Vitamin D Status in Relation to the Clinical Outcome of Hospitalized COVID-19 Patients
et al., Frontiers in Medicine, doi:10.3389/fmed.2022.843737, Mar 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 126 hospitalized COVID-19 patients in the UAE, showing vitamin D deficiency associated with mortality.
This is the 128th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
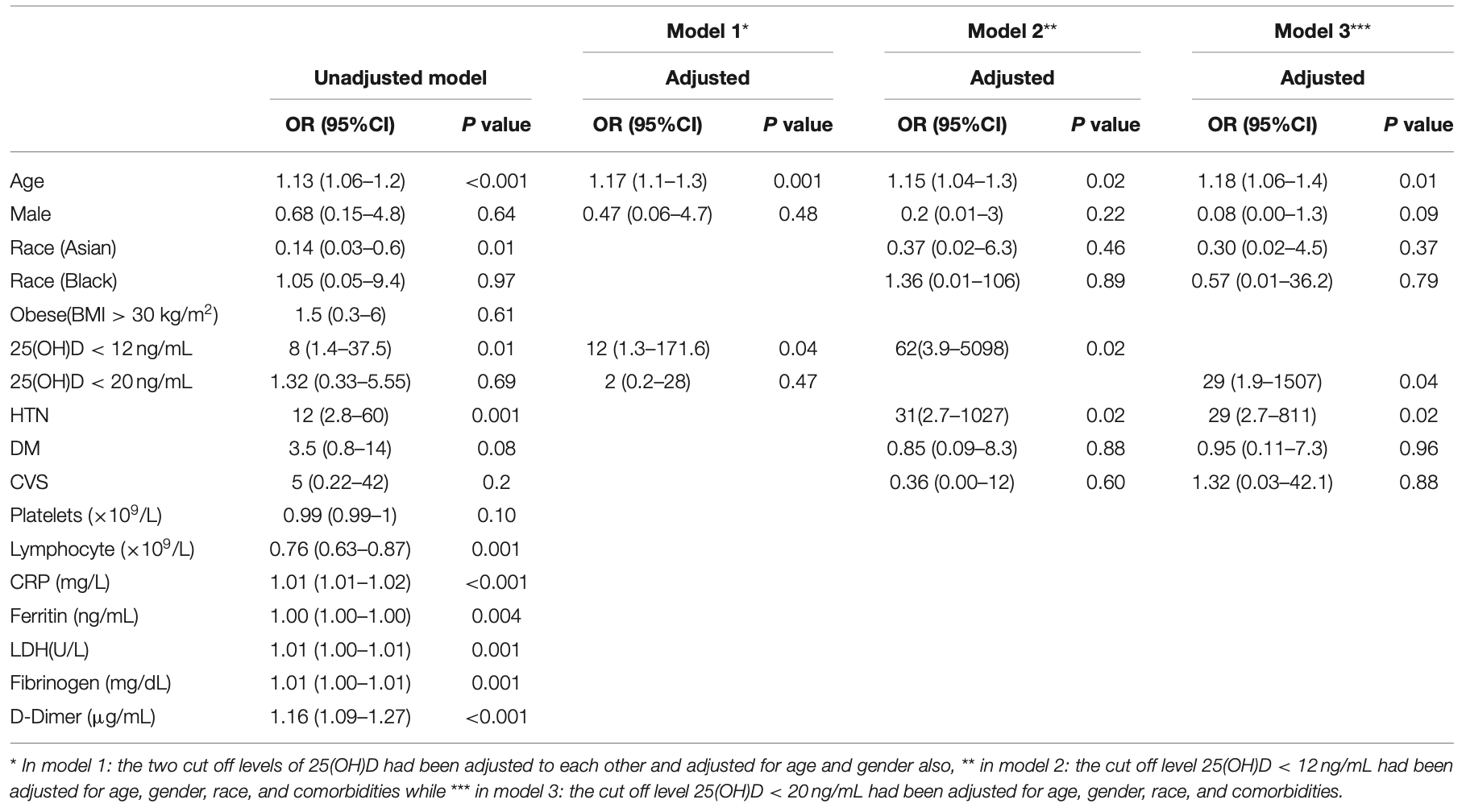
risk of death, 97.7% lower, RR 0.02, p = 0.02, high D levels (≥12ng/mL) 6 of 116 (5.2%), low D levels (<12ng/mL) 3 of 10 (30.0%), NNT 4.0, adjusted per study, inverted to make RR<1 favor high D levels (≥12ng/mL), odds ratio converted to relative risk, multivariable, model 2.
|
|
risk of death, 96.3% lower, RR 0.04, p = 0.04, high D levels (≥20ng/mL) 4 of 64 (6.2%), low D levels (<20ng/mL) 5 of 62 (8.1%), adjusted per study, inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, multivariable, model 3.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hafez et al., 29 Mar 2022, retrospective, United Arab Emirates, peer-reviewed, mean age 43.0, 11 authors.
Contact: waeelhafez@yahoo.com.
Vitamin D Status in Relation to the Clinical Outcome of Hospitalized COVID-19 Patients
Frontiers in Medicine, doi:10.3389/fmed.2022.843737
Coronavirus Disease (COVID-19) is a newly emerged infectious disease that first appeared in China. Vitamin D is a steroid hormone with an anti-inflammatory protective role during viral infections, including SARS-CoV-2 infection, via regulating the innate and adaptive immune responses. The study aimed to investigate the correlation between serum 25-hydroxyvitamin D (25[OH]D) levels and clinical outcomes of COVID-19. This was a retrospective study of 126 COVID-19 patients treated in NMC Royal Hospital, UAE. The mean age of patients was 43 ± 12 years. Eighty three percentage of patients were males, 51% patients were with sufficient (> 20 ng/mL), 41% with insufficient (12-20 ng/mL), and 8% with deficient (<12 ng/mL) serum 25(OH)D levels. There was a statistically significant correlation between vitamin D deficiency and mortality (p = 0.04). There was a statistically significant correlation between 25(OH)D levels and ICU admission (p = 0.03), but not with the need for mechanical ventilation (p = 0.07). The results showed increased severity and mortality by 9 and 13%, respectively, for each one-year increase in age. This effect was maintained after adjustment for age and gender (Model-1) and age, gender, race, and co-morbidities (Models-2,3). 25(OH)D levels (<12 ng/mL) showed a significant increase in mortality by eight folds before adjustments (p = 0.01), by 12 folds in Model-1 (p = 0.04), and by 62 folds in the Model-2. 25(OH)D levels (< 20 ng/mL) showed no association with mortality before adjustment and in Model-1. However, it showed a significant increase in mortality by 29 folds in Model-3. Neither 25(OH)D levels (<12 ng/mL) nor (< 20 ng/mL) were risk factors for severity. Radiological findings were not significantly different among patients with different 25(OH)D levels. Despite observed shorter time till viral clearance and time from cytokine release storm to recovery among patients with sufficient 25(OH)D levels, the findings were statistically insignificant. In conclusion, we demonstrated a significant correlation between vitamin D deficiency and poor COVID-19 outcomes.
CONCLUSION In summary, our study showed a statistically significant correlation between deficient serum 25(OH)D levels (<12 ng/mL) and poor clinical outcomes among COVID-19 patients. Given our findings and vitamin D's safety as well as its broad therapeutic window, public health policies may recommend vitamin D supplementation to improve COVID-19 patient outcomes, particularly among individuals at high risk of SARS-CoV-2 infection and patients with risk factors for poor COVID-19 outcomes and initial vitamin d deficiency. Larger controlled trials are recommended to control possible confounding factors and determine the optimal cut-off values of serum vitamin D levels.
ETHICS STATEMENT The studies involving human participants were reviewed and approved by Abu Dhabi Health COVID-19 Research Ethics Committee (DOH/CVDC/2020/231). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AUTHOR CONTRIBUTIONS WH: literature review, conceptualization, project administration, data analysis and interpretation, revising, writing of original and final draft, and sharing in writing the manuscript. AA, HS, SA, OF, KL, SR, MA, WA, SK, and WE: literature review, analysis, interpretation of data, revising the work, editing, final approval of the version to be published, and agreement to be accountable for all aspects of the work. All authors have contributed to the article, and read and..
References
Aglipay, Birken, Parkin, Loeb, Thorpe et al., Effect of high-dose vs standard-dose wintertime vitamin D supplementation on viral upper respiratory tract infections in young healthy children, JAMA, doi:10.1001/jama.2017.8708
Akbar, Wibowo, Pranata, Setiabudiawan, Low serum 25-hydroxyvitamin D (Vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: a systematic review and meta-analysis, Front Nutr, doi:10.3389/fnut.2021.660420
Alsafar, Grant, Hijazi, Uddin, Alkaabi et al., COVID-19 disease severity and death in relation to vitamin D status among SARS-CoV-2-positive UAE residents, Nutrients, doi:10.3390/nu13051714
Angelidi, Belanger, Lorinsky, Karamanis, Chamorro-Pareja et al., Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients, Mayo Clin Proc, doi:10.1016/j.mayocp.2021.01.001
Arihiro, Nakashima, Matsuoka, Suto, Uchiyama et al., Randomized trial of vitamin D supplementation to prevent seasonal influenza and upper respiratory infection in patients with inflammatory bowel disease, Inflamm Bowel Dis, doi:10.1093/ibd/izy346
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J, doi:10.1136/postgradmedj-2020-138712
Bui, Zhu, Hawkins, Cortez-Resendiz, Bellon, Vitamin D regulation of the immune system and its implications for COVID-19: a mini review, SAGE Open Med, doi:10.1177/20503121211014073
Bwire, Coronavirus: why men are more vulnerable to COVID-19 than women?, SN Compr Clin Med, doi:10.1007/s42399-020-00341-w
Cantorna, Vitamin D and lung infection, Infect Immun, doi:10.1128/IAI.00679-16
Capuano, Rossi, Paolisso, COVID-19 kills more men than women: an overview of possible reasons, Front Cardiovasc Med, doi:10.3389/fcvm.2020.00131
Cereda, Bogliolo, Klersy, Lobascio, Masi et al., Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital, Clini Nutrit, doi:10.1016/j.clnu.2020.10.055
Cucinotta, Vanelli, WHO declares COVID-19 a pandemic, Acta Biomed, doi:10.23750/abm.v91i1.9397
Gruber-Bzura, Vitamin D and influenza-prevention or therapy?, Int J Mol Sci, doi:10.3390/ijms19082419
Haraj, Aziz, Chadli, Dafir, Mjabber et al., Nutritional status assessment in patients with COVID-19 after discharge from the intensive care unit, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2020.09.214
Hofer, Münzker, Schwetz, Ulbing, Hutz et al., Testicular synthesis and vitamin D action, J Clin Endocrinol Metab, doi:10.1210/jc.2014-1690
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Li, Zai, Zhao, Nie, Li et al., Evolutionary history, potential intermediate animal host, and cross-species analyses of SARS-CoV-2, J Med Virol, doi:10.1002/jmv.25731
Liu, Stenger, Li, Wenzel, Tan et al., Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response, Science, doi:10.1126/science.1123933
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS ONE, doi:10.1371/journal.pone.0239799
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Mohan, Cherian, Sharma, Exploring links between vitamin D deficiency and COVID-19, PLoS Pathog, doi:10.1371/journal.ppat.1008874
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol, doi:10.1002/jmv.26360
Orchard, Baldry, Nasim-Mohi, Monck, Saeed et al., Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients, Clin Chem Lab Med, doi:10.1515/cclm-2020-1567
Palacios, Gonzalez, Is vitamin D deficiency a major global public health problem?, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2013.11.003
Papadopoulos, Li, Samplaski, Why does COVID-19 kill more elderly men than women? Is there a role for testosterone?, Andrology, doi:10.1111/andr.12868
Pilz, Frisch, Koertke, Kuhn, Dreier et al., Effect of vitamin D supplementation on testosterone levels in men, Horm Metab Res, doi:10.1055/s-0030-1269854
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients, doi:10.3390/nu12092757
Rhodes, Subramanian, Laird, Kenny, Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity, Aliment Pharmacol Ther, doi:10.1111/apt.15777
Sanghera, Sapkota, Aston, Blackett, Vitamin D Status, Gender differences, and cardiometabolic health disparities, Ann Nutr Metab, doi:10.1159/000458765
Sengupta, Majumder, Majumder, Role of vitamin D in treating COVID-19-associated coagulopathy: problems and perspectives, Mol Cell Biochem, doi:10.1007/s11010-021-04093-6
Shakoor, Feehan, Dhaheri, Ali, Platat et al., Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: Could they help against COVID-19?, Maturitas, doi:10.1016/j.maturitas.2020.08.003
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality, Am J Clin Pathol, doi:10.1093/ajcp/aqaa252
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the editor: vitamin D deficiency in COVID-19: Mixing up cause and consequence, Metabolism, doi:10.1016/j.metabol.2020.154434
Sridhar, Rao, Multani, Jain, Assessment of prevalence of hypovitaminosis D in multiethnic population of the United Arab Emirates, J Adv Pharm Technol Res, doi:10.4103/2231-4040.177202
Taha, Abureesh, Alghamdi, Hassan, Cheikh et al., The relationship between vitamin D and infections including COVID-19: any hopes? IJGM, doi:10.2147/IJGM.S317421
Tan, Wang, Zhang, Ding, Huang et al., Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study, Signal Transduct Target Ther, doi:10.1038/s41392-020-0159-1
Teymoori-Rad, Shokri, Salimi, Marashi, The interplay between vitamin D and viral infections, Rev Med Virol, doi:10.1002/rmv.2032
Tsang, Chan, Cho, Yu, Yim et al., An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies, Expert Rev Anti Infect Ther, doi:10.1080/14787210.2021.1863146
Van Schoor, Lips, Worldwide vitamin D status, Best Pract Res Clin Endocrinol Metab, doi:10.1016/j.beem.2011.06.007
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide induced acute lung injury via regulation of the renin angiotensin system, Mol Med Rep, doi:10.3892/mmr.2017.7546
Zhou, Yang, Wang, Hu, Zhang et al., A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:10.1038/s41586-020-2951-z
DOI record:
{
"DOI": "10.3389/fmed.2022.843737",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2022.843737",
"abstract": "<jats:p>Coronavirus Disease (COVID-19) is a newly emerged infectious disease that first appeared in China. Vitamin D is a steroid hormone with an anti-inflammatory protective role during viral infections, including SARS-CoV-2 infection, via regulating the innate and adaptive immune responses. The study aimed to investigate the correlation between serum 25-hydroxyvitamin D (25[OH]D) levels and clinical outcomes of COVID-19. This was a retrospective study of 126 COVID-19 patients treated in NMC Royal Hospital, UAE. The mean age of patients was 43 ± 12 years. Eighty three percentage of patients were males, 51% patients were with sufficient (&gt; 20 ng/mL), 41% with insufficient (12–20 ng/mL), and 8% with deficient (&lt;12 ng/mL) serum 25(OH)D levels. There was a statistically significant correlation between vitamin D deficiency and mortality (<jats:italic>p</jats:italic> = 0.04). There was a statistically significant correlation between 25(OH)D levels and ICU admission (<jats:italic>p</jats:italic> = 0.03), but not with the need for mechanical ventilation (<jats:italic>p</jats:italic> = 0.07). The results showed increased severity and mortality by 9 and 13%, respectively, for each one-year increase in age. This effect was maintained after adjustment for age and gender (Model-1) and age, gender, race, and co-morbidities (Models-2,3). 25(OH)D levels (&lt;12 ng/mL) showed a significant increase in mortality by eight folds before adjustments (<jats:italic>p</jats:italic> = 0.01), by 12 folds in Model-1 (<jats:italic>p</jats:italic> = 0.04), and by 62 folds in the Model-2. 25(OH)D levels (&lt; 20 ng/mL) showed no association with mortality before adjustment and in Model-1. However, it showed a significant increase in mortality by 29 folds in Model-3. Neither 25(OH)D levels (&lt;12 ng/mL) nor (&lt; 20 ng/mL) were risk factors for severity. Radiological findings were not significantly different among patients with different 25(OH)D levels. Despite observed shorter time till viral clearance and time from cytokine release storm to recovery among patients with sufficient 25(OH)D levels, the findings were statistically insignificant. In conclusion, we demonstrated a significant correlation between vitamin D deficiency and poor COVID-19 outcomes.</jats:p>",
"alternative-id": [
"10.3389/fmed.2022.843737"
],
"author": [
{
"affiliation": [],
"family": "Hafez",
"given": "Wael",
"sequence": "first"
},
{
"affiliation": [],
"family": "Saleh",
"given": "Husam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Arya",
"given": "Arun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alzouhbi",
"given": "Mouhamad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fdl Alla",
"given": "Osman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lal",
"given": "Kumar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kishk",
"given": "Samy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ali",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Raghu",
"given": "Srinivasa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elgaili",
"given": "Walaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdul Hadi",
"given": "Wissam",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
3,
30
]
],
"date-time": "2022-03-30T08:22:36Z",
"timestamp": 1648628556000
},
"deposited": {
"date-parts": [
[
2022,
3,
30
]
],
"date-time": "2022-03-30T08:22:39Z",
"timestamp": 1648628559000
},
"indexed": {
"date-parts": [
[
2023,
4,
13
]
],
"date-time": "2023-04-13T15:24:33Z",
"timestamp": 1681399473182
},
"is-referenced-by-count": 7,
"issued": {
"date-parts": [
[
2022,
3,
29
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
3,
29
]
],
"date-time": "2022-03-29T00:00:00Z",
"timestamp": 1648512000000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.843737/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
3,
29
]
]
},
"published-online": {
"date-parts": [
[
2022,
3,
29
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1038/s41586-020-2951-z",
"article-title": "A pneumonia outbreak associated with a new coronavirus of probable bat origin",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "270",
"journal-title": "Nature.",
"key": "B1",
"volume": "579",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25731",
"article-title": "Evolutionary history, potential intermediate animal host, and cross-species analyses of SARS-CoV-2",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "602",
"journal-title": "J Med Virol.",
"key": "B2",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.23750/abm.v91i1.9397",
"article-title": "WHO declares COVID-19 a pandemic",
"author": "Cucinotta",
"doi-asserted-by": "publisher",
"first-page": "157",
"journal-title": "Acta Biomed.",
"key": "B3",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "Lancet.",
"key": "B4",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1080/14787210.2021.1863146",
"article-title": "An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies",
"author": "Tsang",
"doi-asserted-by": "publisher",
"first-page": "877",
"journal-title": "Expert Rev Anti Infect Ther.",
"key": "B5",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.3390/ijms19082419",
"article-title": "Vitamin D and influenza-prevention or therapy?",
"author": "Gruber-Bzura",
"doi-asserted-by": "publisher",
"first-page": "2419",
"journal-title": "Int J Mol Sci.",
"key": "B6",
"volume": "19",
"year": "2018"
},
{
"DOI": "10.1002/rmv.2032",
"article-title": "The interplay between vitamin D and viral infections",
"author": "Teymoori-Rad",
"doi-asserted-by": "publisher",
"first-page": "e2032",
"journal-title": "Rev Med Virol.",
"key": "B7",
"volume": "29",
"year": "2019"
},
{
"DOI": "10.1016/j.maturitas.2020.08.003",
"article-title": "Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: Could they help against COVID-19?",
"author": "Shakoor",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Maturitas.",
"key": "B8",
"volume": "143",
"year": "2021"
},
{
"DOI": "10.1371/journal.ppat.1008874",
"article-title": "Exploring links between vitamin D deficiency and COVID-19",
"author": "Mohan",
"doi-asserted-by": "publisher",
"first-page": "e1008874",
"journal-title": "PLoS Pathog.",
"key": "B9",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1016/j.beem.2011.06.007",
"article-title": "Worldwide vitamin D status",
"author": "van Schoor",
"doi-asserted-by": "publisher",
"first-page": "671",
"journal-title": "Best Pract Res Clin Endocrinol Metab.",
"key": "B10",
"volume": "25",
"year": "2011"
},
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"article-title": "Is vitamin D deficiency a major global public health problem?",
"author": "Palacios",
"doi-asserted-by": "publisher",
"first-page": "138",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "B11",
"volume": "144",
"year": "2014"
},
{
"DOI": "10.1093/ibd/izy346",
"article-title": "Randomized trial of vitamin D supplementation to prevent seasonal influenza and upper respiratory infection in patients with inflammatory bowel disease",
"author": "Arihiro",
"doi-asserted-by": "publisher",
"first-page": "1088",
"journal-title": "Inflamm Bowel Dis",
"key": "B12",
"volume": "25",
"year": "2019"
},
{
"DOI": "10.1001/jama.2017.8708",
"article-title": "Effect of high-dose vs standard-dose wintertime vitamin D supplementation on viral upper respiratory tract infections in young healthy children",
"author": "Aglipay",
"doi-asserted-by": "publisher",
"first-page": "245",
"journal-title": "JAMA.",
"key": "B13",
"volume": "318",
"year": "2017"
},
{
"DOI": "10.1111/apt.15777",
"article-title": "Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity",
"author": "Rhodes",
"doi-asserted-by": "publisher",
"first-page": "1434",
"journal-title": "Aliment Pharmacol Ther.",
"key": "B14",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.1016/j.clnesp.2020.09.214",
"article-title": "Nutritional status assessment in patients with COVID-19 after discharge from the intensive care unit",
"author": "Haraj",
"doi-asserted-by": "publisher",
"first-page": "423",
"journal-title": "Clin Nutr ESPEN.",
"key": "B15",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1111/febs.15495",
"article-title": "Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study",
"author": "Merzon",
"doi-asserted-by": "publisher",
"first-page": "3693",
"journal-title": "FEBS J.",
"key": "B16",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"article-title": "The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality",
"author": "Ilie",
"doi-asserted-by": "publisher",
"first-page": "1195",
"journal-title": "Aging Clin Exp Res",
"key": "B17",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1515/cclm-2020-1567",
"article-title": "Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients",
"author": "Orchard",
"doi-asserted-by": "publisher",
"first-page": "1155",
"journal-title": "Clin Chem Lab Med.",
"key": "B18",
"volume": "59",
"year": "2021"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"article-title": "Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality",
"author": "De Smet",
"doi-asserted-by": "publisher",
"first-page": "381",
"journal-title": "Am J Clin Pathol.",
"key": "B19",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.3390/nu12092757",
"article-title": "Vitamin D deficiency and outcome of COVID-19 patients",
"author": "Radujkovic",
"doi-asserted-by": "publisher",
"first-page": "2757",
"journal-title": "Nutrients.",
"key": "B20",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26360",
"article-title": "Vitamin D insufficiency as a potential culprit in critical COVID-19 patients",
"author": "Munshi",
"doi-asserted-by": "publisher",
"first-page": "733",
"journal-title": "J Med Virol.",
"key": "B21",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"article-title": "Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients",
"author": "Angelidi",
"doi-asserted-by": "publisher",
"first-page": "875",
"journal-title": "Mayo Clin Proc.",
"key": "B22",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"author": "Baktash",
"doi-asserted-by": "publisher",
"first-page": "442",
"journal-title": "Postgrad Med J.",
"key": "B23",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239799",
"article-title": "Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection",
"author": "Maghbooli",
"doi-asserted-by": "publisher",
"first-page": "e0239799",
"journal-title": "PLoS ONE.",
"key": "B24",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.4103/2231-4040.177202",
"article-title": "Assessment of prevalence of hypovitaminosis D in multiethnic population of the United Arab Emirates",
"author": "Sridhar",
"doi-asserted-by": "publisher",
"first-page": "48",
"journal-title": "J Adv Pharm Technol Res.",
"key": "B25",
"volume": "7",
"year": "2016"
},
{
"DOI": "10.3390/nu13051714",
"article-title": "COVID-19 disease severity and death in relation to vitamin D status among SARS-CoV-2-positive UAE residents",
"author": "AlSafar",
"doi-asserted-by": "publisher",
"first-page": "1714",
"journal-title": "Nutrients.",
"key": "B26",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2021.660420",
"article-title": "Low serum 25-hydroxyvitamin D (Vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: a systematic review and meta-analysis",
"author": "Akbar",
"doi-asserted-by": "publisher",
"first-page": "660420",
"journal-title": "Front Nutr.",
"key": "B27",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"article-title": "Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital",
"author": "Cereda",
"doi-asserted-by": "publisher",
"first-page": "2469",
"journal-title": "Clini Nutrit. (Edinburgh, Scotland).",
"key": "B28",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1007/s42399-020-00341-w",
"article-title": "Coronavirus: why men are more vulnerable to COVID-19 than women?",
"author": "Bwire",
"doi-asserted-by": "publisher",
"first-page": "874",
"journal-title": "SN Compr Clin Med.",
"key": "B29",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.3389/fcvm.2020.00131",
"article-title": "COVID-19 kills more men than women: an overview of possible reasons",
"author": "Capuano",
"doi-asserted-by": "publisher",
"first-page": "131",
"journal-title": "Front Cardiovasc Med.",
"key": "B30",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1177/20503121211014073",
"article-title": "Vitamin D regulation of the immune system and its implications for COVID-19: a mini review",
"author": "Bui",
"doi-asserted-by": "publisher",
"first-page": "20503121211014073",
"journal-title": "SAGE Open Med",
"key": "B31",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1007/s11010-021-04093-6",
"article-title": "Role of vitamin D in treating COVID-19-associated coagulopathy: problems and perspectives",
"author": "Sengupta",
"doi-asserted-by": "publisher",
"first-page": "2421",
"journal-title": "Mol Cell Biochem.",
"key": "B32",
"volume": "476",
"year": "2021"
},
{
"DOI": "10.1111/andr.12868",
"article-title": "Why does COVID-19 kill more elderly men than women? Is there a role for testosterone?",
"author": "Papadopoulos",
"doi-asserted-by": "publisher",
"first-page": "65",
"journal-title": "Andrology",
"key": "B33",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1055/s-0030-1269854",
"article-title": "Effect of vitamin D supplementation on testosterone levels in men",
"author": "Pilz",
"doi-asserted-by": "publisher",
"first-page": "223",
"journal-title": "Horm Metab Res",
"key": "B34",
"volume": "43",
"year": "2011"
},
{
"DOI": "10.1210/jc.2014-1690",
"article-title": "Testicular synthesis and vitamin D action",
"author": "Hofer",
"doi-asserted-by": "publisher",
"first-page": "3766",
"journal-title": "J Clin Endocrinol Metab.",
"key": "B35",
"volume": "99",
"year": "2014"
},
{
"DOI": "10.1159/000458765",
"article-title": "Vitamin D Status, Gender differences, and cardiometabolic health disparities",
"author": "Sanghera",
"doi-asserted-by": "publisher",
"first-page": "79",
"journal-title": "Ann Nutr Metab.",
"key": "B36",
"volume": "70",
"year": "2017"
},
{
"DOI": "10.1038/s41392-020-0159-1",
"article-title": "Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study",
"author": "Tan",
"doi-asserted-by": "publisher",
"first-page": "33",
"journal-title": "Signal Transduct Target Ther.",
"key": "B37",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.2147/IJGM.S317421",
"article-title": "The relationship between vitamin D and infections including COVID-19: any hopes?",
"author": "Taha",
"doi-asserted-by": "publisher",
"first-page": "3849",
"journal-title": "IJGM.",
"key": "B38",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2020.154434",
"article-title": "Letter to the editor: vitamin D deficiency in COVID-19: Mixing up cause and consequence",
"author": "Smolders",
"doi-asserted-by": "publisher",
"first-page": "154434",
"journal-title": "Metabolism.",
"key": "B39",
"volume": "115",
"year": "2021"
},
{
"DOI": "10.3892/mmr.2017.7546",
"article-title": "Vitamin D alleviates lipopolysaccharide induced acute lung injury via regulation of the renin angiotensin system",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "7432",
"journal-title": "Mol Med Rep.",
"key": "B40",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1126/science.1123933",
"article-title": "Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "1770",
"journal-title": "Science.",
"key": "B41",
"volume": "311",
"year": "2006"
},
{
"DOI": "10.1128/IAI.00679-16",
"article-title": "Vitamin D and lung infection",
"author": "Cantorna",
"doi-asserted-by": "publisher",
"first-page": "3094",
"journal-title": "Infect Immun.",
"key": "B42",
"volume": "84",
"year": "2016"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data",
"author": "Martineau",
"doi-asserted-by": "publisher",
"first-page": "i6583",
"journal-title": "BMJ.",
"key": "B43",
"volume": "356",
"year": "2017"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.843737/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin D Status in Relation to the Clinical Outcome of Hospitalized COVID-19 Patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "9"
}
