Effectiveness of famotidine on the risk of poor prognosis in patients with COVID-19: A nationwide cohort study in Korea
et al., Heliyon, doi:10.1016/j.heliyon.2023.e16171, May 2023
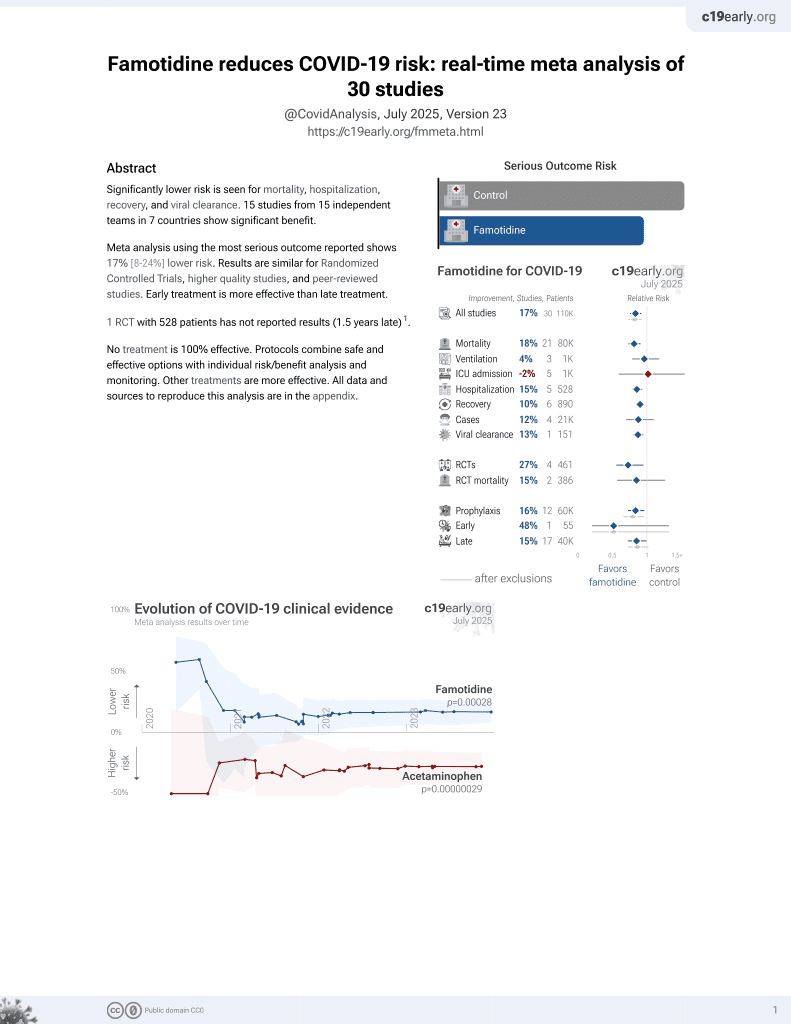
Famotidine for COVID-19
29th treatment shown to reduce risk in
October 2021, now with p = 0.00028 from 30 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
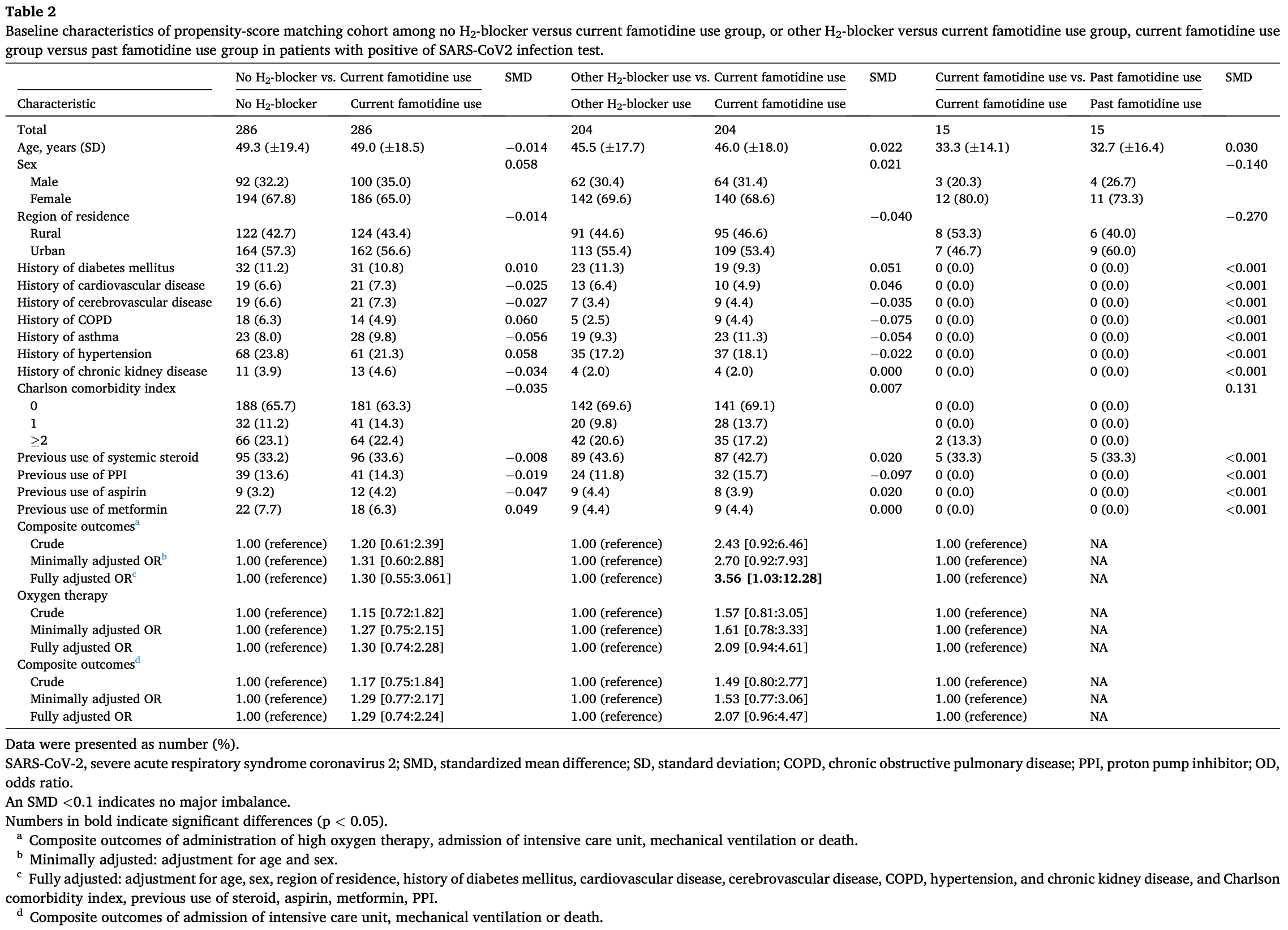
PSM retrospective 6,556 COVID-19 patients in South Korea, showing higher risk of poor outcomes with famotidine vs. other H2-blocker use.
|
risk of progression, 107.0% higher, OR 2.07, p = 0.06, treatment 204, control 204, adjusted per study, ICU, mechanical ventilation, or death, famotidine vs. other H2-blocker use, multivariable, RR approximated with OR.
|
|
risk of progression, 256.0% higher, OR 3.56, p = 0.04, treatment 204, control 204, adjusted per study, high oxygen, ICU, mechanical ventilation, or death, famotidine vs. other H2-blocker use, multivariable, RR approximated with OR.
|
|
risk of oxygen therapy, 109.0% higher, OR 2.09, p = 0.07, treatment 204, control 204, adjusted per study, famotidine vs. other H2-blocker use, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Kwon et al., 31 May 2023, retrospective, South Korea, peer-reviewed, 8 authors, study period 1 July, 2020 - 31 December, 2020.
Contact: shinji@yuhs.ac, knstar@ewha.ac.kr, yonkkang@gmail.com.
Effectiveness of famotidine on the risk of poor prognosis in patients with COVID-19: A nationwide cohort study in Korea
Heliyon, doi:10.1016/j.heliyon.2023.e16171
Famotidine has been proposed as a promising candidate for the treatment of coronavirus disease 2019 . However, there is limited research on the association of famotidine with the poor prognosis of COVID-19. Methods: The Korean nationwide cohort included 6,556 patients who tested positive on RT-PCR for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The poor COVID-19-related outcomes were defined on the basis of having encountered the composite outcome of high oxygen therapy, intensive care unit admission, administration of mechanical ventilation, or death. In addition, we performed exposure-driven propensity score matching for no H 2 -blocker use versus current famotidine use, and other H 2 -blocker use versus current famotidine use. Results: 4,785 (73.0%) patients did not use a H 2 -blocker, 393 (6.0%) patients were currently used famotidine, and 1,292 (19.7%) patients currently used H 2 -blocker other than famotidine. In multivariable analysis after matching (no H 2 -blocker use versus current famotidine use), there was no significant association between current famotidine use and composite outcomes (adjusted odd ratios [aOR]: 1.30, 95% confidence interval [CI]: 0.55-3.06). On the other hand, another matched cohort (other H 2 -blocker use versus current famotidine use), demonstrated a positive association between current famotidine use and composite outcomes (aOR: 3.56, 95% CI: 1. 03-12.28
Author contribution statement Rosie Kwon, Hyung Jun Kim,Seung Won Lee,: Performed the experiments; Analyzed and interpreted the data; Wrote the paper. Lee Smith, Ai Koyanagi: Contributed reagents, materials, analysis tools or data. Jae Il Shin, Tae-Jin Song, Dong Keon Yon: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Table 3 Propensity-score-matching subgroup analyses for difference in length of stay at hospitalization according to famotidine use using analysis-ofcovariance model.
Declaration of competing interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e16171.
References
References
Brennan, Oral famotidine versus placebo in non-hospitalised patients with COVID-19: a randomised, double-blind, data-intense, phase 2 clinical trial, Gut, doi:10.1136/gutjnl-2022-326952
Cha, Jung, Seo, Rahmati, The emerging pandemic recent: SARS-CoV-2, doi:10.54724/lc.2023.e2
Chang, Woo, Park, Lee, Song, Improved oral hygiene care is associated with decreased risk of occurrence for atrial fibrillation and heart failure: a nationwide population-based cohort study, Eur. J. Prev. Cardiol, doi:10.1177/2047487319886018
Freedberg, Famotidine use is associated with improved clinical outcomes in hospitalized COVID-19 patients: a propensity score matched retrospective cohort study, Gastroenterology, doi:10.1053/j.gastro.2020.05.053
Hogan Ii, Dual-histamine receptor blockade with cetirizine -famotidine reduces pulmonary symptoms in COVID-19 patients, Pulm. Pharmacol. Ther, doi:10.1016/j.pupt.2020.101942
Janowitz, Famotidine use and quantitative symptom tracking for COVID-19 in non-hospitalised patients: a case series, Gut, doi:10.1136/gutjnl-2020-321852
Kim, Kim, Kim, Kim, Short and long-term mortality trends for cancer patients with septic shock stratified by cancer type from 2009 to 2017: a population-based cohort study, Cancers, doi:10.3390/cancers13040657
Kim, Yeniova, Global, regional, and national incidence and mortality of COVID-19 in 237 countries and territories, Life Cycle, doi:10.54724/lc.2022.e10
Kow, Abdul Sattar Burud, Hasan, Use of famotidine and risk of severe course of illness in patients with COVID-19: a meta-analysis, Mayo Clin. Proc, doi:10.1016/j.mayocp.2021.03.001
Kritas, Mast cells contribute to coronavirus-induced inflammation: new anti-inflammatory strategy, J. Biol. Regul. Homeost. Agents, doi:10.23812/20-Editorial-Kritas
Kuno, So, Takahashi, Egorova, The association between famotidine and in-hospital mortality of patients with COVID-19, J. Med. Virol, doi:10.1002/jmv.27375
Kwon, National trends in physical activity among adolescents in South Korea before and during the COVID-19 pandemic, J. Med. Virol, doi:10.1002/jmv.28456
Kwon, None
Lee, Acharya, Propensity score matching for causal inference and reducing the confounding effects: statistical standard and guideline of Life Cycle Committee, Life Cycle, doi:10.54724/lc.2022.e18
Lee, Association between mental illness and COVID-19 in South Korea: a post-hoc analysis, Lancet Psychiatr, doi:10.1016/s2215-0366(21)00043-2
Lee, Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study, Lancet Psychiatr, doi:10.1016/s2215-0366(20)30421-1
Lee, Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: a Korean nationwide cohort study, J. Allergy Clin. Immunol, doi:10.1016/j.jaip.2021.03.044
Lee, Methods for testing statistical differences between groups in medical research: statistical standard and guideline of Life Cycle Committee, doi:10.54724/lc.2022.e1
Lee, Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study, Br. J. Sports Med, doi:10.1136/bjsports-2021-104203
Lee, Proton pump inhibitors and the risk of severe COVID-19: a post-hoc analysis from the Korean nationwide cohort, Gut, doi:10.1136/gutjnl-2020-323672
Lee, Regression analysis for continuous independent variables in medical research: statistical standard and guideline of Life Cycle Committee, Life Cycle, doi:10.54724/lc.2022.e3
Lee, Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching, Gut, doi:10.1136/gutjnl-2020-322248
Lee, Yoon, Jang, Lee, Renin-angiotensin system blocker and outcomes of COVID-19: a systematic review and meta-analysis, Thorax, doi:10.1136/thoraxjnl-2020-215322
Ma, Patel, Vemparala, Krishnamurthy, Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus, Sci. Rep, doi:10.1038/s41598-022-09639-2
Malone, COVID-19: famotidine, histamine, mast cells, and mechanisms, Res. Sq, doi:10.21203/rs.3.rs-30934/v2
Mather, Seip, Mckay, Impact of famotidine use on clinical outcomes of hospitalized patients with COVID-19, Am. J. Gastroenterol, doi:10.14309/ajg.0000000000000832
Mukherjee, Famotidine inhibits toll-like receptor 3-mediated inflammatory signaling in SARS-CoV-2 infection, J. Biol. Chem, doi:10.1016/j.jbc.2021.100925
Mura, Real-world evidence for improved outcomes with histamine antagonists and aspirin in 22,560 COVID-19 patients, Signal Transduct. Targeted Ther, doi:10.1038/s41392-021-00689-y
Pahwani, Efficacy of oral famotidine in patients hospitalized with severe acute respiratory syndrome coronavirus 2, Cureus, doi:10.7759/cureus.22404
Reis, Effect of early treatment with metformin on risk of emergency care and hospitalization among patients with COVID-19: the TOGETHER randomized platform clinical trial, Lanc. Reg. Heal. Am, doi:10.1016/j.lana.2021.100142
Rommasi, Nasiri, Mirsaeidi, Immunomodulatory agents for COVID-19 treatment: possible mechanism of action and immunopathology features, Mol. Cell. Biochem, doi:10.1007/s11010-021-04325-9
Shin, Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study, Lancet, doi:10.1016/s2665-9913(21)00151-x
Shin, Papain-like protease regulates SARS-CoV-2 viral spread and innate immunity, Nature, doi:10.1038/s41586-020-2601-5
Shoaibi, Fortin, Weinstein, Berlin, Ryan, Comparative effectiveness of famotidine in hospitalized COVID-19 patients, Am. J. Gastroenterol, doi:10.14309/ajg.0000000000001153
Son, Lim, Park, Trend of prevalence of atrial fibrillation and use of oral anticoagulation therapy in patients with atrial fibrillation in South Korea, J. Epidemiol, doi:10.2188/jea.JE20160149
Sun, Does famotidine reduce the risk of progression to severe disease, death, and intubation for COVID-19 patients? A systemic review and metaanalysis, Dig. Dis. Sci, doi:10.1007/s10620-021-06872-z
Wen, Efficacy and safety of three new oral antiviral treatment (molnupiravir, fluvoxamine and Paxlovid) for COVID-19:a meta-analysis, Ann. Med, doi:10.1080/07853890.2022.2034936
Woo, Lee, Kim, Effect of pioglitazone in acute ischemic stroke patients with diabetes mellitus: a nested case-control study, Cardiovasc. Diabetol, doi:10.1186/s12933-019-0874-5
Wu, Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods, Acta Pharm. Sin. B, doi:10.1016/j.apsb.2020.02.008
Xu, A meta-analysis on the risk factors adjusted association between cardiovascular disease and COVID-19 severity, BMC Publ. Health, doi:10.1186/s12889-021-11051-w
Yeramaneni, Famotidine use is not associated with 30-day mortality: a coarsened exact match study in 7158 hospitalized patients with coronavirus disease 2019 from a large healthcare system, Gastroenterology, doi:10.1053/j.gastro.2020.10.011
Yoo, Marshall, Cho, Yoo, Lee, N-Nitrosodimethylamine-contaminated ranitidine and risk of cancer in South Korea: a nationwide cohort study, Life Cycle, doi:10.54724/lc.2021.e1
DOI record:
{
"DOI": "10.1016/j.heliyon.2023.e16171",
"ISSN": [
"2405-8440"
],
"URL": "http://dx.doi.org/10.1016/j.heliyon.2023.e16171",
"alternative-id": [
"S2405844023033789"
],
"article-number": "e16171",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Effectiveness of famotidine on the risk of poor prognosis in patients with COVID-19: A nationwide cohort study in Korea"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Heliyon"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.heliyon.2023.e16171"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Authors. Published by Elsevier Ltd."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5422-4446",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kwon",
"given": "Rosie",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kim",
"given": "Hyung Jun",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5632-5208",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lee",
"given": "Seung Won",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9565-5004",
"affiliation": [],
"authenticated-orcid": false,
"family": "Koyanagi",
"given": "Ai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shin",
"given": "Jae Il",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9937-762X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Song",
"given": "Tae-Jin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1628-9948",
"affiliation": [],
"authenticated-orcid": false,
"family": "Yon",
"given": "Dong Keon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith",
"given": "Lee",
"sequence": "additional"
}
],
"container-title": "Heliyon",
"container-title-short": "Heliyon",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"cell.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
6,
1
]
],
"date-time": "2023-06-01T10:10:06Z",
"timestamp": 1685614206000
},
"deposited": {
"date-parts": [
[
2023,
6,
7
]
],
"date-time": "2023-06-07T21:49:03Z",
"timestamp": 1686174543000
},
"indexed": {
"date-parts": [
[
2023,
6,
8
]
],
"date-time": "2023-06-08T04:34:47Z",
"timestamp": 1686198887147
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
6
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2023,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
1
]
],
"date-time": "2023-06-01T00:00:00Z",
"timestamp": 1685577600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
9
]
],
"date-time": "2023-05-09T00:00:00Z",
"timestamp": 1683590400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2405844023033789?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2405844023033789?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "e16171",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
6
]
]
},
"published-print": {
"date-parts": [
[
2023,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.54724/lc.2022.e10",
"article-title": "Global, regional, and national incidence and mortality of COVID-19 in 237 countries and territories, January 2022: a systematic analysis for World Health Organization COVID-19 Dashboard",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "e10",
"journal-title": "Life Cycle",
"key": "10.1016/j.heliyon.2023.e16171_bib1",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1016/S2215-0366(21)00043-2",
"article-title": "Association between mental illness and COVID-19 in South Korea: a post-hoc analysis",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Lancet Psychiatr.",
"key": "10.1016/j.heliyon.2023.e16171_bib2",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.54724/lc.2023.e2",
"article-title": "The emerging pandemic recent: SARS-CoV-2",
"author": "Cha",
"doi-asserted-by": "crossref",
"first-page": "e2",
"journal-title": "Life Cycle",
"key": "10.1016/j.heliyon.2023.e16171_bib3",
"volume": "3",
"year": "2023"
},
{
"DOI": "10.1136/gutjnl-2020-323672",
"article-title": "Proton pump inhibitors and the risk of severe COVID-19: a post-hoc analysis from the Korean nationwide cohort",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "2013",
"journal-title": "Gut",
"key": "10.1016/j.heliyon.2023.e16171_bib4",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1186/s12889-021-11051-w",
"article-title": "A meta-analysis on the risk factors adjusted association between cardiovascular disease and COVID-19 severity",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "1533",
"journal-title": "BMC Publ. Health",
"key": "10.1016/j.heliyon.2023.e16171_bib5",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2601-5",
"article-title": "Papain-like protease regulates SARS-CoV-2 viral spread and innate immunity",
"author": "Shin",
"doi-asserted-by": "crossref",
"first-page": "657",
"journal-title": "Nature",
"key": "10.1016/j.heliyon.2023.e16171_bib6",
"volume": "587",
"year": "2020"
},
{
"DOI": "10.1016/j.apsb.2020.02.008",
"article-title": "Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "766",
"journal-title": "Acta Pharm. Sin. B",
"key": "10.1016/j.heliyon.2023.e16171_bib7",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1007/s11010-021-04325-9",
"article-title": "Immunomodulatory agents for COVID-19 treatment: possible mechanism of action and immunopathology features",
"author": "Rommasi",
"doi-asserted-by": "crossref",
"first-page": "711",
"journal-title": "Mol. Cell. Biochem.",
"key": "10.1016/j.heliyon.2023.e16171_bib8",
"volume": "477",
"year": "2022"
},
{
"DOI": "10.1038/s41598-022-09639-2",
"article-title": "Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "5553",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.heliyon.2023.e16171_bib9",
"volume": "12",
"year": "2022"
},
{
"article-title": "Effect of early treatment with metformin on risk of emergency care and hospitalization among patients with COVID-19: the TOGETHER randomized platform clinical trial",
"author": "Reis",
"journal-title": "Lanc. Reg. Heal. Am.",
"key": "10.1016/j.heliyon.2023.e16171_bib10",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.14309/ajg.0000000000000832",
"article-title": "Impact of famotidine use on clinical outcomes of hospitalized patients with COVID-19",
"author": "Mather",
"doi-asserted-by": "crossref",
"first-page": "1617",
"journal-title": "Am. J. Gastroenterol.",
"key": "10.1016/j.heliyon.2023.e16171_bib11",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2020.05.053",
"article-title": "Famotidine use is associated with improved clinical outcomes in hospitalized COVID-19 patients: a propensity score matched retrospective cohort study",
"author": "Freedberg",
"doi-asserted-by": "crossref",
"first-page": "1129",
"journal-title": "Gastroenterology",
"key": "10.1016/j.heliyon.2023.e16171_bib12",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.14309/ajg.0000000000001153",
"article-title": "Comparative effectiveness of famotidine in hospitalized COVID-19 patients",
"author": "Shoaibi",
"doi-asserted-by": "crossref",
"first-page": "692",
"journal-title": "Am. J. Gastroenterol.",
"key": "10.1016/j.heliyon.2023.e16171_bib13",
"volume": "116",
"year": "2021"
},
{
"DOI": "10.1007/s10620-021-06872-z",
"article-title": "Does famotidine reduce the risk of progression to severe disease, death, and intubation for COVID-19 patients? A systemic review and meta-analysis",
"author": "Sun",
"doi-asserted-by": "crossref",
"first-page": "3929",
"journal-title": "Dig. Dis. Sci.",
"key": "10.1016/j.heliyon.2023.e16171_bib14",
"volume": "66",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.03.001",
"article-title": "Use of famotidine and risk of severe course of illness in patients with COVID-19: a meta-analysis",
"author": "Kow",
"doi-asserted-by": "crossref",
"first-page": "1365",
"journal-title": "Mayo Clin. Proc.",
"key": "10.1016/j.heliyon.2023.e16171_bib15",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1053/j.gastro.2020.10.011",
"article-title": "Famotidine use is not associated with 30-day mortality: a coarsened exact match study in 7158 hospitalized patients with coronavirus disease 2019 from a large healthcare system",
"author": "Yeramaneni",
"doi-asserted-by": "crossref",
"first-page": "919",
"journal-title": "Gastroenterology",
"key": "10.1016/j.heliyon.2023.e16171_bib16",
"volume": "160",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27260",
"article-title": "The association between famotidine and in-hospital mortality of patients with COVID-19",
"author": "Kuno",
"doi-asserted-by": "crossref",
"journal-title": "J. Med. Virol.",
"key": "10.1016/j.heliyon.2023.e16171_bib17",
"year": "2021"
},
{
"DOI": "10.1136/gutjnl-2022-326952",
"article-title": "Oral famotidine versus placebo in non-hospitalised patients with COVID-19: a randomised, double-blind, data-intense, phase 2 clinical trial",
"author": "Brennan",
"doi-asserted-by": "crossref",
"first-page": "879",
"journal-title": "Gut",
"key": "10.1016/j.heliyon.2023.e16171_bib18",
"volume": "71",
"year": "2022"
},
{
"article-title": "Efficacy of oral famotidine in patients hospitalized with severe acute respiratory syndrome coronavirus 2",
"author": "Pahwani",
"journal-title": "Cureus",
"key": "10.1016/j.heliyon.2023.e16171_bib19",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1038/s41392-021-00689-y",
"article-title": "Real-world evidence for improved outcomes with histamine antagonists and aspirin in 22,560 COVID-19 patients",
"author": "Mura",
"doi-asserted-by": "crossref",
"first-page": "267",
"journal-title": "Signal Transduct. Targeted Ther.",
"key": "10.1016/j.heliyon.2023.e16171_bib20",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1136/gutjnl-2020-322248",
"article-title": "Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "76",
"journal-title": "Gut",
"key": "10.1016/j.heliyon.2023.e16171_bib21",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"article-title": "Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "901",
"journal-title": "Br. J. Sports Med.",
"key": "10.1016/j.heliyon.2023.e16171_bib22",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.54724/lc.2021.e1",
"article-title": "N-Nitrosodimethylamine-contaminated ranitidine and risk of cancer in South Korea: a nationwide cohort study",
"author": "Yoo",
"doi-asserted-by": "crossref",
"first-page": "e1",
"journal-title": "Life Cycle",
"key": "10.1016/j.heliyon.2023.e16171_bib23",
"volume": "1",
"year": "2021"
},
{
"DOI": "10.1186/s12933-019-0874-5",
"article-title": "Effect of pioglitazone in acute ischemic stroke patients with diabetes mellitus: a nested case-control study",
"author": "Woo",
"doi-asserted-by": "crossref",
"first-page": "67",
"journal-title": "Cardiovasc. Diabetol.",
"key": "10.1016/j.heliyon.2023.e16171_bib24",
"volume": "18",
"year": "2019"
},
{
"DOI": "10.2188/jea.JE20160149",
"article-title": "Trend of prevalence of atrial fibrillation and use of oral anticoagulation therapy in patients with atrial fibrillation in South Korea (2002-2013)",
"author": "Son",
"doi-asserted-by": "crossref",
"first-page": "81",
"journal-title": "J. Epidemiol.",
"key": "10.1016/j.heliyon.2023.e16171_bib25",
"volume": "28",
"year": "2018"
},
{
"article-title": "Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: a Korean nationwide cohort study",
"author": "Lee",
"first-page": "2262",
"journal-title": "J. Allergy Clin. Immunol.",
"key": "10.1016/j.heliyon.2023.e16171_bib26",
"volume": "9",
"year": "2021"
},
{
"article-title": "Short and long-term mortality trends for cancer patients with septic shock stratified by cancer type from 2009 to 2017: a population-based cohort study",
"author": "Kim",
"journal-title": "Cancers",
"key": "10.1016/j.heliyon.2023.e16171_bib27",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/S2215-0366(20)30421-1",
"article-title": "Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "1025",
"journal-title": "Lancet Psychiatr.",
"key": "10.1016/j.heliyon.2023.e16171_bib28",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1177/2047487319886018",
"article-title": "Improved oral hygiene care is associated with decreased risk of occurrence for atrial fibrillation and heart failure: a nationwide population-based cohort study",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "1835",
"journal-title": "Eur. J. Prev. Cardiol.",
"key": "10.1016/j.heliyon.2023.e16171_bib29",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.54724/lc.2022.e18",
"article-title": "Propensity score matching for causal inference and reducing the confounding effects: statistical standard and guideline of Life Cycle Committee",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "e18",
"journal-title": "Life Cycle",
"key": "10.1016/j.heliyon.2023.e16171_bib30",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1016/S2665-9913(21)00151-X",
"article-title": "Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study",
"author": "Shin",
"doi-asserted-by": "crossref",
"first-page": "e698",
"journal-title": "Lancet Rheumat/",
"key": "10.1016/j.heliyon.2023.e16171_bib31",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.54724/lc.2022.e1",
"article-title": "Methods for testing statistical differences between groups in medical research: statistical standard and guideline of Life Cycle Committee",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "e1",
"journal-title": "Life Cycle",
"key": "10.1016/j.heliyon.2023.e16171_bib32",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.54724/lc.2022.e3",
"article-title": "Regression analysis for continuous independent variables in medical research: statistical standard and guideline of Life Cycle Committee",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "e3",
"journal-title": "Life Cycle",
"key": "10.1016/j.heliyon.2023.e16171_bib33",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1002/jmv.28456",
"article-title": "National trends in physical activity among adolescents in South Korea before and during the COVID-19 pandemic, 2009-2021",
"author": "Kwon",
"doi-asserted-by": "crossref",
"journal-title": "J. Med. Virol.",
"key": "10.1016/j.heliyon.2023.e16171_bib34",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.1080/07853890.2022.2034936",
"article-title": "Efficacy and safety of three new oral antiviral treatment (molnupiravir, fluvoxamine and Paxlovid) for COVID-19:a meta-analysis",
"author": "Wen",
"doi-asserted-by": "crossref",
"first-page": "516",
"journal-title": "Ann. Med.",
"key": "10.1016/j.heliyon.2023.e16171_bib35",
"volume": "54",
"year": "2022"
},
{
"article-title": "COVID-19: famotidine, histamine, mast cells, and mechanisms",
"author": "Malone",
"journal-title": "Res. Sq.",
"key": "10.1016/j.heliyon.2023.e16171_bib36",
"year": "2020"
},
{
"article-title": "Mast cells contribute to coronavirus-induced inflammation: new anti-inflammatory strategy",
"author": "Kritas",
"first-page": "9",
"journal-title": "J. Biol. Regul. Homeost. Agents",
"key": "10.1016/j.heliyon.2023.e16171_bib37",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1016/j.jbc.2021.100925",
"article-title": "Famotidine inhibits toll-like receptor 3-mediated inflammatory signaling in SARS-CoV-2 infection",
"author": "Mukherjee",
"doi-asserted-by": "crossref",
"journal-title": "J. Biol. Chem.",
"key": "10.1016/j.heliyon.2023.e16171_bib38",
"volume": "297",
"year": "2021"
},
{
"DOI": "10.1136/gutjnl-2020-321852",
"article-title": "Famotidine use and quantitative symptom tracking for COVID-19 in non-hospitalised patients: a case series",
"author": "Janowitz",
"doi-asserted-by": "crossref",
"first-page": "1592",
"journal-title": "Gut",
"key": "10.1016/j.heliyon.2023.e16171_bib39",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.pupt.2020.101942",
"article-title": "Dual-histamine receptor blockade with cetirizine - famotidine reduces pulmonary symptoms in COVID-19 patients",
"author": "Hogan Ii",
"doi-asserted-by": "crossref",
"journal-title": "Pulm. Pharmacol. Ther.",
"key": "10.1016/j.heliyon.2023.e16171_bib40",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1136/thoraxjnl-2020-215322",
"article-title": "Renin-angiotensin system blocker and outcomes of COVID-19: a systematic review and meta-analysis",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "479",
"journal-title": "Thorax",
"key": "10.1016/j.heliyon.2023.e16171_bib41",
"volume": "76",
"year": "2021"
}
],
"reference-count": 41,
"references-count": 41,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2405844023033789"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Effectiveness of famotidine on the risk of poor prognosis in patients with COVID-19: A nationwide cohort study in Korea",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "9"
}