Prevalence of Micronutrient Deficiencies in Patients Hospitalized with COVID-19: An Observational Cohort Study
et al., Nutrients, doi:10.3390/nu14091862, Apr 2022
Prospective study of 57 consecutive hospitalized COVID-19 patients in Switzerland, showing lower risk of mortality/ICU admission with vitamin B9. Adjustments only considered age.
|
risk of death/ICU, 12.0% lower, OR 0.88, p = 0.02, adjusted per study, multivariable, RR approximated with OR, per standard deviation change.
|
|
risk of death/ICU, 98.3% lower, RR 0.02, p < 0.001, high vitamin B9 levels (≥7nmol/l) 0 of 54 (0.0%), low vitamin B9 levels (<7nmol/l) 3 of 3 (100.0%), NNT 1.0, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Voelkle et al., 30 Apr 2022, prospective, Switzerland, peer-reviewed, median age 67.0, 9 authors, study period 17 March, 2020 - 30 April, 2020.
Contact: schuetzph@gmail.com (corresponding author), manyola.voelkle@ksa.ch, claudia.gregoriano@ksa.ch, daniel.koch@ksa.ch, alexander.kutz@ksa.ch, beat.mueller@ksa.ch, anna.conen@ksa.ch, peter.neyer@ksa.ch, luca.bernasconi@ksa.ch.
Prevalence of Micronutrient Deficiencies in Patients Hospitalized with COVID-19: An Observational Cohort Study
Nutrients, doi:10.3390/nu14091862
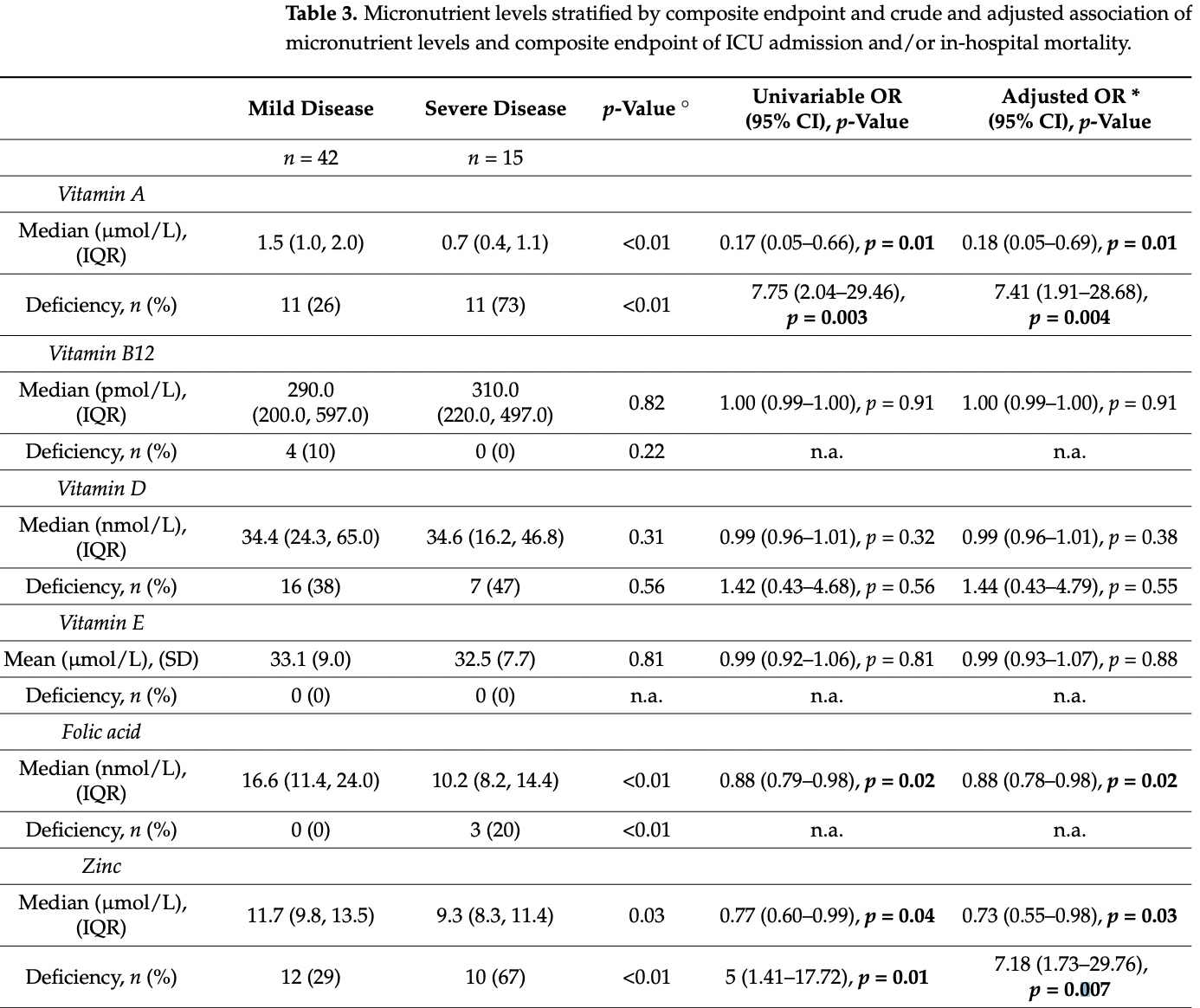
Background: A higher risk for severe clinical courses of coronavirus disease 2019 (COVID-19) has been linked to deficiencies of several micronutrients. We therefore studied the prevalence of deficiencies of eight different micronutrients in a cohort of hospitalized COVID-19-patients. Methods: We measured admission serum/plasma levels of vitamins A, B12, D, and E, as well as folic acid, zinc, selenium, and copper in 57 consecutively admitted adult patients with confirmed COVID-19 and analyzed prevalence of micronutrient deficiencies and correlations among micronutrient levels. Further, we studied associations of micronutrient levels with severe disease progression, a composite endpoint consisting of in-hospital mortality and/or need for intensive care unit (ICU) treatment with logistic regression. Results: Median age was 67.0 years (IQR 60.0, 74.2) and 60% (n = 34) were male. Overall, 79% (n = 45) of patients had at least one deficient micronutrient level and 33% (n = 19) had ≥3 deficiencies. Most prevalent deficiencies were found for selenium, vitamin D, vitamin A, and zinc (51%, 40%, 39%, and 39%, respectively). We found several correlations among micronutrients with correlation coefficients ranging from r = 0.27 to r = 0.42. The strongest associations with lower risk for severe COVID-19 disease progression (adjusted odds ratios) were found for higher levels of vitamin A (0.18, 95% CI 0.05-0.69, p = 0.01), zinc (0.73, 95% CI 0.55-0.98, p = 0.03), and folic acid (0.88, 95% CI 0.78-0.98, p = 0.02). Conclusions: We found a high prevalence of micronutrient deficiencies in mostly older patients hospitalized for COVID-19, particularly regarding selenium, vitamin D, vitamin A, and zinc. Several deficiencies were associated with a higher risk for more severe COVID-19 courses. Whether supplementation of micronutrients is useful for prevention of severe clinical courses or treatment of COVID-19 warrants further research.
References
Ahmad, Haskell, Raqib, Stephensen, Markers of innate immune function are associated with vitamin a stores in men, J. Nutr, doi:10.3945/jn.108.100198
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad. Med. J, doi:10.1136/postgradmedj-2020-138712
Beigmohammadi, Bitarafan, Abdollahi, Amoozadeh, Salahshour et al., The association between serum levels of micronutrients and the severity of disease in patients with COVID-19, Nutrition, doi:10.1016/j.nut.2021.111400
Berardicurti, Ruscitti, Ursini, D'andrea, Ciaffi et al., Mortality in tocilizumab-treated patients with COVID-19: A systematic review and meta-analysis, Clin. Exp. Rheumatol
Berger, Herter-Aeberli, Zimmermann, Spieldenner, Eggersdorfer, Strengthening the immunity of the Swiss population with micronutrients: A narrative review and call for action, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.03.012
Broman, Rantasarkka, Feuth, Valtonen, Waris et al., IL-6 and other biomarkers as predictors of severity in COVID-19, Ann. Med, doi:10.1080/07853890.2020.1840621
Calder, Carr, Gombart, Eggersdorfer, Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections, Nutrients, doi:10.3390/nu12041181
Calder, Feeding the immune system, Proc. Nutr. Soc, doi:10.1017/S0029665113001286
Chandra, Nutrition and the immune system from birth to old age, Eur. J. Clin. Nutr, doi:10.1038/sj.ejcn.1601492
Charlson, Szatrowski, Peterson, Gold, Validation of a combined comorbidity index, J. Clin. Epidemiol, doi:10.1016/0895-4356(94)90129-5
Chen, Mei, Xie, Yuan, Ma et al., Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs, Nutr. J, doi:10.1186/s12937-021-00744-y
Chen, Wu, Guo, Cao, Huang et al., Clinical and immunological features of severe and moderate coronavirus disease 2019, J. Clin. Investig, doi:10.1172/JCI137244
Conzade, Koenig, Heier, Schneider, Grill et al., Prevalence and Predictors of Subclinical Micronutrient Deficiency in German Older Adults: Results from the Population-Based KORA-Age Study, Nutrients
Coomes, Haghbayan, Interleukin-6 in COVID-19: A systematic review and meta-analysis, Rev. Med. Virol, doi:10.1002/rmv.2141
Elham, Azam, Azam, Mostafa, Nasrin et al., Serum vitamin D, calcium, and zinc levels in patients with COVID-19, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.03.040
Fang, Li, Yu, Wang, Zhang et al., Epidemiological, comorbidity factors with severity and prognosis of COVID-19: A systematic review and meta-analysis, Aging, doi:10.18632/aging.103579
Fromonot, Gette, Ben Lassoued, Gueant, Gueant-Rodriguez et al., Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19, Clin. Nutr, doi:10.1016/j.clnu.2021.04.042
Gammoh, Rink, Zinc in Infection and Inflammation, Nutrients, doi:10.3390/nu9060624
Gao, Ding, Dong, Zhang, Kursat Azkur et al., Risk factors for severe and critically ill COVID-19 patients: A review, Allergy, doi:10.1111/all.14657
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Gombart, The vitamin D-antimicrobial peptide pathway and its role in protection against infection, Future Microbiol, doi:10.2217/fmb.09.87
Greaves, Woollard, Hoad, Walmsley, Johnson et al., Laboratory medicine best practice guideline: Vitamins a, e and the carotenoids in blood, Clin. Biochem. Rev
Gregoriano, Koch, Haubitz, Conen, Fux et al., Characteristics, predictors and outcomes among 99 patients hospitalised with COVID-19 in a tertiary care centre in Switzerland: An observational analysis, Swiss Med. Wkly, doi:10.4414/smw.2020.20316
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.08.018
Jahromi, Moradi Tabriz, Togha, Ariyanfar, Ghorbani et al., The correlation between serum selenium, zinc, and COVID-19 severity: An observational study, BMC Infect. Dis, doi:10.1186/s12879-021-06617-3
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci. Rep, doi:10.1038/s41598-020-77093-z
Jaun, Boesing, Luthi-Corridori, Abig, Makhdoomi et al., High-dose vitamin D substitution in patients with COVID-19: Study protocol for a randomized, double-blind, placebo-controlled, multi-center study-VitCov Trial, Trials, doi:10.1186/s13063-022-06016-2
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with zinc deficiency, Int. J. Infect. Dis
Juma, Taabazuing, Montero-Odasso, Clinical Frailty Scale in an Acute Medicine Unit: A Simple Tool That Predicts Length of Stay, Can. Geriatr. J, doi:10.5770/cgj.19.196
Koekkoek, Hettinga, De Vries, Van Zanten, Micronutrient deficiencies in critical illness, Clin. Nutr, doi:10.1016/j.clnu.2021.05.003
Kondrup, Rasmussen, Hamberg, Stanga, Ad Hoc, Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials, Clin. Nutr, doi:10.1016/S0261-5614(02)00214-5
Laing, Petrovic, Lachat, De Boevre, Klingenberg et al., Course and Survival of COVID-19 Patients with Comorbidities in Relation to the Trace Element Status at Hospital Admission, Nutrients, doi:10.3390/nu13103304
Lin, Li, The Roles of Vitamin D and Its Analogs in Inflammatory Diseases, Curr. Top. Med. Chem
Liuzzi, Lichten, Rivera, Blanchard, Aydemir et al., Interleukin-6 regulates the zinc transporter Zip14 in liver and contributes to the hypozincemia of the acute-phase response, Proc. Natl. Acad. Sci, doi:10.1073/pnas.0502257102
Mucida, Park, Kim, Turovskaya, Scott et al., Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid, Science, doi:10.1126/science.1145697
Munns, Shaw, Kiely, Specker, Thacher et al., Global Consensus Recommendations on Prevention and Management of Nutritional Rickets, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2015-2175
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J. Med. Virol, doi:10.1002/jmv.26360
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Sadeghi, Tahmasebi, Mahmood, Kuznetsova, Valizadeh et al., Th17 and Treg cells function in SARS-CoV2 patients compared with healthy controls, J. Cell Physiol, doi:10.1002/jcp.30047
Sarohan, Kizil, Inkaya, Mahmud, Akram et al., A novel hypothesis for COVID-19 pathogenesis: Retinol depletion and retinoid signaling disorder, Cell Signal, doi:10.1016/j.cellsig.2021.110121
Schroeder, Cousins, Interleukin 6 regulates metallothionein gene expression and zinc metabolism in hepatocyte monolayer cultures, Proc. Natl. Acad. Sci, doi:10.1073/pnas.87.8.3137
Schuetz, Gregoriano, Keller, Supplementation of the population during the COVID-19 pandemic with vitamins and micronutrients-How much evidence is needed?, Swiss Med Wkly, doi:10.4414/smw.2021.20522
Schupbach, Wegmuller, Berguerand, Bui, Herter-Aeberli, Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland, Eur. J. Nutr, doi:10.1007/s00394-015-1079-7
Stephensen, Vitamin A, infection, and immune function, Annu. Rev. Nutr, doi:10.1146/annurev.nutr.21.1.167
Tepasse, Vollenberg, Fobker, Kabar, Schmidt et al., Vitamin A Plasma Levels in COVID-19 Patients: A Prospective Multicenter Study and Hypothesis, Nutrients, doi:10.3390/nu13072173
Tomasa-Irriguible, Bielsa-Berrocal, Bordeje-Laguna, Tural-Llacher, Barallat et al., Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave, Metabolites, doi:10.3390/metabo11090565
Wintergerst, Maggini, Hornig, Immune-enhancing role of vitamin C and zinc and effect on clinical conditions, Ann. Nutr. Metab, doi:10.1159/000090495
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Zhang, Sun, Yan, Yi, Yue, Correlation of serum vitamin A, D, and E with recurrent respiratory infection in children, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_201909_19033
Zhang, Taylor, Bennett, Saad, Rayman, Association between regional selenium status and reported outcome of COVID-19 cases in China, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqaa095
DOI record:
{
"DOI": "10.3390/nu14091862",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14091862",
"abstract": "<jats:p>Background: A higher risk for severe clinical courses of coronavirus disease 2019 (COVID-19) has been linked to deficiencies of several micronutrients. We therefore studied the prevalence of deficiencies of eight different micronutrients in a cohort of hospitalized COVID-19-patients. Methods: We measured admission serum/plasma levels of vitamins A, B12, D, and E, as well as folic acid, zinc, selenium, and copper in 57 consecutively admitted adult patients with confirmed COVID-19 and analyzed prevalence of micronutrient deficiencies and correlations among micronutrient levels. Further, we studied associations of micronutrient levels with severe disease progression, a composite endpoint consisting of in-hospital mortality and/or need for intensive care unit (ICU) treatment with logistic regression. Results: Median age was 67.0 years (IQR 60.0, 74.2) and 60% (n = 34) were male. Overall, 79% (n = 45) of patients had at least one deficient micronutrient level and 33% (n = 19) had ≥3 deficiencies. Most prevalent deficiencies were found for selenium, vitamin D, vitamin A, and zinc (51%, 40%, 39%, and 39%, respectively). We found several correlations among micronutrients with correlation coefficients ranging from r = 0.27 to r = 0.42. The strongest associations with lower risk for severe COVID-19 disease progression (adjusted odds ratios) were found for higher levels of vitamin A (0.18, 95% CI 0.05–0.69, p = 0.01), zinc (0.73, 95% CI 0.55–0.98, p = 0.03), and folic acid (0.88, 95% CI 0.78–0.98, p = 0.02). Conclusions: We found a high prevalence of micronutrient deficiencies in mostly older patients hospitalized for COVID-19, particularly regarding selenium, vitamin D, vitamin A, and zinc. Several deficiencies were associated with a higher risk for more severe COVID-19 courses. Whether supplementation of micronutrients is useful for prevention of severe clinical courses or treatment of COVID-19 warrants further research.</jats:p>",
"alternative-id": [
"nu14091862"
],
"author": [
{
"affiliation": [],
"family": "Voelkle",
"given": "Manyola",
"sequence": "first"
},
{
"affiliation": [],
"family": "Gregoriano",
"given": "Claudia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8682-9578",
"affiliation": [],
"authenticated-orcid": false,
"family": "Neyer",
"given": "Peter",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4660-5924",
"affiliation": [],
"authenticated-orcid": false,
"family": "Koch",
"given": "Daniel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7549-5648",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kutz",
"given": "Alexander",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bernasconi",
"given": "Luca",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5216-4109",
"affiliation": [],
"authenticated-orcid": false,
"family": "Conen",
"given": "Anna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mueller",
"given": "Beat",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6400-4949",
"affiliation": [],
"authenticated-orcid": false,
"family": "Schuetz",
"given": "Philipp",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
5,
2
]
],
"date-time": "2022-05-02T11:08:58Z",
"timestamp": 1651489738000
},
"deposited": {
"date-parts": [
[
2022,
5,
2
]
],
"date-time": "2022-05-02T11:32:24Z",
"timestamp": 1651491144000
},
"funder": [
{
"award": [
"n.a."
],
"name": "Research Council KSA, Kantonsspital Aarau"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
15
]
],
"date-time": "2024-03-15T20:27:40Z",
"timestamp": 1710534460864
},
"is-referenced-by-count": 23,
"issue": "9",
"issued": {
"date-parts": [
[
2022,
4,
29
]
]
},
"journal-issue": {
"issue": "9",
"published-online": {
"date-parts": [
[
2022,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
29
]
],
"date-time": "2022-04-29T00:00:00Z",
"timestamp": 1651190400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/9/1862/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1862",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
4,
29
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
29
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref1",
"unstructured": "WHO Coronavirus Disease (COVID-19) Dashboardhttps://covid19.who.int/"
},
{
"DOI": "10.1001/jama.2020.2648",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1111/all.14657",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.18632/aging.103579",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.3390/nu9121276",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1038/sj.ejcn.1601492",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.clnesp.2021.03.012",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3390/nu12041181",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1146/annurev.nutr.21.1.167",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1159/000090495",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3390/nu9060624",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.2217/fmb.09.87",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.2174/1568026615666150915111557",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1186/s12937-021-00744-y",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.3390/metabo11090565",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.3390/nu13103304",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1186/s12879-021-06617-3",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.4414/smw.2021.20522",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"key": "ref22",
"series-title": "Vitamin D Deficiency: Evidence, Safety, and Recommendations for the Swiss Population",
"year": "2012"
},
{
"DOI": "10.1007/s00394-015-1079-7",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.4414/smw.2020.20316",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"key": "ref25",
"unstructured": "Clinical Management of Severe Acute Respiratory Infection When Novel Coronovirus (nCov) Infection Is Suspected; Interim Guidancehttps://apps.who.int/iris/handle/10665/330893"
},
{
"DOI": "10.1016/0895-4356(94)90129-5",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.5770/cgj.19.196",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/S0261-5614(02)00214-5",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"article-title": "Laboratory medicine best practice guideline: Vitamins a, e and the carotenoids in blood",
"author": "Greaves",
"first-page": "81",
"journal-title": "Clin. Biochem. Rev.",
"key": "ref29",
"volume": "35",
"year": "2014"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1002/jmv.26360",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1016/j.nut.2021.111400",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1016/j.clnesp.2021.03.040",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1186/s13063-022-06016-2",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1093/ajcn/nqaa095",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.3390/nu13072173",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1016/j.cellsig.2021.110121",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1126/science.1145697",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1002/jcp.30047",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1172/JCI137244",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.3945/jn.108.100198",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1002/rmv.2141",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1080/07853890.2020.1840621",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"article-title": "Mortality in tocilizumab-treated patients with COVID-19: A systematic review and meta-analysis",
"author": "Berardicurti",
"first-page": "1247",
"journal-title": "Clin. Exp. Rheumatol.",
"key": "ref46",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1001/jama.2021.11330",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1016/j.clnu.2021.04.042",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1073/pnas.0502257102",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1073/pnas.87.8.3137",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1017/S0029665113001286",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.26355/eurrev_201909_19033",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1016/j.clnu.2021.05.003",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1210/jc.2015-2175",
"doi-asserted-by": "publisher",
"key": "ref54"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/14/9/1862"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Prevalence of Micronutrient Deficiencies in Patients Hospitalized with COVID-19: An Observational Cohort Study",
"type": "journal-article",
"volume": "14"
}
voelkle