25 Hydroxyvitamin D Serum Concentration and COVID-19 Severity and Outcome—A Retrospective Survey in a Romanian Hospital
et al., Nutrients, doi:10.3390/nu15051227, Feb 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 2,342 hospitalized COVID-19 patients in Romania with vitamin D levels measured on admission day, showing lower risk of mortality and severe/critical cases with vitamin D levels ≥ 20ng/mL.
This is the 160th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
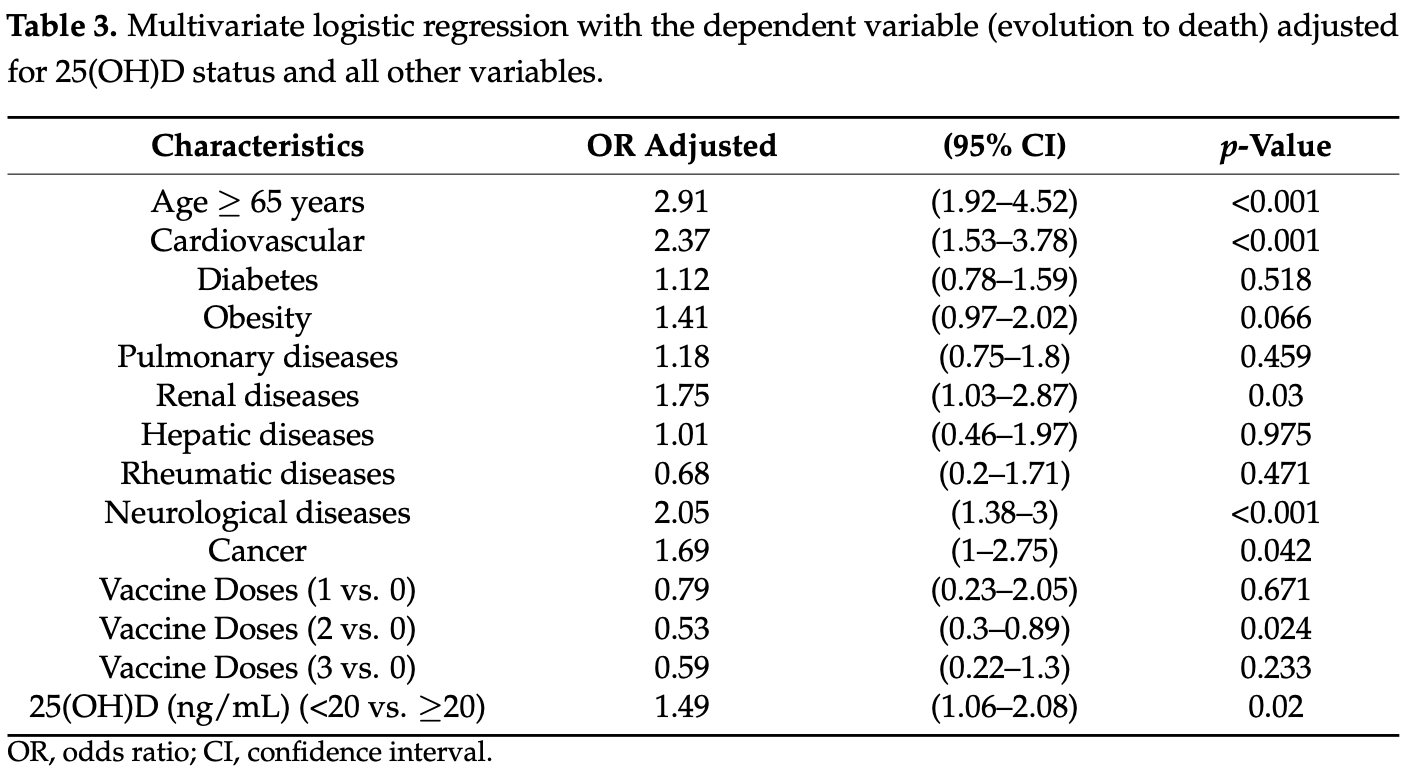
risk of death, 30.6% lower, RR 0.69, p = 0.02, high D levels (≥20ng/mL) 61 of 1,148 (5.3%), low D levels (<20ng/mL) 118 of 1,194 (9.9%), adjusted per study, inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, multivariable.
|
|
risk of severe case, 10.9% lower, RR 0.89, p = 0.02, high D levels (≥20ng/mL) 432 of 1,148 (37.6%), low D levels (<20ng/mL) 560 of 1,194 (46.9%), NNT 11, adjusted per study, inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, severe/critical case, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Topan et al., 28 Feb 2023, retrospective, Romania, peer-reviewed, survey, 6 authors, study period April 2020 - May 2022.
Contact: mihaela.lupse@yahoo.com (corresponding author).
25 Hydroxyvitamin D Serum Concentration and COVID-19 Severity and Outcome—A Retrospective Survey in a Romanian Hospital
Nutrients, doi:10.3390/nu15051227
Interest in the immunomodulatory function of vitamin D has grown since the COVID-19 pandemic started. Our study investigated the possible association between vitamin D deficiency and COVID-19 severity, intensive care needs, and mortality in patients hospitalized with COVID-19. A prospective cohort study was performed on 2342 COVID-19 hospitalized patients between April 2020 and May 2022 in a Romanian tertiary hospital for infectious diseases. A multivariate generalized linear model for binary data was fit with dependent variables: severe/critical form of COVID-19, intensive care need, and fatal outcome as a function of vitamin D deficiency, controlling for age, comorbidities, and vaccination status. More than half of the patients (50.9%) were classified with vitamin D deficiency based on a serum concentration of less than 20 ng/mL. There was a negative association between vitamin D and age. Vitamin D-deficient patients presented with more cardiovascular, neurological, and pulmonary diseases, as well as diabetes, and cancer. In multivariate logistic regression models, vitamin D-deficient patients had higher odds of severe/critical forms of COVID-19 [OR = 1.23 (95% CI 1.03-1.47), p = 0.023] and higher odds of death [OR = 1.49 (95% CI 1.06-2.08), p = 0.02]. Vitamin D deficiency was associated with disease severity and death outcome in hospitalized COVID-19 patients.
Supplementary Materials: The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/nu15051227/s1, Table S1 : Patients characteristics according to deficient, insufficient, and sufficient 25(OH)D; Table S2 : Multivariate logistic regression with dependent variable severe/critical form of COVID-19 adjusted for 25(OH)D (deficient, insufficient, and sufficient) and all the other variables; Table S3 : Multivariate logistic regression with dependent variable (evolution to death) adjusted for 25(OH)D (deficient, insufficient, and sufficient) and all the other variables; Table S4 : Multivariate logistic regression with dependent variable evolution to intensive care need adjusted for 25(OH)D (deficient, insufficient, and sufficient) and all the other variables; Figure S1 : Smoothing spline graphical representation of the relationship between 25(OH)D as a continuous variable and the log odds of severe/critical form in the multiple logistic regression model adjusted for Age ≥ 65 years, cardiovascular, diabetes, obesity, pulmonary diseases, renal diseases, hepatic diseases, rheumatic diseases, neurological diseases, cancer, vaccine doses; Figure S2 Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflict of interest.
References
Ahmad, Arora, Khan, Mohsin, Mohan et al., Vitamin D and its therapeutic relevance in pulmonary diseases, J. Nutr. Biochem, doi:10.1016/j.jnutbio.2020.108571
Amrein, Scherkl, Hoffmann, Neuwersch-Sommeregger, Köstenberger et al., deficiency 2.0: An update on the current status worldwide, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0558-y
Aranow, Vitamin D and the immune system, J. Investig. Med, doi:10.2310/JIM.0b013e31821b8755
Argano, Mallaci Bocchio, Natoli, Scibetta, Lo Monaco et al., Protective Effect of Vitamin D Supplementation on COVID-19-Related Intensive Care Hospitalization and Mortality: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis, Pharmaceuticals, doi:10.3390/ph16010130
Avdeeva, Suplotova, Pigarova, Rozhinskaya, Troshina, Vitamin D deficiency in Russia: The first results of a registered, non-interventional study of the frequency of vitamin D deficiency and insufficiency in various geographic regions of the country, Probl. Endokrinol, doi:10.14341/probl12736
Baeke, Takiishi, Korf, Gysemans, Mathieu et al., Modulator of the immune system, Curr. Opin. Pharmacol, doi:10.1016/j.coph.2010.04.001
Bennouar, Cherif, Kessira, Bennouar, Abdi, Vitamin D deficiency and low serum calcium as predictors of poor prognosis in patients with severe COVID-19, J. Am. Coll. Nutr, doi:10.1080/07315724.2020.1856013
Bikle, Vitamin D metabolism, mechanism of action, and clinical applications, Chem. Biol, doi:10.1016/j.chembiol.2013.12.016
Bouillon, Manousaki, Rosen, Trajanoska, Rivadeneira et al., The health effects of vitamin D supplementation: Evidence from human studies, Nat. Rev. Endocrinol, doi:10.1038/s41574-021-00593-z
Buckley, Guyatt, Fink, Cannon, Grossman et al., American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis, Arthritis Rheumatol, doi:10.1002/art.40137
Cashman, Dowling, Škrabáková, Gonzalez-Gross, Valtueña et al., Vitamin D deficiency in Europe:pandemic?, Am. J. Clin. Nutr, doi:10.3945/ajcn.115.120873
Castillo, Entrenas Costa, Vaquero Barrios, Alcalá Díaz, López Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid. Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Cereda, Bogliolo, Lobascio, Barichella, Zecchinelli et al., Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy, Nutrition, doi:10.1016/j.nut.2020.111055
Chen, Mei, Xie, Yuan, Ma et al., Low 25(OH)D concentration do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs, Nutr. J, doi:10.1186/s12937-021-00744-y
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front. Public Health, doi:10.3389/fpubh.2021.736665
Chirita-Emandi, Socolov, Haivas, Calapis, Gheorghiu et al., Vitamin D Status: A Different Story in the Very Young versus the Very Old Romanian Patients, PLoS ONE, doi:10.1371/journal.pone.0128010
Cianferotti, Bertoldo, Bischoff-Ferrari, Bruyere, Cooper et al., Vitamin D supplementation in the prevention and management of major chronic diseases not related to mineral homeostasis in adults: Research for evidence and a scientific statement from the European society for clinical and economic aspects of osteoporosis and osteoarthritis (ESCEO), Endocrine
Core, R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing
Daly, Gagnon, Lu, Magliano, Dunstan et al., Prevalence of vitamin D deficiency and its determinants in Australian adults aged 25 years and older: A national, population-based study, Clin. Endocrinol, doi:10.1111/j.1365-2265.2011.04320.x
De La Guía-Galipienso, Martínez-Ferran, Vallecillo, Lavie, Sanchis-Gomar et al., Vitamin D and cardiovascular health, Clin. Nutr, doi:10.1016/j.clnu.2020.12.025
De Smet, De Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality, Am. J. Clin. Pathol, doi:10.1093/ajcp/aqaa252
Dissanayake, De Silva, Sumanatilleke, De Silva, Gamage et al., Prognostic and Therapeutic Role of Vitamin D in COVID-19: Systematic Review and Meta-analysis, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgab892
Ferrari, Locatelli, Briguglio, Lombardi, Is there a link between vitamin D status, SARS-CoV-2 infection risk and COVID-19 severity?, Cell Biochem. Funct, doi:10.1002/cbf.3597
Food, Authority, Scientific opinion on dietary reference values for vitamin D, EFSA J
Galus, Popoviciu, Babes, Vidican, Zaha et al., Vitamin D Implications and Effect of Supplementation in Endocrine Disorders: Autoimmune Thyroid Disorders (Hashimoto's Disease and Grave's Disease), Diabetes Mellitus and Obesity, Medicina, doi:10.3390/medicina58020194
Garland, Gorham, Mohr, Garland, Vitamin D for cancer prevention: Global perspective, Ann. Epidemiol, doi:10.1016/j.annepidem.2009.03.021
Giovannucci, The epidemiology of vitamin D and cancer incidence and mortality: A review (United States), Cancer Causes Control, doi:10.1007/s10552-004-1661-4
Harrison, Buckley, Rivera-Caravaca, Zhang, Lip, Cardiovascular risk factors, cardiovascular disease, and COVID-19: An umbrella review of systematic reviews, Eur. Heart J. Qual. Care Clin. Outcomes, doi:10.1093/ehjqcco/qcab029
Holick, The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention, Rev. Endocr. Metab. Disord, doi:10.1007/s11154-017-9424-1
Hosseini, El Abd, Ducharme, Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134
Hut, Georgescu, Voidăzan, Andrejkovits, Negrea et al., Low Serum Vitamin D in COVID-19 Patients Is Not Related to Inflammatory Markers and Patients' Outcomes-A Single-Center Experience and a Brief Review of the Literature, Nutrients, doi:10.3390/nu14101998
Infante, Buoso, Pieri, Lupisella, Nuccetelli et al., Low Vitamin D Status at Admission as a Risk Factor for Poor Survival in Hospitalized Patients With COVID-19: An Italian Retrospective Study, J. Am. Nutr. Assoc, doi:10.1080/07315724.2021.1877580
Kim, The Role of Vitamin D in Thyroid Diseases, Int. J. Mol. Sci, doi:10.3390/ijms18091949
Kupisz-Urba Ńska, Płudowski, Marcinowska-Suchowierska, Vitamin D Deficiency in Older Patients-Problems of Sarcopenia, Drug Interactions, Management in Deficiency, Nutrients, doi:10.3390/nu13041247
Lips, Cashman, Lamberg-Allardt, Bischoff-Ferrari, Obermayer-Pietsch et al., Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: A position statement of the European Calcified Tissue Society, Eur. J. Endocrinol, doi:10.1530/EJE-18-0736
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS ONE, doi:10.1371/journal.pone.0239799
Mahmood, Levy, Vasan, Wang, The Framingham Heart Study and the epidemiology of cardiovascular disease: A historical perspective, Lancet, doi:10.1016/S0140-6736(13)61752-3
Martineau, Cantorna, Vitamin D for COVID-19: Where are we now?, Nat. Rev. Immunol, doi:10.1038/s41577-022-00765-6
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J. Med. Virol
Niculescu, Capatina, Dusceac, Caragheorgheopol, Ghemigian et al., Seasonal variation of serum 25(OH)D concentration in Romania, Arch Osteoporos, doi:10.1007/s11657-017-0407-3
Pereira-Santos, Costa, Assis, Santos, Santos, Obesity and vitamin D deficiency: A systematic review and meta-analysis, Obes. Rev, doi:10.1111/obr.12239
Pike, Meyer, Lee, Onal, Benkusky, The vitamin D receptor: Contemporary genomic approaches reveal new basic and translational insights, J. Clin. Investig, doi:10.1172/JCI88887
Pál, Ungvári, Benyó, Várbíró, Role of Vitamin D Deficiency in the Pathogenesis of Cardiovascular and Cerebrovascular Diseases, Nutrients, doi:10.3390/nu15020334
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Scragg, Sowers, Bell, Serum 25-hydroxyvitamin D, Ethnicity, and Blood Pressure in the Third National Health and Nutrition Examination Survey, Am. J. Hypertens, doi:10.1016/j.amjhyper.2007.01.017
Seidu, Gillies, Zaccardi, Kunutsor, Hartmann-Boyce et al., The impact of obesity on severe disease and mortality in people with SARS-CoV-2: A systematic review and meta-analysis, Endocrinol. Diabetes Metab, doi:10.1002/edm2.176
Seneviratne, Wijerathne, Yasawardene, Somawardana, COVID-19 in cancer patients, Trans. R. Soc. Trop. Med. Hyg, doi:10.1093/trstmh/trac015
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal, J. Heart Lung Transplant, doi:10.1016/j.healun.2020.03.012
Thompson, Natarajan, Irving, Rowley, Griggs et al., Effectiveness of a Third Dose of mRNA Vaccines Against COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance-VISION Network, 10 States, MMWR Morb. Mortal Wkly. Rep
Urashima, Segawa, Okazaki, Kurihara, Wada et al., Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren, Am. J. Clin. Nutr, doi:10.3945/ajcn.2009.29094
Virtanen, Nurmi, Aro, Bertone-Johnson, Hyppönen et al., Vitamin D supplementation and prevention of cardiovascular disease and cancer in the Finnish Vitamin D Trial: A randomized controlled trial, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqab419
Vranić, Mikolašević, Milić, Vitamin, Deficiency: Consequence or Cause of Obesity?, Medicina, doi:10.3390/medicina55090541
Wang, Pencina, Booth, Jacques, Ingelsson et al., Vitamin D Deficiency and Risk of Cardiovascular Disease, Circulation, doi:10.1161/CIRCULATIONAHA.107.706127
Witte, Byrom, Gierula, Paton, Jamil et al., Effects of Vitamin D on Cardiac Function in Patients With Chronic HF: The VINDICATE Study, J. Am. Coll. Cardiol, doi:10.1016/j.jacc.2016.03.508
DOI record:
{
"DOI": "10.3390/nu15051227",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu15051227",
"abstract": "<jats:p>Interest in the immunomodulatory function of vitamin D has grown since the COVID-19 pandemic started. Our study investigated the possible association between vitamin D deficiency and COVID-19 severity, intensive care needs, and mortality in patients hospitalized with COVID-19. A prospective cohort study was performed on 2342 COVID-19 hospitalized patients between April 2020 and May 2022 in a Romanian tertiary hospital for infectious diseases. A multivariate generalized linear model for binary data was fit with dependent variables: severe/critical form of COVID-19, intensive care need, and fatal outcome as a function of vitamin D deficiency, controlling for age, comorbidities, and vaccination status. More than half of the patients (50.9%) were classified with vitamin D deficiency based on a serum concentration of less than 20 ng/mL. There was a negative association between vitamin D and age. Vitamin D-deficient patients presented with more cardiovascular, neurological, and pulmonary diseases, as well as diabetes, and cancer. In multivariate logistic regression models, vitamin D-deficient patients had higher odds of severe/critical forms of COVID-19 [OR = 1.23 (95% CI 1.03–1.47), p = 0.023] and higher odds of death [OR = 1.49 (95% CI 1.06–2.08), p = 0.02]. Vitamin D deficiency was associated with disease severity and death outcome in hospitalized COVID-19 patients.</jats:p>",
"alternative-id": [
"nu15051227"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-3339-9711",
"affiliation": [
{
"name": "Department of Infectious Diseases, “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
},
{
"name": "The Clinical Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"authenticated-orcid": false,
"family": "Topan",
"given": "Adriana",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases, “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
},
{
"name": "The Clinical Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"family": "Lupse",
"given": "Mihaela",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Clinical Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"family": "Calin",
"given": "Mihai",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Clinical Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"family": "Jianu",
"given": "Cristian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4218-8622",
"affiliation": [
{
"name": "Department of Medical Informatics and Biostatistics, “Iuliu Hatieganu” University of Medicine and Pharmacy, 400349 Cluj-Napoca, Romania"
}
],
"authenticated-orcid": false,
"family": "Leucuta",
"given": "Daniel-Corneliu",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases, “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
},
{
"name": "The Clinical Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"family": "Briciu",
"given": "Violeta",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
1
]
],
"date-time": "2023-03-01T06:36:09Z",
"timestamp": 1677652569000
},
"deposited": {
"date-parts": [
[
2023,
3,
2
]
],
"date-time": "2023-03-02T07:15:37Z",
"timestamp": 1677741337000
},
"funder": [
{
"award": [
"40PFE/30.12.2021"
],
"name": "Increasing the Performance of Scientific Research, Supporting Excellence in Medical Research and Innovation, PROGRES"
}
],
"indexed": {
"date-parts": [
[
2023,
3,
3
]
],
"date-time": "2023-03-03T05:33:54Z",
"timestamp": 1677821634022
},
"is-referenced-by-count": 0,
"issue": "5",
"issued": {
"date-parts": [
[
2023,
2,
28
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2023,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
2,
28
]
],
"date-time": "2023-02-28T00:00:00Z",
"timestamp": 1677542400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/15/5/1227/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1227",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
2,
28
]
]
},
"published-online": {
"date-parts": [
[
2023,
2,
28
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "World Health Organization (2023, January 22). Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/."
},
{
"key": "ref_2",
"unstructured": "World Health Organization (2023, February 01). Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---25-january-2023."
},
{
"key": "ref_3",
"unstructured": "World Health Organization (2023, February 01). Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-therapeutics-2023.1."
},
{
"key": "ref_4",
"unstructured": "UK Health Security Agency (2022, December 03). COVID-19 Vaccine Surveillance Report, Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1050721/Vaccine-surveillance-report-week-4.pdf."
},
{
"DOI": "10.15585/mmwr.mm7104e3",
"article-title": "Effectiveness of a Third Dose of mRNA Vaccines Against COVID-19–Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance—VISION Network, 10 States, August 2021–January 2022",
"author": "Thompson",
"doi-asserted-by": "crossref",
"first-page": "139",
"journal-title": "MMWR Morb. Mortal Wkly. Rep.",
"key": "ref_5",
"volume": "71",
"year": "2022"
},
{
"article-title": "Cardiovascular risk factors, cardiovascular disease, and COVID-19: An umbrella review of systematic reviews",
"author": "Harrison",
"first-page": "330",
"journal-title": "Eur. Heart J. Qual. Care Clin. Outcomes",
"key": "ref_6",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1093/trstmh/trac015",
"article-title": "COVID-19 in cancer patients",
"author": "Seneviratne",
"doi-asserted-by": "crossref",
"first-page": "767",
"journal-title": "Trans. R. Soc. Trop. Med. Hyg.",
"key": "ref_7",
"volume": "116",
"year": "2022"
},
{
"article-title": "The impact of obesity on severe disease and mortality in people with SARS-CoV-2: A systematic review and meta-analysis",
"author": "Seidu",
"first-page": "e00176",
"journal-title": "Endocrinol. Diabetes Metab.",
"key": "ref_8",
"volume": "4",
"year": "2020"
},
{
"key": "ref_9",
"unstructured": "(2023, February 01). Our World in Data. Available online: https://ourworldindata.org/mortality-risk-covid."
},
{
"DOI": "10.1038/s41574-021-00593-z",
"article-title": "The health effects of vitamin D supplementation: Evidence from human studies",
"author": "Bouillon",
"doi-asserted-by": "crossref",
"first-page": "96",
"journal-title": "Nat. Rev. Endocrinol.",
"key": "ref_10",
"volume": "18",
"year": "2022"
},
{
"DOI": "10.1016/j.chembiol.2013.12.016",
"article-title": "Vitamin D metabolism, mechanism of action, and clinical applications",
"author": "Bikle",
"doi-asserted-by": "crossref",
"first-page": "319",
"journal-title": "Chem. Biol.",
"key": "ref_11",
"volume": "21",
"year": "2014"
},
{
"DOI": "10.1007/s11154-017-9424-1",
"article-title": "The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "153",
"journal-title": "Rev. Endocr. Metab. Disord.",
"key": "ref_12",
"volume": "18",
"year": "2017"
},
{
"key": "ref_13",
"unstructured": "European Food Safety Authority EEFS (2016). Scientific opinion on dietary reference values for vitamin D. EFSA J., 14, 4547."
},
{
"DOI": "10.1007/s12020-017-1290-9",
"article-title": "Vitamin D supplementation in the prevention and management of major chronic diseases not related to mineral homeostasis in adults: Research for evidence and a scientific statement from the European society for clinical and economic aspects of osteoporosis and osteoarthritis (ESCEO)",
"author": "Cianferotti",
"doi-asserted-by": "crossref",
"first-page": "245",
"journal-title": "Endocrine",
"key": "ref_14",
"volume": "56",
"year": "2017"
},
{
"DOI": "10.1172/JCI88887",
"article-title": "The vitamin D receptor: Contemporary genomic approaches reveal new basic and translational insights",
"author": "Pike",
"doi-asserted-by": "crossref",
"first-page": "1146",
"journal-title": "J. Clin. Investig.",
"key": "ref_15",
"volume": "127",
"year": "2017"
},
{
"DOI": "10.2310/JIM.0b013e31821b8755",
"article-title": "Vitamin D and the immune system",
"author": "Aranow",
"doi-asserted-by": "crossref",
"first-page": "881",
"journal-title": "J. Investig. Med.",
"key": "ref_16",
"volume": "59",
"year": "2011"
},
{
"DOI": "10.1016/j.coph.2010.04.001",
"article-title": "Vitamin D: Modulator of the immune system",
"author": "Baeke",
"doi-asserted-by": "crossref",
"first-page": "482",
"journal-title": "Curr. Opin. Pharmacol.",
"key": "ref_17",
"volume": "10",
"year": "2010"
},
{
"DOI": "10.1038/s41577-022-00765-6",
"article-title": "Vitamin D for COVID-19: Where are we now?",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "529",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_18",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1016/j.healun.2020.03.012",
"article-title": "COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal",
"author": "Siddiqi",
"doi-asserted-by": "crossref",
"first-page": "405",
"journal-title": "J. Heart Lung Transplant.",
"key": "ref_19",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.3945/ajcn.2009.29094",
"article-title": "Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren",
"author": "Urashima",
"doi-asserted-by": "crossref",
"first-page": "1255",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_20",
"volume": "91",
"year": "2010"
},
{
"key": "ref_21",
"unstructured": "(2022, February 01). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online: https://www.who.int/publications/i/item/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19)."
},
{
"key": "ref_22",
"unstructured": "(2023, February 02). International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available online: https://icd.who.int/browse10/2016/en#/."
},
{
"key": "ref_23",
"unstructured": "R Core Team (2013). R: A Language and Environment for Statistical Computing, R Foundation for Statistical Computing. Available online: http://www.R-project.org/."
},
{
"DOI": "10.1002/cbf.3597",
"article-title": "Is there a link between vitamin D status, SARS-CoV-2 infection risk and COVID-19 severity?",
"author": "Ferrari",
"doi-asserted-by": "crossref",
"first-page": "35",
"journal-title": "Cell Biochem. Funct.",
"key": "ref_24",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26360",
"article-title": "Vitamin D insufficiency as a potential culprit in critical COVID-19 patients",
"author": "Munshi",
"doi-asserted-by": "crossref",
"first-page": "733",
"journal-title": "J. Med. Virol.",
"key": "ref_25",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.3389/fpubh.2021.736665",
"article-title": "Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes",
"author": "Chiodini",
"doi-asserted-by": "crossref",
"first-page": "736665",
"journal-title": "Front. Public Health",
"key": "ref_26",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study",
"author": "Bouillon",
"doi-asserted-by": "crossref",
"first-page": "105751",
"journal-title": "J. Steroid. Biochem. Mol. Biol.",
"key": "ref_27",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1016/j.nut.2020.111055",
"article-title": "Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy",
"author": "Cereda",
"doi-asserted-by": "crossref",
"first-page": "111055",
"journal-title": "Nutrition",
"key": "ref_28",
"volume": "82",
"year": "2021"
},
{
"DOI": "10.1186/s12937-021-00744-y",
"article-title": "Low 25(OH)D concentration do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "89",
"journal-title": "Nutr. J.",
"key": "ref_29",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab892",
"article-title": "Prognostic and Therapeutic Role of Vitamin D in COVID-19: Systematic Review and Meta-analysis",
"author": "Dissanayake",
"doi-asserted-by": "crossref",
"first-page": "1484",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_30",
"volume": "107",
"year": "2022"
},
{
"DOI": "10.3390/nu14102134",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Hosseini, B., El Abd, A., and Ducharme, F.M. (2022). Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis. Nutrients, 14."
},
{
"DOI": "10.3390/ph16010130",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Argano, C., Mallaci Bocchio, R., Natoli, G., Scibetta, S., Lo Monaco, M., and Corrao, S. (2023). Protective Effect of Vitamin D Supplementation on COVID-19-Related Intensive Care Hospitalization and Mortality: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis. Pharmaceuticals, 16."
},
{
"DOI": "10.3945/ajcn.115.120873",
"article-title": "Vitamin D deficiency in Europe:pandemic?",
"author": "Cashman",
"doi-asserted-by": "crossref",
"first-page": "1033",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_33",
"volume": "103",
"year": "2016"
},
{
"DOI": "10.1038/s41430-020-0558-y",
"article-title": "Vitamin D deficiency 2.0: An update on the current status worldwide",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "1498",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "ref_34",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1111/j.1365-2265.2011.04320.x",
"article-title": "Prevalence of vitamin D deficiency and its determinants in Australian adults aged 25 years and older: A national, population-based study",
"author": "Daly",
"doi-asserted-by": "crossref",
"first-page": "26",
"journal-title": "Clin. Endocrinol.",
"key": "ref_35",
"volume": "77",
"year": "2012"
},
{
"DOI": "10.1371/journal.pone.0128010",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "Chirita-Emandi, A., Socolov, D., Haivas, C., Calapiș, A., Gheorghiu, C., and Puiu, M. (2015). Vitamin D Status: A Different Story in the Very Young versus the Very Old Romanian Patients. PLoS ONE, 10."
},
{
"DOI": "10.1007/s11657-017-0407-3",
"article-title": "Seasonal variation of serum 25(OH)D concentration in Romania",
"author": "Niculescu",
"doi-asserted-by": "crossref",
"first-page": "113",
"journal-title": "Arch Osteoporos",
"key": "ref_37",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1530/EJE-18-0736",
"article-title": "Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: A position statement of the European Calcified Tissue Society",
"author": "Lips",
"doi-asserted-by": "crossref",
"first-page": "P23",
"journal-title": "Eur. J. Endocrinol.",
"key": "ref_38",
"volume": "1",
"year": "2019"
},
{
"DOI": "10.14341/probl12736",
"article-title": "Vitamin D deficiency in Russia: The first results of a registered, non-interventional study of the frequency of vitamin D deficiency and insufficiency in various geographic regions of the country",
"author": "Avdeeva",
"doi-asserted-by": "crossref",
"first-page": "84",
"journal-title": "Probl. Endokrinol.",
"key": "ref_39",
"volume": "67",
"year": "2021"
},
{
"DOI": "10.3390/nu13041247",
"doi-asserted-by": "crossref",
"key": "ref_40",
"unstructured": "Kupisz-Urbańska, M., Płudowski, P., and Marcinowska-Suchowierska, E. (2021). Vitamin D Deficiency in Older Patients-Problems of Sarcopenia, Drug Interactions, Management in Deficiency. Nutrients, 13."
},
{
"DOI": "10.1016/j.clnu.2020.12.025",
"article-title": "Vitamin D and cardiovascular health",
"author": "Vallecillo",
"doi-asserted-by": "crossref",
"first-page": "2946",
"journal-title": "Clin. Nutr.",
"key": "ref_41",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1016/j.amjhyper.2007.01.017",
"article-title": "Serum 25-hydroxyvitamin D, Ethnicity, and Blood Pressure in the Third National Health and Nutrition Examination Survey",
"author": "Scragg",
"doi-asserted-by": "crossref",
"first-page": "713",
"journal-title": "Am. J. Hypertens.",
"key": "ref_42",
"volume": "20",
"year": "2007"
},
{
"DOI": "10.1161/CIRCULATIONAHA.107.706127",
"article-title": "Vitamin D Deficiency and Risk of Cardiovascular Disease",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "503",
"journal-title": "Circulation",
"key": "ref_43",
"volume": "117",
"year": "2008"
},
{
"DOI": "10.1016/S0140-6736(13)61752-3",
"article-title": "The Framingham Heart Study and the epidemiology of cardiovascular disease: A historical perspective",
"author": "Mahmood",
"doi-asserted-by": "crossref",
"first-page": "999",
"journal-title": "Lancet",
"key": "ref_44",
"volume": "383",
"year": "2014"
},
{
"DOI": "10.1016/j.jacc.2016.03.508",
"article-title": "Effects of Vitamin D on Cardiac Function in Patients With Chronic HF: The VINDICATE Study",
"author": "Witte",
"doi-asserted-by": "crossref",
"first-page": "2593",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "ref_45",
"volume": "67",
"year": "2016"
},
{
"DOI": "10.3390/nu15020334",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Pál, É., Ungvári, Z., Benyó, Z., and Várbíró, S. (2023). Role of Vitamin D Deficiency in the Pathogenesis of Cardiovascular and Cerebrovascular Diseases. Nutrients, 15."
},
{
"DOI": "10.1016/j.annepidem.2009.03.021",
"article-title": "Vitamin D for cancer prevention: Global perspective",
"author": "Garland",
"doi-asserted-by": "crossref",
"first-page": "468",
"journal-title": "Ann. Epidemiol.",
"key": "ref_47",
"volume": "19",
"year": "2009"
},
{
"DOI": "10.1007/s10552-004-1661-4",
"article-title": "The epidemiology of vitamin D and cancer incidence and mortality: A review (United States)",
"author": "Giovannucci",
"doi-asserted-by": "crossref",
"first-page": "83",
"journal-title": "Cancer Causes Control",
"key": "ref_48",
"volume": "16",
"year": "2005"
},
{
"DOI": "10.1093/ajcn/nqab419",
"article-title": "Vitamin D supplementation and prevention of cardiovascular disease and cancer in the Finnish Vitamin D Trial: A randomized controlled trial",
"author": "Virtanen",
"doi-asserted-by": "crossref",
"first-page": "1300",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_49",
"volume": "115",
"year": "2022"
},
{
"DOI": "10.1016/j.jnutbio.2020.108571",
"article-title": "Vitamin D and its therapeutic relevance in pulmonary diseases",
"author": "Ahmad",
"doi-asserted-by": "crossref",
"first-page": "108571",
"journal-title": "J. Nutr. Biochem.",
"key": "ref_50",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "i6583",
"journal-title": "BMJ",
"key": "ref_51",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.1111/obr.12239",
"article-title": "Obesity and vitamin D deficiency: A systematic review and meta-analysis",
"author": "Costa",
"doi-asserted-by": "crossref",
"first-page": "341",
"journal-title": "Obes. Rev.",
"key": "ref_52",
"volume": "16",
"year": "2015"
},
{
"DOI": "10.3390/medicina55090541",
"doi-asserted-by": "crossref",
"key": "ref_53",
"unstructured": "Vranić, L., Mikolašević, I., and Milić, S. (2019). Vitamin D Deficiency: Consequence or Cause of Obesity?. Medicina, 55."
},
{
"DOI": "10.1002/art.40137",
"article-title": "2017 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis",
"author": "Buckley",
"doi-asserted-by": "crossref",
"first-page": "1521",
"journal-title": "Arthritis Rheumatol.",
"key": "ref_54",
"volume": "69",
"year": "2017"
},
{
"DOI": "10.3390/ijms18091949",
"doi-asserted-by": "crossref",
"key": "ref_55",
"unstructured": "Kim, D. (2017). The Role of Vitamin D in Thyroid Diseases. Int. J. Mol. Sci., 18."
},
{
"DOI": "10.3390/medicina58020194",
"doi-asserted-by": "crossref",
"key": "ref_56",
"unstructured": "Galușca, D., Popoviciu, M.S., Babeș, E.E., Vidican, M., Zaha, A.A., Babeș, V.V., Jurca, A.D., Zaha, D.C., and Bodog, F. (2022). Vitamin D Implications and Effect of Supplementation in Endocrine Disorders: Autoimmune Thyroid Disorders (Hashimoto’s Disease and Grave’s Disease), Diabetes Mellitus and Obesity. Medicina, 58."
},
{
"DOI": "10.1080/07315724.2020.1856013",
"article-title": "Vitamin D deficiency and low serum calcium as predictors of poor prognosis in patients with severe COVID-19",
"author": "Bennouar",
"doi-asserted-by": "crossref",
"first-page": "104",
"journal-title": "J. Am. Coll. Nutr.",
"key": "ref_57",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "crossref",
"key": "ref_58",
"unstructured": "Maghbooli, Z., Sahraian, M.A., Ebrahimi, M., Pazoki, M., Kafan, S., Tabriz, H.M., Hadadi, A., Montazeri, M., Nasiri, M., and Shirvani, A. (2020). Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS ONE, 15."
},
{
"key": "ref_59",
"unstructured": "(2023, February 01). Our World in Data. Available online: https://ourworldindata.org/coronavirus/country/romania#daily-confirmed-deaths-how-do-they-compare-to-other-countries."
},
{
"article-title": "Low Vitamin D Status at Admission as a Risk Factor for Poor Survival in Hospitalized Patients With COVID-19: An Italian Retrospective Study",
"author": "Infante",
"first-page": "250",
"journal-title": "J. Am. Nutr. Assoc.",
"key": "ref_60",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"article-title": "Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality",
"author": "Herroelen",
"doi-asserted-by": "crossref",
"first-page": "381",
"journal-title": "Am. J. Clin. Pathol.",
"key": "ref_61",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "crossref",
"key": "ref_62",
"unstructured": "Radujkovic, A., Hippchen, T., Tiwari-Heckler, S., Dreher, S., Boxberger, M., and Merle, U. (2020). Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients, 12."
},
{
"DOI": "10.3390/nu14101998",
"doi-asserted-by": "crossref",
"key": "ref_63",
"unstructured": "Huțanu, A., Georgescu, A.M., Voidăzan, S., Andrejkovits, A.V., Negrea, V., and Dobreanu, M. (2022). Low Serum Vitamin D in COVID-19 Patients Is Not Related to Inflammatory Markers and Patients’ Outcomes—A Single-Center Experience and a Brief Review of the Literature. Nutrients, 14."
},
{
"key": "ref_64",
"unstructured": "World Health Organisation (2023, January 21). Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-COVID-19—8-February-2022."
}
],
"reference-count": 64,
"references-count": 64,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/15/5/1227"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "25 Hydroxyvitamin D Serum Concentration and COVID-19 Severity and Outcome—A Retrospective Survey in a Romanian Hospital",
"type": "journal-article",
"volume": "15"
}
