A Retrospective Cohort Study Assessing the Impact of Statin Therapy on Hospital Length of Stay and Inpatient Mortality in COVID-19 Patients
et al., HCA Healthcare Journal of Medicine, doi:10.36518/2689-0216.1546, Oct 2023
Retrospective 26,445 hospitalized COVID-19 patients in the USA, showing higher mortality with remdesivir.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments15.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
Study covers tocilizumab and remdesivir.
|
risk of death, 62.0% higher, OR 1.62, p < 0.001, treatment 5,294, control 21,151, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
13.
Mohammed et al., Bradycardia associated with remdesivir treatment in coronavirus disease 2019 patients: A propensity score-matched analysis, Medicine, doi:10.1097/MD.0000000000044501.
Ho et al., 31 Oct 2023, retrospective, USA, peer-reviewed, 9 authors, study period 1 January, 2020 - 31 August, 2021.
A Retrospective Cohort Study Assessing the Impact of Statin Therapy on Hospital Length of Stay and Inpatient Mortality in COVID-19 Patients
HCA Healthcare Journal of Medicine, doi:10.36518/2689-0216.1546
Background Coronaviruses, known for their crown-like appearance, cause mild gastrointestinal and respiratory diseases. Some cause outbreaks of respiratory diseases, most recently, SARS-CoV-2, the coronavirus disease 2019 (COVID-19). Individuals with COVID-19 are reported to be in both arterial and venous prothrombotic states. In addition to a lipid-lowering effect, statin also has an anti-inflammatory effect, which addresses one of the underlying causes of thrombosis. An in-silico study revealed that statins could directly interact with the main protease enzyme of SARS-CoV-2 and prevent infectivity. Due to these pleiotropic properties, statins may positively impact the outcome of hospitalized patients with COVID-19 infections.
Methods A total of 26 445 acute COVID-19-infected patients were included in this study. Patients were stratified based on home statin use status: no statins, high-intensity statins (atorvastatin 40-80 mg daily and rosuvastatin 20-40 mg daily), and low-to-moderate intensity statins (all other statins). A multivariate generalized linear model and logistic regression were used to predict the hospital length of stay and inpatient mortality, respectively.
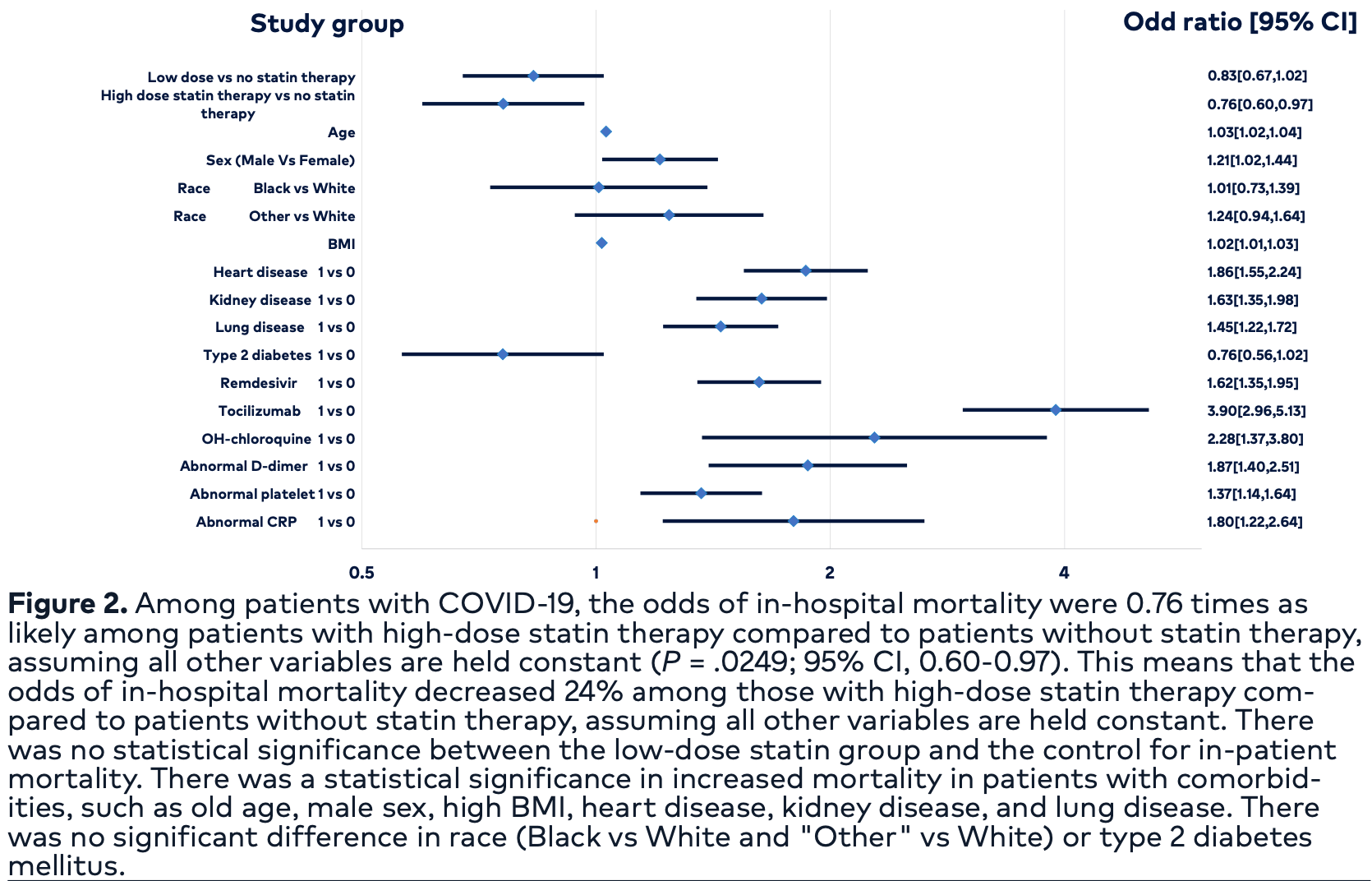
Results The hospital length of stay was compared between low-intensity and high-intensity statin use against no statin therapy. The length of stay was 3.88 days (95% CI, 3.56-4.20; P < .0001) longer among patients with low-dose statin therapy compared to patients without. The length of stay was 4.77 days (95% CI, 4.42-5.13; P <.0001) longer among patients with high-intensity statin therapy than those without. The odds of in-hospital mortality decreased by 24% (OR, 0.76; 95% CI, 0.76-0.97) among those with high-dose statin therapy compared to patients without (P = .02). There was no statistical significance between the low-dose statin group and the no statin group for inpatient mortality.
Conclusion Hospitalized COVID-19 patients on statin therapy, regardless of intensity, are more likely to have a longer length of stay. There may be a mortality benefit in using high-intensity statin in acute COVID-19-infected patients. The results of this study are insufficient to recommend statin therapy for inpatient COVID-19 treatment. However, patients with significant cardiovascular comorbidities, where statins are indicated, should be on these medications, especially amidst the COVID-19 pandemic. Randomized controlled trials are needed to assess the potential in-hospital benefit of statin therapy on COVID-19 patients.
Conflicts of Interest The authors declare they have no conflicts of interest. Drs Ahmed, Eddib, Ho, and Modi are employees of HCA Florida Citrus Hospital, a hospital affiliated with the journal's publisher. Drs Patel and Sorresso are employees of HCA Florida Bayonet Point Hospital, a hospital affiliated with the journal's publisher. Dr Oyesanmi is an employee of HCA Healthcare/USF Morsani College of Medicine Graduate Medical Education, an organization affiliated with the journal's publisher. This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare-affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Author Affiliations
References
Abou-Ismail, Diamond, Kapoor, Arafah, Nayak, The hypercoagulable state in COVID-19: incidence, pathophysiology, and management, Thromb Res, doi:10.1016/j.throm-res.2020.06.02
Cheung, Hung, Chan, Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis, Gastroenterology, doi:10.1053/j.gastro.2020.03.065
Chow, Im, Chiu, The protective association between statins use and adverse outcomes among COVID-19 patients: a systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0253576
Ctt) Collaboration ; Baigent, Blackwell, Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials, Lancet, doi:10.1016/S0140-6736(10)61350-5
Darif, Hammi, Kihel, Idrissi Saik, Guessous et al., The pro-inflammatory cytokines in COVID-19 pathogenesis: what goes wrong?, Microb Pathog, doi:10.1016/j.micpath.2021.104799
De Luca, Debel, Cercek, Impact of SARS-CoV-2 positivity on clinical outcome among STEMI patients undergoing mechanical reperfusion: insights from the ISACS STEMI COVID 19 registry, Atherosclerosis, doi:10.1016/j.atherosclerosis.2021.06.926
Katsoularis, Fonseca-Rodríguez, Farrington, Lindmark, Connolly, Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study, Lancet, doi:10.1016/S0140-6736(21)00896-5
Larosa, Grundy, Waters, Intensive lipid lowering with atorvastatin in patients with stable coronary disease, N Engl J Med, doi:10.1056/NEJ-Moa050461
Lefer, Statins as potent antiinflammatory drugs, Circulation, doi:10.1161/01.cir.0000033635.42612
Morawska, Milton, It is time to address airborne transmission of coronavirus disease 2019 (COVID-19), Clin Infect Dis, doi:10.1093/cid/ciaa939
Schartl, Bocksch, Koschyk, Use of intravascular ultrasound to compare effects of different strategies of lipid-lowering therapy on plaque volume and composition in patients with coronary artery disease, Circulation, doi:10.1161/hc2901.093188
Umakanthan, Senthil, John, The protective role of statins in COVID-19 patients: a retrospective observational study, Transl Med Commun, doi:10.1186/s41231-021-00102-4
DOI record:
{
"DOI": "10.36518/2689-0216.1546",
"ISSN": [
"2689-0216"
],
"URL": "http://dx.doi.org/10.36518/2689-0216.1546",
"author": [
{
"affiliation": [],
"family": "Ho",
"given": "Huy V",
"sequence": "first"
},
{
"affiliation": [],
"family": "Patel",
"given": "Hamish",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ahmed",
"given": "Mohammed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eddib",
"given": "Ahmed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Modi",
"given": "Fagunkumar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sorresso",
"given": "Domenick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mhaskar",
"given": "Rahul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Phrathep",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Oyesanmi",
"given": "Olugbenga",
"sequence": "additional"
}
],
"container-title": "HCA Healthcare Journal of Medicine",
"container-title-short": "HCA Healthcare Journal of Medicine",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
11,
1
]
],
"date-time": "2023-11-01T17:21:42Z",
"timestamp": 1698859302000
},
"deposited": {
"date-parts": [
[
2023,
11,
4
]
],
"date-time": "2023-11-04T11:11:42Z",
"timestamp": 1699096302000
},
"indexed": {
"date-parts": [
[
2023,
11,
5
]
],
"date-time": "2023-11-05T00:42:13Z",
"timestamp": 1699144933779
},
"is-referenced-by-count": 0,
"issue": "5",
"issued": {
"date-parts": [
[
2023,
10,
31
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2023,
10,
31
]
]
}
},
"language": "en",
"member": "22435",
"original-title": [],
"prefix": "10.36518",
"published": {
"date-parts": [
[
2023,
10,
31
]
]
},
"published-online": {
"date-parts": [
[
2023,
10,
31
]
]
},
"publisher": "HCA Healthcare",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://scholarlycommons.hcahealthcare.com/hcahealthcarejournal/vol4/iss5/5"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "A Retrospective Cohort Study Assessing the Impact of Statin Therapy on Hospital Length of Stay and Inpatient Mortality in COVID-19 Patients",
"type": "journal-article",
"volume": "4"
}