Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave
et al., Metabolites, doi:10.3390/metabo11090565, Oct 2020 (preprint)
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000019 from 42 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 120 hospitalized patients in Spain showing zinc deficiency associated with higher ICU admission.
|
risk of mechanical ventilation, 49.3% lower, RR 0.51, p = 0.06, high zinc levels 7 of 31 (22.6%), low zinc levels 49 of 89 (55.1%), NNT 3.1, adjusted per study, inverted to make RR<1 favor high zinc levels, odds ratio converted to relative risk, ≥84 mcg/dL, multivariate logistic regression.
|
|
risk of ICU admission, 52.0% lower, RR 0.48, p = 0.02, high zinc levels 9 of 31 (29.0%), low zinc levels 55 of 89 (61.8%), NNT 3.1, adjusted per study, inverted to make RR<1 favor high zinc levels, odds ratio converted to relative risk, ≥84 mcg/dL, multivariate logistic regression, final model.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Tomasa-Irriguible et al., 26 Oct 2020, retrospective, Spain, peer-reviewed, 7 authors, study period March 2020 - May 2020.
Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave
Metabolites, doi:10.3390/metabo11090565
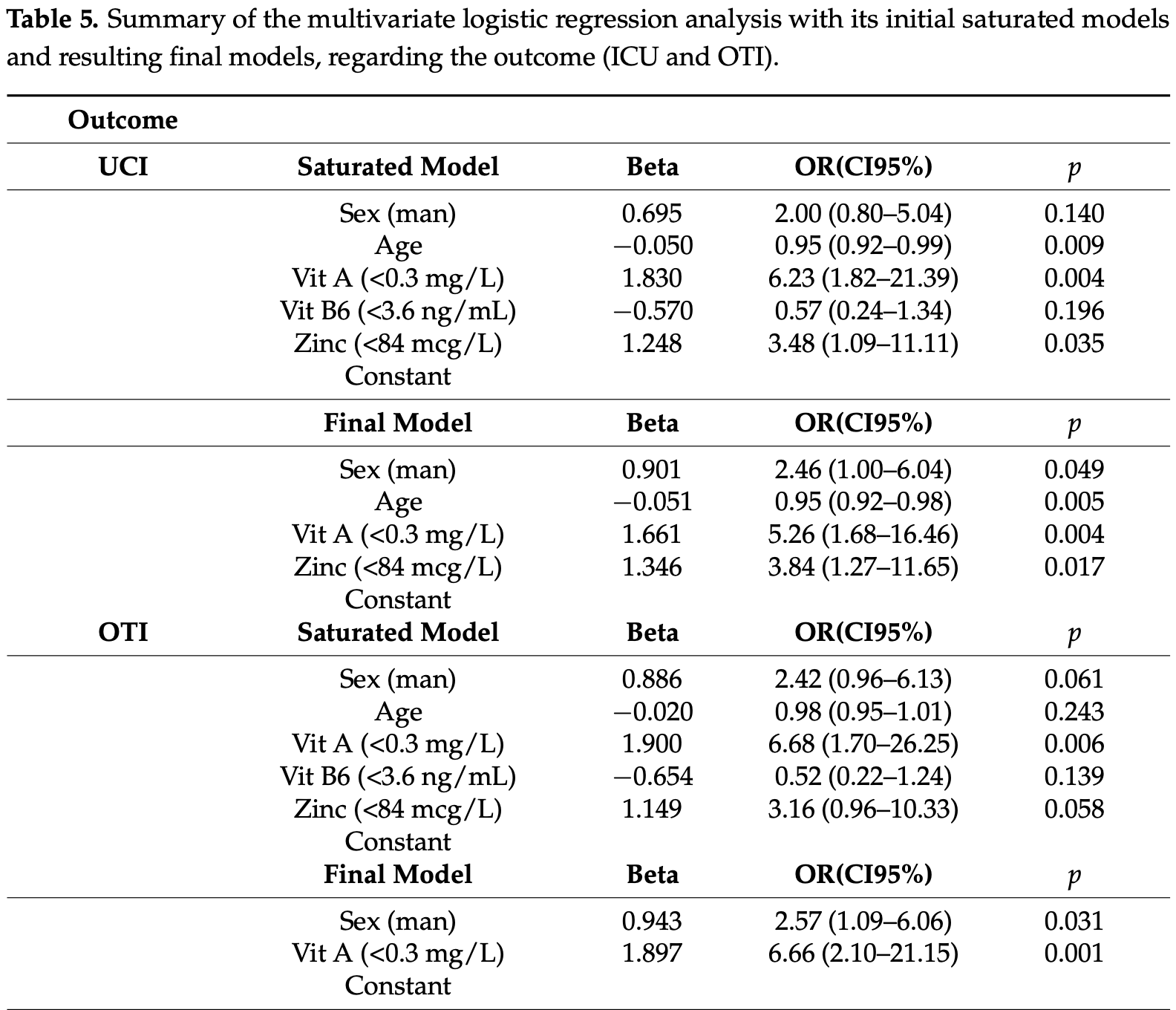
We report an observational study performed between March and May 2020 in a Spanish university hospital during the SARS-CoV-2 pandemic. The main objective was to analyse the association between the levels of micronutrients in severe COVID-19 patients and their outcome. Adult patients with a positive polymerase-chain-reaction (PCR) for SARS-CoV-2 in the nasopharyngeal swab or in tracheal aspirate culture in the case of intubation were included. Micronutrient data were obtained from plasma analysis of a standard nutritional assessment performed within the first 24 h of hospital admission. Vitamins A, B 6 , C and E were analysed with HPLC methods; 25-OH-vitamin D by immunoassay and zinc by colorimetric measurements. One hundred and twenty patients were included. We found that 74.2% patients had low levels of zinc (normal levels >84 µg/dL) with a mean value of 63.5 (SD 13.5); 71.7% patients had low levels of vitamin A (normal levels >0.3 mg/L) with a mean value of 0.17 (SD 0.06); 42.5% patients had low levels of vitamin B 6 (normal levels >3.6 ng/mL) with a mean value of 2.2 (SD 0.9); 100% patients had low levels of vitamin C (normal levels >0.4 mg/dL) with a mean value of 0.14 (SD 0.05); 74.3% patients had low values of vitamin D (normal levels >20 ng/mL) with mean value of 11.4 (SD 4.3); but only 5.8% of patients had low levels of vitamin E (normal levels >5 mg/L) with a mean value of 3.95 (SD 0.87). The variables associated with the need for ICU admission were low levels of zinc (standard error 0.566, 95% CI 0.086 to 0.790, p = 0.017), low levels of vitamin A (standard error 0.582, 95% CI 0.061 to 0.594, p = 0.004), age over 65 (standard error 0.018, 95% CI 0.917 to 0.985, p = 0.005) and male gender (standard error 0.458, 95% CI 1.004 to 6.040, p = 0.049). The only variable that was independently associated with the need for orotracheal intubation was low levels of vitamin A (standard error 0.58, 95% CI 0.042 to 0.405, p = 0.000). Conclusions: Low levels of vitamin A and zinc are associated with a greater need for admission to the ICU and orotracheal intubation. Patients older than 65 years had higher mortality. Randomized clinical trials are needed to examine whether micronutrient supplementation could be beneficial as an adjunctive treatment in COVID-19.
Informed Consent Statement: Patient consent was waived due to the retrospective analyses of data obtained from an anonymized data base obtained from the Information Systems of the Center.
Conflicts of Interest: The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
Amrein, Oudemans-Van Straaten, Berger, Vitamin therapy in critically ill patients: Focus on thiamine, vitamin C, and vitamin D, Intensive Care Med, doi:10.1007/s00134-018-5107-y
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study, Nutrients, doi:10.3390/nu12113377
Arabi, Gordon, Derde, Nichol, Murthy et al., Lopinavir-ritonavir and hydroxychloroquine for critically ill patients with COVID-19: REMAP-CAP randomized controlled trial, Intensive Care Med, doi:10.1007/s00134-021-06448-5
Beigmohammadi, Bitarafan, Hoseindokht, Abdollahi, Amoozadeh et al., and E supplementation on improvement and mortality rate in ICU patients with Coronavirus-19: A structured summary of a study protocol for a randomized controlled trial, Trials, doi:10.1186/s13063-020-04547-0
Berry, Hesketh, Power, Hypönen, Vitamin D status has a linear association with seasonal infections and lung function in British adults, Br. J. Nutr, doi:10.1017/S0007114511001991
Carlucci, Ahuja, Petrilli, Rajagopalan, Jones et al., Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients, J. Med. Microbiol, doi:10.1099/jmm.0.001250
Carr, A new clinical trial to test high-dose vitamin C in patients with COVID-19, Crit. Care, doi:10.1186/s13054-020-02851-4
Carr, Rosengrave, Bayer, Chambers, Mehrtens et al., Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes, Crit. Care, doi:10.1186/s13054-017-1891-y
Casaer, Bellomo, Micronutrient deficiency in critical illness: An invisible foe?, Intensive Care Med
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Choi, Jeong, Lee, Association between EGFR mutation and ageing, history of pneumonia and gastroesophageal reflux disease among patients with advanced lung cancer, Eur. J. Cancer, doi:10.1016/j.ejca.2019.09.010
De Melo, Homem-De-Mello, High-dose intravenous vitamin C may help in cytokine storm in severe SARS-CoV-2 infection, Crit. Care, doi:10.1186/s13054-020-03228-3
De Pascale, Vallecoccia, Schiattarella, Di Gravio, Cutuli et al., Clinical and microbiological outcome in septic patients with extremely low 25-hydroxyvitamin D levels at initiation of critical care, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2015.12.015
Domingo, Mur, Mateo, Gutierrez, Pomar et al., Association between Administration of IL-6 Antagonists and Mortality among Patients Hospitalized for COVID-19: A Meta-analysis, JAMA
Duncan, Talwar, Mcmillan, Stefanowicz, O'reilly, Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements, Am. J. Clin. Nutr
Fiorino, Gallo, Zippi, Sabbatani, Manfredi et al., Cytokine storm in aged people with CoV-2: Possible role of vitamins as therapy or preventive strategy, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01669-y
Force, Ranieri, Rubenfeld, Thompson, Ferguson et al., Acute Respiratory Distress Syndrome, JAMA, doi:10.1001/jama.2012.5669
Galmés, Serra, Palou, Current state of evidence: Influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic framework, Nutrients, doi:10.3390/nu12092738
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Gonçalves, Bertrand, Ke, Comets, De Lamballerie et al., Timing of antiviral treatment initiation is critical to reduce SARS-CoV-2 viral load, CPT: Pharmacometrics Syst. Pharmacol, doi:10.1002/psp4.12543
Gonçalves, Gonçalves, Guarnieri, Risegato, Guimarães et al., Association Between Low Zinc Levels and Severity of Acute Respiratory Distress Syndrome by New Coronavirus SARS-CoV-2, Nutr. Clin. Pract, doi:10.1002/ncp.10612
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with zinc deficiency, Int. J. Infect. Dis
Jovic, Ali, Ibrahim, Jessop, Tarassoli et al., Could Vitamins Help in the Fight Against COVID-19?, Nutrients, doi:10.3390/nu12092550
Karlsen, Sommerfelt, Klomstad, Andersen, Strand et al., Intestinal and Systemic Immune Responses to an Oral Cholera Toxoid B Subunit Whole-Cell Vaccine Administered during Zinc Supplementation, Infect. Immun, doi:10.1128/IAI.71.7.3909-3913.2003
Lee, Lin, Lei, Chang, Lee et al., Does Vitamin D Deficiency Affect the Immunogenic Responses to Influenza Vaccination? A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu10040409
Li, Wu, Li, Liang, Tse et al., Revealing the targets and mechanisms of vitamin A in the treatment of COVID-19, Aging, doi:10.18632/aging.103888
Ling, Broad, Murphy, Pappachan, Pardesi-Newton et al., High-Dose Cholecalciferol Booster Therapy is Associated with a Reduced Risk of Mortality in Patients with COVID-19: A Cross-Sectional Multi-Centre Observational Study, Nutrients, doi:10.3390/nu12123799
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium Deficiency Is Associated with Mortality Risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients with Moderate to Severe COVID-19, JAMA, doi:10.1001/jama.2020.26848
Suarca, Arhana, Suandi, The Role of Zinc Supplementation in Humoral Immune Response to Hepatitis B Vaccination in Infants: A Double-Blind Randomized Placebo-Controlled Trial
Tepasse, Vollenberg, Fobker, Kabar, Schmidt et al., Vitamin A Plasma Levels in COVID-19 Patients: A Prospective Multicenter Study and Hypothesis, Nutrients, doi:10.3390/nu13072173
The, Group, Dexamethasone in hospitalized patients with COVID-19-Preliminary report, N. Engl. J. Med, doi:10.1056/NEJMoa2021436
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.0369
Velthuis, Van Den Worml, Sims, Baric, Snijder et al., Zn 2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog, doi:10.1371/journal.ppat.1001176
Xu, Baylink, Chen, Reeves, Xiao et al., The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19, J. Transl. Med, doi:10.1186/s12967-020-02488-5
Yasui, Yasui, Suzuki, Saitou, Yamamoto et al., Analysis of the predictive factors for a critical illness of COVID-19 during treatment-Relationship between serum zinc level and critical illness of COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.09.008
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., Effects of Vitamin D on COVID-19 Infection and Prognosis: A Systematic Review, Risk Manag. Healthc. Policy, doi:10.2147/RMHP.S291584
Zhang, Yang, Chen, Liao, Deng et al., Vitamin A deficiency in critically ill children with sepsis, Crit. Care, doi:10.1186/s13054-019-2548-9
Zhou, Huang, Xiao, Huang, Fan, Protecting Chinese healthcare workers while combating the 2019 novel coronavirus, Infect. Control Hosp. Epidemiol, doi:10.1017/ice.2020.60
DOI record:
{
"DOI": "10.3390/metabo11090565",
"ISSN": [
"2218-1989"
],
"URL": "http://dx.doi.org/10.3390/metabo11090565",
"abstract": "<jats:p>We report an observational study performed between March and May 2020 in a Spanish university hospital during the SARS-CoV-2 pandemic. The main objective was to analyse the association between the levels of micronutrients in severe COVID-19 patients and their outcome. Adult patients with a positive polymerase-chain-reaction (PCR) for SARS-CoV-2 in the nasopharyngeal swab or in tracheal aspirate culture in the case of intubation were included. Micronutrient data were obtained from plasma analysis of a standard nutritional assessment performed within the first 24 h of hospital admission. Vitamins A, B6, C and E were analysed with HPLC methods; 25-OH-vitamin D by immunoassay and zinc by colorimetric measurements. One hundred and twenty patients were included. We found that 74.2% patients had low levels of zinc (normal levels >84 µg/dL) with a mean value of 63.5 (SD 13.5); 71.7% patients had low levels of vitamin A (normal levels >0.3 mg/L) with a mean value of 0.17 (SD 0.06); 42.5% patients had low levels of vitamin B6 (normal levels >3.6 ng/mL) with a mean value of 2.2 (SD 0.9); 100% patients had low levels of vitamin C (normal levels >0.4 mg/dL) with a mean value of 0.14 (SD 0.05); 74.3% patients had low values of vitamin D (normal levels >20 ng/mL) with mean value of 11.4 (SD 4.3); but only 5.8% of patients had low levels of vitamin E (normal levels >5 mg/L) with a mean value of 3.95 (SD 0.87). The variables associated with the need for ICU admission were low levels of zinc (standard error 0.566, 95% CI 0.086 to 0.790, p = 0.017), low levels of vitamin A (standard error 0.582, 95% CI 0.061 to 0.594, p = 0.004), age over 65 (standard error 0.018, 95% CI 0.917 to 0.985, p = 0.005) and male gender (standard error 0.458, 95% CI 1.004 to 6.040, p = 0.049). The only variable that was independently associated with the need for orotracheal intubation was low levels of vitamin A (standard error 0.58, 95% CI 0.042 to 0.405, p = 0.000). Conclusions: Low levels of vitamin A and zinc are associated with a greater need for admission to the ICU and orotracheal intubation. Patients older than 65 years had higher mortality. Randomized clinical trials are needed to examine whether micronutrient supplementation could be beneficial as an adjunctive treatment in COVID-19.</jats:p>",
"alternative-id": [
"metabo11090565"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-8033-8527",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tomasa-Irriguible",
"given": "Teresa-Maria",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bielsa-Berrocal",
"given": "Lara",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4129-7309",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bordejé-Laguna",
"given": "Luisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tural-Llàcher",
"given": "Cristina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3493-5958",
"affiliation": [],
"authenticated-orcid": false,
"family": "Barallat",
"given": "Jaume",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8306-5798",
"affiliation": [],
"authenticated-orcid": false,
"family": "Manresa-Domínguez",
"given": "Josep-Maria",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9865-7427",
"affiliation": [],
"authenticated-orcid": false,
"family": "Torán-Monserrat",
"given": "Pere",
"sequence": "additional"
}
],
"container-title": "Metabolites",
"container-title-short": "Metabolites",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
8,
25
]
],
"date-time": "2021-08-25T02:12:22Z",
"timestamp": 1629857542000
},
"deposited": {
"date-parts": [
[
2021,
8,
26
]
],
"date-time": "2021-08-26T03:27:43Z",
"timestamp": 1629948463000
},
"indexed": {
"date-parts": [
[
2024,
3,
15
]
],
"date-time": "2024-03-15T20:27:36Z",
"timestamp": 1710534456440
},
"is-referenced-by-count": 25,
"issue": "9",
"issued": {
"date-parts": [
[
2021,
8,
24
]
]
},
"journal-issue": {
"issue": "9",
"published-online": {
"date-parts": [
[
2021,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
24
]
],
"date-time": "2021-08-24T00:00:00Z",
"timestamp": 1629763200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2218-1989/11/9/565/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "565",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
8,
24
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
24
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref1",
"series-title": "WHO Coronavirus Disease (COVID-19) Dashboard",
"year": "2021"
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1002/psp4.12543",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1007/s00134-021-06448-5",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1017/ice.2020.60",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1186/s12967-020-02488-5",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.3390/nu12092550",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1007/s40520-020-01669-y",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1186/s13063-020-04547-0",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1017/S0007114511001991",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3390/nu10040409",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"key": "ref13",
"unstructured": "The Role of Zinc Supplementation in Humoral Immune Response to Hepatitis B Vaccination in Infants: A Double-Blind Randomized Placebo-Controlled Trialhttps://paediatricaindonesiana.org/index.php/paediatrica-indonesiana/article/view/632"
},
{
"DOI": "10.1128/IAI.71.7.3909-3913.2003",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.2147/RMHP.S291584",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/j.ijid.2020.09.008",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.3390/nu12072098",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.3390/nu12123799",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1099/jmm.0.001250",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.3390/nu12092738",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1186/s13054-019-2548-9",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1007/s00134-019-05678-y",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/j.cmi.2015.12.015",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1186/s13054-017-1891-y",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.18632/aging.103888",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1016/j.ejca.2019.09.010",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1007/s00134-018-5107-y",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1186/s13054-020-02851-4",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1186/s13054-020-03228-3",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1056/NEJMoa2021436",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1001/jama.2021.11330",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.3945/ajcn.111.023812",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1002/ncp.10612",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.3390/nu13072173",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1001/jama.2012.5669",
"doi-asserted-by": "publisher",
"key": "ref42"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2218-1989/11/9/565"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Molecular Biology",
"Biochemistry",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave",
"type": "journal-article",
"volume": "11"
}
tomasairriguible
