-Costa, Amorim, Recycling Endosomes and Viral Infection, Viruses, doi:10.3390/v8030064
Volk, Moreland, ROS-containing endosomal compartments: Implications for signaling, Methods Enzym, doi:10.1016/B978-0-12-397925-4.00013-4
Vomund, Schafer, Parnham, Brune, Von Knethen, Nrf2, the Master Regulator of Anti-Oxidative Responses, Int. J. Mol. Sci, doi:10.3390/ijms18122772
Walsh, Mohr, Viral subversion of the host protein synthesis machinery, Nat. Rev. Microbiol, doi:10.1038/nrmicro2655
Wang, Joshua, Jin, Du, Li, Ferroptosis in viral infection: The unexplored possibility, Acta Pharmacol. Sin, doi:10.1038/s41401-021-00814-1
Wang, Li, Li, Miao, Xiao, The Effects of Resveratrol on Inflammation and Oxidative Stress in a Rat Model of Chronic Obstructive Pulmonary Disease, Molecules, doi:10.3390/molecules22091529
Wang, Li, Niu, Xu, Ma et al., Antiviral effects of ferric ammonium citrate, Cell Discov, doi:10.1038/s41421-018-0013-6
Wang, Zhang, Han, Guo, Zhong et al., Hemin ameliorates influenza pneumonia by attenuating lung injury and regulating the immune response, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2016.09.030
Wong, Zhang, Si, Gao, Mao et al., Autophagosome supports coxsackievirus B3 replication in host cells, J. Virol, doi:10.1128/JVI.00641-08
Wu, Lu, Bai, Nrf2 in cancers: A double-edged sword, Cancer Med, doi:10.1002/cam4.2101
Wu, Van Dyk, Jiang, Dakhama, Li et al., Interleukin-1 receptor-associated kinase M (IRAK-M) promotes human rhinovirus infection in lung epithelial cells via the autophagic pathway, Virology, doi:10.1016/j.virol.2013.08.005
Wu, Zhang, Yuan, Ma, Li et al., Progress of cGAS-STING signaling in response to SARS-CoV-2 infection, Front. Immunol, doi:10.3389/fimmu.2022.1010911
Yageta, Ishii, Morishima, Ano, Ohtsuka et al., Carbocisteine reduces virus-induced pulmonary inflammation in mice exposed to cigarette smoke, Am. J. Respir. Cell Mol. Biol, doi:10.1165/rcmb.2012-0292OC
Yageta, Ishii, Morishima, Masuko, Ano et al., Role of Nrf2 in host defense against influenza virus in cigarette smoke-exposed mice, J. Virol, doi:10.1128/JVI.02456-10
Yamada, Limmon, Zheng, Li, Li et al., Major shifts in the spatio-temporal distribution of lung antioxidant enzymes during influenza pneumonia, PLoS ONE, doi:10.1371/journal.pone.0031494
Yang, Park, Chang, Shapiro, Vassilopoulos et al., Sirtuin 2 regulates cellular iron homeostasis via deacetylation of transcription factor NRF2, J. Clin. Investig, doi:10.1172/JCI88574
Yin, Mcbride, Fewell, Lacey, Wang et al., MicroRNA-155 is an Epstein-Barr virus-induced gene that modulates Epstein-Barr virus-regulated gene expression pathways, J. Virol, doi:10.1128/JVI.02380-07
Yu, Chen, Tseng, Lin, Hsu et al., Sulforaphane Suppresses Hepatitis C Virus Replication by Up-Regulating Heme Oxygenase-1 Expression through PI3K/Nrf2 Pathway, PLoS ONE, doi:10.1371/journal.pone.0152236
Yue, Nabar, Shi, Kamenyeva, Xiao et al., SARS-Coronavirus Open Reading Frame-3a drives multimodal necrotic cell death, Cell Death Dis, doi:10.1038/s41419-018-0917-y
Zhang, An, Gao, Leak, Chen et al., Emerging roles of Nrf2 and phase II antioxidant enzymes in neuroprotection, Prog. Neurobiol, doi:10.1016/j.pneurobio.2012.09.003
Zhang, Wang, Wang, Aliyari, Cheng, SARS-CoV-2 virus NSP14 Impairs NRF2/HMOX1 activation by targeting Sirtuin 1, Cell Mol. Immunol, doi:10.1038/s41423-022-00887-w
Zhang, Zhang, Zang, Chen, Lu et al., Curcumin Inhibits Replication of Human Parainfluenza Virus Type 3 by Affecting Viral Inclusion Body Formation, Biomed. Res. Int, doi:10.1155/2021/1807293
Zhao, Ghosh, Lo, Chenier, Scholey et al., Nrf2 Deficiency Upregulates Intrarenal Angiotensin-Converting Enzyme-2 and Angiotensin 1-7 Receptor Expression and Attenuates Hypertension and Nephropathy in Diabetic Mice, Endocrinology, doi:10.1210/en.2017-00752
Zhao, Thackray, Miller, Lynn, Becker et al., Coronavirus replication does not require the autophagy gene ATG5, Autophagy, doi:10.4161/auto.4782
Zhou, Jiang, Liu, Fan, Hu et al., Autophagy is involved in influenza A virus replication, Autophagy, doi:10.4161/auto.5.3.7406
Zhou, Xue, He, Liu, Yin et al., Resveratrol delays postovulatory aging of mouse oocytes through activating mitophagy, Aging, doi:10.18632/aging.102551
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
Zhu, Mathahs, Schmidt, Restoration of type I interferon expression by heme and related tetrapyrroles through inhibition of NS3/4A protease, J. Infect. Dis, doi:10.1093/infdis/jit338