Antiplatelet therapy prior to COVID-19 infection impacts on patients mortality: a propensity score-matched cohort study
et al., Scientific Reports, doi:10.1038/s41598-024-55407-9, Feb 2024
Retrospective 2,170 hospitalized COVID-19 patients showing no difference in mortality with remdesivir in unadjusted results.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
Study covers remdesivir and aspirin.
|
risk of death, no change, HR 1.00, p = 1.00, treatment 88, control 460, Cox proportional hazards, day 90.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
Sokolski et al., 28 Feb 2024, retrospective, Poland, peer-reviewed, 11 authors.
Contact: mateusz.sokolski@umw.edu.pl.
Antiplatelet therapy prior to COVID-19 infection impacts on patients mortality: a propensity score-matched cohort study
Scientific Reports, doi:10.1038/s41598-024-55407-9
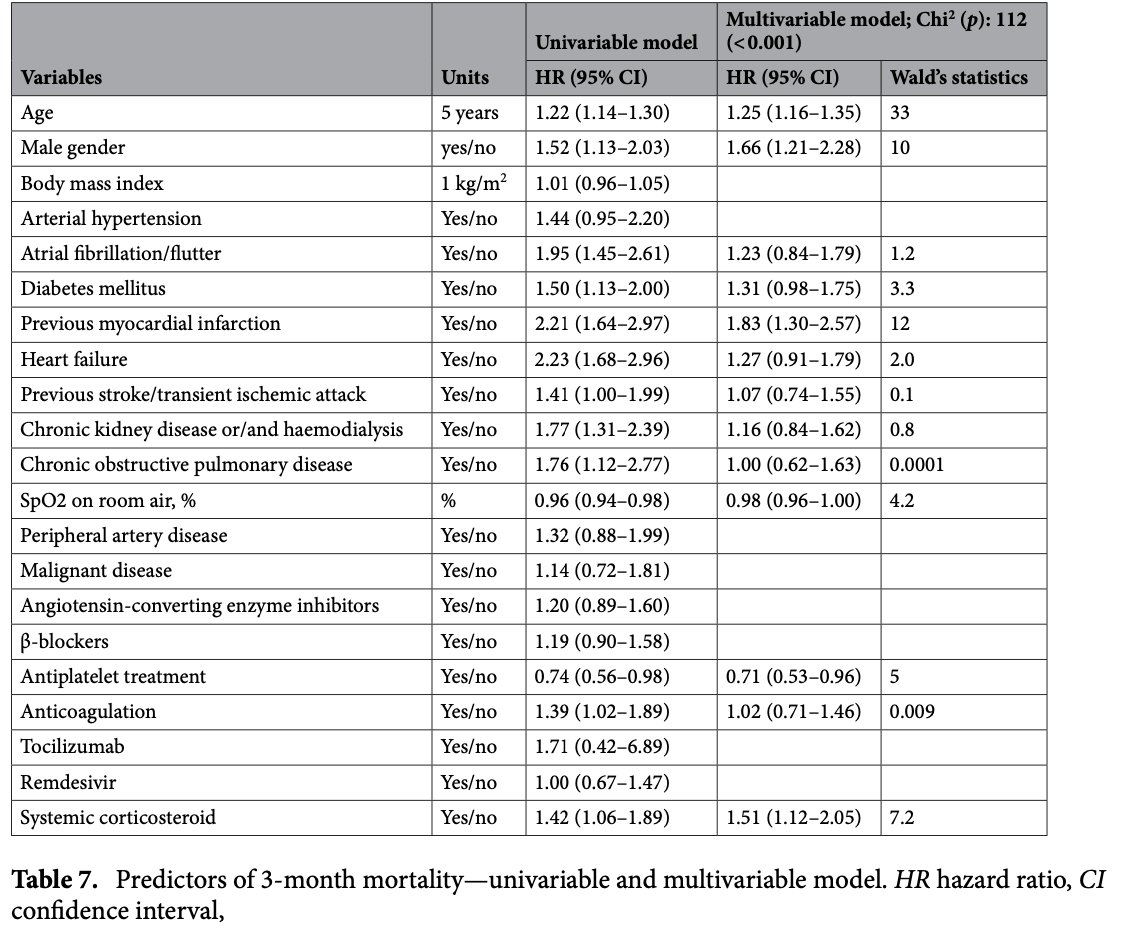
One of the major pathomechanisms of COVID-19 is the interplay of hyperinflammation and disruptions in coagulation processes, involving thrombocytes. Antiplatelet therapy (AP) by antiinflammatory effect and inhibition of platelet aggregation may affect these pathways. The aim of this study was to investigate if AP has an impact on the in-hospital course and medium-term outcomes in hospitalized COVID-19 patients. The study population (2170 COVID-19 patients: mean ± SD age 60 ± 19 years old, 50% male) was divided into a group of 274 patients receiving any AP prior to COVID-19 infection (AP group), and after propensity score matching, a group of 274 patients without previous AP (non-AP group). Patients from the AP group were less frequently hospitalized in the intensive care unit: 9% vs. 15%, 0.55 (0.33-0.94), developed less often shock: 9% vs. 15%, 0.56 (0.33-0.96), and required less aggressive forms of therapy. The AP group had more coronary revascularizations: 5% vs. 1%, 3.48 (2.19-5.55) and strokes/TIA: 5% vs. 1%, 3.63 (1.18-11.2). The bleeding rate was comparable: 7% vs. 7%, 1.06 (0.54-2.06). The patients from the AP group had lower 3-month mortality: 31% vs. 39%, 0.69 (0.51-0.93) and didn't differ significantly in 6-month mortality: 34% vs. 41%, 0.79 (0.60-1.04). When analyzing the subgroup with a history of myocardial infarction and/or coronary revascularization and/or previous stroke/transient ischemic attack and/or peripheral artery disease, AP had a beneficial effect on both 3-month: 37% vs. 56%, 0.58 (0.40-0.86) and 6-month mortality: 42% vs. 57%, 0.63 (0.44-0.92). Moreover, the favourable effect was highly noticeable in this subgroup where acetylsalicylic acid was continued during hospitalization with reduction of in-hospital: 19% vs. 43%, 0.31 (0.15-0.67), 3-month: 30% vs. 54%, 044 (0.26-0.75) and 6-month mortality: 33% vs. 54%, 0.49 (0.29-0.82) when confronted with the subgroup who had acetylsalicylic acid suspension during hospitalization. The AP may have a beneficial impact on hospital course and mortality in COVID-19 and shouldn't be discontinued, especially in high-risk patients. Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has become a global health crisis 1 . SARS-CoV-2 is a single-stranded RNA virus with a high mutation rate 2,3 . Five SARS-CoV-2 variants (alpha, beta, gamma, delta, and omicron) have been identified by WHO as variants of concern. While approximately 80% of SARS-CoV-2 infections are mild to moderate, the clinical presentation and case fatality rate vary depending on the viral variant and comorbidities 4,5 . Thus, the infection fatality rates vary from 0.3 to 5%. The major causes of death are respiratory failure, sepsis/multi-organ failure, OPEN
Author contributions Conceptualization: M.S., M.P.r; formal analysis: M.S., M.Pr..; investigation: M.S., K.R., B.A., K.K-P, W.L., M.Po., J.S., A.D., K.M., E.A.J., M.Pr.; methodology: M.S., M.Pr.; project administration: A.D., K.M., M.Pr., E.A.J.; supervision: M.S., A.D., K.M., M.Pr., EAJ.; visualization: M.S., K.R; writing-original draft, M.S., K.R.; writingreview and editing, M.S., K.R., K.R., B.A., K. K-P, W.L., M.Po., J.S., A.D., K.M., M.Pr., E.A.J. All authors have contributed substantially to this work and have read and agreed to the published version of the manuscript.
Competing interests The authors declare no competing interests.
References
Ackermann, Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in covid-19, N. Engl. J. Med
Ali, Spinler, COVID-19 and thrombosis: From bench to bedside, Trends Cardiovasc. Med
Berger, Effect of P2Y12 inhibitors on survival free of organ support among non-critically ill hospitalized patients with COVID-19: a randomized clinical trial, JAMA
Bianconi, Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?, Drugs
Brambilla, Canzano, Becchetti, Tremoli, Camera, Alterations in platelets during SARS-CoV-2 infection, Platelets
Carsana, Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: A two-centre descriptive study, Lancet Infect. Dis
Case, Comparison of outcomes in patients with COVID-19 and thrombosis versus those without thrombosis, Am. J. Cardiol
Di Minno, Ambrosino, Calcaterra, Di Minno, COVID-19 and venous thromboembolism: A meta-analysis of literature studies, Semin. Thromb. Hemost
Dwiputra Hernugrahanto, Thromboembolic involvement and its possible pathogenesis in COVID-19 mortality: Lesson from post-mortem reports, Eur. Rev. Med. Pharmacol. Sci
Fernandes, Emerging COVID-19 variants and their impact on SARS-CoV-2 diagnosis, therapeutics and vaccines, Ann. Med
Fischer, Antiplatelet agents for the treatment of adults with COVID-19, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD015078
Heitzer, Clopidogrel improves systemic endothelial nitric oxide bioavailability in patients with coronary artery disease: Evidence for antioxidant and antiinflammatory effects, Arterioscler. Thromb. Vasc. Biol
Iba, Connors, Levy, The coagulopathy, endotheliopathy, and vasculitis of COVID-19, Inflamm. Res
Jin, Virology, epidemiology, pathogenesis, and control of COVID-19, Viruses
Kumar, Rivkin, Raffini, Thrombotic complications in children with Coronavirus disease 2019 and Multisystem Inflammatory Syndrome of Childhood, J. Thromb. Haemost
Levi, Van Der Poll, Inflammation and coagulation, Crit. Care Med
Li, Geraghty, Mehta, Rothwell, Oxford Vascular Study. Age-specific risks, severity, time course, and outcome of bleeding on long-term antiplatelet treatment after vascular events: a population-based cohort study, Lancet
Liao, Identification of potential new COVID-19 treatments via RWD-driven drug repurposing, Sci. Rep
Litvinov, Altered platelet and coagulation function in moderate-to-severe COVID-19, Sci. Rep
Ludwikowska, Moksud, Tracewski, Sokolski, Szenborn, Cardiac involvement in patients with multisystem inflammatory syndrome in children (MIS-C) in Poland, Biomedicines
Malik, The SARS-CoV-2 mutations versus vaccine effectiveness: New opportunities to new challenges, J. Infect. Public Health
Matli, Combined anticoagulant and antiplatelet therapy is associated with an improved outcome in hospitalised patients with COVID-19: a propensity matched cohort study, Open Heart, doi:10.1136/openhrt-2021-001785
Mcmullen, A descriptive and quantitative immunohistochemical study demonstrating a spectrum of platelet recruitment patterns across pulmonary infections including COVID-19, Am. J. Clin. Pathol
Mondal, Quintili, Karamchandani, Bose, Thromboembolic disease in COVID-19 patients: A brief narrative review, J. Intensive Care
Neumann, ESC/EACTS Guidelines on myocardial revascularization, EuroIntervention
Patoulias, Dimosiari, Michailidis, Coronary microvascular dysfunction in the context of long COVID-19: What is the effect of anti-inflammatory treatment?, Kardiol. Pol
Protasiewicz, Anticoagulation prior to COVID-19 infection has no impact on 6 months mortality: A propensity scorematched cohort study, J. Clin. Med
Protasiewicz, Szymkiewicz, Kuliczkowski, Mysiak, Witkiewicz, Modern antiplatelet therapy-opportunities and risks, Adv. Clin. Exp. Med
Rapkiewicz, Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series, EClinicalMedicine, doi:10.1016/j.eclinm.2020.100434
Rayes, Bourne, Brill, Watson, The dual role of platelet-innate immune cell interactions in thrombo-inflammation, Res. Pract. Thromb. Haemost
Rola, Invasive assessment of coronary microvascular dysfunction in patients with long COVID: Outcomes of a pilot study, Kardiol. Pol
Salah, Mehta, Meta-analysis of the effect of aspirin on mortality in COVID-19, Am. J. Cardiol
Sisinni, Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: The ASA-CARE study, Int. J. Cardiol
Sokolski, Cardiac emergencies during the coronavirus disease 2019 pandemic in the light of the current evidence, Kardiol. Pol
Sokolski, Heart failure in COVID-19: The multicentre, multinational PCHF-COVICAV registry, ESC Heart Fail
Sokolski, History of heart failure in patients hospitalized due to COVID-19: Relevant factor of in-hospital complications and all-cause mortality up to six months, J. Clin. Med
Stone, FREEDOM COVID anticoagulation strategy randomized trial investigators. randomized trial of anticoagulation strategies for noncritically ill patients hospitalized with COVID-19, J. Am. Coll. Cardiol
Streeck, Infection fatality rate of SARS-CoV2 in a super-spreading event in Germany, Nat. Commun
Su, Associations between the use of aspirin or other antiplatelet drugs and all-cause mortality among patients with COVID-19: A meta-analysis, Front. Pharmacol, doi:10.3389/fphar.2022.989903
Taus, Platelets promote thromboinflammation in SARS-CoV-2 pneumonia, Arterioscler. Thromb. Vasc. Biol
Thomas, Storey, Effect of P2Y12 inhibitors on inflammation and immunity, Thromb. Haemost
Toubasi, Effect on morbidity and mortality of direct oral anticoagulants in patients with COVID-19, Am. J. Cardiol
Yang, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A singlecentered, retrospective, observational study, Lancet Respir. Med
Zhang, Clinical characteristics of 82 cases of death from COVID-19, PLoS One, doi:10.1371/journal.pone.0235458
Zuin, Prevalence of acute pulmonary embolism at autopsy in patients with COVID-19, Am. J. Cardiol
DOI record:
{
"DOI": "10.1038/s41598-024-55407-9",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-024-55407-9",
"abstract": "<jats:title>Abstract</jats:title><jats:p>One of the major pathomechanisms of COVID-19 is the interplay of hyperinflammation and disruptions in coagulation processes, involving thrombocytes. Antiplatelet therapy (AP) by anti-inflammatory effect and inhibition of platelet aggregation may affect these pathways. The aim of this study was to investigate if AP has an impact on the in-hospital course and medium-term outcomes in hospitalized COVID-19 patients. The study population (2170 COVID-19 patients: mean ± SD age 60 ± 19 years old, 50% male) was divided into a group of 274 patients receiving any AP prior to COVID-19 infection (AP group), and after propensity score matching, a group of 274 patients without previous AP (non-AP group). Patients from the AP group were less frequently hospitalized in the intensive care unit: 9% vs. 15%, 0.55 (0.33–0.94), developed less often shock: 9% vs. 15%, 0.56 (0.33–0.96), and required less aggressive forms of therapy. The AP group had more coronary revascularizations: 5% vs. 1%, 3.48 (2.19–5.55) and strokes/TIA: 5% vs. 1%, 3.63 (1.18–11.2). The bleeding rate was comparable: 7% vs. 7%, 1.06 (0.54–2.06). The patients from the AP group had lower 3-month mortality: 31% vs. 39%, 0.69 (0.51–0.93) and didn’t differ significantly in 6-month mortality: 34% vs. 41%, 0.79 (0.60–1.04). When analyzing the subgroup with a history of myocardial infarction and/or coronary revascularization and/or previous stroke/transient ischemic attack and/or peripheral artery disease, AP had a beneficial effect on both 3-month: 37% vs. 56%, 0.58 (0.40–0.86) and 6-month mortality: 42% vs. 57%, 0.63 (0.44–0.92). Moreover, the favourable effect was highly noticeable in this subgroup where acetylsalicylic acid was continued during hospitalization with reduction of in-hospital: 19% vs. 43%, 0.31 (0.15–0.67), 3-month: 30% vs. 54%, 044 (0.26–0.75) and 6-month mortality: 33% vs. 54%, 0.49 (0.29–0.82) when confronted with the subgroup who had acetylsalicylic acid suspension during hospitalization. The AP may have a beneficial impact on hospital course and mortality in COVID-19 and shouldn’t be discontinued, especially in high-risk patients.</jats:p>",
"alternative-id": [
"55407"
],
"article-number": "4832",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "7 October 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "22 February 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "28 February 2024"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Sokolski",
"given": "Mateusz",
"sequence": "first"
},
{
"affiliation": [],
"family": "Reszka",
"given": "Konrad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Adamik",
"given": "Barbara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kilis-Pstrusinska",
"given": "Katarzyna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lis",
"given": "Weronika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pomorski",
"given": "Michał",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sokolowski",
"given": "Janusz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Doroszko",
"given": "Adrian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Madziarska",
"given": "Katarzyna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jankowska",
"given": "Ewa Anita",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Protasiewicz",
"given": "Marcin",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
2,
28
]
],
"date-time": "2024-02-28T04:32:43Z",
"timestamp": 1709094763000
},
"deposited": {
"date-parts": [
[
2024,
2,
28
]
],
"date-time": "2024-02-28T04:35:47Z",
"timestamp": 1709094947000
},
"indexed": {
"date-parts": [
[
2024,
2,
29
]
],
"date-time": "2024-02-29T00:39:25Z",
"timestamp": 1709167165691
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
2,
28
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
28
]
],
"date-time": "2024-02-28T00:00:00Z",
"timestamp": 1709078400000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
28
]
],
"date-time": "2024-02-28T00:00:00Z",
"timestamp": 1709078400000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-024-55407-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-55407-9",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-55407-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2024,
2,
28
]
]
},
"published-online": {
"date-parts": [
[
2024,
2,
28
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "55407_CR1",
"unstructured": "World Health Organisation. WHO director-general’s opening remarks at the media briefing on COVID-19, https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (2020)."
},
{
"DOI": "10.1016/j.jiph.2021.12.014",
"author": "JA Malik",
"doi-asserted-by": "publisher",
"first-page": "228",
"journal-title": "J. Infect. Public Health.",
"key": "55407_CR2",
"unstructured": "Malik, J. A. et al. The SARS-CoV-2 mutations versus vaccine effectiveness: New opportunities to new challenges. J. Infect. Public Health. 15, 228–240 (2022).",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.3390/v12040372",
"author": "Y Jin",
"doi-asserted-by": "publisher",
"first-page": "372",
"journal-title": "Viruses.",
"key": "55407_CR3",
"unstructured": "Jin, Y. et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 12, 372 (2020).",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1080/07853890.2022.2031274",
"author": "Q Fernandes",
"doi-asserted-by": "publisher",
"first-page": "524",
"journal-title": "Ann. Med.",
"key": "55407_CR4",
"unstructured": "Fernandes, Q. et al. Emerging COVID-19 variants and their impact on SARS-CoV-2 diagnosis, therapeutics and vaccines. Ann. Med. 54, 524–540 (2022).",
"volume": "54",
"year": "2022"
},
{
"DOI": "10.1016/j.amjcard.2022.01.051",
"author": "M Zuin",
"doi-asserted-by": "publisher",
"first-page": "159",
"journal-title": "Am. J. Cardiol.",
"key": "55407_CR5",
"unstructured": "Zuin, M. et al. Prevalence of acute pulmonary embolism at autopsy in patients with COVID-19. Am. J. Cardiol. 171, 159–164 (2022).",
"volume": "171",
"year": "2022"
},
{
"DOI": "10.1038/s41467-020-19509-y",
"author": "H Streeck",
"doi-asserted-by": "publisher",
"first-page": "5829",
"journal-title": "Nat. Commun.",
"key": "55407_CR6",
"unstructured": "Streeck, H. et al. Infection fatality rate of SARS-CoV2 in a super-spreading event in Germany. Nat. Commun. 11, 5829 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"author": "X Yang",
"doi-asserted-by": "publisher",
"first-page": "475",
"journal-title": "Lancet Respir. Med.",
"key": "55407_CR7",
"unstructured": "Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 8, 475–481 (2020).",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0235458",
"doi-asserted-by": "publisher",
"key": "55407_CR8",
"unstructured": "Zhang, B. et al. Clinical characteristics of 82 cases of death from COVID-19. PLoS One. 15, e0235458. https://doi.org/10.1371/journal.pone.0235458 (2020)."
},
{
"DOI": "10.1002/ehf2.13549",
"author": "M Sokolski",
"doi-asserted-by": "publisher",
"first-page": "4955",
"journal-title": "ESC Heart Fail.",
"key": "55407_CR9",
"unstructured": "Sokolski, M. et al. Heart failure in COVID-19: The multicentre, multinational PCHF-COVICAV registry. ESC Heart Fail. 8, 4955–4967 (2021).",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3390/jcm11010241",
"author": "M Sokolski",
"doi-asserted-by": "publisher",
"first-page": "241",
"journal-title": "J. Clin. Med.",
"key": "55407_CR10",
"unstructured": "Sokolski, M. et al. History of heart failure in patients hospitalized due to COVID-19: Relevant factor of in-hospital complications and all-cause mortality up to six months. J. Clin. Med. 11, 241 (2022).",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1007/s00011-020-01401-6",
"author": "T Iba",
"doi-asserted-by": "publisher",
"first-page": "1181",
"journal-title": "Inflamm. Res.",
"key": "55407_CR11",
"unstructured": "Iba, T., Connors, J. M. & Levy, J. H. The coagulopathy, endotheliopathy, and vasculitis of COVID-19. Inflamm. Res. 69, 1181–1189 (2020).",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-95397-6",
"author": "RI Litvinov",
"doi-asserted-by": "publisher",
"first-page": "16290",
"journal-title": "Sci. Rep.",
"key": "55407_CR12",
"unstructured": "Litvinov, R. I. et al. Altered platelet and coagulation function in moderate-to-severe COVID-19. Sci. Rep. 1, 16290 (2021).",
"volume": "1",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2015432",
"author": "M Ackermann",
"doi-asserted-by": "publisher",
"first-page": "120",
"journal-title": "N. Engl. J. Med.",
"key": "55407_CR13",
"unstructured": "Ackermann, M. et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in covid-19. N. Engl. J. Med. 383, 120–128 (2020).",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/j.eclinm.2020.100434",
"doi-asserted-by": "publisher",
"key": "55407_CR14",
"unstructured": "Rapkiewicz, A.V. et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series. EClinicalMedicine. 24, 100434. https://doi.org/10.1016/j.eclinm.2020.100434 (2020)."
},
{
"DOI": "10.1080/09537104.2021.1962519",
"author": "M Brambilla",
"doi-asserted-by": "publisher",
"first-page": "192",
"journal-title": "Platelets.",
"key": "55407_CR15",
"unstructured": "Brambilla, M., Canzano, P., Becchetti, A., Tremoli, E. & Camera, M. Alterations in platelets during SARS-CoV-2 infection. Platelets. 33, 192–199 (2022).",
"volume": "33",
"year": "2022"
},
{
"key": "55407_CR16",
"unstructured": "Dwiputra Hernugrahanto, K. et al. Thromboembolic involvement and its possible pathogenesis in COVID-19 mortality: Lesson from post-mortem reports. Eur. Rev. Med. Pharmacol. Sci. 25, 1670–1679 (2021)."
},
{
"DOI": "10.1093/ajcp/aqaa230",
"author": "PD McMullen",
"doi-asserted-by": "publisher",
"first-page": "354",
"journal-title": "Am. J. Clin. Pathol.",
"key": "55407_CR17",
"unstructured": "McMullen, P. D. et al. A descriptive and quantitative immunohistochemical study demonstrating a spectrum of platelet recruitment patterns across pulmonary infections including COVID-19. Am. J. Clin. Pathol. 155, 354–363 (2021).",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(20)30434-5",
"author": "L Carsana",
"doi-asserted-by": "publisher",
"first-page": "1135",
"journal-title": "Lancet Infect. Dis.",
"key": "55407_CR18",
"unstructured": "Carsana, L. et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: A two-centre descriptive study. Lancet Infect. Dis. 20, 1135–1140 (2020).",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1186/s40560-020-00483-y",
"author": "S Mondal",
"doi-asserted-by": "publisher",
"first-page": "70",
"journal-title": "J. Intensive Care.",
"key": "55407_CR19",
"unstructured": "Mondal, S., Quintili, A. L., Karamchandani, K. & Bose, S. Thromboembolic disease in COVID-19 patients: A brief narrative review. J. Intensive Care. 8, 70 (2020).",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.tcm.2020.12.004",
"author": "MAM Ali",
"doi-asserted-by": "publisher",
"first-page": "143",
"journal-title": "Trends Cardiovasc. Med.",
"key": "55407_CR20",
"unstructured": "Ali, M. A. M. & Spinler, S. A. COVID-19 and thrombosis: From bench to bedside. Trends Cardiovasc. Med. 31, 143–160 (2021).",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1016/j.amjcard.2021.08.038",
"author": "BC Case",
"doi-asserted-by": "publisher",
"first-page": "106",
"journal-title": "Am. J. Cardiol.",
"key": "55407_CR21",
"unstructured": "Case, B. C. et al. Comparison of outcomes in patients with COVID-19 and thrombosis versus those without thrombosis. Am. J. Cardiol. 160, 106–111 (2021).",
"volume": "160",
"year": "2021"
},
{
"DOI": "10.1097/CCM.0b013e3181c98d21",
"author": "M Levi",
"doi-asserted-by": "publisher",
"first-page": "S26",
"journal-title": "Crit. Care Med.",
"key": "55407_CR22",
"unstructured": "Levi, M. & van der Poll, T. Inflammation and coagulation. Crit. Care Med. 38, S26-34 (2010).",
"volume": "38",
"year": "2010"
},
{
"DOI": "10.33963/KP.15516",
"author": "M Sokolski",
"doi-asserted-by": "publisher",
"first-page": "818",
"journal-title": "Kardiol. Pol.",
"key": "55407_CR23",
"unstructured": "Sokolski, M. et al. Cardiac emergencies during the coronavirus disease 2019 pandemic in the light of the current evidence. Kardiol. Pol. 78, 818–824 (2020).",
"volume": "78",
"year": "2020"
},
{
"DOI": "10.1161/ATVBAHA.120.315175",
"author": "F Taus",
"doi-asserted-by": "publisher",
"first-page": "2975",
"journal-title": "Arterioscler. Thromb. Vasc. Biol.",
"key": "55407_CR24",
"unstructured": "Taus, F. et al. Platelets promote thromboinflammation in SARS-CoV-2 pneumonia. Arterioscler. Thromb. Vasc. Biol. 40, 2975–2989 (2020).",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.33963/KP.a2022.0239",
"author": "P Rola",
"doi-asserted-by": "publisher",
"first-page": "1252",
"journal-title": "Kardiol. Pol.",
"key": "55407_CR25",
"unstructured": "Rola, P. et al. Invasive assessment of coronary microvascular dysfunction in patients with long COVID: Outcomes of a pilot study. Kardiol. Pol. 80, 1252–1255 (2022).",
"volume": "80",
"year": "2022"
},
{
"DOI": "10.33963/KP.a2022.0272",
"author": "D Patoulias",
"doi-asserted-by": "publisher",
"first-page": "318",
"journal-title": "Kardiol. Pol.",
"key": "55407_CR26",
"unstructured": "Patoulias, D., Dimosiari, A. & Michailidis, T. Coronary microvascular dysfunction in the context of long COVID-19: What is the effect of anti-inflammatory treatment?. Kardiol. Pol. 81, 318–319 (2023).",
"volume": "81",
"year": "2023"
},
{
"DOI": "10.1002/rth2.12266",
"author": "J Rayes",
"doi-asserted-by": "publisher",
"first-page": "23",
"journal-title": "Res. Pract. Thromb. Haemost.",
"key": "55407_CR27",
"unstructured": "Rayes, J., Bourne, J. H., Brill, A. & Watson, S. P. The dual role of platelet-innate immune cell interactions in thrombo-inflammation. Res. Pract. Thromb. Haemost. 4, 23–35 (2019).",
"volume": "4",
"year": "2019"
},
{
"DOI": "10.1016/j.amjcard.2020.12.073",
"author": "HM Salah",
"doi-asserted-by": "publisher",
"first-page": "158",
"journal-title": "Am. J. Cardiol.",
"key": "55407_CR28",
"unstructured": "Salah, H. M. & Mehta, J. L. Meta-analysis of the effect of aspirin on mortality in COVID-19. Am. J. Cardiol. 142, 158–159 (2021).",
"volume": "142",
"year": "2021"
},
{
"DOI": "10.1001/jama.2021.23605",
"author": "JS Berger",
"doi-asserted-by": "publisher",
"first-page": "227",
"journal-title": "JAMA.",
"key": "55407_CR29",
"unstructured": "Berger, J. S. et al. Effect of P2Y12 inhibitors on survival free of organ support among non-critically ill hospitalized patients with COVID-19: a randomized clinical trial. JAMA. 327, 227–236 (2022).",
"volume": "327",
"year": "2022"
},
{
"DOI": "10.1136/openhrt-2021-001785",
"doi-asserted-by": "publisher",
"key": "55407_CR30",
"unstructured": "Matli, K. et al. Combined anticoagulant and antiplatelet therapy is associated with an improved outcome in hospitalised patients with COVID-19: a propensity matched cohort study. Open Heart. 8, e001785. https://doi.org/10.1136/openhrt-2021-001785 (2021)."
},
{
"DOI": "10.3389/fphar.2022.989903",
"doi-asserted-by": "publisher",
"key": "55407_CR31",
"unstructured": "Su, W. et al. Associations between the use of aspirin or other antiplatelet drugs and all-cause mortality among patients with COVID-19: A meta-analysis. Front. Pharmacol. 13, 989903. https://doi.org/10.3389/fphar.2022.989903 (2022)."
},
{
"DOI": "10.1055/s-0040-1715456",
"author": "A Di Minno",
"doi-asserted-by": "publisher",
"first-page": "763",
"journal-title": "Semin. Thromb. Hemost.",
"key": "55407_CR32",
"unstructured": "Di Minno, A., Ambrosino, P., Calcaterra, I. & Di Minno, M. N. D. COVID-19 and venous thromboembolism: A meta-analysis of literature studies. Semin. Thromb. Hemost. 46, 763–771 (2020).",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.amjcard.2022.02.007",
"author": "AA Toubasi",
"doi-asserted-by": "publisher",
"first-page": "174",
"journal-title": "Am. J. Cardiol.",
"key": "55407_CR33",
"unstructured": "Toubasi, A. A. Effect on morbidity and mortality of direct oral anticoagulants in patients with COVID-19. Am. J. Cardiol. 171, 174–177 (2022).",
"volume": "171",
"year": "2022"
},
{
"key": "55407_CR34",
"unstructured": "Stone, G. W. et al. FREEDOM COVID anticoagulation strategy randomized trial investigators. randomized trial of anticoagulation strategies for noncritically ill patients hospitalized with COVID-19. J. Am. Coll. Cardiol. 81, 1747–1762 (2023)."
},
{
"DOI": "10.3390/jcm11020352",
"author": "M Protasiewicz",
"doi-asserted-by": "publisher",
"first-page": "352",
"journal-title": "J. Clin. Med.",
"key": "55407_CR35",
"unstructured": "Protasiewicz, M. et al. Anticoagulation prior to COVID-19 infection has no impact on 6 months mortality: A propensity score-matched cohort study. J. Clin. Med. 11, 352 (2022).",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.4244/EIJY19M01_01",
"author": "FJ Neumann",
"doi-asserted-by": "publisher",
"first-page": "1435",
"journal-title": "EuroIntervention.",
"key": "55407_CR36",
"unstructured": "Neumann, F. J. et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention. 14, 1435–1534 (2019).",
"volume": "14",
"year": "2019"
},
{
"author": "M Protasiewicz",
"first-page": "875",
"journal-title": "Adv. Clin. Exp. Med.",
"key": "55407_CR37",
"unstructured": "Protasiewicz, M., Szymkiewicz, P., Kuliczkowski, W., Mysiak, A. & Witkiewicz, W. Modern antiplatelet therapy—opportunities and risks. Adv. Clin. Exp. Med. 22, 875–878 (2013).",
"volume": "22",
"year": "2013"
},
{
"DOI": "10.1016/S0140-6736(17)30770-5",
"doi-asserted-by": "crossref",
"key": "55407_CR38",
"unstructured": "Li, L., Geraghty, O.C., Mehta, Z., Rothwell, P.M.; Oxford Vascular Study. Age-specific risks, severity, time course, and outcome of bleeding on long-term antiplatelet treatment after vascular events: a population-based cohort study. Lancet. 390, 490–499 (2017)."
},
{
"DOI": "10.1002/14651858.CD015078",
"doi-asserted-by": "publisher",
"key": "55407_CR39",
"unstructured": "Fischer, A.L. et al. Antiplatelet agents for the treatment of adults with COVID-19. Cochrane Database Syst. Rev. 7, CD015078. https://doi.org/10.1002/14651858.CD015078 (2023)."
},
{
"DOI": "10.3390/biomedicines11051251",
"author": "KM Ludwikowska",
"doi-asserted-by": "publisher",
"first-page": "1251",
"journal-title": "Biomedicines.",
"key": "55407_CR40",
"unstructured": "Ludwikowska, K. M., Moksud, N., Tracewski, P., Sokolski, M. & Szenborn, L. Cardiac involvement in patients with multisystem inflammatory syndrome in children (MIS-C) in Poland. Biomedicines. 11, 1251 (2023).",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1016/j.jtha.2023.05.020",
"author": "R Kumar",
"doi-asserted-by": "publisher",
"first-page": "2313",
"journal-title": "J. Thromb. Haemost.",
"key": "55407_CR41",
"unstructured": "Kumar, R., Rivkin, M. J. & Raffini, L. Thrombotic complications in children with Coronavirus disease 2019 and Multisystem Inflammatory Syndrome of Childhood. J. Thromb. Haemost. 21, 2313–2326 (2023).",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1038/s41598-023-40033-8",
"author": "Y Liao",
"doi-asserted-by": "publisher",
"first-page": "14586",
"journal-title": "Sci. Rep.",
"key": "55407_CR42",
"unstructured": "Liao, Y. Identification of potential new COVID-19 treatments via RWD-driven drug repurposing. Sci. Rep. 13, 14586 (2023).",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1160/TH14-12-1068",
"author": "MR Thomas",
"doi-asserted-by": "publisher",
"first-page": "490",
"journal-title": "Thromb. Haemost.",
"key": "55407_CR43",
"unstructured": "Thomas, M. R. & Storey, R. F. Effect of P2Y12 inhibitors on inflammation and immunity. Thromb. Haemost. 114, 490–497 (2015).",
"volume": "114",
"year": "2015"
},
{
"DOI": "10.1161/01.ATV.0000225288.74170.dc",
"author": "T Heitzer",
"doi-asserted-by": "publisher",
"first-page": "1648",
"journal-title": "Arterioscler. Thromb. Vasc. Biol.",
"key": "55407_CR44",
"unstructured": "Heitzer, T. et al. Clopidogrel improves systemic endothelial nitric oxide bioavailability in patients with coronary artery disease: Evidence for antioxidant and antiinflammatory effects. Arterioscler. Thromb. Vasc. Biol. 26, 1648–1652 (2006).",
"volume": "26",
"year": "2006"
},
{
"DOI": "10.1007/s40265-020-01365-1",
"author": "V Bianconi",
"doi-asserted-by": "publisher",
"first-page": "1383",
"journal-title": "Drugs.",
"key": "55407_CR45",
"unstructured": "Bianconi, V. et al. Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?. Drugs. 80, 1383–1396 (2020).",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1016/j.ijcard.2021.09.058",
"author": "A Sisinni",
"doi-asserted-by": "publisher",
"first-page": "240",
"journal-title": "Int. J. Cardiol.",
"key": "55407_CR46",
"unstructured": "Sisinni, A. et al. Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: The ASA-CARE study. Int. J. Cardiol. 344, 240–245 (2021).",
"volume": "344",
"year": "2021"
}
],
"reference-count": 46,
"references-count": 46,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-024-55407-9"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Antiplatelet therapy prior to COVID-19 infection impacts on patients mortality: a propensity score-matched cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "14"
}
sokolski