Immunoregulatory effects of nanocurcumin in inflammatory milieu: Focus on COVID-19
et al., Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2024.116131, Jan 2024
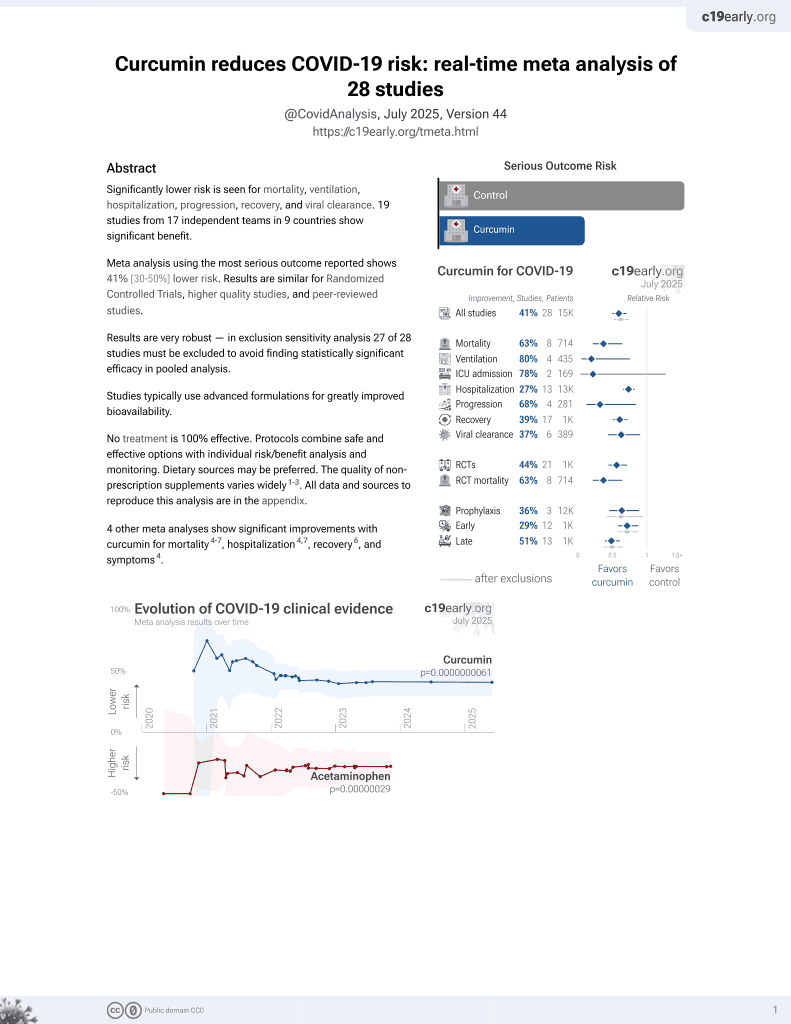
Curcumin for COVID-19
17th treatment shown to reduce risk in
February 2021, now with p = 0.0000000061 from 28 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
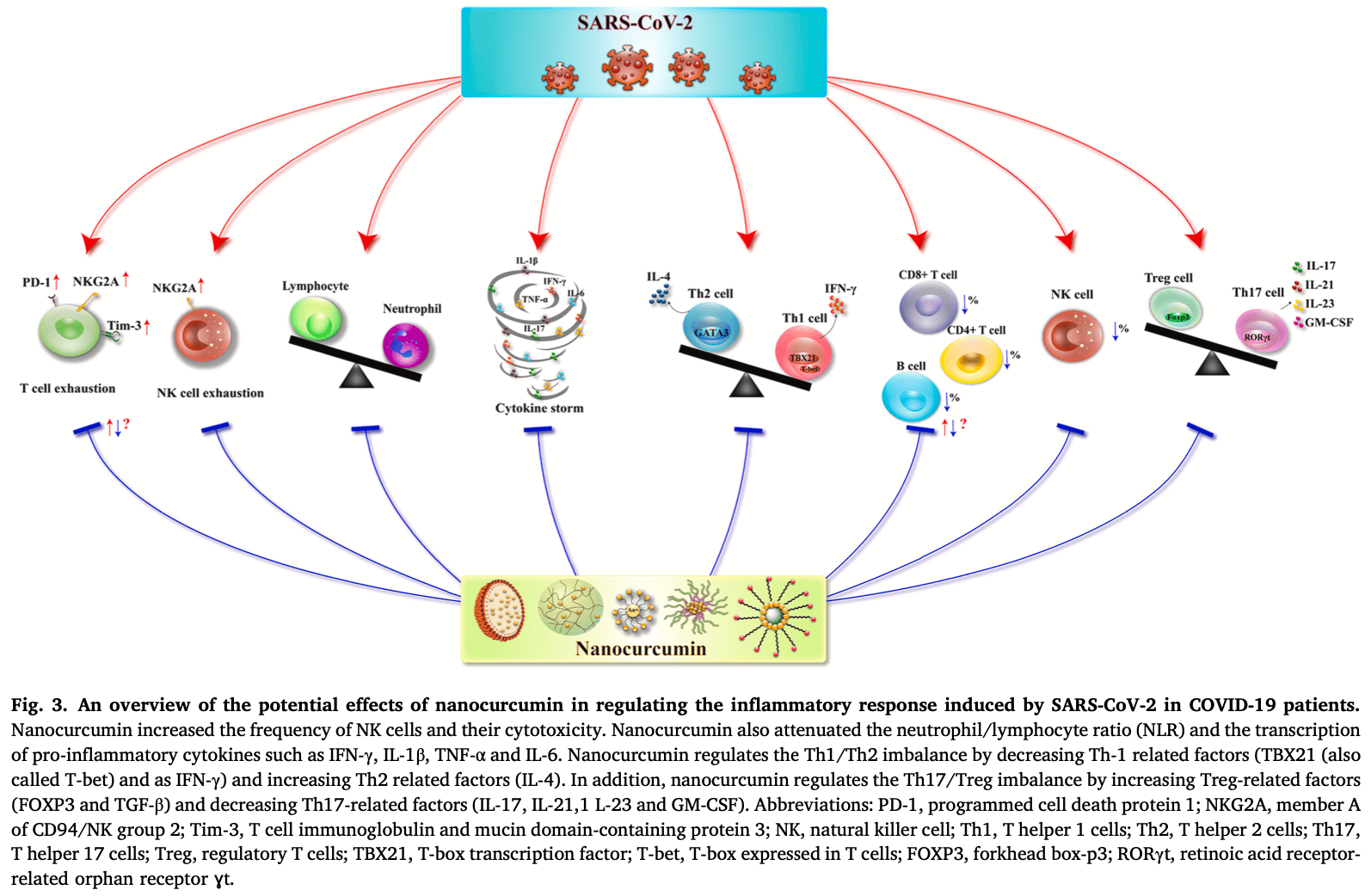
Review of immunoregulatory effects of nanocurcumin in inflammatory conditions including COVID-19. Authors note that curcumin has shown therapeutic potential but has poor bioavailability, which nanoformulations can address. Studies suggest nanocurcumin reduces expression and secretion of inflammatory cytokines like IL-6 and IL-1beta involved in COVID-19 cytokine storms, increases lymphocyte counts, and improves clinical symptoms. Potential mechanisms include regulating Th1/Th2 and Th17/Treg imbalances and reducing proinflammatory signaling.
1.
Shokri-Afra et al., Targeting SIRT1: A Potential Strategy for Combating Severe COVID‐19, BioMed Research International, doi:10.1155/bmri/9507417.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Duan et al., Bioactive compounds,quercetin, curcumin and β-glucan,regulate innate immunity via the gut-liver-brain axis, Trends in Food Science & Technology, doi:10.1016/j.tifs.2024.104864.
4.
Rajak et al., Antiallergic Implications of Curcumin During COVID-19: Current Status and Perspectives, Biotechnology of Medicinal Plants with Antiallergy Properties, doi:10.1007/978-981-97-1467-4_4.
5.
Kali et al., Curcumin as a Promising Therapy for COVID-19: A Review, Global Journal of Medical, Pharmaceutical, and Biomedical Update, doi:10.25259/GJMPBU_78_2023.
6.
Vajdi et al., Effect of polyphenols against complications of COVID-19: current evidence and potential efficacy, Pharmacological Reports, doi:10.1007/s43440-024-00585-6.
7.
Yong et al., Natural Products-Based Inhaled Formulations for Treating Pulmonary Diseases, International Journal of Nanomedicine, doi:10.2147/ijn.s451206.
8.
Halma et al., Exploring autophagy in treating SARS-CoV-2 spike protein-related pathology, Endocrine and Metabolic Science, doi:10.1016/j.endmts.2024.100163.
9.
Arab et al., Immunoregulatory effects of nanocurcumin in inflammatory milieu: Focus on COVID-19, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2024.116131.
10.
Daskou et al., The Role of the NRF2 Pathway in the Pathogenesis of Viral Respiratory Infections, Pathogens, doi:10.3390/pathogens13010039.
11.
Law et al., Photodynamic Action of Curcumin and Methylene Blue against Bacteria and SARS-CoV-2—A Review, Pharmaceuticals, doi:10.3390/ph17010034.
12.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
13.
Hulscher et al., Clinical Approach to Post-acute Sequelae After COVID-19 Infection and Vaccination, Cureus, doi:10.7759/cureus.49204.
14.
Hegde et al., Curcumin Formulations for Better Bioavailability: What We Learned from Clinical Trials Thus Far?, ACS Omega, doi:10.1021/acsomega.2c07326.
Arab et al., 9 Jan 2024, peer-reviewed, 6 authors.
Contact: laviaf@mums.ac.ir, mahmoudim1@mums.ac.ir.
Immunoregulatory effects of nanocurcumin in inflammatory milieu: Focus on COVID-19
Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2024.116131
The use of natural compounds, such as curcumin, to treat infections caused by bacteria, viruses, fungi, parasites, inflammatory diseases, and various types of cancer is an active and dynamic area of research. Curcumin has a long history of use in the food industry, and there is currently a growing interest in its therapeutic applications. Numerous clinical trials have consistently shown that curcumin, a polyphenolic compound, is safe and welltolerated even at high doses. There is no toxicity limit. However, the clinical efficacy of curcumin has been limited by its constraints. However, scientific evidence indicates that the use of adjuvants and carriers, such as nanoparticles, exosomes, micelles, and liposomes, can help overcome this limitation. The properties, functions, and human benefits of using nanocurcumin are well-supported by scientific research. Recent evidence suggests that nanocurcumin may be a beneficial therapeutic modality due to its potential to decrease gene expression and secretion of specific inflammatory biomarkers involved in the cytokinestorm seen in severe COVID-19, as well as increase lymphocyte counts. Nanocurcumin has demonstrated the ability to improve clinical manifestations and modulate immune response and inflammation in various autoinflammatory diseases. Additionally, its efficacy, affordability, and safety make it a promising replacement for residual cancer cells after tumor removal. However, further studies are necessary to evaluate the safety and efficacy of nanocurcumin as a new therapeutic in clinical trials, including appropriate dosage, frequency, and duration.
Authors' contributions Fahimeh Lavi Arab has drafted the work. Akram Hoseinzadeh, Fatemeh Sadat Mohammadi, Arezoo Rajabian, Arezoo Faridzadeh, and Mahmoud Mahmoudi, thoroughly reviewed it. Akram Hoseinzadeh has drawn the Fig. 1 . All authors read and approved the final manuscript.
CRediT authorship contribution statement Faridzadeh Arezoo: Writingoriginal draft. Lavi Arab Fahimeh: Writingreview & editing, Writingoriginal draft. Mohammadi Fatemeh Sadat: Writingreview & editing, Writingoriginal draft.
Declaration of Competing Interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
-F Li, T cell responses to whole SARS coronavirus in humans, J. Immunol
Abbasian, Nanocurcumin supplementation ameliorates Behcet's disease by modulating regulatory T cells: a randomized, double-blind, placebo-controlled trial, Int. Immunopharmacol
Abbaspour-Aghdam, Immunomodulatory role of Nanocurcumin in COVID-19 patients with dropped natural killer cells frequency and function, Eur. J. Pharm
Abbaspour-Aghdam, Immunomodulatory role of Nanocurcumin in COVID-19 patients with dropped natural killer cells frequency and function, Eur. J. Pharmacol
Abdel-Ghany, El-Sisy, Salem, A comparative study of effects of curcumin and its nanoparticles on the growth, immunity and heat stress resistance of Nile tilapia (Oreochromis niloticus), Sci. Rep
Abubakar, Haque, Preparation of medicinal plants: basic extraction and fractionation procedures for experimental purposes, J. Pharm. Bioallied Sci
Ahmad, A comparative study of PNIPAM nanoparticles of curcumin, demethoxycurcumin, and bisdemethoxycurcumin and their effects on oxidative stress markers in experimental stroke, Protoplasma
Ahmadi, Oral nano-curcumin formulation efficacy in the management of mild to moderate outpatient COVID-19: A randomized triple-blind placebocontrolled clinical trial, Food Sci. Nutr
Ahmadi, Oral nano-curcumin formulation efficacy in the management of mild to moderate outpatient COVID-19: a randomized triple-blind placebocontrolled clinical trial, Food Sci. Nutr
Akbik, Ghadiri, Chrzanowski, Rohanizadeh, Curcumin as a wound healing agent, Life Sci
Akdemir, The efficacy of dietary curcumin on growth performance, lipid peroxidation and hepatic transcription factors in rainbow trout Oncorhynchus mykiss (Walbaum) reared under different stocking densities, Aquac. Res
Alinezhad, Alinezhad, Ataee, Ataie, Utilization of curcumine and nanocurcumine compounds in cancer therapy, Pharm. Biomed. Res
Aloisio, A comprehensive appraisal of laboratory biochemistry tests as major predictors of COVID-19 severity, Arch. Pathol. Lab. Med
Ansari, Ahmad, Haqqi, Oxidative stress and inflammation in osteoarthritis pathogenesis: Role of polyphenols, Biomed. Pharmacother
Aqil, Munagala, Jeyabalan, Vadhanam, Bioavailability of phytochemicals and its enhancement by drug delivery systems, Cancer Lett
Asadirad, Antiinflammatory potential of nano-curcumin as an alternative therapeutic agent for the treatment of mild-to-moderate hospitalized COVID-19 patients in a placebo-controlled clinical trial, Phytother. Res
Asadirad, Antiinflammatory potential of nano-curcumin as an alternative therapeutic agent for the treatment of mild-to-moderate hospitalized COVID-19 patients in a placebo-controlled clinical trial, Phytother. Res
Askari, The efficacy of curcumin-piperine co-supplementation on clinical symptoms, duration, severity, and inflammatory factors in COVID-19 outpatients: a randomized double-blind, placebo-controlled trial, Trials
Badria, Development of provesicular nanodelivery system of curcumin as a safe and effective antiviral agent: statistical optimization, in vitro characterization, and antiviral effectiveness, Molecules
Bagheri, In vitro and in vivo studies on HPMA-based polymeric micelles loaded with curcumin, Mol. Pharm
Bangphumi, Pharmacokinetics of curcumin diethyl disuccinate, a prodrug of curcumin, in wistar rats, Eur. J. Drug Metab. Pharmacokinet
Barchitta, Nutrition and wound healing: an overview focusing on the beneficial effects of curcumin, Int. J. Mol. Sci
Basnet, Skalko-Basnet, Curcumin: an anti-inflammatory molecule from a curry spice on the path to cancer treatment, Molecules
Basuini, Microbial, immune and antioxidant responses of Nile tilapia with dietary nano-curcumin supplements under chronic low temperatures
Began, Sudharshan, Rao, Inhibition of lipoxygenase 1 by phosphatidylcholine micelles-bound curcumin, Lipids
Belcaro, Efficacy and safety of Meriva®, a curcumin-phosphatidylcholine complex, during extended administration in osteoarthritis patients, Alter. Med. Rev
Bitwell, Indra, Luke, Kakoma, A review of modern and conventional extraction techniques and their applications for extracting phytochemicals from plants, Sci. Afr
Bost, Host-viral infection maps reveal signatures of severe COVID-19 patients, Cell
Cao, Effects of curcumin on antioxidative activities and cytokine production in Jian carp (Cyprinus carpio var. Jian) with CCl4-induced liver damage, Fish, Shellfish Immunol
Cao, Mitochondrial and nuclear DNA damage induced by curcumin in human hepatoma G2 cells, Toxicol. Sci
Charan, Nanomaterials of curcumin-hyaluronic acid": their various methods of formulations, clinical and therapeutic applications, present gap, and future directions, Future J. Pharm. Sci
Chen, Clinical and immunological features of severe and moderate coronavirus disease 2019, J. Clin. Investig
Chen, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, lancet
Cheng, Topically applicated curcumin/gelatin-blended nanofibrous mat inhibits pancreatic adenocarcinoma by increasing ROS production and endoplasmic reticulum stress mediated apoptosis, J. Nanobiotechnology
Cho, Wang, Nie, Shin, Therapeutic nanoparticles for drug delivery in cancer, Clin. Cancer Res
Córdoba, Glycodendrimers as new tools in the search for effective anti-HIV DC-based immunotherapies, Nanomed, Nanotechnol. Biol. Med
De Coen, pH-degradable mannosylated nanogels for dendritic cell targeting, Biomacromolecules
De Gomes, Curcumin-loaded lipid-core nanocapsules attenuates the immune challenge LPS-induced in rats: neuroinflammatory and behavioral response in sickness behavior, J. Neuroimmunol
Denver, Mcclean, Distinguishing normal brain aging from the development of Alzheimer's disease: inflammation, insulin signaling and cognition, Neural Regen. Res
Dhule, Curcumin-loaded γ-cyclodextrin liposomal nanoparticles as delivery vehicles for osteosarcoma, Nanomed, Nanotechnol. Biol. Med
Djalali, The effects of nano-curcumin supplementation on Th1/Th17 balance in migraine patients: A randomized controlled clinical trial, Complement. Ther. Clin. Pract
Dolati, Nanocurcumin is a potential novel therapy for multiple sclerosis by influencing inflammatory mediators, Pharmacol. Rep
Dolati, Nanocurcumin restores aberrant miRNA expression profile in multiple sclerosis, randomized, double-blind, placebo-controlled trial, J. Cell. Physiol
Ebrahiminaseri, Combination treatment of dendrosomal nanocurcumin and low-level laser therapy develops proliferation and migration of mouse embryonic fibroblasts and alter TGF-β, VEGF, TNF-α and IL-6 expressions involved in wound healing process, PloS One
El-Dawy, Dowidar, Soliman, Arisha, Ameliorative effects of nanocurcumin on cyclophosphamide induced immunosuppression in male rats, Zagazig Vet. J
Faraji, Wipf, Nanoparticles in cellular drug delivery, Bioorg. Med. Chem
Farzaei, Curcumin in liver diseases: a systematic review of the cellular mechanisms of oxidative stress and clinical perspective, Nutrients
Farzaei, Curcumin in liver diseases: a systematic review of the cellular mechanisms of oxidative stress and clinical perspective, Nutrients
Fessler, Chang, Liu, Johnston, Curcumin confers anti-inflammatory effects in adults who recovered from COVID-19 and were subsequently vaccinated: a randomized controlled trial, Nutrients
Gao, Neuronal mitochondria-targeted delivery of curcumin by biomimetic engineered nanosystems in Alzheimer's disease mice, Acta Biomater
Gasmi, The role of diet and supplementation of natural products in COVID-19 prevention, Biol. Trace Elem. Res
Gayathri, Bhaskaran, Selvam, Thilagavathi, Nano formulation approaches for curcumin delivery-a review, J. Drug Deliv. Sci. Technol
Gera, Nanoformulations of curcumin: an emerging paradigm for improved remedial application, Oncotarget
Gera, Nanoformulations of curcumin: an emerging paradigm for improved remedial application, Oncotarget
Ghalandarlaki, Alizadeh, Ashkani-Esfahani, Nanotechnology-applied curcumin for different diseases therapy, BioMed. Res. Int
Ghalandarlaki, Alizadeh, Ashkani-Esfahani, Nanotechnology-applied curcumin for different diseases therapy, BioMed. Res. Int
Ghasemi, Curcumin inhibits NF-kB and Wnt/β-catenin pathways in cervical cancer cells, Pathol. Res. Pract
Giacomeli, Neuroprotective effects of curcumin lipid-core nanocapsules in a model Alzheimer's disease induced by β-amyloid 1-42 peptide in aged female mice, Brain Res
Giamarellos-Bourboulis, Complex immune dysregulation in COVID-19 patients with severe respiratory failure, Cell Host Microbe
Giulbudagian, Enhanced topical delivery of dexamethasone by β-cyclodextrin decorated thermoresponsive nanogels, Nanoscale
Goswami, Review of curcumin and its different formulations: pharmacokinetics, pharmacodynamics and pharmacokinetic-pharmacodynamic interactions, OBM Integr. Complement. Med
Gupta, Patchva, Aggarwal, Therapeutic roles of curcumin: lessons learned from clinical trials, AAPS J
Gupta, Patchva, Aggarwal, Therapeutic roles of curcumin: lessons learned from clinical trials, AAPS J
Hafez Ghoran, Curcumin-based nanoformulations: a promising adjuvant towards cancer treatment, Molecules
Hafez Ghoran, Curcumin-based nanoformulations: a promising adjuvant towards cancer treatment, Molecules
Hameeda, Comparison of effects of curcumin and nano-curcumin on the survival of human-derived mesenchymal stem cells: an experimental study, J. Adv. Oral. Res
Hanafy, El-Kemary, Silymarin/curcumin loaded albumin nanoparticles coated by chitosan as muco-inhalable delivery system observing anti-inflammatory and anti COVID-19 characterizations in oleic acid triggered lung injury and in vitro COVID-19 experiment, Int. J. Biol. Macromol
Hanai, Sugimoto, Curcumin has bright prospects for the treatment of inflammatory bowel disease, Curr. Pharm. Des
Hashemian, Mesenchymal stem cells derived from perinatal tissues for treatment of critically ill COVID-19-induced ARDS patients: a case series, Stem Cell Res. Ther
Hassaniazad, A triple-blind, placebo-controlled, randomized clinical trial to evaluate the effect of curcumin-containing nanomicelles on cellular immune responses subtypes and clinical outcome in COVID-19 patients, Phytother. Res
Hassaniazad, A triple-blind, placebo-controlled, randomized clinical trial to evaluate the effect of curcumin-containing nanomicelles on cellular immune responses subtypes and clinical outcome in COVID-19 patients, Phytother. Res
Hatamipour, Novel nanomicelle formulation to enhance bioavailability and stability of curcuminoids, Iran, J. Basic Med. Sci
He, Curcumin-loaded mesenchymal stem cell-derived exosomes efficiently attenuate proliferation and inflammatory response in rheumatoid arthritis fibroblast-like synoviocytes, Appl. Biochem Biotechnol
Hegde, Curcumin formulations for better bioavailability: what we learned from clinical trials thus far?, ACS Omega
Hellou, Effect of ArtemiC in patients with COVID-19: a Phase II prospective study, J. Cell. Mol. Med
Hewlings, Kalman, Curcumin: a review of its effects on human health, Foods
Honarkar Shafie, Effect of nanocurcumin supplementation on the severity of symptoms and length of hospital stay in patients with COVID-19: a randomized double-blind placebo-controlled trial, Phytother. Res
Hooff, Modulation of cholesterol, farnesylpyrophosphate, and geranylgeranylpyrophosphate in neuroblastoma SH-SY5Y-APP695 cells: impact on amyloid beta-protein production, Mol. Neurobiol
Huang, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, lancet
Jaimes-Aguirre, Polymer-based drug delivery systems, development and pre-clinical status, Curr. Pharm. Des
Jain, Singh, Mishra, Vyas, Mannosylated niosomes as adjuvant-carrier system for oral genetic immunization against Hepatitis B, Immunol. Lett
Jantan, Rohani, Sumantri, Immunomodulatory effects and mechanisms of curcuma species and their bioactive compounds: a review, Front. Pharmacol
Jones, Leroux, Polymeric micelles-a new generation of colloidal drug carriers, Eur. J. Pharm. Biopharm
Joshi, Recent updates on clinical developments of curcumin and its derivatives, Phytother. Res
Kakkar, Muppu, Chopra, Kaur, Curcumin loaded solid lipid nanoparticles: an efficient formulation approach for cerebral ischemic reperfusion injury in rats, Eur. J. Pharm. Biopharm
Kalani, Tyagi, Exosomes in neurological disease, neuroprotection, repair and therapeutics: problems and perspectives, Neural Regen. Res
Kang, Acid-activatable polymeric curcumin nanoparticles as therapeutic agents for osteoarthritis, Nanomed, Nanotechnol. Biol. Med
Karimi, Effects of nanocurcumin on inflammatory factors and clinical outcomes in critically ill patients with sepsis: a pilot randomized clinical trial, Eur. J. Integr. Med
Karimi, Evaluating the effects of curcumin nanomicelles on clinical outcome and cellular immune responses in critically ill sepsis patients: a randomized, double-blind, and placebo-controlled trial, Front. Nutr
Karimi, Nano-curcumin supplementation in critically ill patients with sepsis: a randomized clinical trial investigating the inflammatory biomarkers, oxidative stress indices, endothelial function, clinical outcomes and nutritional status, Food Funct
Karthic, Cyclodextrin nanoparticles for diagnosis and potential cancer therapy: A systematic review, Front. Cell Dev. Biol
Khezri, Saeedi, Mohammadamini, Zakaryaei, A comprehensive review of the therapeutic potential of curcumin nanoformulations, Phytother. Res
King, Steroid-associated side effects: a symptom management update on multiple myeloma treatment
Kishimoto, Newly developed highly bioavailable curcumin formulation, curcuRougeTM, reduces neutrophil/lymphocyte ratio in the elderly: a doubleblind, placebo-controlled clinical trial, J. Nutr. Sci. Vitaminol
Kloesch, In vitro study of a liposomal curcumin formulation (Lipocurc™): Toxicity and biological activity in synovial fibroblasts and macrophages, vivo
Kunnumakkara, Is curcumin bioavailability a problem in humans: Lessons from clinical trials, Expert Opin. Drug Metab. Toxicol
Leibovich, Macrophage-induced angiogenesis is mediated by tumour necrosis factor-α, Nature
Li, Shi, Li, Xu, Application of functional biocompatible nanomaterials to improve curcumin bioavailability, Front. Chem
Li, Wang, Xu, Cao, Potential antiviral therapeutics for 2019 Novel Coronavirus. Zhonghua jie he he hu xi za zhi= Zhonghua, jiehe he huxi zazhi= Chinese journal of tuberculosis and respiratory diseases
Liao, Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19, Nat. Med
Lin, Regulatory T cells and acute lung injury: cytokines, uncontrolled inflammation, and therapeutic implications, Front. Immunol
Lippi, Plebani, Laboratory abnormalities in patients with COVID-2019 infection, Clin. Chem. Lab. Med. (CCLM)
Liu, Curcumin ameliorates asthmatic airway inflammation by activating nuclear factor-E2-related factor 2/haem oxygenase (HO)-1 signalling pathway, Clin. Exp. Pharmacol. Physiol
Mahjoob, Stochaj, Curcumin nanoformulations to combat aging-related diseases, Ageing Res. Rev
Mahjoub, Bakhshinejad, Sadeghizadeh, Babashah, Combination treatment with dendrosomal nanocurcumin and doxorubicin improves anticancer effects on breast cancer cells through modulating CXCR4/NF-κB/Smo regulatory network, Mol. Biol. Rep
Maiti, Paladugu, Dunbar, Solid lipid curcumin particles provide greater anti-amyloid, anti-inflammatory and neuroprotective effects than curcumin in the 5xFAD mouse model of Alzheimer's disease, BMC Neurosci
Manca, Development of curcumin loaded sodium hyaluronate immobilized vesicles (hyalurosomes) and their potential on skin inflammation and wound restoring, Biomaterials
Manca, Nanoincorporation of curcumin in polymer-glycerosomes and evaluation of their in vitro-in vivo suitability as pulmonary delivery systems, RSC Adv
Manca, Potential therapeutic effect of curcumin loaded hyalurosomes against inflammatory and oxidative processes involved in the pathogenesis of rheumatoid arthritis: The use of fibroblast-like synovial cells cultured in synovial fluid, Eur. J. Pharm. Biopharm
Manconi, Chitosan and hyaluronan coated liposomes for pulmonary administration of curcumin, Int. J. Pharm
Marslin, Prakash, Qi, Franklin, Oral delivery of curcumin polymeric nanoparticles ameliorates CCl₄-induced subacute hepatotoxicity in wistar rats, Polymers (Basel)
Masuda, Structural identification of new curcumin dimers and their contribution to the antioxidant mechanism of curcumin, J. Agric. Food Chem
Mcnally, Curcumin induces heme oxygenase 1 through generation of reactive oxygen species, p38 activation and phosphatase inhibition, Int. J. Mol. Med
Mehta, COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet
Menuel, Synthesis and inclusion ability of a bis-β-cyclodextrin pseudocryptand towards Busulfan anticancer agent, Tetrahedron
Merad, Martin, Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages, Nat. Rev. Immunol
Miao, Fan, Li, Potential treatments for COVID-19 related cytokine storm-beyond corticosteroids, Front. Immunol
Milano, Nano-curcumin inhibits proliferation of esophageal adenocarcinoma cells and enhances the T cell mediated immune response, Front. Oncol
Mirzaei, Phytosomal curcumin: a review of pharmacokinetic, experimental and clinical studies, Biomed. Pharmacother
Moon, Fighting COVID-19 exhausts T cells, Nat. Rev. Immunol
Mounce, Curcumin inhibits Zika and chikungunya virus infection by inhibiting cell binding, Antivir. Res
Nabila, Antiviral action of curcumin encapsulated in nanoemulsion against four serotypes of dengue virus, Pharm. Nanotechnol
Naksuriya, Okonogi, Schiffelers, Hennink, Curcumin nanoformulations: a review of pharmaceutical properties and preclinical studies and clinical data related to cancer treatment, Biomaterials
Nanjwade, Dendrimers: emerging polymers for drug-delivery systems, Eur. J. Pharm. Sci
Naz, Ahmad, Curcumin-loaded colloidal carrier system: formulation optimization, mechanistic insight, ex vivo and in vivo evaluation, Int. J. Nanomed
Negi, Jayaprakasha, Jagan Mohan Rao, Sakariah, Antibacterial activity of turmeric oil: a byproduct from curcumin manufacture, J. Agric. Food Chem
Ng, Assessing the potential of liposomes loaded with curcumin as a therapeutic intervention in asthma, Colloids Surf, B: Biointerfaces
Ni, Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals, Immunity
Nienhold, Two distinct immunopathological profiles in autopsy lungs of COVID-19, Nat. Commun
Nivetha, Efficacy of nanocurcumin with application of iontophoresis on inflammatory arthritis patients, Res. J. Pharm. Technol
Noori, Potency of BNT162b2 and mRNA-1273 vaccine-induced neutralizing antibodies against severe acute respiratory syndrome-CoV-2 variants of concern: a systematic review of in vitro studies, Rev. Med. Virol
Ohno, Nanoparticle curcumin ameliorates experimental colitis via modulation of gut microbiota and induction of regulatory T cells, PloS One
Osali, Aerobic exercise and nano-curcumin supplementation improve inflammation in elderly females with metabolic syndrome, Diabetol. Metab. Syndr
Panzarini, Novel therapeutic delivery of nanocurcumin in central nervous system related disorders, Nanomaterials
Patwekar, Khavane, Chainpure, Shivpuje, A review on different preparation methods used for development of curcumin nanoparticles, Int. J. Creat. Res. Thoughts
Prado-Audelo, Formulations of curcumin nanoparticles for brain diseases, Biomolecules
Proal, Vanelzakker, Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms, Front. Microbiol
Prompetchara, Ketloy, Palaga, Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic, Asian Pac, J. Allergy Immunol
Qiu, Overdose intake of curcumin initiates the unbalanced state of bodies, J. Agric. Food Chem
Quispe, Nanoderived therapeutic formulations with curcumin in inflammation-related diseases, Oxid. Med. Cell. Longev
Rad, Optimization of curcumin loaded niosomes for drug delivery applications, Colloids Surf. A: Physicochem. Eng. Asp
Rafiee, Nejatian, Daeihamed, Jafari, Application of curcuminloaded nanocarriers for food, drug and cosmetic purposes, Trends Food Sci. Technol
Rafiee, Nejatian, Daeihamed, Jafari, Application of different nanocarriers for encapsulation of curcumin, Crit. Rev. Food Sci. Nutr
Rahimi, Curcumin: a dietary phytochemical for targeting the phenotype and function of dendritic cells, Curr. Med. Chem
Reda, Effect of dietary supplementation of biological curcumin nanoparticles on growth and carcass traits, antioxidant status, immunity and caecal microbiota of Japanese quails, Animals
Remuzzi, Remuzzi, COVID-19 and Italy: what next?, lancet
Remy, Immunotherapies for COVID-19: lessons learned from sepsis, Lancet Respir. Med
Ritchie, Singanayagam, Immunosuppression for hyperinflammation in COVID-19: a double-edged sword, Lancet
Rocha, De Assis, Curcumin as a potential treatment for COVID-19, Phytother. Res
Russell, Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence, ecancermedicalscience
Russell, Millar, Baillie, Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury, Lancet
Saber-Moghaddam, Oral nano-curcumin formulation efficacy in management of mild to moderate hospitalized coronavirus disease-19 patients: An open label nonrandomized clinical trial, Phytother. Res
Saber-Moghaddam, Oral nano-curcumin formulation efficacy in management of mild to moderate hospitalized coronavirus disease-19 patients: An open label nonrandomized clinical trial, Phytother. Res
Sabouni, Role of curcumin and its nanoformulations in the treatment of neurological diseases through the effects on stem cells, J. Drug Target
Sadeghizadeh, Promising clinical outcomes of nano-curcumin treatment as an adjunct therapy in hospitalized COVID-19 patients: A randomized, doubleblinded, placebo-controlled trial, Phytother. Res
Schneider, Lipid based therapy for ulcerative colitis-modulation of intestinal mucus membrane phospholipids as a tool to influence inflammation, Int. J. Mol. Sci
Schultze, Aschenbrenner, COVID-19 and the human innate immune system, Cell
Sedighiyan, The effects of nano-curcumin supplementation on adipokines levels in obese and overweight patients with migraine: a double blind clinical trial study, BMC Res. Notes
Sette, Crotty, Adaptive immunity to SARS-CoV-2 and COVID-19, Cell
Sharma, Immunomodulatory activities of curcumin-stabilized silver nanoparticles: Efficacy as an antiretroviral therapeutic, Immunol. Investig
Sharma, Nanocurcumin Potently Inhibits SARS-CoV-2 Spike Protein-Induced Cytokine Storm by Deactivation of MAPK/NF-κB Signaling in Epithelial Cells, ACS Appl. Bio Mater
Shi, Extraction and characterization of phenolic compounds and their potential antioxidant activities, Environ. Sci. Pollut. Res
Sohn, Biomedical applications and bioavailability of curcumin-an updated overview, Pharmaceutics
Soveyd, The combined effects of ω-3 fatty acids and nano-curcumin supplementation on intercellular adhesion molecule-1 (ICAM-1) gene expression and serum levels in migraine patients, CNS Neurol. Disord. -Drug Targets (Former. Curr. Drug Targets-CNS Neurol. Disord.)
Tahmasebi, Immunomodulatory effects of nanocurcumin on Th17 cell responses in mild and severe COVID-19 patients, J. Cell Physiol
Tahmasebi, Immunomodulatory effects of nanocurcumin on Th17 cell responses in mild and severe COVID-19 patients, J. Cell. Physiol
Tahmasebi, Nanocurcumin improves Treg cell responses in patients with mild and severe SARS-CoV2, Life Sci
Teiten, Eifes, Dicato, Diederich, Curcumin-the paradigm of a multi-target natural compound with applications in cancer prevention and treatment, Toxins
Tian, Immune suppression in the early stage of COVID-19 disease, Nat. Commun
Trivedi, Mondal, Gangwar, Jana, Immunomodulatory potential of nanocurcumin-based formulation, Inflammopharmacology
Trivedi, Mondal, Gangwar, Jana, Immunomodulatory potential of nanocurcumin-based formulation, Inflammopharmacology
Tyagi, Identification of a novel compound (β-sesquiphellandrene) from turmeric (Curcuma longa) with anticancer potential: comparison with curcumin, Invest N. Drugs
Vafadar_Afshar, Khadem-Ansari, Makhdomii, Rasooli, The effects of nano-curcumin supplementation on serum level of hs-CRP, adhesion molecules, and lipid profiles in hemodialysis patients, a randomized controlled clinical trial, Iran, J. Kidney Dis
Vahedian-Azimi, Effectiveness of curcumin on outcomes of hospitalized COVID-19 patients: a systematic review of clinical trials, Nutrients
Valizadeh, Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients, Int Immunopharmacol
Valizadeh, Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients, Int. Immunopharmacol
Vaninov, In the eye of the COVID-19 cytokine storm, Nat. Rev. Immunol
Venkatas, Daniels, Singh, The potential of curcumin-capped nanoparticle synthesis in cancer therapy: a green synthesis approach, Nanomaterials
Vitaglione, Curcumin bioavailability from enriched bread: the effect of microencapsulated ingredients, J. Agric. Food Chem
Wang, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, Jama
Wen, Li, Yan, Su, Turmeric carbon quantum dots enhanced chitosan nanocomposite films based on photodynamic inactivation technology for antibacterial food packaging, Carbohydr. Polym
Wilken, Veena, Wang, Srivatsan, Curcumin: A review of anticancer properties and therapeutic activity in head and neck squamous cell carcinoma, Mol. Cancer
Wu, Yang, TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib, J. Microbiol. Immunol. Infect
Xu, Kim, Saylor, Koo, Polymer degradation and drug delivery in PLGA-based drug-polymer applications: A review of experiments and theories, J. Biomed. Mater. Res. Part B: Appl. Biomater
Xu, The differential immune responses to COVID-19 in peripheral and lung revealed by single-cell RNA sequencing, Cell Discov
Yadav, Suresh, Devi, Yadav, Effect of cyclodextrin complexation of curcumin on its solubility and antiangiogenic and anti-inflammatory activity in rat colitis model, Aaps Pharmscitech
Yallapu, Interaction of curcumin nanoformulations with human plasma proteins and erythrocytes, Int. J. Nanomed
Yan, Green synthesis of carbon quantum dots from plant turmeric holds promise as novel photosensitizer for in vitro photodynamic antimicrobial activity, J. Mater. Res. Technol
Yang, COVID-19: immunopathogenesis and Immunotherapeutics, Signal Transduct. Target. Ther
Yang, Zhang, Fan, Liu, Curcumin upregulates transcription factor Nrf2, HO-1 expression and protects rat brains against focal ischemia, Brain Res
Yang, Zheng, Wang, Zhao, Curcumin-loaded chitosan-bovine serum albumin nanoparticles potentially enhanced Aβ 42 phagocytosis and modulated macrophage polarization in Alzheimer's disease, Nanoscale Res. Lett
Ye, Wang, Mao, The pathogenesis and treatment of theCytokine Storm'in COVID-19, J. Infect
Zha, Banik, Alexis, Stimulus responsive nanogels for drug delivery, Soft Matter
Zhang, CD44 assists the topical anti-psoriatic efficacy of curcuminloaded hyaluronan-modified ethosomes: a new strategy for clustering drug in inflammatory skin, Theranostics
Zhang, COVID-19 infection induces readily detectable morphological and inflammation-related phenotypic changes in peripheral blood monocytes, the severity of which correlate with patient outcome, MedRxiv
Zhang, Comparison of ethosomes and liposomes for skin delivery of psoralen for psoriasis therapy, Int. J. Pharm
Zhang, Nanoparticles containing a liver X receptor agonist inhibit inflammation and atherosclerosis, Adv. Healthc. Mater
Zhang, Zhang, Curcumin loading on alginate nano-micelle for anti-infection and colonic wound healing, J. Biomed. Nanotechnol
Zheng, Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients, Cell. Mol. Immunol
Zheng, The effect of curcumin and its nanoformulation on adjuvantinduced arthritis in rats, Drug Des, Dev. Ther
Zhou, Fu, Zheng, Aberrant pathogenic GM-CSF+ T cells and inflammatory CD14+CD16+monocytes in severe pulmonary syndrome patients of a new coronavirus, bioRxiv
Zocchi, Tosetti, Benelli, Poggi, Cancer nanomedicine special issue review anticancer drug delivery with nanoparticles: extracellular vesicles or synthetic nanobeads as therapeutic tools for conventional treatment or immunotherapy, Cancers
Zou, Polymeric curcumin nanoparticle pharmacokinetics and metabolism in bile duct cannulated rats, Mol. Pharm
DOI record:
{
"DOI": "10.1016/j.biopha.2024.116131",
"ISSN": [
"0753-3322"
],
"URL": "http://dx.doi.org/10.1016/j.biopha.2024.116131",
"alternative-id": [
"S075333222400012X"
],
"article-number": "116131",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Immunoregulatory effects of nanocurcumin in inflammatory milieu: Focus on COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Biomedicine & Pharmacotherapy"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.biopha.2024.116131"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2024 The Authors. Published by Elsevier Masson SAS."
}
],
"author": [
{
"affiliation": [],
"family": "Arab",
"given": "Fahimeh Lavi",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hoseinzadeh",
"given": "Akram",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohammadi",
"given": "Fatemeh Sadat",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rajabian",
"given": "Arezoo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Faridzadeh",
"given": "Arezoo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mahmoudi",
"given": "Mahmoud",
"sequence": "additional"
}
],
"container-title": "Biomedicine & Pharmacotherapy",
"container-title-short": "Biomedicine & Pharmacotherapy",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"em-consulte.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2024,
1,
9
]
],
"date-time": "2024-01-09T19:06:29Z",
"timestamp": 1704827189000
},
"deposited": {
"date-parts": [
[
2024,
1,
10
]
],
"date-time": "2024-01-10T06:30:46Z",
"timestamp": 1704868246000
},
"indexed": {
"date-parts": [
[
2024,
1,
11
]
],
"date-time": "2024-01-11T00:26:12Z",
"timestamp": 1704932772057
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
2
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
1
]
],
"date-time": "2024-02-01T00:00:00Z",
"timestamp": 1706745600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
2
]
],
"date-time": "2024-01-02T00:00:00Z",
"timestamp": 1704153600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S075333222400012X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S075333222400012X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "116131",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2024,
2
]
]
},
"published-print": {
"date-parts": [
[
2024,
2
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1002/ptr.7974",
"article-title": "Recent updates on clinical developments of curcumin and its derivatives",
"author": "Joshi",
"doi-asserted-by": "crossref",
"first-page": "5109",
"issue": "11",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib1",
"volume": "37",
"year": "2023"
},
{
"DOI": "10.1208/s12248-012-9432-8",
"article-title": "Therapeutic roles of curcumin: lessons learned from clinical trials",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "195",
"issue": "1",
"journal-title": "AAPS J.",
"key": "10.1016/j.biopha.2024.116131_bib2",
"volume": "15",
"year": "2013"
},
{
"DOI": "10.1021/acs.molpharmaceut.0c01114",
"article-title": "In vitro and in vivo studies on HPMA-based polymeric micelles loaded with curcumin",
"author": "Bagheri",
"doi-asserted-by": "crossref",
"first-page": "1247",
"issue": "3",
"journal-title": "Mol. Pharm.",
"key": "10.1016/j.biopha.2024.116131_bib3",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1186/s12951-020-00687-2",
"article-title": "Topically applicated curcumin/gelatin-blended nanofibrous mat inhibits pancreatic adenocarcinoma by increasing ROS production and endoplasmic reticulum stress mediated apoptosis",
"author": "Cheng",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J. Nanobiotechnology",
"key": "10.1016/j.biopha.2024.116131_bib4",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.3390/nu14020256",
"article-title": "Effectiveness of curcumin on outcomes of hospitalized COVID-19 patients: a systematic review of clinical trials",
"author": "Vahedian-Azimi",
"doi-asserted-by": "crossref",
"first-page": "256",
"issue": "2",
"journal-title": "Nutrients",
"key": "10.1016/j.biopha.2024.116131_bib5",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1002/rmv.2277",
"article-title": "Potency of BNT162b2 and mRNA‐1273 vaccine‐induced neutralizing antibodies against severe acute respiratory syndrome‐CoV‐2 variants of concern: a systematic review of in vitro studies",
"author": "Noori",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "Rev. Med. Virol.",
"key": "10.1016/j.biopha.2024.116131_bib6",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.3389/fmicb.2021.698169",
"article-title": "Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms",
"author": "Proal",
"doi-asserted-by": "crossref",
"first-page": "1494",
"journal-title": "Front. Microbiol.",
"key": "10.1016/j.biopha.2024.116131_bib7",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"article-title": "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "507",
"issue": "10223",
"journal-title": "lancet",
"key": "10.1016/j.biopha.2024.116131_bib8",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"issue": "10223",
"journal-title": "lancet",
"key": "10.1016/j.biopha.2024.116131_bib9",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1061",
"issue": "11",
"journal-title": "Jama",
"key": "10.1016/j.biopha.2024.116131_bib10",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2021.02.029",
"article-title": "COVID-19 and the human innate immune system",
"author": "Schultze",
"doi-asserted-by": "crossref",
"first-page": "1671",
"issue": "7",
"journal-title": "Cell",
"key": "10.1016/j.biopha.2024.116131_bib11",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2021.01.007",
"article-title": "Adaptive immunity to SARS-CoV-2 and COVID-19",
"author": "Sette",
"doi-asserted-by": "crossref",
"first-page": "861",
"issue": "4",
"journal-title": "Cell",
"key": "10.1016/j.biopha.2024.116131_bib12",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.1038/s41392-020-00243-2",
"article-title": "COVID-19: immunopathogenesis and Immunotherapeutics",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "128",
"issue": "1",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "10.1016/j.biopha.2024.116131_bib13",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.chom.2020.04.009",
"article-title": "Complex immune dysregulation in COVID-19 patients with severe respiratory failure",
"author": "Giamarellos-Bourboulis",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Cell Host Microbe",
"key": "10.1016/j.biopha.2024.116131_bib14",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30217-4",
"article-title": "Immunotherapies for COVID-19: lessons learned from sepsis",
"author": "Remy",
"doi-asserted-by": "crossref",
"first-page": "946",
"issue": "10",
"journal-title": "Lancet Respir. Med.",
"key": "10.1016/j.biopha.2024.116131_bib15",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30691-7",
"article-title": "Immunosuppression for hyperinflammation in COVID-19: a double-edged sword",
"author": "Ritchie",
"doi-asserted-by": "crossref",
"first-page": "1111",
"issue": "10230",
"journal-title": "Lancet",
"key": "10.1016/j.biopha.2024.116131_bib16",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1002/jcp.30233",
"article-title": "Immunomodulatory effects of nanocurcumin on Th17 cell responses in mild and severe COVID‐19 patients",
"author": "Tahmasebi",
"doi-asserted-by": "crossref",
"first-page": "5325",
"issue": "7",
"journal-title": "J. Cell. Physiol.",
"key": "10.1016/j.biopha.2024.116131_bib17",
"volume": "236",
"year": "2021"
},
{
"DOI": "10.1007/s12011-021-02623-3",
"article-title": "The role of diet and supplementation of natural products in COVID-19 prevention",
"author": "Gasmi",
"doi-asserted-by": "crossref",
"first-page": "27",
"issue": "1",
"journal-title": "Biol. Trace Elem. Res.",
"key": "10.1016/j.biopha.2024.116131_bib18",
"volume": "200",
"year": "2022"
},
{
"article-title": "Immunomodulatory effects and mechanisms of curcuma species and their bioactive compounds: a review",
"author": "Jantan",
"journal-title": "Front. Pharmacol.",
"key": "10.1016/j.biopha.2024.116131_bib19",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.2174/0929867327666200515101228",
"article-title": "Curcumin: a dietary phytochemical for targeting the phenotype and function of dendritic cells",
"author": "Rahimi",
"doi-asserted-by": "crossref",
"first-page": "1549",
"issue": "8",
"journal-title": "Curr. Med. Chem.",
"key": "10.1016/j.biopha.2024.116131_bib20",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.prp.2019.152556",
"article-title": "Curcumin inhibits NF-kB and Wnt/β-catenin pathways in cervical cancer cells",
"author": "Ghasemi",
"doi-asserted-by": "crossref",
"issue": "10",
"journal-title": "Pathol. Res. Pract.",
"key": "10.1016/j.biopha.2024.116131_bib21",
"volume": "215",
"year": "2019"
},
{
"DOI": "10.1002/ptr.6745",
"article-title": "Curcumin as a potential treatment for COVID‐19",
"author": "Rocha",
"doi-asserted-by": "crossref",
"first-page": "2085",
"issue": "9",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib22",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.3390/molecules25235668",
"article-title": "Development of provesicular nanodelivery system of curcumin as a safe and effective antiviral agent: statistical optimization, in vitro characterization, and antiviral effectiveness",
"author": "Badria",
"doi-asserted-by": "crossref",
"first-page": "5668",
"issue": "23",
"journal-title": "Molecules",
"key": "10.1016/j.biopha.2024.116131_bib23",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.3390/foods6100092",
"article-title": "Curcumin: a review of its effects on human health",
"author": "Hewlings",
"doi-asserted-by": "crossref",
"first-page": "92",
"issue": "10",
"journal-title": "Foods",
"key": "10.1016/j.biopha.2024.116131_bib24",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1208/s12248-012-9432-8",
"article-title": "Therapeutic roles of curcumin: lessons learned from clinical trials",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "195",
"journal-title": "AAPS J.",
"key": "10.1016/j.biopha.2024.116131_bib25",
"volume": "15",
"year": "2013"
},
{
"DOI": "10.1080/17425255.2019.1650914",
"article-title": "Is curcumin bioavailability a problem in humans: Lessons from clinical trials",
"author": "Kunnumakkara",
"doi-asserted-by": "crossref",
"first-page": "705",
"issue": "9",
"journal-title": "Expert Opin. Drug Metab. Toxicol.",
"key": "10.1016/j.biopha.2024.116131_bib26",
"volume": "15",
"year": "2019"
},
{
"DOI": "10.1016/j.jmrt.2022.11.090",
"article-title": "Green synthesis of carbon quantum dots from plant turmeric holds promise as novel photosensitizer for in vitro photodynamic antimicrobial activity",
"author": "Yan",
"doi-asserted-by": "crossref",
"first-page": "17",
"journal-title": "J. Mater. Res. Technol.",
"key": "10.1016/j.biopha.2024.116131_bib27",
"volume": "22",
"year": "2023"
},
{
"article-title": "Nano formulation approaches for curcumin delivery- a review",
"author": "Gayathri",
"journal-title": "J. Drug Deliv. Sci. Technol.",
"key": "10.1016/j.biopha.2024.116131_bib28",
"volume": "82",
"year": "2023"
},
{
"DOI": "10.3390/pharmaceutics13122102",
"article-title": "Biomedical applications and bioavailability of curcumin-an updated overview",
"author": "Sohn",
"doi-asserted-by": "crossref",
"issue": "12",
"journal-title": "Pharmaceutics",
"key": "10.1016/j.biopha.2024.116131_bib29",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1155/2014/394264",
"article-title": "Nanotechnology-applied curcumin for different diseases therapy",
"author": "Ghalandarlaki",
"doi-asserted-by": "crossref",
"journal-title": "BioMed. Res. Int.",
"key": "10.1016/j.biopha.2024.116131_bib30",
"volume": "2014",
"year": "2014"
},
{
"DOI": "10.1016/j.tifs.2019.04.017",
"article-title": "Application of curcumin-loaded nanocarriers for food, drug and cosmetic purposes",
"author": "Rafiee",
"doi-asserted-by": "crossref",
"first-page": "445",
"journal-title": "Trends Food Sci. Technol.",
"key": "10.1016/j.biopha.2024.116131_bib31",
"volume": "88",
"year": "2019"
},
{
"DOI": "10.3390/nano12183201",
"article-title": "The potential of curcumin-capped nanoparticle synthesis in cancer therapy: a green synthesis approach",
"author": "Venkatas",
"doi-asserted-by": "crossref",
"first-page": "3201",
"issue": "18",
"journal-title": "Nanomaterials",
"key": "10.1016/j.biopha.2024.116131_bib32",
"volume": "12",
"year": "2022"
},
{
"article-title": "A review on different preparation methods used for development of curcumin nanoparticles",
"author": "Patwekar",
"first-page": "4088",
"issue": "1",
"journal-title": "Int. J. Creat. Res. Thoughts",
"key": "10.1016/j.biopha.2024.116131_bib33",
"volume": "9",
"year": "2021"
},
{
"article-title": "“Nanomaterials of curcumin-hyaluronic acid”: their various methods of formulations, clinical and therapeutic applications, present gap, and future directions",
"author": "Charan",
"first-page": "1",
"issue": "1",
"journal-title": "Future J. Pharm. Sci.",
"key": "10.1016/j.biopha.2024.116131_bib34",
"volume": "7",
"year": "2021"
},
{
"article-title": "A review of modern and conventional extraction techniques and their applications for extracting phytochemicals from plants",
"author": "Bitwell",
"journal-title": "Sci. Afr.",
"key": "10.1016/j.biopha.2024.116131_bib35",
"volume": "19",
"year": "2023"
},
{
"DOI": "10.1007/s11356-022-23337-6",
"article-title": "Extraction and characterization of phenolic compounds and their potential antioxidant activities",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "81112",
"issue": "54",
"journal-title": "Environ. Sci. Pollut. Res.",
"key": "10.1016/j.biopha.2024.116131_bib36",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.4103/jpbs.JPBS_175_19",
"article-title": "Preparation of medicinal plants: basic extraction and fractionation procedures for experimental purposes",
"author": "Abubakar",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "J. Pharm. Bioallied Sci.",
"key": "10.1016/j.biopha.2024.116131_bib37",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.18632/oncotarget.19164",
"article-title": "Nanoformulations of curcumin: an emerging paradigm for improved remedial application",
"author": "Gera",
"doi-asserted-by": "crossref",
"first-page": "66680",
"issue": "39",
"journal-title": "Oncotarget",
"key": "10.1016/j.biopha.2024.116131_bib38",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1016/j.colsurfa.2022.129921",
"article-title": "Optimization of curcumin loaded niosomes for drug delivery applications",
"author": "Esmaeili Rad",
"doi-asserted-by": "crossref",
"journal-title": "Colloids Surf. A: Physicochem. Eng. Asp.",
"key": "10.1016/j.biopha.2024.116131_bib39",
"volume": "654",
"year": "2022"
},
{
"DOI": "10.1002/ptr.7190",
"article-title": "A comprehensive review of the therapeutic potential of curcumin nanoformulations",
"author": "Khezri",
"doi-asserted-by": "crossref",
"first-page": "5527",
"issue": "10",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib40",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2018.1495174",
"article-title": "Application of different nanocarriers for encapsulation of curcumin",
"author": "Rafiee",
"doi-asserted-by": "crossref",
"first-page": "3468",
"issue": "21",
"journal-title": "Crit. Rev. Food Sci. Nutr.",
"key": "10.1016/j.biopha.2024.116131_bib41",
"volume": "59",
"year": "2019"
},
{
"DOI": "10.3389/fchem.2020.589957",
"article-title": "Application of functional biocompatible nanomaterials to improve curcumin bioavailability",
"author": "Li",
"doi-asserted-by": "crossref",
"journal-title": "Front. Chem.",
"key": "10.1016/j.biopha.2024.116131_bib42",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3390/molecules27165236",
"article-title": "Curcumin-based nanoformulations: a promising adjuvant towards cancer treatment",
"author": "Hafez Ghoran",
"doi-asserted-by": "crossref",
"issue": "16",
"journal-title": "Molecules",
"key": "10.1016/j.biopha.2024.116131_bib43",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1016/j.carbpol.2023.120784",
"article-title": "Turmeric carbon quantum dots enhanced chitosan nanocomposite films based on photodynamic inactivation technology for antibacterial food packaging",
"author": "Wen",
"doi-asserted-by": "crossref",
"journal-title": "Carbohydr. Polym.",
"key": "10.1016/j.biopha.2024.116131_bib44",
"volume": "311",
"year": "2023"
},
{
"DOI": "10.3390/molecules27165236",
"article-title": "Curcumin-based nanoformulations: a promising adjuvant towards cancer treatment",
"author": "Hafez Ghoran",
"doi-asserted-by": "crossref",
"first-page": "5236",
"issue": "16",
"journal-title": "Molecules",
"key": "10.1016/j.biopha.2024.116131_bib45",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.3389/fcell.2022.984311",
"article-title": "Cyclodextrin nanoparticles for diagnosis and potential cancer therapy: A systematic review",
"author": "Karthic",
"doi-asserted-by": "crossref",
"journal-title": "Front. Cell Dev. Biol.",
"key": "10.1016/j.biopha.2024.116131_bib46",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1021/acsomega.2c07326",
"article-title": "Curcumin formulations for better bioavailability: what we learned from clinical trials thus far?",
"author": "Hegde",
"doi-asserted-by": "crossref",
"first-page": "10713",
"issue": "12",
"journal-title": "ACS Omega",
"key": "10.1016/j.biopha.2024.116131_bib47",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.21608/zvjz.2020.20524.1090",
"article-title": "Ameliorative effects of nanocurcumin on cyclophosphamide induced immunosuppression in male rats",
"author": "El-Dawy",
"doi-asserted-by": "crossref",
"first-page": "228",
"issue": "3",
"journal-title": "Zagazig Vet. J.",
"key": "10.1016/j.biopha.2024.116131_bib48",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.3390/cancers12071886",
"article-title": "Cancer nanomedicine special issue review anticancer drug delivery with nanoparticles: extracellular vesicles or synthetic nanobeads as therapeutic tools for conventional treatment or immunotherapy",
"author": "Zocchi",
"doi-asserted-by": "crossref",
"first-page": "1886",
"issue": "7",
"journal-title": "Cancers",
"key": "10.1016/j.biopha.2024.116131_bib49",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1038/s41598-023-29343-z",
"article-title": "A comparative study of effects of curcumin and its nanoparticles on the growth, immunity and heat stress resistance of Nile tilapia (Oreochromis niloticus)",
"author": "Abdel-Ghany",
"doi-asserted-by": "crossref",
"first-page": "2523",
"issue": "1",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.biopha.2024.116131_bib50",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1016/j.fsi.2014.12.025",
"article-title": "Effects of curcumin on antioxidative activities and cytokine production in Jian carp (Cyprinus carpio var. Jian) with CCl4-induced liver damage",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "150",
"issue": "1",
"journal-title": "Fish. Shellfish Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib51",
"volume": "43",
"year": "2015"
},
{
"DOI": "10.1093/toxsci/kfj153",
"article-title": "Mitochondrial and nuclear DNA damage induced by curcumin in human hepatoma G2 cells",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "476",
"issue": "2",
"journal-title": "Toxicol. Sci.",
"key": "10.1016/j.biopha.2024.116131_bib52",
"volume": "91",
"year": "2006"
},
{
"DOI": "10.1021/acs.jafc.6b00053",
"article-title": "Overdose intake of curcumin initiates the unbalanced state of bodies",
"author": "Qiu",
"doi-asserted-by": "crossref",
"first-page": "2765",
"issue": "13",
"journal-title": "J. Agric. Food Chem.",
"key": "10.1016/j.biopha.2024.116131_bib53",
"volume": "64",
"year": "2016"
},
{
"DOI": "10.3390/nu10070855",
"article-title": "Curcumin in liver diseases: a systematic review of the cellular mechanisms of oxidative stress and clinical perspective",
"author": "Farzaei",
"doi-asserted-by": "crossref",
"first-page": "855",
"issue": "7",
"journal-title": "Nutrients",
"key": "10.1016/j.biopha.2024.116131_bib54",
"volume": "10",
"year": "2018"
},
{
"article-title": "Curcumin induces heme oxygenase 1 through generation of reactive oxygen species, p38 activation and phosphatase inhibition",
"author": "McNally",
"first-page": "165",
"issue": "1",
"journal-title": "Int. J. Mol. Med.",
"key": "10.1016/j.biopha.2024.116131_bib55",
"volume": "19",
"year": "2007"
},
{
"DOI": "10.3390/biom9020056",
"article-title": "Formulations of curcumin nanoparticles for brain diseases",
"author": "Prado-Audelo",
"doi-asserted-by": "crossref",
"first-page": "56",
"issue": "2",
"journal-title": "Biomolecules",
"key": "10.1016/j.biopha.2024.116131_bib56",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.2174/1381612822666160217125028",
"article-title": "Polymer-based drug delivery systems, development and pre-clinical status",
"author": "Jaimes-Aguirre",
"doi-asserted-by": "crossref",
"first-page": "2886",
"issue": "19",
"journal-title": "Curr. Pharm. Des.",
"key": "10.1016/j.biopha.2024.116131_bib57",
"volume": "22",
"year": "2016"
},
{
"DOI": "10.1002/jbm.b.33648",
"article-title": "Polymer degradation and drug delivery in PLGA‐based drug–polymer applications: A review of experiments and theories",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "1692",
"issue": "6",
"journal-title": "J. Biomed. Mater. Res. Part B: Appl. Biomater.",
"key": "10.1016/j.biopha.2024.116131_bib58",
"volume": "105",
"year": "2017"
},
{
"DOI": "10.1002/adhm.201400337",
"article-title": "Nanoparticles containing a liver X receptor agonist inhibit inflammation and atherosclerosis",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "228",
"issue": "2",
"journal-title": "Adv. Healthc. Mater.",
"key": "10.1016/j.biopha.2024.116131_bib59",
"volume": "4",
"year": "2015"
},
{
"DOI": "10.1016/j.ejpb.2013.02.005",
"article-title": "Curcumin loaded solid lipid nanoparticles: an efficient formulation approach for cerebral ischemic reperfusion injury in rats",
"author": "Kakkar",
"doi-asserted-by": "crossref",
"first-page": "339",
"issue": "3",
"journal-title": "Eur. J. Pharm. Biopharm.",
"key": "10.1016/j.biopha.2024.116131_bib60",
"volume": "85",
"year": "2013"
},
{
"DOI": "10.3390/ijms11104149",
"article-title": "Lipid based therapy for ulcerative colitis—modulation of intestinal mucus membrane phospholipids as a tool to influence inflammation",
"author": "Schneider",
"doi-asserted-by": "crossref",
"first-page": "4149",
"issue": "10",
"journal-title": "Int. J. Mol. Sci.",
"key": "10.1016/j.biopha.2024.116131_bib61",
"volume": "11",
"year": "2010"
},
{
"DOI": "10.1016/j.bmc.2009.02.043",
"article-title": "Nanoparticles in cellular drug delivery",
"author": "Faraji",
"doi-asserted-by": "crossref",
"first-page": "2950",
"issue": "8",
"journal-title": "Bioorg. Med. Chem.",
"key": "10.1016/j.biopha.2024.116131_bib62",
"volume": "17",
"year": "2009"
},
{
"DOI": "10.1158/1078-0432.CCR-07-1441",
"article-title": "Therapeutic nanoparticles for drug delivery in cancer",
"author": "Cho",
"doi-asserted-by": "crossref",
"first-page": "1310",
"issue": "5",
"journal-title": "Clin. Cancer Res.",
"key": "10.1016/j.biopha.2024.116131_bib63",
"volume": "14",
"year": "2008"
},
{
"DOI": "10.1155/2014/394264",
"article-title": "Nanotechnology-applied curcumin for different diseases therapy",
"author": "Ghalandarlaki",
"doi-asserted-by": "crossref",
"journal-title": "BioMed. Res. Int.",
"key": "10.1016/j.biopha.2024.116131_bib64",
"volume": "2014",
"year": "2014"
},
{
"DOI": "10.1186/s11671-018-2759-z",
"article-title": "Curcumin-loaded chitosan–bovine serum albumin nanoparticles potentially enhanced Aβ 42 phagocytosis and modulated macrophage polarization in Alzheimer’s disease",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Nanoscale Res. Lett.",
"key": "10.1016/j.biopha.2024.116131_bib65",
"volume": "13",
"year": "2018"
},
{
"DOI": "10.1016/j.brainres.2019.146325",
"article-title": "Neuroprotective effects of curcumin lipid-core nanocapsules in a model Alzheimer’s disease induced by β-amyloid 1-42 peptide in aged female mice",
"author": "Giacomeli",
"doi-asserted-by": "crossref",
"journal-title": "Brain Res.",
"key": "10.1016/j.biopha.2024.116131_bib66",
"volume": "1721",
"year": "2019"
},
{
"DOI": "10.1016/S0939-6411(99)00039-9",
"article-title": "Polymeric micelles–a new generation of colloidal drug carriers",
"author": "Jones",
"doi-asserted-by": "crossref",
"first-page": "101",
"issue": "2",
"journal-title": "Eur. J. Pharm. Biopharm.",
"key": "10.1016/j.biopha.2024.116131_bib67",
"volume": "48",
"year": "1999"
},
{
"DOI": "10.1016/j.canlet.2013.02.032",
"article-title": "Bioavailability of phytochemicals and its enhancement by drug delivery systems",
"author": "Aqil",
"doi-asserted-by": "crossref",
"first-page": "133",
"issue": "1",
"journal-title": "Cancer Lett.",
"key": "10.1016/j.biopha.2024.116131_bib68",
"volume": "334",
"year": "2013"
},
{
"DOI": "10.1208/s12249-009-9264-8",
"article-title": "Effect of cyclodextrin complexation of curcumin on its solubility and antiangiogenic and anti-inflammatory activity in rat colitis model",
"author": "Yadav",
"doi-asserted-by": "crossref",
"first-page": "752",
"issue": "3",
"journal-title": "Aaps Pharmscitech",
"key": "10.1016/j.biopha.2024.116131_bib69",
"volume": "10",
"year": "2009"
},
{
"DOI": "10.1016/j.nano.2011.07.011",
"article-title": "Curcumin-loaded γ-cyclodextrin liposomal nanoparticles as delivery vehicles for osteosarcoma",
"author": "Dhule",
"doi-asserted-by": "crossref",
"first-page": "440",
"issue": "4",
"journal-title": "Nanomed.: Nanotechnol. Biol. Med.",
"key": "10.1016/j.biopha.2024.116131_bib70",
"volume": "8",
"year": "2012"
},
{
"DOI": "10.1016/j.tet.2006.10.070",
"article-title": "Synthesis and inclusion ability of a bis-β-cyclodextrin pseudo-cryptand towards Busulfan anticancer agent",
"author": "Menuel",
"doi-asserted-by": "crossref",
"first-page": "1706",
"issue": "7",
"journal-title": "Tetrahedron",
"key": "10.1016/j.biopha.2024.116131_bib71",
"volume": "63",
"year": "2007"
},
{
"DOI": "10.18632/oncotarget.19164",
"article-title": "Nanoformulations of curcumin: an emerging paradigm for improved remedial application",
"author": "Gera",
"doi-asserted-by": "crossref",
"first-page": "66680",
"issue": "39",
"journal-title": "Oncotarget",
"key": "10.1016/j.biopha.2024.116131_bib72",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1007/s11745-998-0327-2",
"article-title": "Inhibition of lipoxygenase 1 by phosphatidylcholine micelles-bound curcumin",
"author": "Began",
"doi-asserted-by": "crossref",
"first-page": "1223",
"issue": "12",
"journal-title": "Lipids",
"key": "10.1016/j.biopha.2024.116131_bib73",
"volume": "33",
"year": "1998"
},
{
"DOI": "10.1016/j.imlet.2005.04.002",
"article-title": "Mannosylated niosomes as adjuvant–carrier system for oral genetic immunization against Hepatitis B",
"author": "Jain",
"doi-asserted-by": "crossref",
"first-page": "41",
"issue": "1",
"journal-title": "Immunol. Lett.",
"key": "10.1016/j.biopha.2024.116131_bib74",
"volume": "101",
"year": "2005"
},
{
"DOI": "10.1016/j.ejps.2009.07.008",
"article-title": "Dendrimers: emerging polymers for drug-delivery systems",
"author": "Nanjwade",
"doi-asserted-by": "crossref",
"first-page": "185",
"issue": "3",
"journal-title": "Eur. J. Pharm. Sci.",
"key": "10.1016/j.biopha.2024.116131_bib75",
"volume": "38",
"year": "2009"
},
{
"DOI": "10.1016/j.nano.2013.03.004",
"article-title": "Glycodendrimers as new tools in the search for effective anti-HIV DC-based immunotherapies",
"author": "Córdoba",
"doi-asserted-by": "crossref",
"first-page": "972",
"issue": "7",
"journal-title": "Nanomed.: Nanotechnol. Biol. Med.",
"key": "10.1016/j.biopha.2024.116131_bib76",
"volume": "9",
"year": "2013"
},
{
"article-title": "Interaction of curcumin nanoformulations with human plasma proteins and erythrocytes",
"author": "Yallapu",
"first-page": "2779",
"journal-title": "Int. J. Nanomed.",
"key": "10.1016/j.biopha.2024.116131_bib77",
"volume": "6",
"year": "2011"
},
{
"DOI": "10.1039/C7NR04480A",
"article-title": "Enhanced topical delivery of dexamethasone by β-cyclodextrin decorated thermoresponsive nanogels",
"author": "Giulbudagian",
"doi-asserted-by": "crossref",
"first-page": "469",
"issue": "1",
"journal-title": "Nanoscale",
"key": "10.1016/j.biopha.2024.116131_bib78",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1039/c0sm01307b",
"article-title": "Stimulus responsive nanogels for drug delivery",
"author": "Zha",
"doi-asserted-by": "crossref",
"first-page": "5908",
"issue": "13",
"journal-title": "Soft Matter",
"key": "10.1016/j.biopha.2024.116131_bib79",
"volume": "7",
"year": "2011"
},
{
"DOI": "10.1021/acs.biomac.6b00685",
"article-title": "pH-degradable mannosylated nanogels for dendritic cell targeting",
"author": "De Coen",
"doi-asserted-by": "crossref",
"first-page": "2479",
"issue": "7",
"journal-title": "Biomacromolecules",
"key": "10.1016/j.biopha.2024.116131_bib80",
"volume": "17",
"year": "2016"
},
{
"DOI": "10.2174/138161209788489177",
"article-title": "Curcumin has bright prospects for the treatment of inflammatory bowel disease",
"author": "Hanai",
"doi-asserted-by": "crossref",
"first-page": "2087",
"issue": "18",
"journal-title": "Curr. Pharm. Des.",
"key": "10.1016/j.biopha.2024.116131_bib81",
"volume": "15",
"year": "2009"
},
{
"article-title": "Novel nanomicelle formulation to enhance bioavailability and stability of curcuminoids",
"author": "Hatamipour",
"first-page": "282",
"issue": "3",
"journal-title": "Iran. J. Basic Med. Sci.",
"key": "10.1016/j.biopha.2024.116131_bib82",
"volume": "22",
"year": "2019"
},
{
"DOI": "10.1016/j.biopha.2016.11.098",
"article-title": "Phytosomal curcumin: a review of pharmacokinetic, experimental and clinical studies",
"author": "Mirzaei",
"doi-asserted-by": "crossref",
"first-page": "102",
"journal-title": "Biomed. Pharmacother.",
"key": "10.1016/j.biopha.2024.116131_bib83",
"volume": "85",
"year": "2017"
},
{
"DOI": "10.1021/mp4000019",
"article-title": "Polymeric curcumin nanoparticle pharmacokinetics and metabolism in bile duct cannulated rats",
"author": "Zou",
"doi-asserted-by": "crossref",
"first-page": "1977",
"issue": "5",
"journal-title": "Mol. Pharm.",
"key": "10.1016/j.biopha.2024.116131_bib84",
"volume": "10",
"year": "2013"
},
{
"DOI": "10.21926/obm.icm.2204057",
"article-title": "Review of curcumin and its different formulations: pharmacokinetics, pharmacodynamics and pharmacokinetic-pharmacodynamic interactions",
"author": "Goswami",
"doi-asserted-by": "crossref",
"first-page": "057",
"issue": "04",
"journal-title": "OBM Integr. Complement. Med.",
"key": "10.1016/j.biopha.2024.116131_bib85",
"volume": "07",
"year": "2022"
},
{
"DOI": "10.29252/pbr.3.3.1",
"article-title": "Utilization of curcumine and nanocurcumine compounds in cancer therapy",
"author": "Alinezhad",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "3",
"journal-title": "Pharm. Biomed. Res.",
"key": "10.1016/j.biopha.2024.116131_bib86",
"volume": "3",
"year": "2017"
},
{
"DOI": "10.1007/s13318-015-0308-z",
"article-title": "Pharmacokinetics of curcumin diethyl disuccinate, a prodrug of curcumin, in wistar rats",
"author": "Bangphumi",
"doi-asserted-by": "crossref",
"first-page": "777",
"issue": "6",
"journal-title": "Eur. J. Drug Metab. Pharmacokinet.",
"key": "10.1016/j.biopha.2024.116131_bib87",
"volume": "41",
"year": "2016"
},
{
"DOI": "10.1016/j.jneuroim.2020.577270",
"article-title": "Curcumin-loaded lipid-core nanocapsules attenuates the immune challenge LPS-induced in rats: neuroinflammatory and behavioral response in sickness behavior",
"author": "de Gomes",
"doi-asserted-by": "crossref",
"journal-title": "J. Neuroimmunol.",
"key": "10.1016/j.biopha.2024.116131_bib88",
"year": "2020"
},
{
"DOI": "10.1016/j.actbio.2020.03.029",
"article-title": "Neuronal mitochondria-targeted delivery of curcumin by biomimetic engineered nanosystems in Alzheimer's disease mice",
"author": "Gao",
"doi-asserted-by": "crossref",
"first-page": "285",
"journal-title": "Acta Biomater.",
"key": "10.1016/j.biopha.2024.116131_bib89",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1186/s12868-018-0406-3",
"article-title": "Solid lipid curcumin particles provide greater anti-amyloid, anti-inflammatory and neuroprotective effects than curcumin in the 5xFAD mouse model of Alzheimer’s disease",
"author": "Maiti",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "BMC Neurosci.",
"key": "10.1016/j.biopha.2024.116131_bib90",
"volume": "19",
"year": "2018"
},
{
"DOI": "10.4103/1673-5374.238608",
"article-title": "Distinguishing normal brain aging from the development of Alzheimer's disease: inflammation, insulin signaling and cognition",
"author": "Denver",
"doi-asserted-by": "crossref",
"first-page": "1719",
"issue": "10",
"journal-title": "Neural Regen. Res.",
"key": "10.1016/j.biopha.2024.116131_bib91",
"volume": "13",
"year": "2018"
},
{
"DOI": "10.1007/s10787-017-0395-3",
"article-title": "Immunomodulatory potential of nanocurcumin-based formulation",
"author": "Trivedi",
"doi-asserted-by": "crossref",
"first-page": "609",
"journal-title": "Inflammopharmacology",
"key": "10.1016/j.biopha.2024.116131_bib92",
"volume": "25",
"year": "2017"
},
{
"DOI": "10.1016/j.ejphar.2022.175267",
"article-title": "Immunomodulatory role of Nanocurcumin in COVID-19 patients with dropped natural killer cells frequency and function",
"author": "Abbaspour-Aghdam",
"doi-asserted-by": "crossref",
"journal-title": "Eur. J. Pharmacol.",
"key": "10.1016/j.biopha.2024.116131_bib93",
"volume": "933",
"year": "2022"
},
{
"article-title": "In vitro study of a liposomal curcumin formulation (Lipocurc™): Toxicity and biological activity in synovial fibroblasts and macrophages",
"author": "Kloesch",
"first-page": "413",
"issue": "4",
"journal-title": "vivo",
"key": "10.1016/j.biopha.2024.116131_bib94",
"volume": "30",
"year": "2016"
},
{
"DOI": "10.1016/j.ejpb.2019.01.012",
"article-title": "Potential therapeutic effect of curcumin loaded hyalurosomes against inflammatory and oxidative processes involved in the pathogenesis of rheumatoid arthritis: The use of fibroblast-like synovial cells cultured in synovial fluid",
"author": "Manca",
"doi-asserted-by": "crossref",
"first-page": "84",
"journal-title": "Eur. J. Pharm. Biopharm.",
"key": "10.1016/j.biopha.2024.116131_bib95",
"volume": "136",
"year": "2019"
},
{
"DOI": "10.1016/j.nano.2019.102104",
"article-title": "Acid-activatable polymeric curcumin nanoparticles as therapeutic agents for osteoarthritis",
"author": "Kang",
"doi-asserted-by": "crossref",
"journal-title": "Nanomed.: Nanotechnol. Biol. Med.",
"key": "10.1016/j.biopha.2024.116131_bib96",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1016/j.biopha.2020.110452",
"article-title": "Oxidative stress and inflammation in osteoarthritis pathogenesis: Role of polyphenols",
"author": "Ansari",
"doi-asserted-by": "crossref",
"journal-title": "Biomed. Pharmacother.",
"key": "10.1016/j.biopha.2024.116131_bib97",
"volume": "129",
"year": "2020"
},
{
"article-title": "The effect of curcumin and its nanoformulation on adjuvant-induced arthritis in rats",
"author": "Zheng",
"first-page": "4931",
"journal-title": "Drug Des., Dev. Ther.",
"key": "10.1016/j.biopha.2024.116131_bib98",
"year": "2015"
},
{
"DOI": "10.2147/IJN.S82788",
"article-title": "Curcumin-loaded colloidal carrier system: formulation optimization, mechanistic insight, ex vivo and in vivo evaluation",
"author": "Naz",
"doi-asserted-by": "crossref",
"first-page": "4293",
"journal-title": "Int. J. Nanomed.",
"key": "10.1016/j.biopha.2024.116131_bib99",
"year": "2015"
},
{
"article-title": "Efficacy and safety of Meriva®, a curcumin-phosphatidylcholine complex, during extended administration in osteoarthritis patients",
"author": "Belcaro",
"first-page": "337",
"issue": "4",
"journal-title": "Alter. Med. Rev.",
"key": "10.1016/j.biopha.2024.116131_bib100",
"volume": "15",
"year": "2010"
},
{
"article-title": "The effects of nano-curcumin supplementation on serum level of hs-CRP, adhesion molecules, and lipid profiles in hemodialysis patients, a randomized controlled clinical trial",
"author": "Vafadar_afshar",
"first-page": "52",
"issue": "1",
"journal-title": "Iran. J. Kidney Dis.",
"key": "10.1016/j.biopha.2024.116131_bib101",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1155/2021/3149223",
"article-title": "Nanoderived therapeutic formulations with curcumin in inflammation-related diseases",
"author": "Quispe",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Oxid. Med. Cell. Longev.",
"key": "10.1016/j.biopha.2024.116131_bib102",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.3390/nano11010002",
"article-title": "Novel therapeutic delivery of nanocurcumin in central nervous system related disorders",
"author": "Panzarini",
"doi-asserted-by": "crossref",
"first-page": "2",
"issue": "1",
"journal-title": "Nanomaterials",
"key": "10.1016/j.biopha.2024.116131_bib103",
"volume": "11",
"year": "2020"
},
{
"article-title": "The combined effects of ω-3 fatty acids and nano-curcumin supplementation on intercellular adhesion molecule-1 (ICAM-1) gene expression and serum levels in migraine patients",
"author": "Soveyd",
"first-page": "1120",
"issue": "10",
"journal-title": "CNS Neurol. Disord. -Drug Targets (Former. Curr. Drug Targets-CNS Neurol. Disord.)",
"key": "10.1016/j.biopha.2024.116131_bib104",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1166/jbn.2021.3089",
"article-title": "Curcumin loading on alginate nano-micelle for anti-infection and colonic wound healing",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1160",
"issue": "6",
"journal-title": "J. Biomed. Nanotechnol.",
"key": "10.1016/j.biopha.2024.116131_bib105",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1016/j.lfs.2014.08.016",
"article-title": "Curcumin as a wound healing agent",
"author": "Akbik",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "Life Sci.",
"key": "10.1016/j.biopha.2024.116131_bib106",
"volume": "116",
"year": "2014"
},
{
"DOI": "10.3390/ijms20051119",
"article-title": "Nutrition and wound healing: an overview focusing on the beneficial effects of curcumin",
"author": "Barchitta",
"doi-asserted-by": "crossref",
"first-page": "1119",
"issue": "5",
"journal-title": "Int. J. Mol. Sci.",
"key": "10.1016/j.biopha.2024.116131_bib107",
"volume": "20",
"year": "2019"
},
{
"DOI": "10.1371/journal.pone.0247098",
"article-title": "Combination treatment of dendrosomal nanocurcumin and low-level laser therapy develops proliferation and migration of mouse embryonic fibroblasts and alter TGF-β, VEGF, TNF-α and IL-6 expressions involved in wound healing process",
"author": "Ebrahiminaseri",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "PloS One",
"key": "10.1016/j.biopha.2024.116131_bib108",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.4103/1673-5374.165305",
"article-title": "Exosomes in neurological disease, neuroprotection, repair and therapeutics: problems and perspectives",
"author": "Kalani",
"doi-asserted-by": "crossref",
"first-page": "1565",
"issue": "10",
"journal-title": "Neural Regen. Res.",
"key": "10.1016/j.biopha.2024.116131_bib109",
"volume": "10",
"year": "2015"
},
{
"DOI": "10.1016/j.biomaterials.2015.08.034",
"article-title": "Development of curcumin loaded sodium hyaluronate immobilized vesicles (hyalurosomes) and their potential on skin inflammation and wound restoring",
"author": "Manca",
"doi-asserted-by": "crossref",
"first-page": "100",
"journal-title": "Biomaterials",
"key": "10.1016/j.biopha.2024.116131_bib110",
"volume": "71",
"year": "2015"
},
{
"DOI": "10.1016/j.ijpharm.2014.06.001",
"article-title": "Comparison of ethosomes and liposomes for skin delivery of psoralen for psoriasis therapy",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "449",
"issue": "1-2",
"journal-title": "Int. J. Pharm.",
"key": "10.1016/j.biopha.2024.116131_bib111",
"volume": "471",
"year": "2014"
},
{
"DOI": "10.7150/thno.29715",
"article-title": "CD44 assists the topical anti-psoriatic efficacy of curcumin-loaded hyaluronan-modified ethosomes: a new strategy for clustering drug in inflammatory skin",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "48",
"issue": "1",
"journal-title": "Theranostics",
"key": "10.1016/j.biopha.2024.116131_bib112",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1021/acsabm.1c00874",
"article-title": "Nanocurcumin Potently Inhibits SARS-CoV-2 Spike Protein-Induced Cytokine Storm by Deactivation of MAPK/NF-κB Signaling in Epithelial Cells",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "483",
"issue": "2",
"journal-title": "ACS Appl. Bio Mater.",
"key": "10.1016/j.biopha.2024.116131_bib113",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.1016/j.ijbiomac.2021.12.073",
"article-title": "Silymarin/curcumin loaded albumin nanoparticles coated by chitosan as muco-inhalable delivery system observing anti-inflammatory and anti COVID-19 characterizations in oleic acid triggered lung injury and in vitro COVID-19 experiment",
"author": "Hanafy",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "Int. J. Biol. Macromol.",
"key": "10.1016/j.biopha.2024.116131_bib114",
"volume": "198",
"year": "2022"
},
{
"DOI": "10.1080/08820139.2017.1371908",
"article-title": "Immunomodulatory activities of curcumin-stabilized silver nanoparticles: Efficacy as an antiretroviral therapeutic",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "833",
"issue": "8",
"journal-title": "Immunol. Investig.",
"key": "10.1016/j.biopha.2024.116131_bib115",
"volume": "46",
"year": "2017"
},
{
"DOI": "10.1016/j.biomaterials.2013.12.090",
"article-title": "Curcumin nanoformulations: a review of pharmaceutical properties and preclinical studies and clinical data related to cancer treatment",
"author": "Naksuriya",
"doi-asserted-by": "crossref",
"first-page": "3365",
"issue": "10",
"journal-title": "Biomaterials",
"key": "10.1016/j.biopha.2024.116131_bib116",
"volume": "35",
"year": "2014"
},
{
"DOI": "10.1039/D1FO03746C",
"article-title": "Nano-curcumin supplementation in critically ill patients with sepsis: a randomized clinical trial investigating the inflammatory biomarkers, oxidative stress indices, endothelial function, clinical outcomes and nutritional status",
"author": "Karimi",
"doi-asserted-by": "crossref",
"first-page": "6596",
"issue": "12",
"journal-title": "Food Funct.",
"key": "10.1016/j.biopha.2024.116131_bib117",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.eujim.2020.101122",
"article-title": "Effects of nanocurcumin on inflammatory factors and clinical outcomes in critically ill patients with sepsis: a pilot randomized clinical trial",
"author": "Karimi",
"doi-asserted-by": "crossref",
"journal-title": "Eur. J. Integr. Med.",
"key": "10.1016/j.biopha.2024.116131_bib118",
"volume": "36",
"year": "2020"
},
{
"DOI": "10.3390/polym10050541",
"article-title": "Oral delivery of curcumin polymeric nanoparticles ameliorates CCl₄-induced subacute hepatotoxicity in wistar rats",
"author": "Marslin",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Polymers (Basel)",
"key": "10.1016/j.biopha.2024.116131_bib119",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.3390/nu10070855",
"article-title": "Curcumin in liver diseases: a systematic review of the cellular mechanisms of oxidative stress and clinical perspective",
"author": "Farzaei",
"doi-asserted-by": "crossref",
"issue": "7",
"journal-title": "Nutrients",
"key": "10.1016/j.biopha.2024.116131_bib120",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1039/C5RA24032H",
"article-title": "Nanoincorporation of curcumin in polymer-glycerosomes and evaluation of their in vitro–in vivo suitability as pulmonary delivery systems",
"author": "Manca",
"doi-asserted-by": "crossref",
"first-page": "105149",
"issue": "127",
"journal-title": "RSC Adv.",
"key": "10.1016/j.biopha.2024.116131_bib121",
"volume": "5",
"year": "2015"
},
{
"DOI": "10.1016/j.ijpharm.2017.04.044",
"article-title": "Chitosan and hyaluronan coated liposomes for pulmonary administration of curcumin",
"author": "Manconi",
"doi-asserted-by": "crossref",
"first-page": "203",
"issue": "1",
"journal-title": "Int. J. Pharm.",
"key": "10.1016/j.biopha.2024.116131_bib122",
"volume": "525",
"year": "2017"
},
{
"DOI": "10.1111/1440-1681.12384",
"article-title": "Curcumin ameliorates asthmatic airway inflammation by activating nuclear factor-E2-related factor 2/haem oxygenase (HO)-1 signalling pathway",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "520",
"issue": "5",
"journal-title": "Clin. Exp. Pharmacol. Physiol.",
"key": "10.1016/j.biopha.2024.116131_bib123",
"volume": "42",
"year": "2015"
},
{
"DOI": "10.1016/j.colsurfb.2018.08.027",
"article-title": "Assessing the potential of liposomes loaded with curcumin as a therapeutic intervention in asthma",
"author": "Ng",
"doi-asserted-by": "crossref",
"first-page": "51",
"journal-title": "Colloids Surf. B: Biointerfaces",
"key": "10.1016/j.biopha.2024.116131_bib124",
"volume": "172",
"year": "2018"
},
{
"DOI": "10.1007/s10787-017-0395-3",
"article-title": "Immunomodulatory potential of nanocurcumin-based formulation",
"author": "Trivedi",
"doi-asserted-by": "crossref",
"first-page": "609",
"issue": "6",
"journal-title": "Inflammopharmacology",
"key": "10.1016/j.biopha.2024.116131_bib125",
"volume": "25",
"year": "2017"
},
{
"DOI": "10.1371/journal.pone.0185999",
"article-title": "Nanoparticle curcumin ameliorates experimental colitis via modulation of gut microbiota and induction of regulatory T cells",
"author": "Ohno",
"doi-asserted-by": "crossref",
"issue": "10",
"journal-title": "PloS One",
"key": "10.1016/j.biopha.2024.116131_bib126",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.3390/ani10050754",
"article-title": "Effect of dietary supplementation of biological curcumin nanoparticles on growth and carcass traits, antioxidant status, immunity and caecal microbiota of Japanese quails",
"author": "Reda",
"doi-asserted-by": "crossref",
"first-page": "754",
"issue": "5",
"journal-title": "Animals",
"key": "10.1016/j.biopha.2024.116131_bib127",
"volume": "10",
"year": "2020"
},
{
"article-title": "Microbial, immune and antioxidant responses of Nile tilapia with dietary nano-curcumin supplements under chronic low temperatures",
"author": "El Basuini",
"journal-title": "Aquac. Fish.",
"key": "10.1016/j.biopha.2024.116131_bib128",
"year": "2022"
},
{
"DOI": "10.1186/s13098-020-00532-4",
"article-title": "Aerobic exercise and nano-curcumin supplementation improve inflammation in elderly females with metabolic syndrome",
"author": "Osali",
"doi-asserted-by": "crossref",
"first-page": "26",
"issue": "1",
"journal-title": "Diabetol. Metab. Syndr.",
"key": "10.1016/j.biopha.2024.116131_bib129",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1186/s13104-022-06074-4",
"article-title": "The effects of nano-curcumin supplementation on adipokines levels in obese and overweight patients with migraine: a double blind clinical trial study",
"author": "Sedighiyan",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "BMC Res. Notes",
"key": "10.1016/j.biopha.2024.116131_bib130",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.1016/j.ctcp.2020.101256",
"article-title": "The effects of nano-curcumin supplementation on Th1/Th17 balance in migraine patients: A randomized controlled clinical trial",
"author": "Djalali",
"doi-asserted-by": "crossref",
"journal-title": "Complement. Ther. Clin. Pract.",
"key": "10.1016/j.biopha.2024.116131_bib131",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.3389/fnut.2022.1037861",
"article-title": "Evaluating the effects of curcumin nanomicelles on clinical outcome and cellular immune responses in critically ill sepsis patients: a randomized, double-blind, and placebo-controlled trial",
"author": "Karimi",
"doi-asserted-by": "crossref",
"journal-title": "Front. Nutr.",
"key": "10.1016/j.biopha.2024.116131_bib132",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1016/j.pharep.2018.05.008",
"article-title": "Nanocurcumin is a potential novel therapy for multiple sclerosis by influencing inflammatory mediators",
"author": "Dolati",
"doi-asserted-by": "crossref",
"first-page": "1158",
"journal-title": "Pharmacol. Rep.",
"key": "10.1016/j.biopha.2024.116131_bib133",
"volume": "70",
"year": "2018"
},
{
"DOI": "10.1002/jcp.26301",
"article-title": "Nanocurcumin restores aberrant miRNA expression profile in multiple sclerosis, randomized, double‐blind, placebo‐controlled trial",
"author": "Dolati",
"doi-asserted-by": "crossref",
"first-page": "5222",
"issue": "7",
"journal-title": "J. Cell. Physiol.",
"key": "10.1016/j.biopha.2024.116131_bib134",
"volume": "233",
"year": "2018"
},
{
"DOI": "10.1007/s00709-013-0516-9",
"article-title": "A comparative study of PNIPAM nanoparticles of curcumin, demethoxycurcumin, and bisdemethoxycurcumin and their effects on oxidative stress markers in experimental stroke",
"author": "Ahmad",
"doi-asserted-by": "crossref",
"first-page": "1327",
"journal-title": "Protoplasma",
"key": "10.1016/j.biopha.2024.116131_bib135",
"volume": "250",
"year": "2013"
},
{
"DOI": "10.1080/1061186X.2022.2141755",
"article-title": "Role of curcumin and its nanoformulations in the treatment of neurological diseases through the effects on stem cells",
"author": "Sabouni",
"doi-asserted-by": "crossref",
"first-page": "243",
"issue": "3",
"journal-title": "J. Drug Target.",
"key": "10.1016/j.biopha.2024.116131_bib136",
"volume": "31",
"year": "2023"
},
{
"DOI": "10.1007/s12010-022-04090-5",
"article-title": "Curcumin-loaded mesenchymal stem cell-derived exosomes efficiently attenuate proliferation and inflammatory response in rheumatoid arthritis fibroblast-like synoviocytes",
"author": "He",
"doi-asserted-by": "crossref",
"first-page": "51",
"issue": "1",
"journal-title": "Appl. Biochem Biotechnol.",
"key": "10.1016/j.biopha.2024.116131_bib137",
"volume": "195",
"year": "2023"
},
{
"DOI": "10.1007/s12035-010-8117-5",
"article-title": "Modulation of cholesterol, farnesylpyrophosphate, and geranylgeranylpyrophosphate in neuroblastoma SH-SY5Y-APP695 cells: impact on amyloid beta-protein production",
"author": "Hooff",
"doi-asserted-by": "crossref",
"first-page": "341",
"journal-title": "Mol. Neurobiol.",
"key": "10.1016/j.biopha.2024.116131_bib138",
"volume": "41",
"year": "2010"
},
{
"DOI": "10.1016/j.intimp.2021.108237",
"article-title": "Nanocurcumin supplementation ameliorates Behcet’s disease by modulating regulatory T cells: a randomized, double‐blind, placebo‐controlled trial",
"author": "Abbasian",
"doi-asserted-by": "crossref",
"journal-title": "Int. Immunopharmacol.",
"key": "10.1016/j.biopha.2024.116131_bib139",
"volume": "101",
"year": "2021"
},
{
"DOI": "10.3389/fonc.2013.00137",
"article-title": "Nano-curcumin inhibits proliferation of esophageal adenocarcinoma cells and enhances the T cell mediated immune response",
"author": "Milano",
"doi-asserted-by": "crossref",
"journal-title": "Front. Oncol.",
"key": "10.1016/j.biopha.2024.116131_bib140",
"volume": "3",
"year": "2013"
},
{
"DOI": "10.1177/2320206820949741",
"article-title": "Comparison of effects of curcumin and nano-curcumin on the survival of human-derived mesenchymal stem cells: an experimental study",
"author": "Hameeda",
"doi-asserted-by": "crossref",
"first-page": "148",
"issue": "2",
"journal-title": "J. Adv. Oral. Res.",
"key": "10.1016/j.biopha.2024.116131_bib141",
"volume": "11",
"year": "2020"
},
{
"article-title": "Efficacy of nanocurcumin with application of iontophoresis on inflammatory arthritis patients",
"author": "Nivetha",
"first-page": "825",
"issue": "2",
"journal-title": "Res. J. Pharm. Technol.",
"key": "10.1016/j.biopha.2024.116131_bib142",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.1021/jf204517k",
"article-title": "Curcumin bioavailability from enriched bread: the effect of microencapsulated ingredients",
"author": "Vitaglione",
"doi-asserted-by": "crossref",
"first-page": "3357",
"issue": "13",
"journal-title": "J. Agric. Food Chem.",
"key": "10.1016/j.biopha.2024.116131_bib143",
"volume": "60",
"year": "2012"
},
{
"DOI": "10.1016/j.arr.2021.101364",
"article-title": "Curcumin nanoformulations to combat aging-related diseases",
"author": "Mahjoob",
"doi-asserted-by": "crossref",
"journal-title": "Ageing Res. Rev.",
"key": "10.1016/j.biopha.2024.116131_bib144",
"volume": "69",
"year": "2021"
},
{
"DOI": "10.1007/s11033-017-4115-2",
"article-title": "Combination treatment with dendrosomal nanocurcumin and doxorubicin improves anticancer effects on breast cancer cells through modulating CXCR4/NF-κB/Smo regulatory network",
"author": "Mahjoub",
"doi-asserted-by": "crossref",
"first-page": "341",
"journal-title": "Mol. Biol. Rep.",
"key": "10.1016/j.biopha.2024.116131_bib145",
"volume": "44",
"year": "2017"
},
{
"DOI": "10.1038/s41467-020-19706-9",
"article-title": "Immune suppression in the early stage of COVID-19 disease",
"author": "Tian",
"doi-asserted-by": "crossref",
"first-page": "5859",
"issue": "1",
"journal-title": "Nat. Commun.",
"key": "10.1016/j.biopha.2024.116131_bib146",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-0305-6",
"article-title": "In the eye of the COVID-19 cytokine storm",
"author": "Vaninov",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Nat. Rev. Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib147",
"volume": "20",
"year": "2020"
},
{
"article-title": "Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic",
"author": "Prompetchara",
"first-page": "1",
"issue": "1",
"journal-title": "Asian Pac. J. Allergy Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib148",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.01445",
"article-title": "Potential treatments for COVID-19 related cytokine storm-beyond corticosteroids",
"author": "Miao",
"doi-asserted-by": "crossref",
"first-page": "1445",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib149",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/s41423-020-0401-3",
"article-title": "Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "541",
"issue": "5",
"journal-title": "Cell. Mol. Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib150",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.immuni.2020.04.023",
"article-title": "Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals",
"author": "Ni",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Immunity",
"key": "10.1016/j.biopha.2024.116131_bib151",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.181.8.5490",
"article-title": "T cell responses to whole SARS coronavirus in humans",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "5490",
"issue": "8",
"journal-title": "J. Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib152",
"volume": "181",
"year": "2008"
},
{
"DOI": "10.1038/s41577-020-0304-7",
"article-title": "Fighting COVID-19 exhausts T cells",
"author": "Moon",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Nat. Rev. Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib153",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2018.01545",
"article-title": "Regulatory T cells and acute lung injury: cytokines, uncontrolled inflammation, and therapeutic implications",
"author": "Lin",
"doi-asserted-by": "crossref",
"first-page": "1545",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib154",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1038/s41467-020-18854-2",
"article-title": "Two distinct immunopathological profiles in autopsy lungs of COVID-19",
"author": "Nienhold",
"doi-asserted-by": "crossref",
"first-page": "5086",
"issue": "1",
"journal-title": "Nat. Commun.",
"key": "10.1016/j.biopha.2024.116131_bib155",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-0901-9",
"article-title": "Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19",
"author": "Liao",
"doi-asserted-by": "crossref",
"first-page": "842",
"issue": "6",
"journal-title": "Nat. Med.",
"key": "10.1016/j.biopha.2024.116131_bib156",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1101/2020.02.12.945576",
"doi-asserted-by": "crossref",
"key": "10.1016/j.biopha.2024.116131_bib157",
"unstructured": "Zhou, Y., B. Fu, X. Zheng, Aberrant pathogenic GM-CSF+ T cells and inflammatory CD14+CD16+monocytes in severe pulmonary syndrome patients of a new coronavirus. bioRxiv 20.02. 2020."
},
{
"DOI": "10.1186/s13287-021-02165-4",
"article-title": "Mesenchymal stem cells derived from perinatal tissues for treatment of critically ill COVID-19-induced ARDS patients: a case series",
"author": "Hashemian",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "Stem Cell Res. Ther.",
"key": "10.1016/j.biopha.2024.116131_bib158",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2020.05.006",
"article-title": "Host-viral infection maps reveal signatures of severe COVID-19 patients",
"author": "Bost",
"doi-asserted-by": "crossref",
"issue": "7",
"journal-title": "Cell",
"key": "10.1016/j.biopha.2024.116131_bib159",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.03.037",
"article-title": "The pathogenesis and treatment of theCytokine Storm'in COVID-19",
"author": "Ye",
"doi-asserted-by": "crossref",
"first-page": "607",
"issue": "6",
"journal-title": "J. Infect.",
"key": "10.1016/j.biopha.2024.116131_bib160",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1038/329630a0",
"article-title": "Macrophage-induced angiogenesis is mediated by tumour necrosis factor-α",
"author": "Leibovich",
"doi-asserted-by": "crossref",
"first-page": "630",
"issue": "6140",
"journal-title": "Nature",
"key": "10.1016/j.biopha.2024.116131_bib161",
"volume": "329",
"year": "1987"
},
{
"DOI": "10.1172/JCI137244",
"article-title": "Clinical and immunological features of severe and moderate coronavirus disease 2019",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "2620",
"issue": "5",
"journal-title": "J. Clin. Investig.",
"key": "10.1016/j.biopha.2024.116131_bib162",
"volume": "130",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"article-title": "COVID-19: consider cytokine storm syndromes and immunosuppression",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "1033",
"issue": "10229",
"journal-title": "Lancet",
"key": "10.1016/j.biopha.2024.116131_bib163",
"volume": "395",
"year": "2020"
},
{
"article-title": "COVID-19 infection induces readily detectable morphological and inflammation-related phenotypic changes in peripheral blood monocytes, the severity of which correlate with patient outcome",
"author": "Zhang",
"journal-title": "MedRxiv",
"key": "10.1016/j.biopha.2024.116131_bib164",
"year": "2020"
},
{
"DOI": "10.3332/ecancer.2020.1022",
"article-title": "Associations between immune-suppressive and stimulating drugs and novel COVID-19—a systematic review of current evidence",
"author": "Russell",
"doi-asserted-by": "crossref",
"journal-title": "ecancermedicalscience",
"key": "10.1016/j.biopha.2024.116131_bib165",
"volume": "14",
"year": "2020"
},
{
"key": "10.1016/j.biopha.2024.116131_bib166",
"unstructured": "Li, H., Y. Wang, J. Xu, B. Cao, Potential antiviral therapeutics for 2019 Novel Coronavirus. Zhonghua jie he he hu xi za zhi= Zhonghua jiehe he huxi zazhi= Chinese journal of tuberculosis and respiratory diseases, 2020. 43: p. E002-E002."
},
{
"DOI": "10.1016/j.jmii.2020.03.005",
"article-title": "TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "368",
"issue": "3",
"journal-title": "J. Microbiol. Immunol. Infect.",
"key": "10.1016/j.biopha.2024.116131_bib167",
"volume": "53",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-0331-4",
"article-title": "Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages",
"author": "Merad",
"doi-asserted-by": "crossref",
"first-page": "355",
"issue": "6",
"journal-title": "Nat. Rev. Immunol.",
"key": "10.1016/j.biopha.2024.116131_bib168",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1515/cclm-2020-0198",
"article-title": "Laboratory abnormalities in patients with COVID-2019 infection",
"author": "Lippi",
"doi-asserted-by": "crossref",
"first-page": "1131",
"issue": "7",
"journal-title": "Clin. Chem. Lab. Med. (CCLM)",
"key": "10.1016/j.biopha.2024.116131_bib169",
"volume": "58",
"year": "2020"
},
{
"DOI": "10.5858/arpa.2020-0389-SA",
"article-title": "A comprehensive appraisal of laboratory biochemistry tests as major predictors of COVID-19 severity",
"author": "Aloisio",
"doi-asserted-by": "crossref",
"first-page": "1457",
"issue": "12",
"journal-title": "Arch. Pathol. Lab. Med.",
"key": "10.1016/j.biopha.2024.116131_bib170",
"volume": "144",
"year": "2020"
},
{
"DOI": "10.1038/s41421-020-00225-2",
"article-title": "The differential immune responses to COVID-19 in peripheral and lung revealed by single-cell RNA sequencing",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "73",
"issue": "1",
"journal-title": "Cell Discov.",
"key": "10.1016/j.biopha.2024.116131_bib171",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30627-9",
"article-title": "COVID-19 and Italy: what next?",
"author": "Remuzzi",
"doi-asserted-by": "crossref",
"first-page": "1225",
"issue": "10231",
"journal-title": "lancet",
"key": "10.1016/j.biopha.2024.116131_bib172",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30317-2",
"article-title": "Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury",
"author": "Russell",
"doi-asserted-by": "crossref",
"first-page": "473",
"issue": "10223",
"journal-title": "Lancet",
"key": "10.1016/j.biopha.2024.116131_bib173",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1188/17.CJON.240-249",
"doi-asserted-by": "crossref",
"key": "10.1016/j.biopha.2024.116131_bib174",
"unstructured": "King, T., Steroid-associated side effects: a symptom management update on multiple myeloma treatment. Number 2/April 2017, 2017. 21(2): p. 240–249."
},
{
"DOI": "10.1111/are.13223",
"article-title": "The efficacy of dietary curcumin on growth performance, lipid peroxidation and hepatic transcription factors in rainbow trout Oncorhynchus mykiss (Walbaum) reared under different stocking densities",
"author": "Akdemir",
"doi-asserted-by": "crossref",
"first-page": "4012",
"issue": "8",
"journal-title": "Aquac. Res.",
"key": "10.1016/j.biopha.2024.116131_bib175",
"volume": "48",
"year": "2017"
},
{
"DOI": "10.1021/jf011601s",
"article-title": "Structural identification of new curcumin dimers and their contribution to the antioxidant mechanism of curcumin",
"author": "Masuda",
"doi-asserted-by": "crossref",
"first-page": "2524",
"issue": "9",
"journal-title": "J. Agric. Food Chem.",
"key": "10.1016/j.biopha.2024.116131_bib176",
"volume": "50",
"year": "2002"
},
{
"DOI": "10.1021/jf990308d",
"article-title": "Antibacterial activity of turmeric oil: a byproduct from curcumin manufacture",
"author": "Negi",
"doi-asserted-by": "crossref",
"first-page": "4297",
"issue": "10",
"journal-title": "J. Agric. Food Chem.",
"key": "10.1016/j.biopha.2024.116131_bib177",
"volume": "47",
"year": "1999"
},
{
"DOI": "10.1016/j.brainres.2009.05.009",
"article-title": "Curcumin upregulates transcription factor Nrf2, HO-1 expression and protects rat brains against focal ischemia",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "133",
"journal-title": "Brain Res.",
"key": "10.1016/j.biopha.2024.116131_bib178",
"volume": "1282",
"year": "2009"
},
{
"DOI": "10.3390/molecules16064567",
"article-title": "Curcumin: an anti-inflammatory molecule from a curry spice on the path to cancer treatment",
"author": "Basnet",
"doi-asserted-by": "crossref",
"first-page": "4567",
"issue": "6",
"journal-title": "Molecules",
"key": "10.1016/j.biopha.2024.116131_bib179",
"volume": "16",
"year": "2011"
},
{
"DOI": "10.3390/toxins2010128",
"article-title": "Curcumin―the paradigm of a multi-target natural compound with applications in cancer prevention and treatment",
"author": "Teiten",
"doi-asserted-by": "crossref",
"first-page": "128",
"issue": "1",
"journal-title": "Toxins",
"key": "10.1016/j.biopha.2024.116131_bib180",
"volume": "2",
"year": "2010"
},
{
"DOI": "10.1186/1476-4598-10-12",
"article-title": "Curcumin: A review of anti-cancer properties and therapeutic activity in head and neck squamous cell carcinoma",
"author": "Wilken",
"doi-asserted-by": "crossref",
"first-page": "12",
"issue": "1",
"journal-title": "Mol. Cancer",
"key": "10.1016/j.biopha.2024.116131_bib181",
"volume": "10",
"year": "2011"
},
{
"DOI": "10.1016/j.antiviral.2017.03.014",
"article-title": "Curcumin inhibits Zika and chikungunya virus infection by inhibiting cell binding",
"author": "Mounce",
"doi-asserted-by": "crossref",
"first-page": "148",
"journal-title": "Antivir. Res.",
"key": "10.1016/j.biopha.2024.116131_bib182",
"volume": "142",
"year": "2017"
},
{
"DOI": "10.2174/2211738507666191210163408",
"article-title": "Antiviral action of curcumin encapsulated in nanoemulsion against four serotypes of dengue virus",
"author": "Nabila",
"doi-asserted-by": "crossref",
"first-page": "54",
"issue": "1",
"journal-title": "Pharm. Nanotechnol.",
"key": "10.1016/j.biopha.2024.116131_bib183",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s10637-015-0296-5",
"article-title": "Identification of a novel compound (β-sesquiphellandrene) from turmeric (Curcuma longa) with anticancer potential: comparison with curcumin",
"author": "Tyagi",
"doi-asserted-by": "crossref",
"first-page": "1175",
"issue": "6",
"journal-title": "Invest N. Drugs",
"key": "10.1016/j.biopha.2024.116131_bib184",
"volume": "33",
"year": "2015"
},
{
"DOI": "10.1002/ptr.7844",
"article-title": "Promising clinical outcomes of nano‐curcumin treatment as an adjunct therapy in hospitalized COVID‐19 patients: A randomized, double‐blinded, placebo‐controlled trial",
"author": "Sadeghizadeh",
"doi-asserted-by": "crossref",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib185",
"year": "2023"
},
{
"DOI": "10.1002/ptr.7004",
"article-title": "Oral nano‐curcumin formulation efficacy in management of mild to moderate hospitalized coronavirus disease‐19 patients: An open label nonrandomized clinical trial",
"author": "Saber‐Moghaddam",
"doi-asserted-by": "crossref",
"first-page": "2616",
"issue": "5",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib186",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1016/j.intimp.2020.107088",
"article-title": "Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients",
"author": "Valizadeh",
"doi-asserted-by": "crossref",
"journal-title": "Int. Immunopharmacol.",
"key": "10.1016/j.biopha.2024.116131_bib187",
"volume": "89",
"year": "2020"
},
{
"DOI": "10.1002/fsn3.2226",
"article-title": "Oral nano‐curcumin formulation efficacy in the management of mild to moderate outpatient COVID‐19: a randomized triple‐blind placebo‐controlled clinical trial",
"author": "Ahmadi",
"doi-asserted-by": "crossref",
"first-page": "4068",
"issue": "8",
"journal-title": "Food Sci. Nutr.",
"key": "10.1016/j.biopha.2024.116131_bib188",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7294",
"article-title": "A triple‐blind, placebo‐controlled, randomized clinical trial to evaluate the effect of curcumin‐containing nanomicelles on cellular immune responses subtypes and clinical outcome in COVID‐19 patients",
"author": "Hassaniazad",
"doi-asserted-by": "crossref",
"first-page": "6417",
"issue": "11",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib189",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7375",
"article-title": "Antiinflammatory potential of nano‐curcumin as an alternative therapeutic agent for the treatment of mild‐to‐moderate hospitalized COVID‐19 patients in a placebo‐controlled clinical trial",
"author": "Asadirad",
"doi-asserted-by": "crossref",
"first-page": "1023",
"issue": "2",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib190",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1016/j.lfs.2021.119437",
"article-title": "Nanocurcumin improves Treg cell responses in patients with mild and severe SARS-CoV2",
"author": "Tahmasebi",
"doi-asserted-by": "crossref",
"journal-title": "Life Sci.",
"key": "10.1016/j.biopha.2024.116131_bib191",
"volume": "276",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7374",
"article-title": "Effect of nanocurcumin supplementation on the severity of symptoms and length of hospital stay in patients with COVID‐19: a randomized double‐blind placebo‐controlled trial",
"author": "Honarkar Shafie",
"doi-asserted-by": "crossref",
"first-page": "1013",
"issue": "2",
"journal-title": "Phytother. Res.",
"key": "10.1016/j.biopha.2024.116131_bib192",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.3177/jnsv.67.249",
"article-title": "Newly developed highly bioavailable curcumin formulation, curcuRougeTM, reduces neutrophil/lymphocyte ratio in the elderly: a double-blind, placebo-controlled clinical trial",
"author": "Kishimoto",
"doi-asserted-by": "crossref",
"first-page": "249",
"issue": "4",
"journal-title": "J. Nutr. Sci. Vitaminol.",
"key": "10.1016/j.biopha.2024.116131_bib193",
"volume": "67",
"year": "2021"
},
{
"DOI": "10.3390/nu15071548",
"article-title": "Curcumin confers anti-inflammatory effects in adults who recovered from COVID-19 and were subsequently vaccinated: a randomized controlled trial",
"author": "Fessler",
"doi-asserted-by": "crossref",
"first-page": "1548",
"issue": "7",
"journal-title": "Nutrients",
"key": "10.1016/j.biopha.2024.116131_bib194",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1186/s13063-022-06375-w",
"article-title": "The efficacy of curcumin-piperine co-supplementation on clinical symptoms, duration, severity, and inflammatory factors in COVID-19 outpatients: a randomized double-blind, placebo-controlled trial",
"author": "Askari",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "Trials",
"key": "10.1016/j.biopha.2024.116131_bib195",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1111/jcmm.17337",
"article-title": "Effect of ArtemiC in patients with COVID‐19: a Phase II prospective study",
"author": "Hellou",
"doi-asserted-by": "crossref",
"first-page": "3281",
"issue": "11",
"journal-title": "J. Cell. Mol. Med.",
"key": "10.1016/j.biopha.2024.116131_bib196",
"volume": "26",
"year": "2022"
},
{
"article-title": "Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients",
"author": "Valizadeh",
"issue": "Pt B",
"journal-title": "Int Immunopharmacol.",
"key": "10.1016/j.biopha.2024.116131_bib197",
"volume": "89",
"year": "2020"
},
{
"DOI": "10.1002/fsn3.2226",
"article-title": "Oral nano-curcumin formulation efficacy in the management of mild to moderate outpatient COVID-19: A randomized triple-blind placebo-controlled clinical trial",
"author": "Ahmadi",
"doi-asserted-by": "crossref",
"first-page": "4068",
"issue": "8",
"journal-title": "Food Sci. Nutr.",
"key": "10.1016/j.biopha.2024.116131_bib198",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7294",
"article-title": "A triple-blind, placebo-controlled, randomized clinical trial to evaluate the effect of curcumin-containing nanomicelles on cellular immune responses subtypes and clinical outcome in COVID-19 patients",
"author": "Hassaniazad",
"doi-asserted-by": "crossref",
"first-page": "6417",
"issue": "11",
"journal-title": "Phytother. Res",
"key": "10.1016/j.biopha.2024.116131_bib199",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7004",
"article-title": "Oral nano-curcumin formulation efficacy in management of mild to moderate hospitalized coronavirus disease-19 patients: An open label nonrandomized clinical trial",
"author": "Saber-Moghaddam",
"doi-asserted-by": "crossref",
"journal-title": "Phytother. Res",
"key": "10.1016/j.biopha.2024.116131_bib200",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7375",
"article-title": "Antiinflammatory potential of nano-curcumin as an alternative therapeutic agent for the treatment of mild-to-moderate hospitalized COVID-19 patients in a placebo-controlled clinical trial",
"author": "Asadirad",
"doi-asserted-by": "crossref",
"first-page": "1023",
"issue": "2",
"journal-title": "Phytother. Res",
"key": "10.1016/j.biopha.2024.116131_bib201",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1002/jcp.30233",
"article-title": "Immunomodulatory effects of nanocurcumin on Th17 cell responses in mild and severe COVID-19 patients",
"author": "Tahmasebi",
"doi-asserted-by": "crossref",
"first-page": "5325",
"issue": "7",
"journal-title": "J. Cell Physiol.",
"key": "10.1016/j.biopha.2024.116131_bib202",
"volume": "236",
"year": "2021"
},
{
"DOI": "10.1016/j.ejphar.2022.175267",
"article-title": "Immunomodulatory role of Nanocurcumin in COVID-19 patients with dropped natural killer cells frequency and function",
"author": "Abbaspour-Aghdam",
"doi-asserted-by": "crossref",
"journal-title": "Eur. J. Pharm.",
"key": "10.1016/j.biopha.2024.116131_bib203",
"volume": "933",
"year": "2022"
}
],
"reference-count": 203,
"references-count": 203,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S075333222400012X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology",
"General Medicine"
],
"subtitle": [],
"title": "Immunoregulatory effects of nanocurcumin in inflammatory milieu: Focus on COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "171"
}